Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Immunofluorescence description | Immunofluorescence images | Videos | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Occidental M, Kim RH. Bullous pemphigoid. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorbullouspemphigoid.html. Accessed April 23rd, 2024.
Definition / general
- Most common autoimmune blistering skin disorder
- Characterized by autoantibodies against hemidesmosomal antigens, bullous pemphigoid antigens 1 and 2
- Patients present with tense bullae on an erythematous base and pruritus
Essential features
- Subepidermal blister with eosinophils, often accompanied by eosinophilic spongiosis
- Early lesions can appear urticarial or eczematous
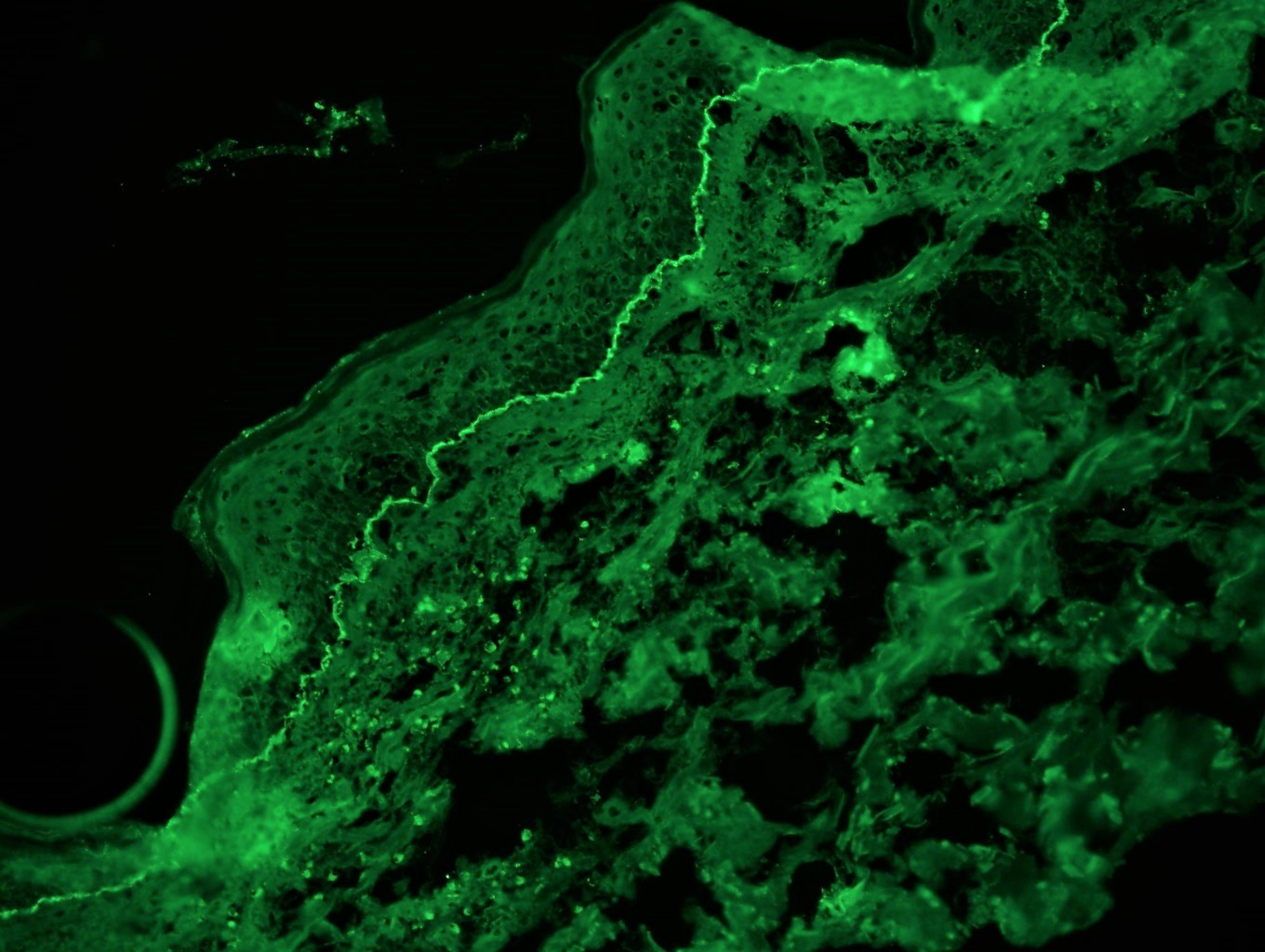
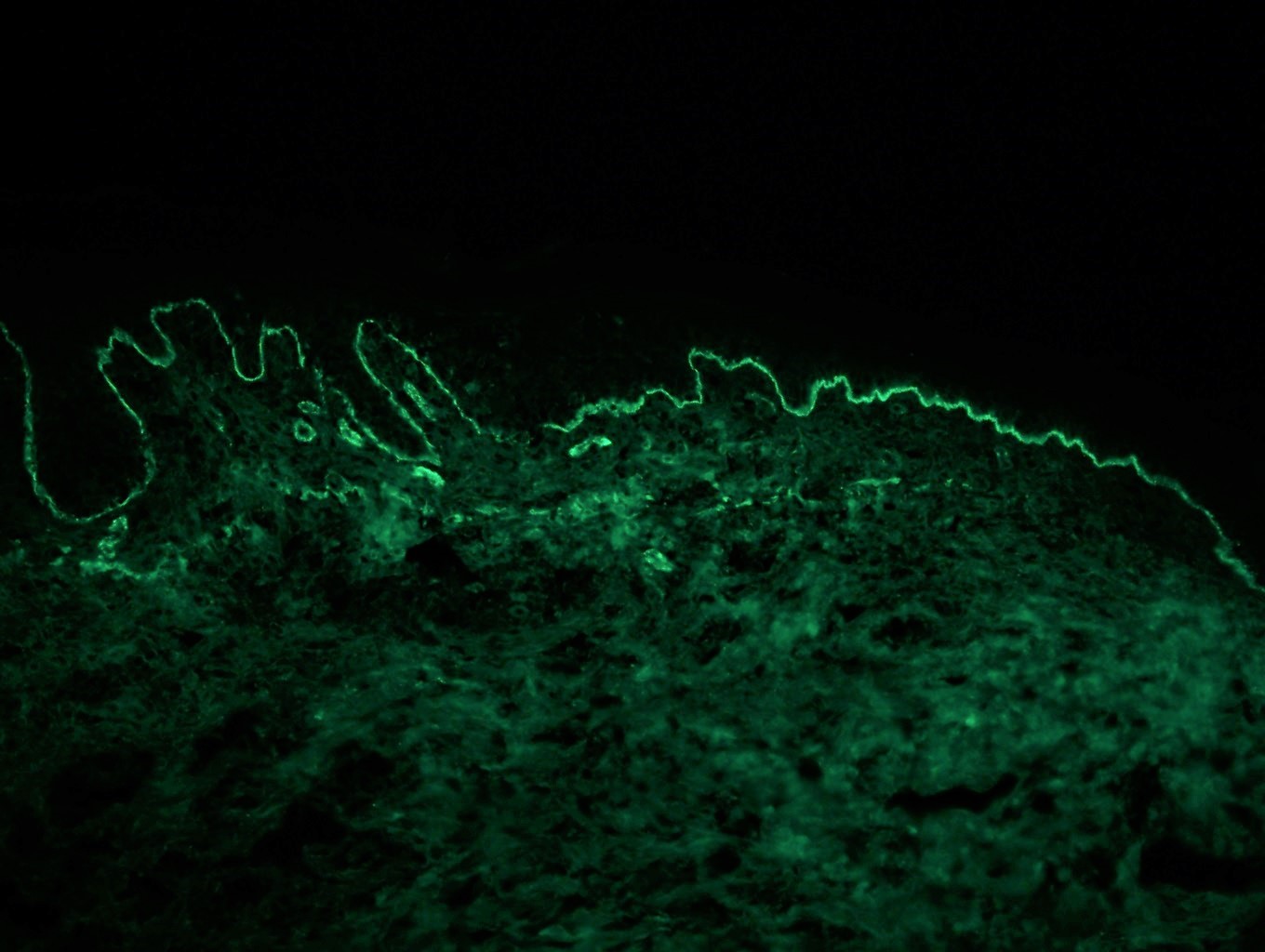
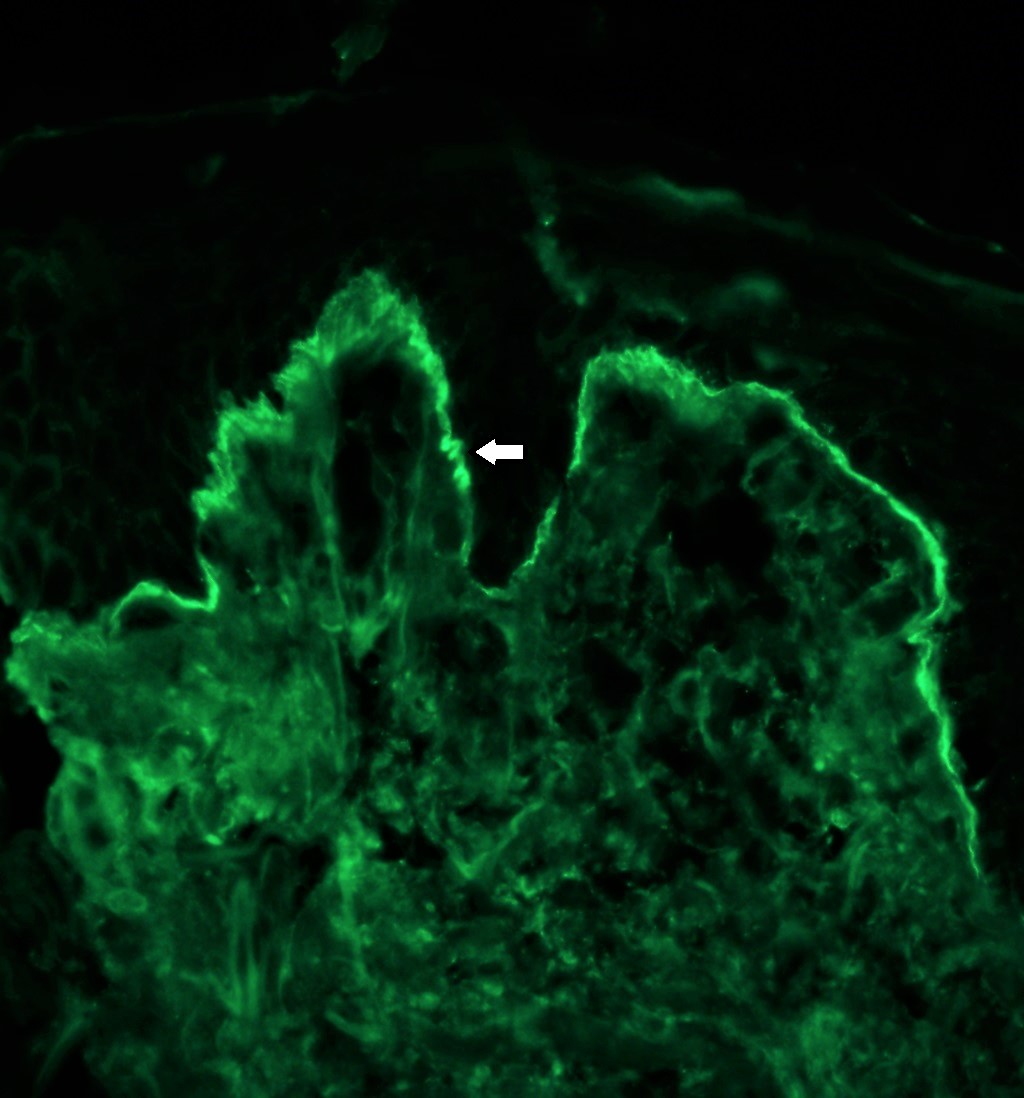
- Direct immunofluorescence (DIF): linear C3 > IgG along the basement membrane zone, n-serrated pattern
- DIF on salt split skin: immunoreactants deposited on the blister roof (40%) or on both roof and floor (60%)
- Indirect immunofluoresence: can be performed on human skin or monkey esophagus; immunoreactants localize to blister roof (95%) on salt split analysis
