Table of Contents
Definition / general | Terminology | Epidemiology | Sites | Etiology | Diagrams / tables | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Differential diagnosis | Additional referencesCite this page: Nagarajan P, Suo L. Myiasis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorbotfly.html. Accessed April 19th, 2024.
Definition / general
- Infestation by larvae of the human botfly (Dermatobia hominis) and tumbu fly (Cordylobia anthropophaga) are common causes of myiasis
- Skin lesions are due to growth and burrowing of the larva, which feed on the host tissues, liquid body substance or ingested food
- Other cutaneous locations such as eye, mucosa, breast and gastrointestinal tract can be affected (West Afr J Med 2013;32:149)
Terminology
- Human botfly, Dermatobia hominis, myiasis
Epidemiology
- Tropical and subtropical areas with warm and humid climate, such as the Americas, Central and South Africa are most common (CDC: Parasites - Myiasis [Accessed 10 October 2018])
- Rarely seen in the continental United States; most commonly seen in travelers
Sites
- Any body site can be affected, especially wounded or exposed skin (Infect Genet Evol 2014;23:209)
- Other cutaneous and mucosal locations such as eyes and gastrointestinal tract can also be affected (West Afr J Med 2013;32:149)
- When mucosal sites such as nasal sinuses are affected, the sequelae are grave (J Clin Neurosci 2013;20:1178, BMJ Case Rep 2010 Dec 29;2010)
Etiology
Life cycle:
- In endemic areas, D. hominis flies typically lay their eggs on mosquitoes, which in turn deposit them on warmblooded mammals such as humans
- In wound myiasis, an open wound or orifice attracts flies to deposit their eggs
- The eggs hatch in the skin, stimulated by the heat from the host
