Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Welch J, Ho JD. Central centrifugal cicatricial alopecia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorcentralcentrifugalalopecia.html. Accessed April 25th, 2024.
Definition / general
- Central centrifugal cicatricial alopecia (CCCA) is a lymphocytic scarring alopecia that predominantly affects women of African descent
Essential features
- A form of lymphocytic scarring alopecia primarily affecting females of African descent (StatPearls: Central Centrifugal Cicatricial Alopecia [Accessed 7 December 2022])
- Hair loss starts on the scalp vertex and progresses outward in a centrifugal and symmetric pattern
- Premature desquamation of the inner root sheath may play an important role (Clin Cosmet Investig Dermatol 2016;9:175)
- Clinicopathologic correlation is required for definitive diagnosis as histologic features overlap lichen planopilaris and frontal fibrosing alopecia
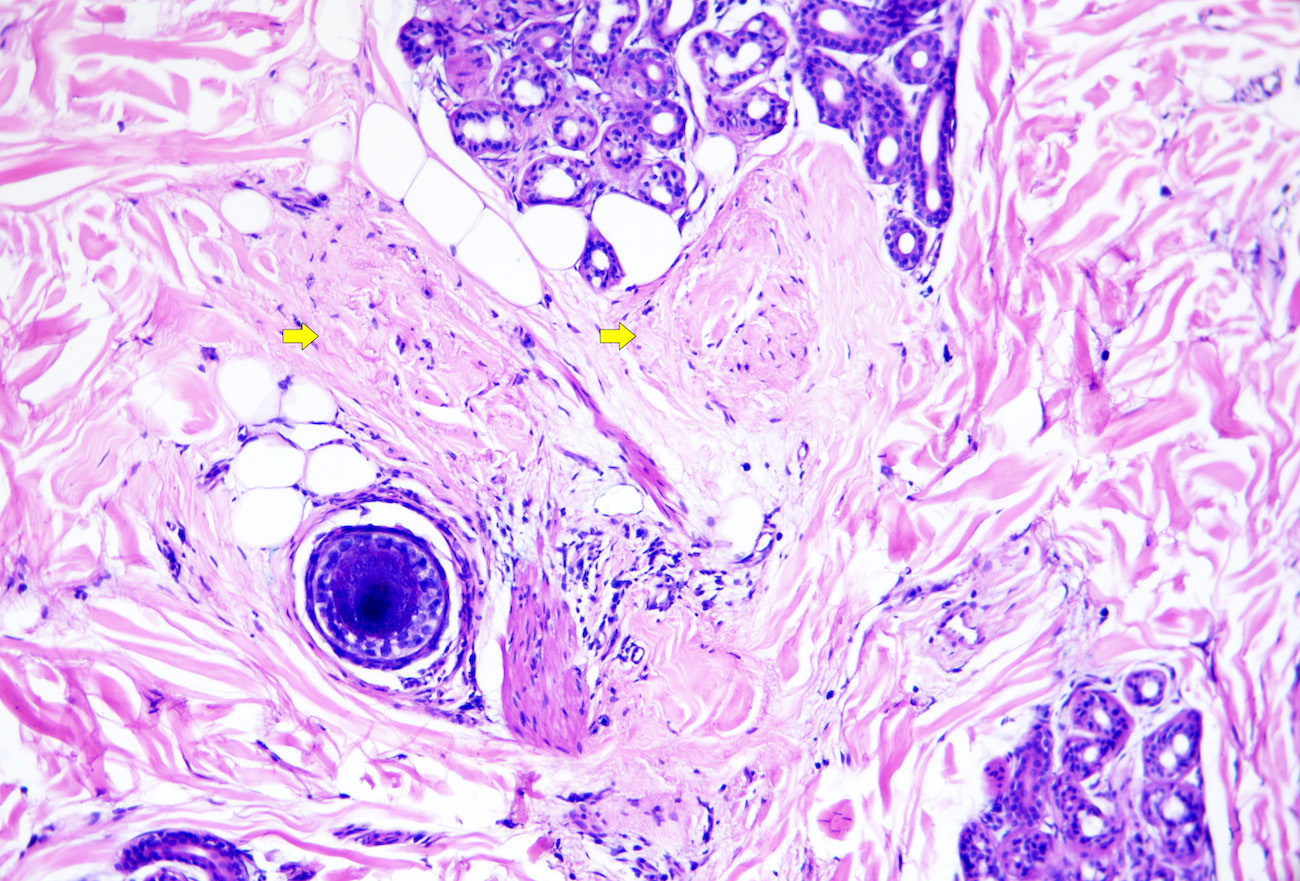
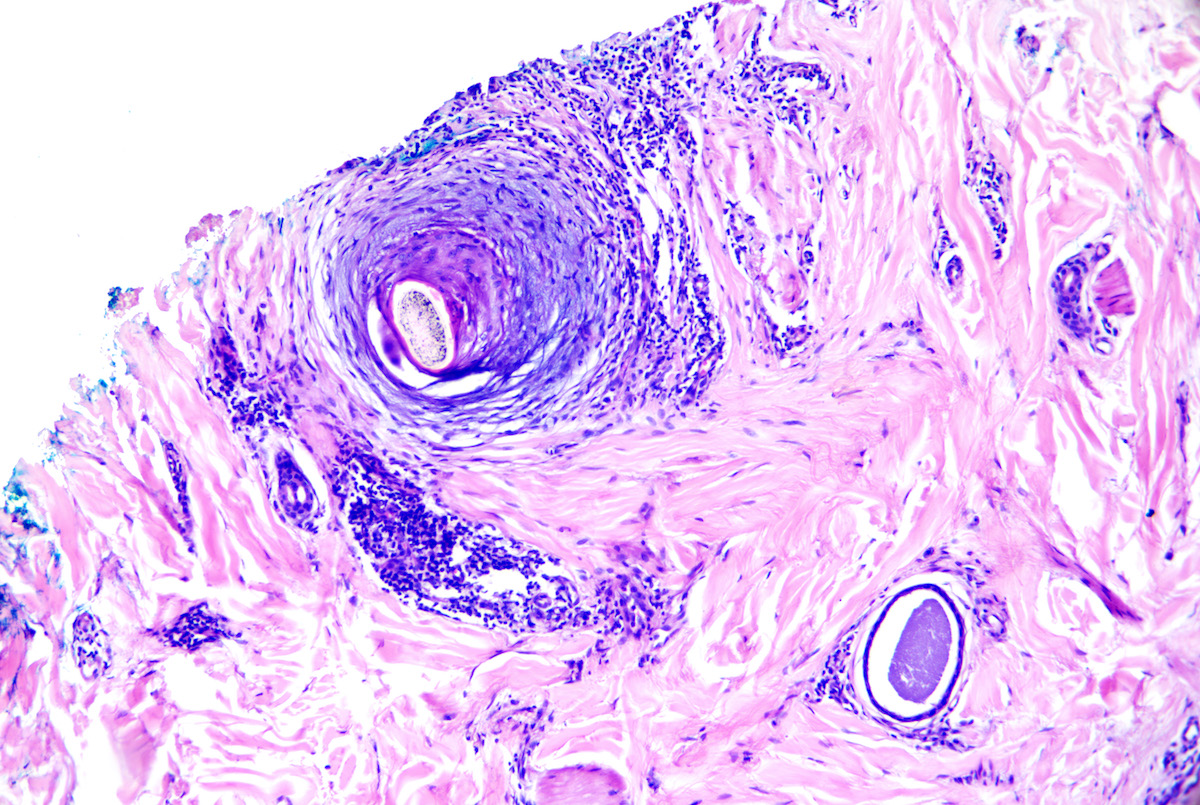
- Microscopic features of active disease include variably dense perifollicular lymphocytic infiltrate, concentric, lamellated perifollicular fibrosis (onion skin-like), premature desquamation of the inner root sheath and asymmetric thinning of follicular epithelium
- Microscopic features of more advanced disease include follicular drop out, fibrous tracts, minimal inflammation, compound follicles and naked hair shafts
Terminology
- Central centrifugal scarring alopecia (CCSA)
- Follicular degeneration syndrome (historical)
- Hot comb alopecia (historical)
ICD coding
Epidemiology
- Middle aged women of African descent (StatPearls: Central Centrifugal Cicatricial Alopecia [Accessed 7 December 2022])
- Prevalence: ~3 - 6% (J Am Acad Dermatol 2016;75:1101, J Am Acad Dermatol 2011;64:245)
- Uncommon in children and men
- Rare familial cases have been described (J Am Acad Dermatol 2014;70:679)
Sites