- Treatment: corticosteroids, tetracyclines, cytotoxic steroid sparing agents and rituximab, IVIG infusions
ICD coding
- ICD-10: L12.0 - bullous pemphigoid
Epidemiology
- Incidence rate: 7.63 per 100,000 person years (Br J Dermatol 2021;184:68)
- Increases with age
- 80% of subepidermal immunobullous dermatoses
- M = F
- Elderly > children and infants
Sites
- Inner and anterior thighs, groin, flexor surfaces of upper extremities, lower abdomen
- Childhood bullous pemphigoid: vulvar localization is most common
Pathophysiology
- Development of IgG autoantibodies against hemidesmosomal proteins BPAG1 and BPAG2
Etiology
- Autoimmune disease associated with bullous pemphigoid antigen 180 (BP180, BPAG2) and bullous pemphigoid antigen 230 (BP230, BPAG1, BPAG1e) (Am J Clin Dermatol 2017;18:513)
- Associated with medication use:
- Anti-PD1 immunotherapy
- Diuretics, ACE inhibitors, antibiotics, D penicillamine
- Pediatric cases associated with viral illness and immunization (BMC Pediatr 2017;17:60)
Clinical features
- Prodrome phase: mild to severe pruritus and eczematous, papular or urticarial lesions
- Bullous stage: tense bullae containing serous fluid or hemorrhage