- The larvae mature through 3 stages during which they develop posterior spines, which makes them difficult to dislodge
- 5 - 10 weeks after deposition, the mature third stage larvae drop from the host and complete the pupal stage in soil
- Adult botfly emerges from soil after 4 - 11 weeks
Clinical features
- May clinically resemble insect bites, allergic reactions, herpes virus or molluscum contagiosum
- Furuncular myiasis: a pruritic papule that develops within 24 hours of penetration, enlarging to 1 - 3 cm in diameter
- These lesions can be painful or tender and may become crusted and purulent
- In wound myiasis, the larvae are deposited in a suppurating wound or on decomposing flesh
- Creeping (or migratory) cutaneous myiasis resembles cutaneous larva migrans, but the larvae migrate more slowly, persist for longer (often months) and are larger than helminth larvae
- In most cases, myiasis is self limited with minimal morbidity
- Secondary infection by bacteria may be a complication
Diagnosis
- Thorough physical examination and documentation of relevant exposure history, including travel to warm humid climates
- Surgical extraction and histologic examination can confirm the presence of larvae
- Supportive travel history
Case reports
- 10 year old Indian boy with redness of both eyes (Ocul Immunol Inflamm 2011;19:444)
- 29 year old man with an unusual cause of an abscess (BMJ Case Rep 2014 Oct 21;2014)
- 50 year old male traveler to Belize (CJEM 2007;9:380)
- 61 year old woman traveler to Belize with pruritic lesions on back, thigh and supraclavicular area (Arch Pathol Lab Med 2001;125:453)
- Patient returning from Bolivia with nonhealing furuncle containing botfly (Pritt: Creepy Dreadful Wonderful Parasites Blog - Case of the Week 505 [Accessed 9 October 2018])
Treatment