- Vertex and crown of scalp (Clin Cosmet Investig Dermatol 2016;9:175)
Pathophysiology
- Incompletely understood
- Likely results from a combination of external insults to hair and genetic susceptibility
- Premature desquamation of the inner root sheath is thought to play an important role (StatPearls: Central Centrifugal Cicatricial Alopecia [Accessed 7 December 2022])
- Some families have an autosomal dominant genetic defect in the inner root sheath (J Am Acad Dermatol 2014;70:679)
- Mutations in the PADI3 (peptidyl arginine deiminase type III) gene were recently described in ~30% of a small cohort of women with central centrifugal cicatricial alopecia (n = 16) (N Engl J Med 2019;380:833)
- Follicular destruction occurs as a result of the inflammatory response
- Resultant follicular scarring develops at the site of inflammatory response
Etiology
- Multifactorial
- Controversial but traumatic hair styling (e.g., tight braids, weaves and use of heat or chemical relaxants) may play a role (J Am Acad Dermatol 2016;75:1101, J Investig Dermatol Symp Proc 2017;18:S54)
- Genetic susceptibility as described above
- Potential association with type II diabetes mellitus (Int J Dermatol 2016;55:e338)
Clinical features
- Onset in fourth through sixth decades of life (J Investig Dermatol Symp Proc 2017;18:S54)
- Vast majority of patients are women but men may rarely be affected
- Begins on vertex
- Hair loss progresses outward centrifugally and symmetrically
- Some patients report associated burning, pain and itching
- Hair thinning or breakage at vertex is an early sign of central centrifugal cicatricial alopecia (Arch Dermatol 2012;148:1047)
- Perifollicular hyperpigmentation, follicular papules, scaling, erythema and pustules may be seen (StatPearls: Central Centrifugal Cicatricial Alopecia [Accessed 7 December 2022])
- Variant pattern: presence of scattered alopecia patches (Skin Appendage Disord 2015;1:1)