- Unusual to have mucosal involvement (seen in oral cavity in 10 - 30% of cases) (Lancet 2013;381:320)
Diagnosis
- Requires histological evaluation in addition to confirmation by direct immunofluorescence studies or detection of circulating autoantibodies
Laboratory
- Enzyme linked immunosorbent assay (ELISA):
- NC16A domain of BPAG2: sensitivity = 84%, specificity = 98% (J Dermatol Sci 2002;30:224)
- BPAG1: sensitivity = 48%, specificity = 94% (Arch Dermatol Res 2016;308:269)
Prognostic factors
- 30% relapse during first year of treatment (N Engl J Med 2002;346:321)
- Risk factors: disease severity, neurological conditions, positive anti-BP180 antibody titers (Ann Med 2018;50:234)
Case reports
- 61 year old man with tender blisters on his feet, upper legs and central upper back, diagnosed with dyshidrosiform bullous pemphigoid (Cureus 2020;12:e6630)
- 72 year old woman with metastatic non small cell lung cancer develops nivolumab induced bullous pemphigoid (Oncologist 2018;23:1119)
- 84 year old woman with clear cell renal cell carcinoma and widespread paraneoplastic bullous pemphigoid (Urol Case Rep 2020;30:101119)
- 88 year old woman with newly diagnosed melanoma and associated bullous pemphigoid (Melanoma Res 2017;27:65)
Treatment
- First line: topical or systemic corticosteroids
- Systemic corticosteroid therapy should be accompanied by steroid sparing agents whenever possible (Am J Clin Dermatol 2017;18:513)
- Steroid sparing agents (mycophenolate mofetil, methotrexate)
- Tetracycline
- IVIG in steroid resistant disease
- Rituximab or IVIG for refractory disease (not resistant)
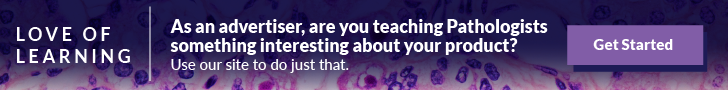
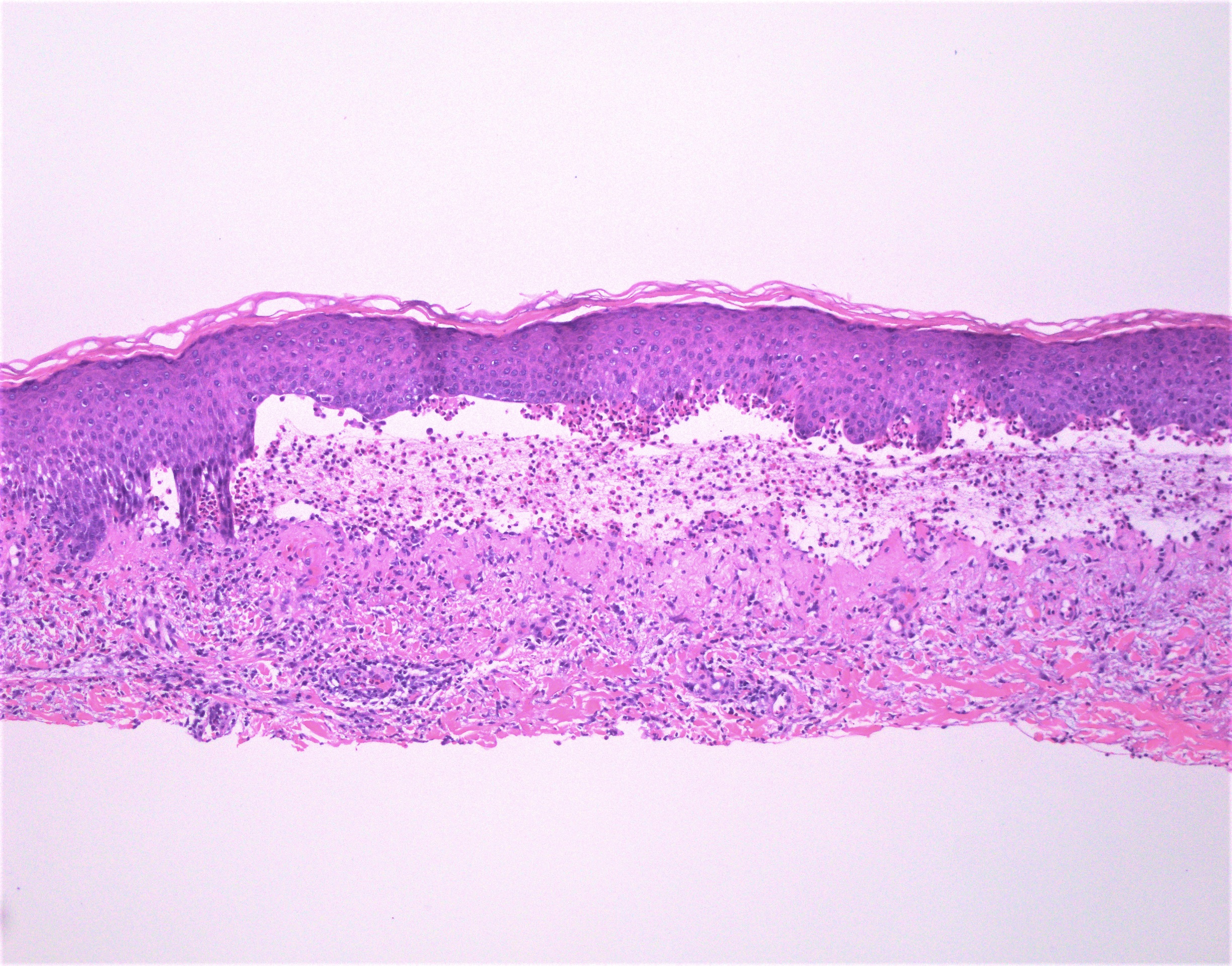
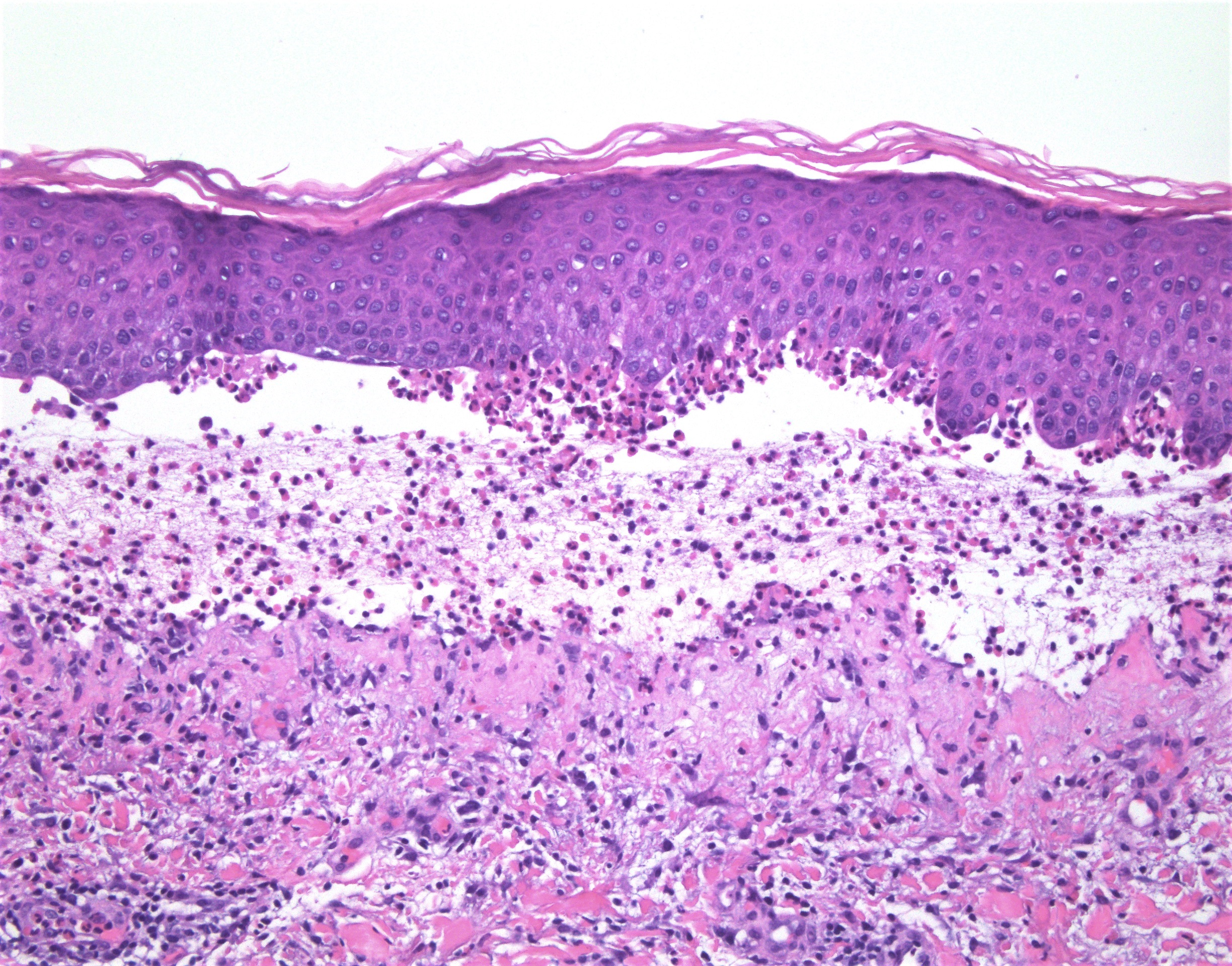
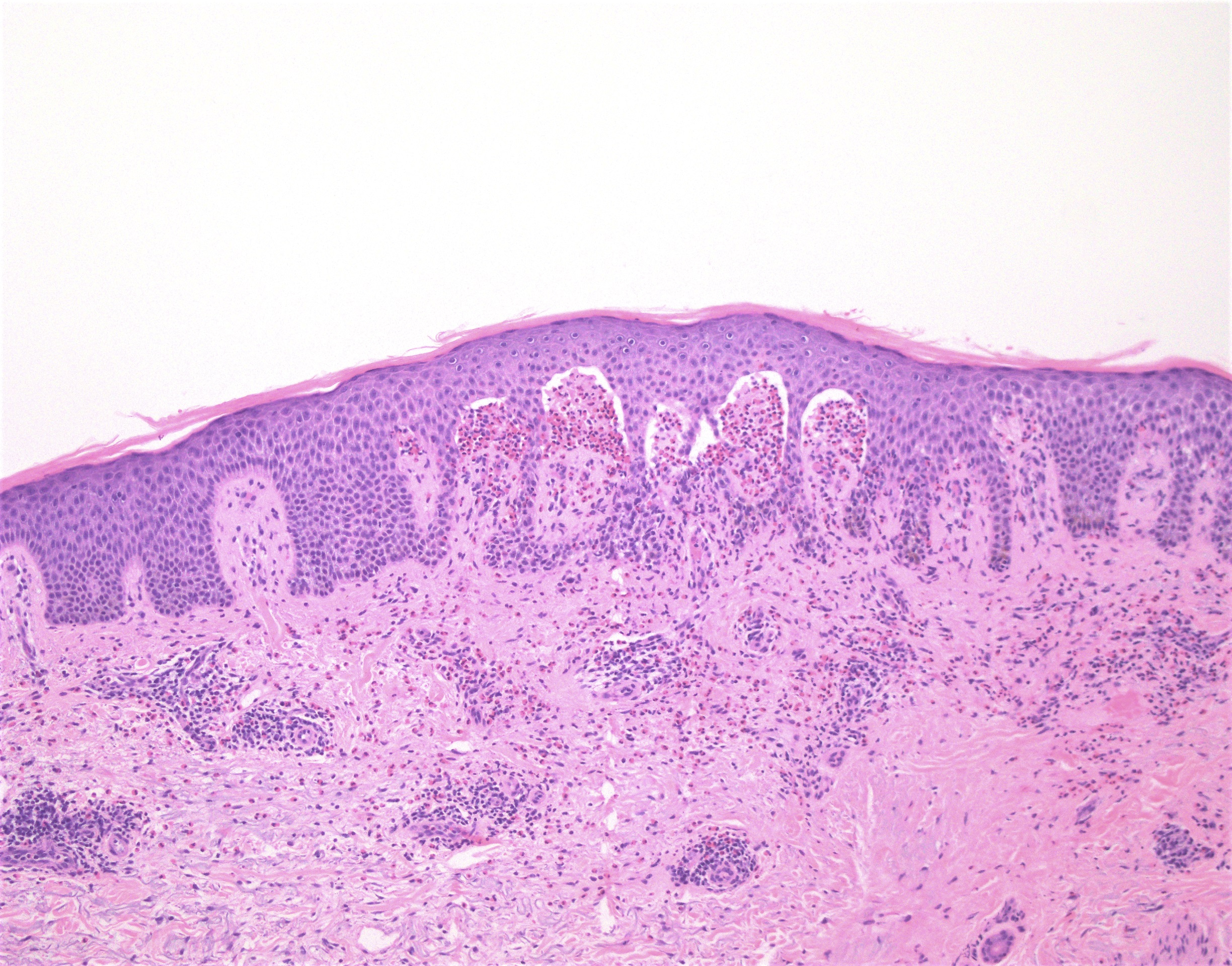
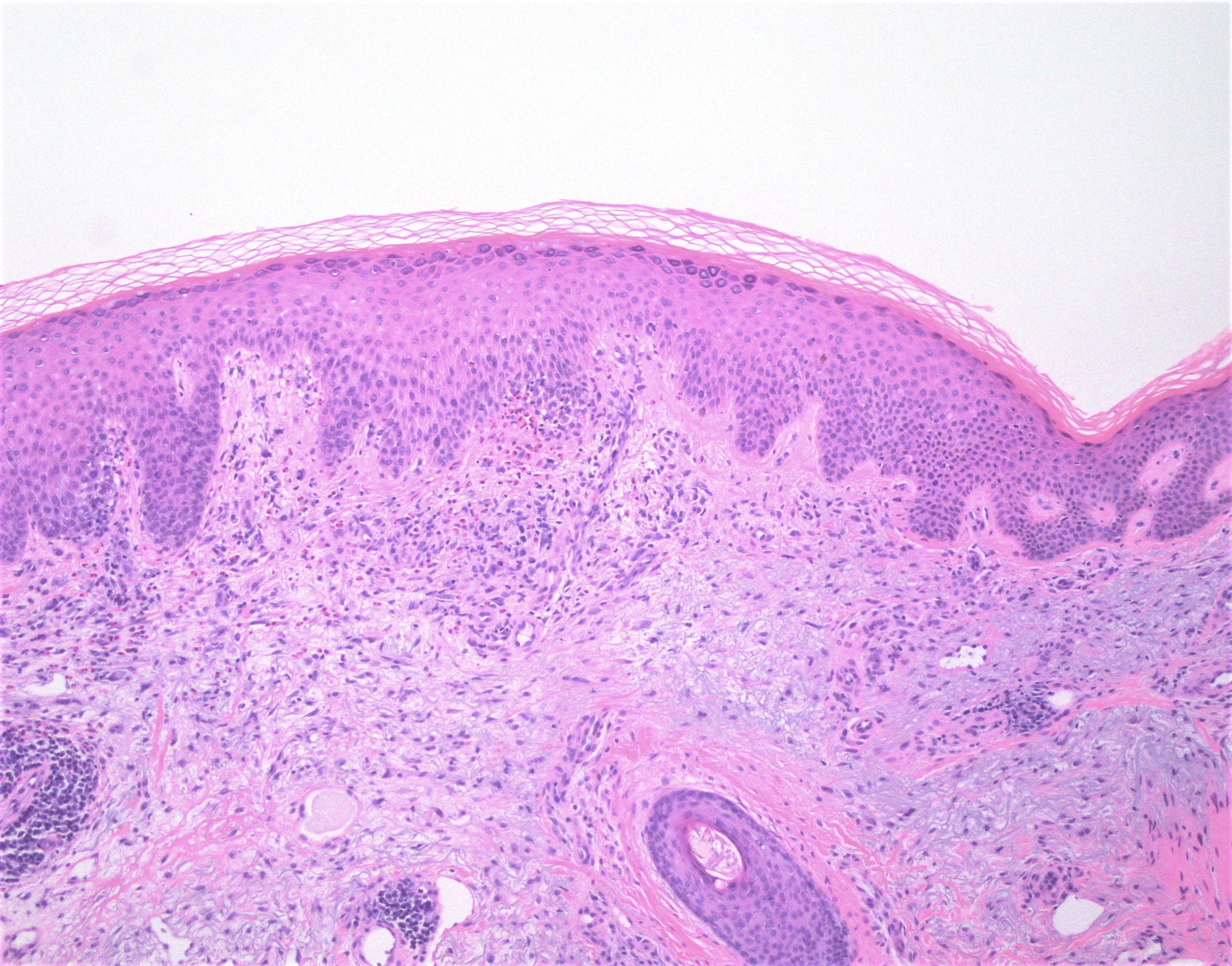
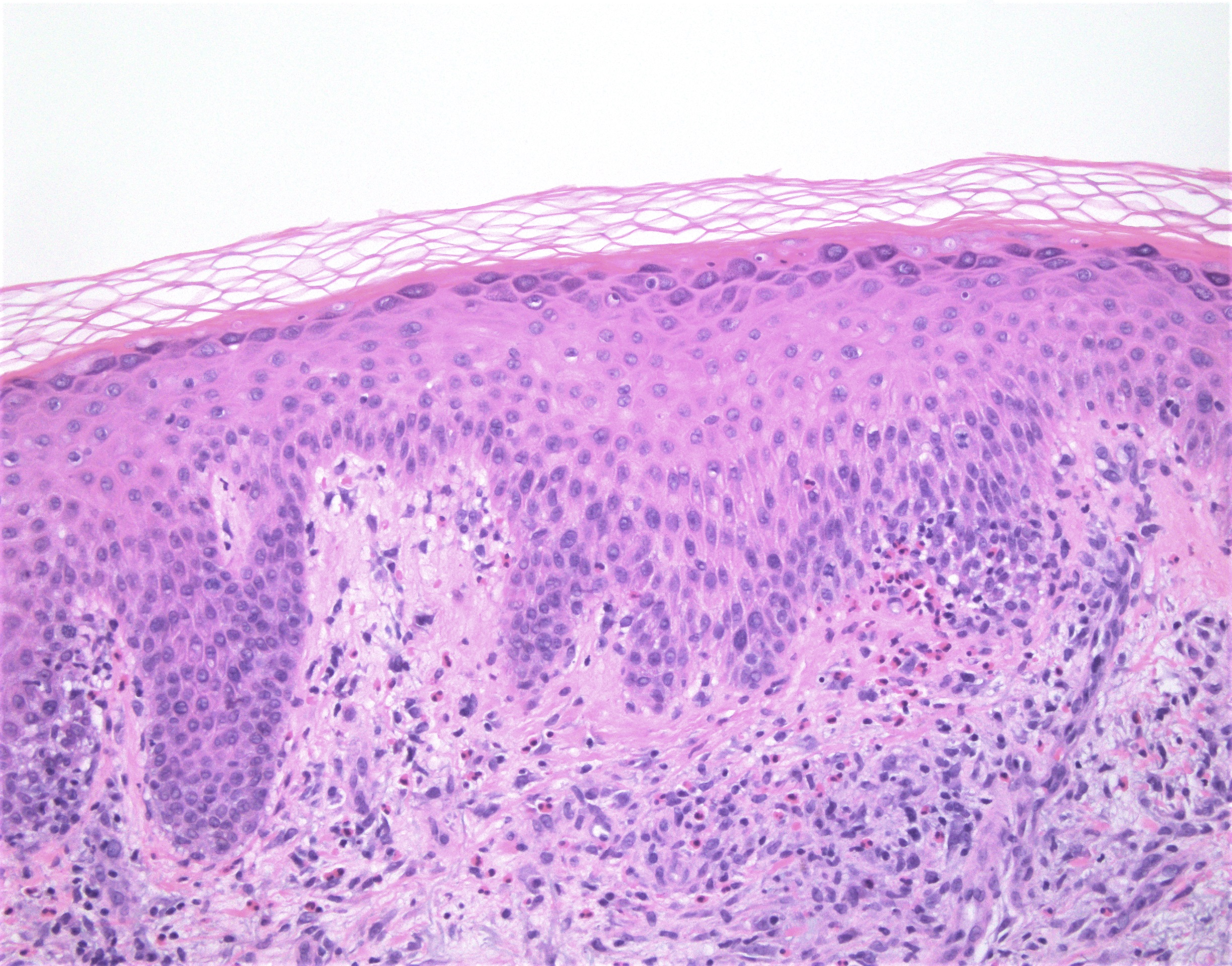
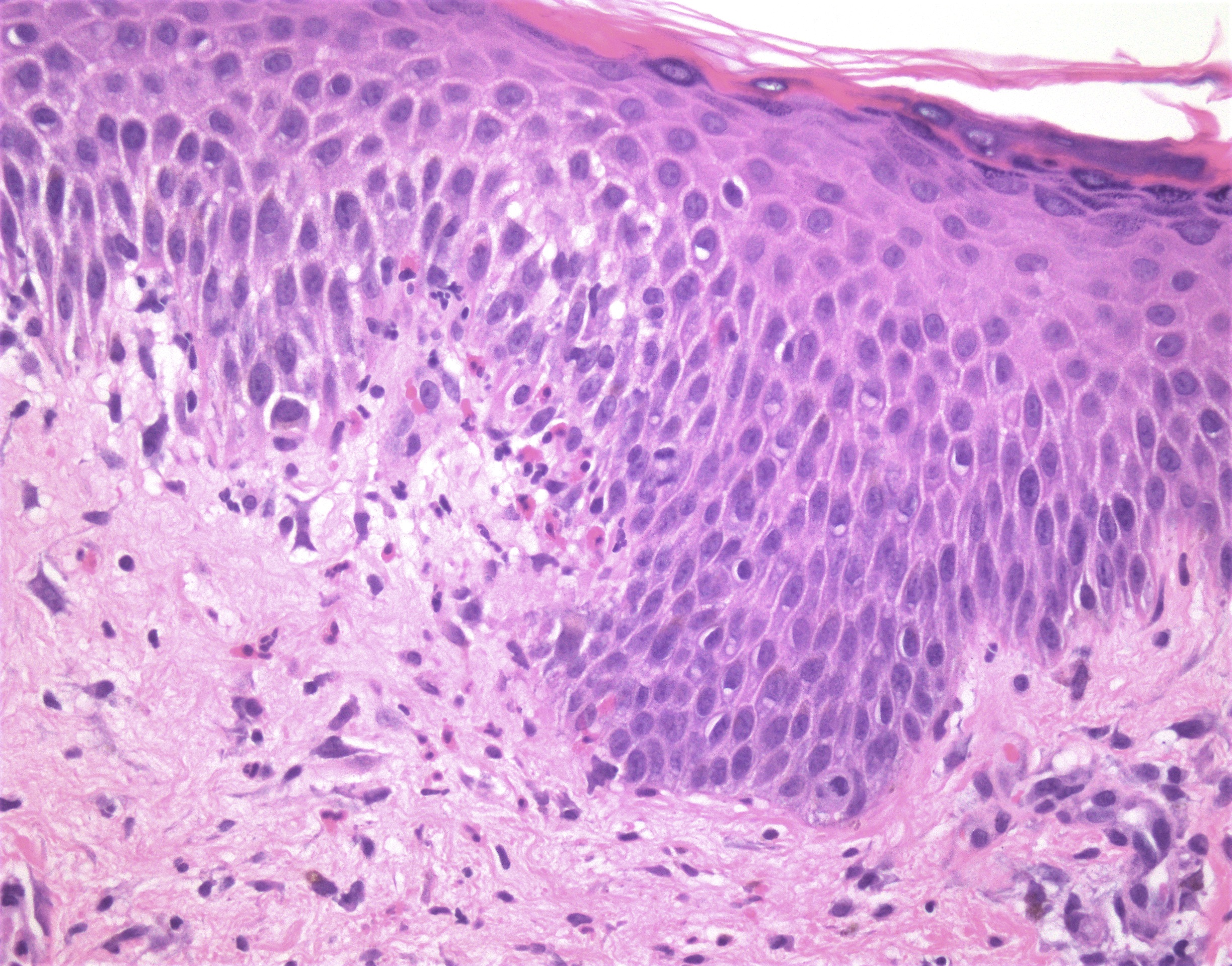
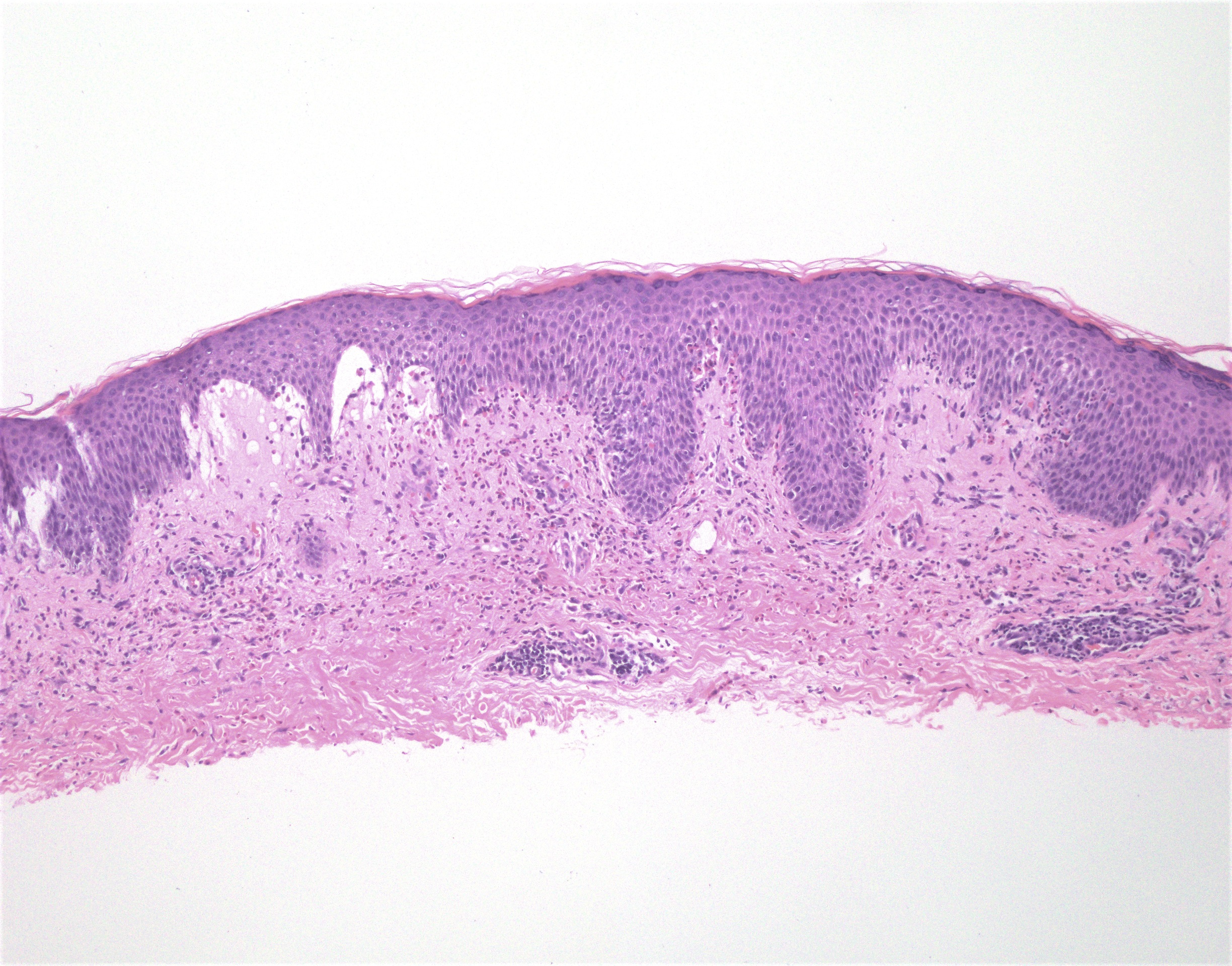
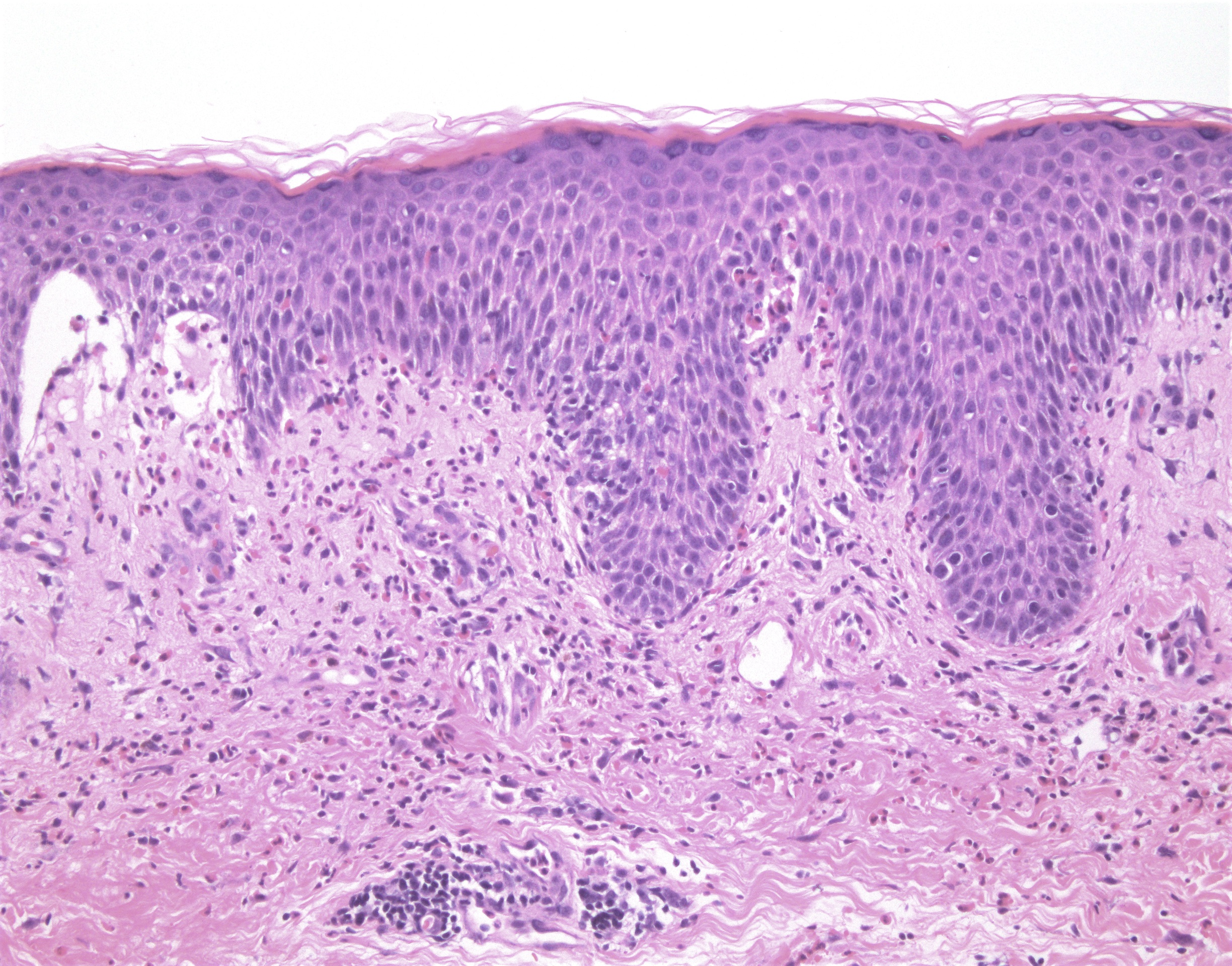
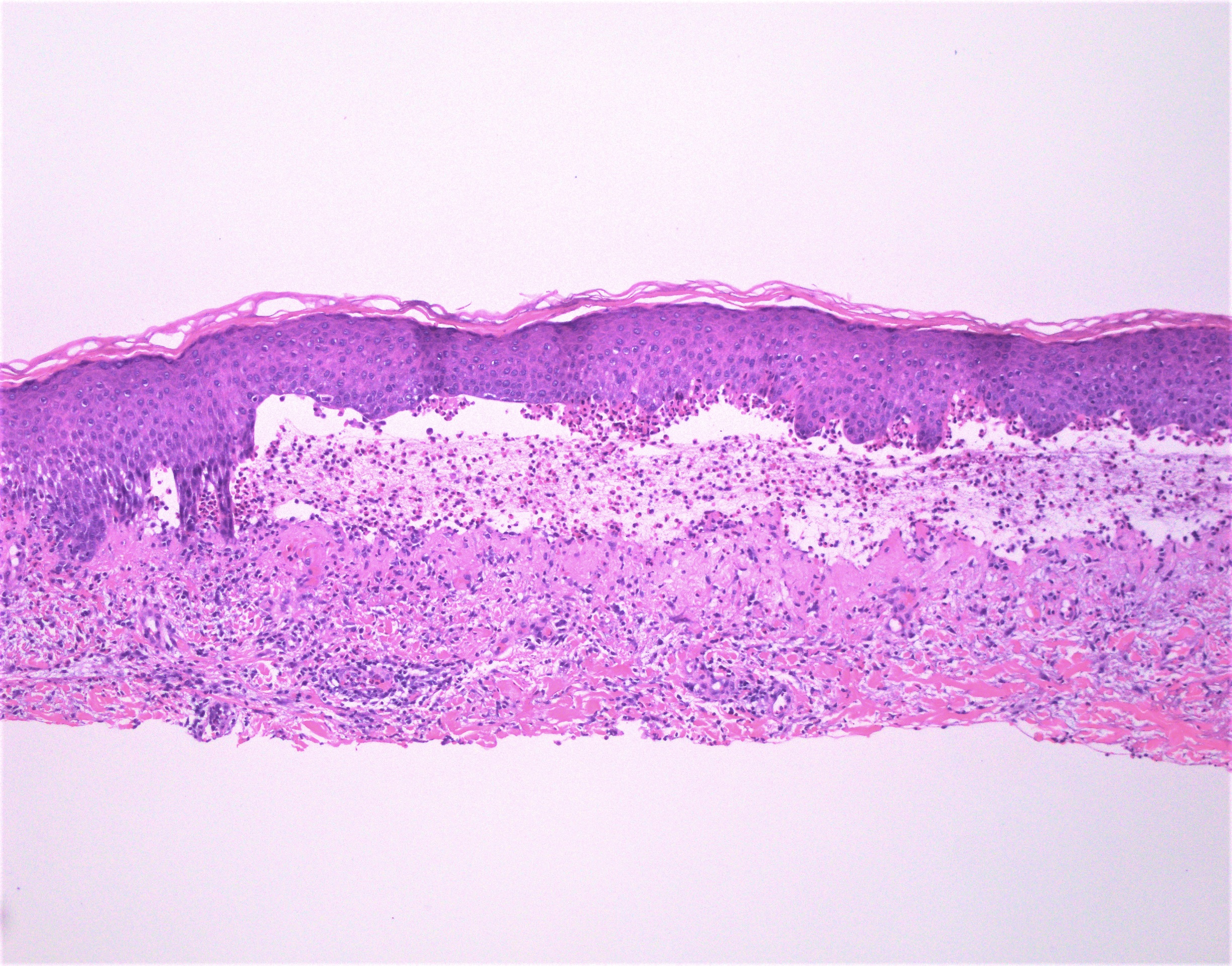
Microscopic (histologic) description
- Subepidermal blister
- Superficial perivascular mixed inflammatory infiltrate with eosinophils in the dermis and blister cavity
- Eosinophils may line up along the dermal epidermal junction and extend into the epidermis (eosinophilic spongiosis) (Am J Clin Dermatol 2017;18:513)
- Urticarial stage:
- Eosinophil rich perivascular and interstitial infiltrate in the papillary dermis
- Eosinophilic spongiosis with pseudovacuolar interface change
- Rare eosinophilic flame figures
- Uncommon presentations include neutrophil rich and cell poor infiltrates
Microscopic (histologic) images
Virtual slides
Positive stains
- Collagen IV immunohistochemistry:
- Can be helpful in differentiating subepidermal blistering disorders with level of split below lamina densa (EBA, antilaminin gamma1/p200 pemphigoid, p105 pemphigoid) from BP and other disorders with split within lamina lucida or above lamina densa
- If split above lamina densa - dermal staining pattern
- If split below lamina densa - epidermal staining pattern
Immunofluorescence description
- Linear C3 > IgG and C3 deposition along the basement membrane zone of epithelium, hair follicles and eccrine glands, n-serrated pattern (Br J Dermatol 2013;169:100)
- Only C3 may be present in early stage lesions
- Salt split skin analysis:
- Direct immunofluoresence: localization of immunoreactants to either roof only (40%) or roof and blister (60%)
- Indirect immunofluorescence: localization of immunoreactants to the roof of the blister (95%)
Immunofluorescence images
Videos
Bullous pemphigoid
Dr. Phillip McKee
Bullous pemphigoid
Dr. Christine Ko
Sample pathology report
- Skin, left medial thigh, shave biopsy:
- Bullous pemphigoid (see comment)
- Comment: There is a subepidermal vesicle beneath which there is a mixed cell infiltrate including eosinophils. The associated specimen submitted for immunofluoresence studies shows linear C3 and IgG in an n-serrated pattern along the basement membrane.
- Skin, left abdomen, shave biopsy:
- Subepidermal blister with eosinophils (see comment)
- Comment: There is a subepidermal vesicle beneath which there is a mixed cell infiltrate including eosinophils. The periphery of the lesion shows areas of eosinophilic spongiosis. The differential diagnosis includes bullous pemphigoid, cicatricial pemphigoid, linear IgA disease, a bullous drug eruption and a severe arthropod bite reaction. Additional material for immunofluorescence studies is recommended.
Differential diagnosis
- Epidermolysis bullosa acquisita:
- Immunofluorescence positive on dermal side of salt split skin (u-serrated pattern) (Br J Dermatol 2004;151:112)
- IgG > C3
- Bullous lupus erythematosus:
- Neutrophil rich infiltrate, variable interface changes
- Dermal mucin deposition
- Eosinophils not present
- DIF: immunoreactive on dermal side of salt split skin (multiple reactants or IgG and C3), u-serrated pattern
- Positive lupus serology
- Positive epidermal nuclear Ig deposition(in vivo ANA) (J Rheumatol 1983;10:733)
- IgG1 is the predominant subclass found (J Dermatol Sci 1990;1:207)
- Dermatitis herpetiformis:
- Papillary neutrophilic microabscesses
- Immunofluorescence = granular IgA in dermal papillae
- May also have fibrillary IgA deposits in the dermal papillae or microgranular deposits along the dermo-epidermal junction (Postepy Dermatol Alergol 2019;36:655)
- Linear IgA bullous disease:
- Neutrophil rich infiltrate
- Immunofluorescence = linear IgA along the basement membrane zone
- Porphyria cutanea tarda:
- Pauci-inflammatory
- Festooning dermal papillae
- Hyalinized superficial blood vessels (positive PAS deposits)
- Caterpillar bodies (positive for PAS and collagen IV)
- Direct immunofluoresence: multiple immunoreactants at the dermo-epidermal junction and within superficial vessels (granular deposition)
Board review style question #1
An 87 year old man presents with erythema and blistering of his chest and upper extremities. Examination shows tense bullae on an erythematous base. A skin biopsy is obtained which reveals subepidermal blister with a mixed inflammatory infiltrate with numerous eosinophils. Which of the following is true for the direct immunofluorescence findings regarding the diagnosis?
- Direct immunofluorescence would show granular IgA deposition at the tips of the dermal papillae
- Direct immunofluorescence would show IgG and C3 reactivity in the epidermis in a fishnet-like pattern in the intercellular squamous region
- Direct immunofluorescence would show linear IgA reactivity along the basement membrane
- Direct immunofluorescence would show linear IgG and C3 reactivity at the basement membrane
Board review style answer #1
D. Direct immunofluorescence would show linear IgG and C3 reactivity at the basement membrane
Comment Here
Reference: Bullous pemphigoid
Comment Here
Reference: Bullous pemphigoid
Board review style question #2
What is / are the antigen(s) targeted in bullous pemphigoid?
- BPAG1 and BPAG2
- Collagen VII
- Desmoglein 1 and Desmoglein 3
- Envoplakin and periplakin
Board review style answer #2