- The major reasons for treatment are reduction of pain, cosmesis, psychological relief and to prevent secondary infections
- Surgical extraction of larvae is the key treatment
- Systemic medication: broad spectrum antibiotics, oral steroid and ivermectin may also be used (Ocul Immunol Inflamm 2011;19:444)
Gross description
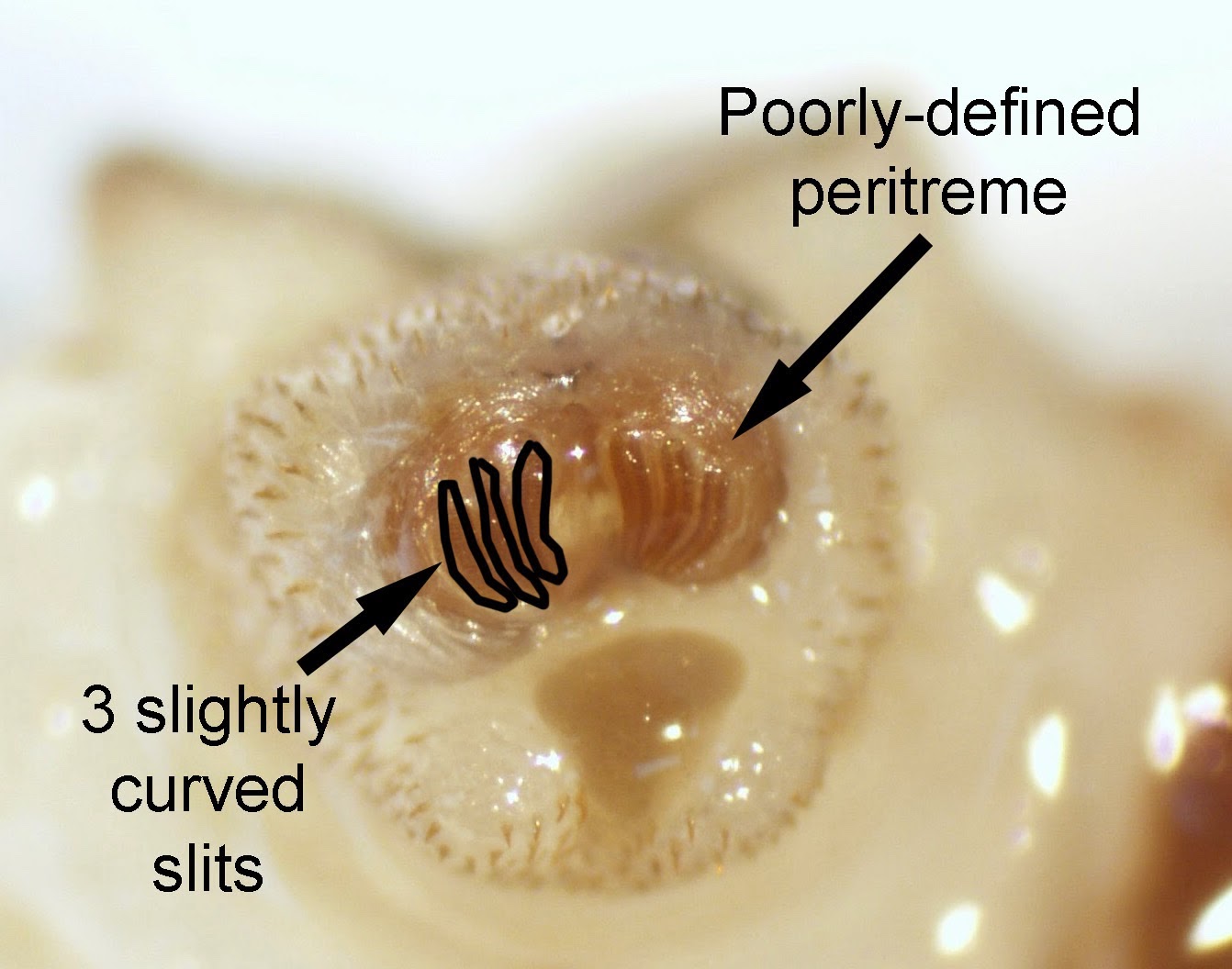
- Helpful features for identification (Pritt: Creepy Dreadful Wonderful Parasites Blog - Answer to Case 505 [Accessed 9 October 2018]):
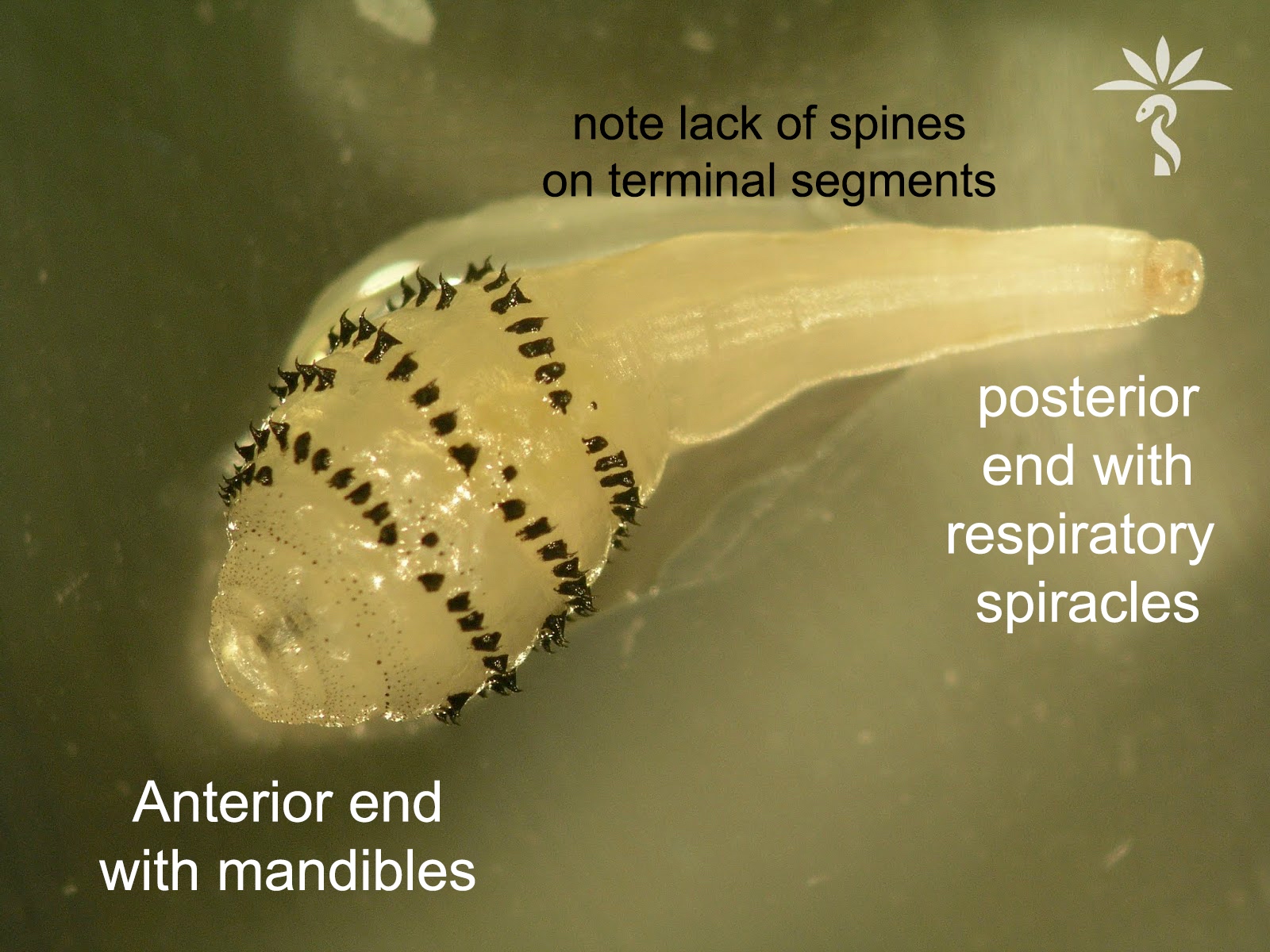
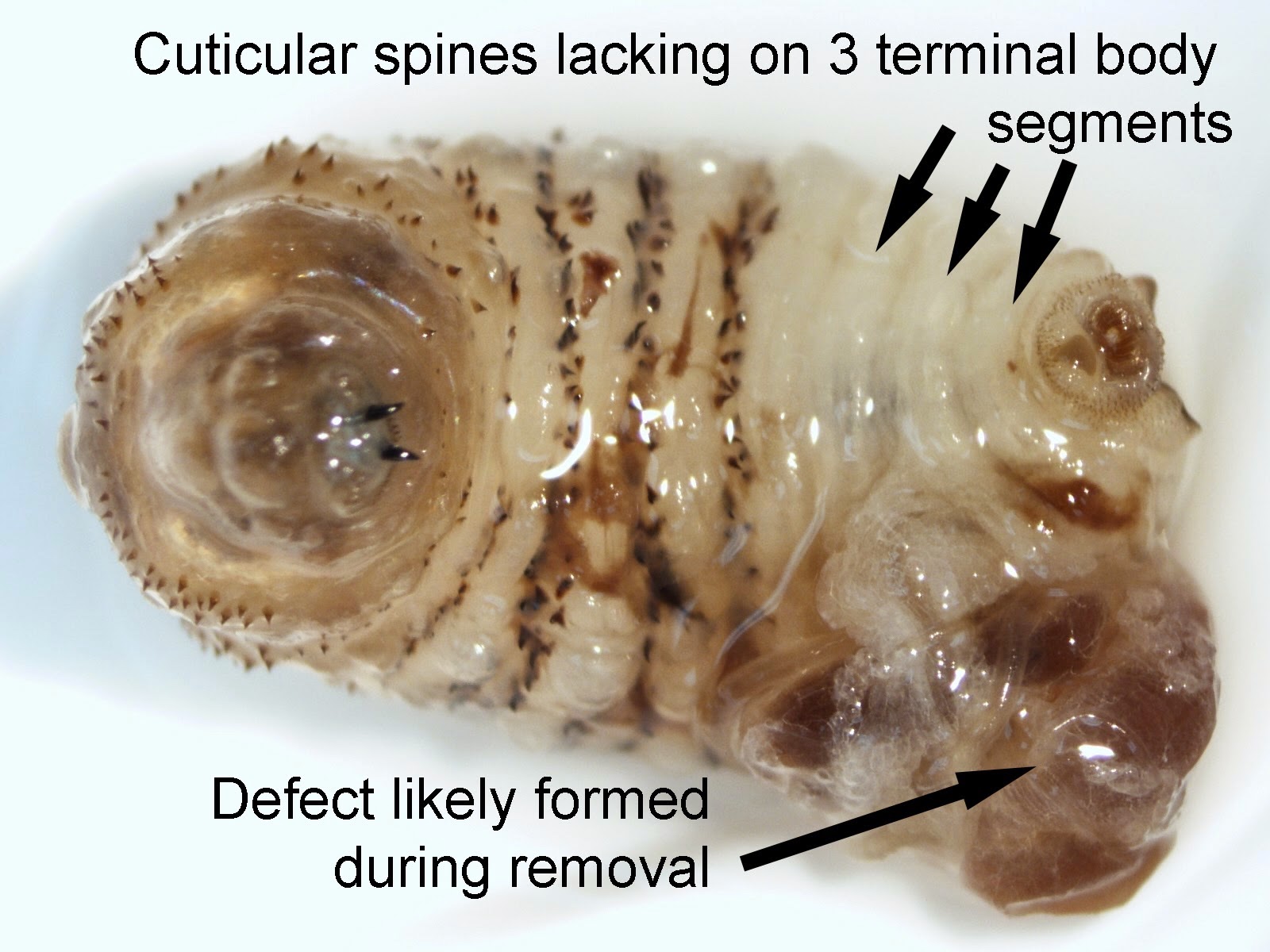
- Overall robust and somewhat pear shaped body with a narrow posterior
- Large spines on all but the terminal 3 body segments
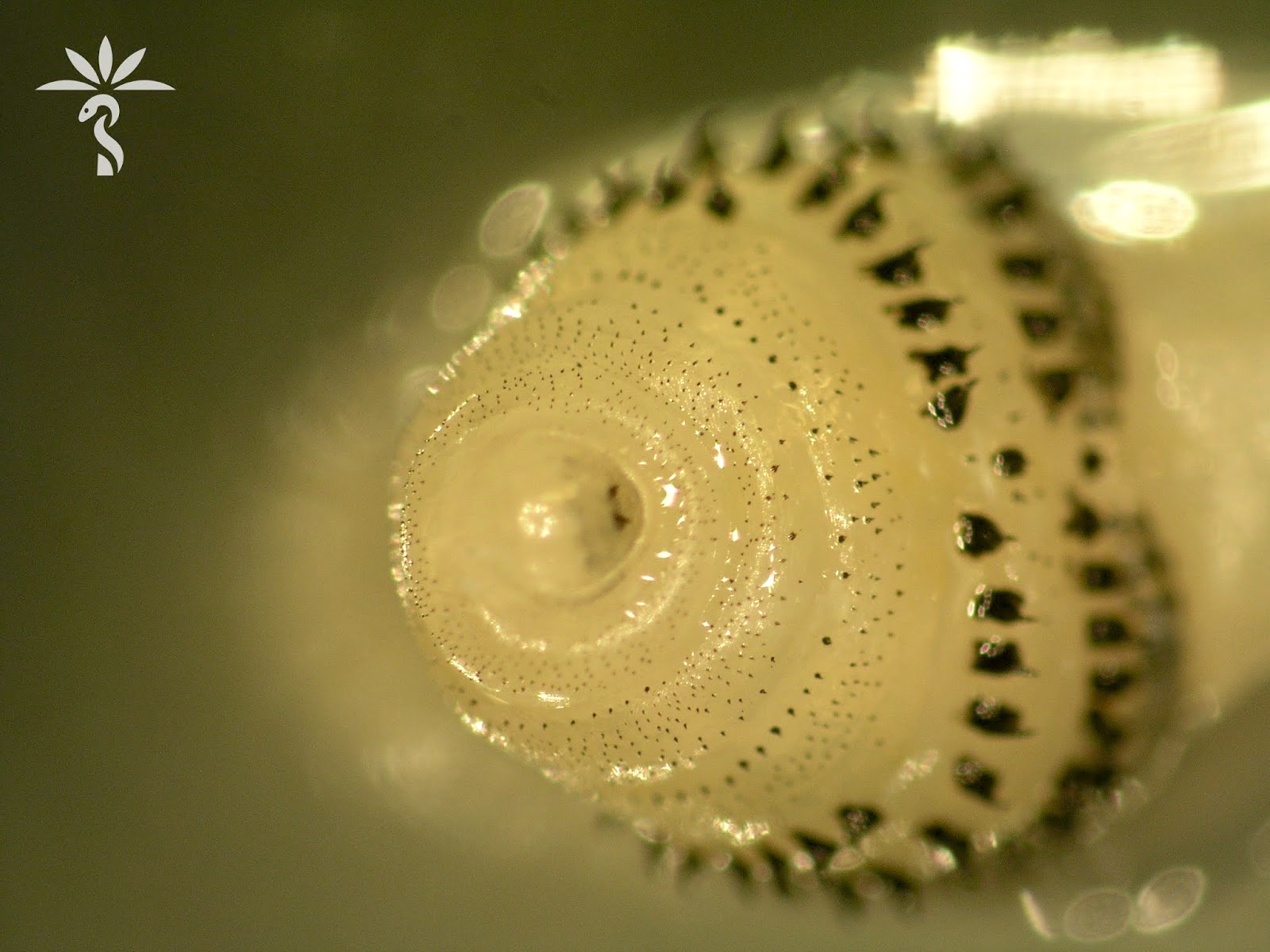
- Posterior spiracle with 3 slightly curved slits and a weak peritreme
Microscopic (histologic) description
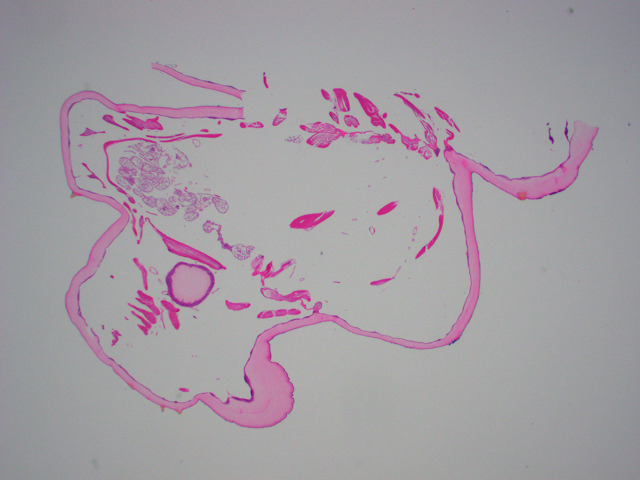
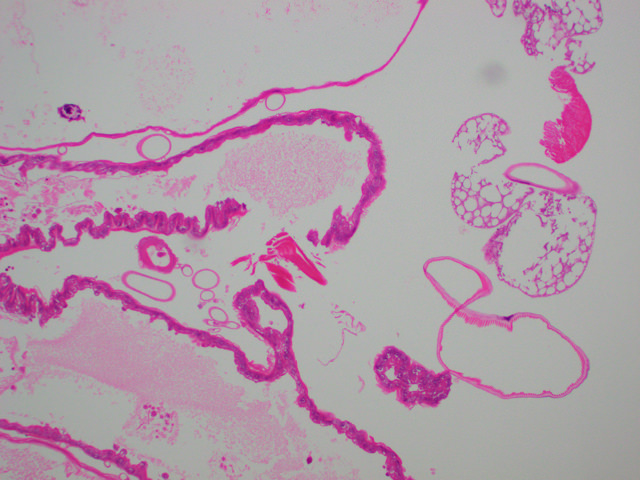
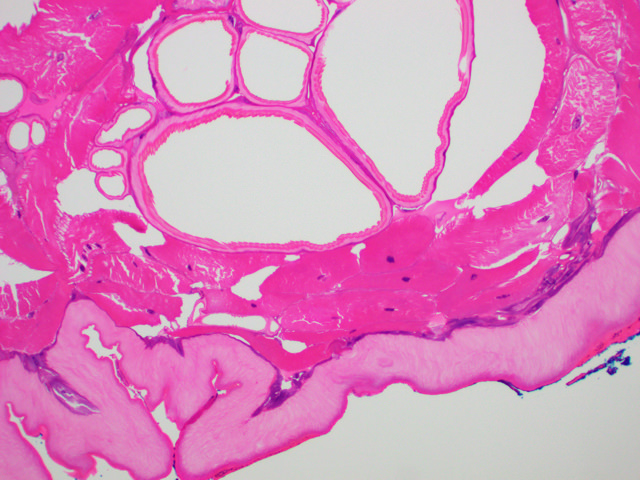
- Histologically, a mixed acute and chronic inflammatory infiltrate composed of varying proportions of neutrophils (early), lymphocytes, plasma cells and histiocytes (late), admixed with eosinophils (J Am Acad Dermatol 2004;50:S26)
- Histologically, larvae are characterized by an undulating chitinous exoskeleton and pigmented spines (setae) protruding from exoskeleton
Microscopic (histologic) images
Videos
Differential diagnosis
- Furuncular cutaneous myiasis should be differentiated from:
- Ruptured epidermoid cyst
- Abscess
- Furunculosis
- Foreign body reaction
- Exaggerated arthropod bite reaction
- Lymphadenopathy
- Tungiasis
- Onchocerciasis
- Tick infestation (tick head burrows; lack pigmented setae)
- Creeping cutaneous myiasis should be differentiated from:
- Scabies (scabies or burrows may be seen in biopsies)
- Larva migrans
- Cellulitis (no parasite seen)