- Dermatoscopic findings (J Am Acad Dermatol 2014;71:443)
- Peripilar gray-white halo
- Honeycomb pigmented network
- Pinpoint white dots
- Erythema
- White patches
- Individual broken hairs
- Presence of scales
- Asterisk-like brown blotches
- Hair shaft variability
Diagnosis
- History and clinical examination
- Dermoscopy
- Scalp biopsy
- References: Clin Cosmet Investig Dermatol 2016;9:175, Int J Dermatol 2011;50:1457
Prognostic factors
- Dependent on the stage at diagnosis
- Hair regrowth is possible in early inflammatory stage
- Stabilization rather than regrowth is the aim in advanced disease
- References: StatPearls: Central Centrifugal Cicatricial Alopecia [Accessed 7 December 2022], Int J Dermatol 2011;50:1457
Case reports
- 27 year old African American man with thinning to the vertex of scalp for 1.5 years (J Clin Aesthet Dermatol 2012;5:37)
- 49 year old African American woman with pustule on vertex of scalp (JAAD Case Rep 2022;23:67)
- 50 year old woman of African descent with central alopecic patch to vertex (Int J Trichology 2019;11:216)
- 69 year old black woman with hair loss that began in her 50s on vertex of scalp (JAAD Case Rep 2020;6:106)
Treatment
- Topical corticosteroids (StatPearls: Central Centrifugal Cicatricial Alopecia [Accessed 7 December 2022])
- Topical calcineurin inhibitors
- Intralesional steroid injections
- Oral tetracycline antibiotics (e.g., doxycycline)
- Hydroxychloroquine (Clin Cosmet Investig Dermatol 2016;9:175)
- Cyclosporin (J Am Acad Dermatol 2009;60:660)
- Minoxidil
- Topical metformin (JAAD Case Rep 2020;6:106)
Microscopic (histologic) description
- Features are best appreciated on transversely bisected, 4 mm punch biopsies taken from the active edge (fringe) of the process
- Features may be consistent or compatible with central centrifugal cicatricial alopecia but clinicopathologic correlation is essential, as pathologic features overlap with other lymphocytic scarring alopecias
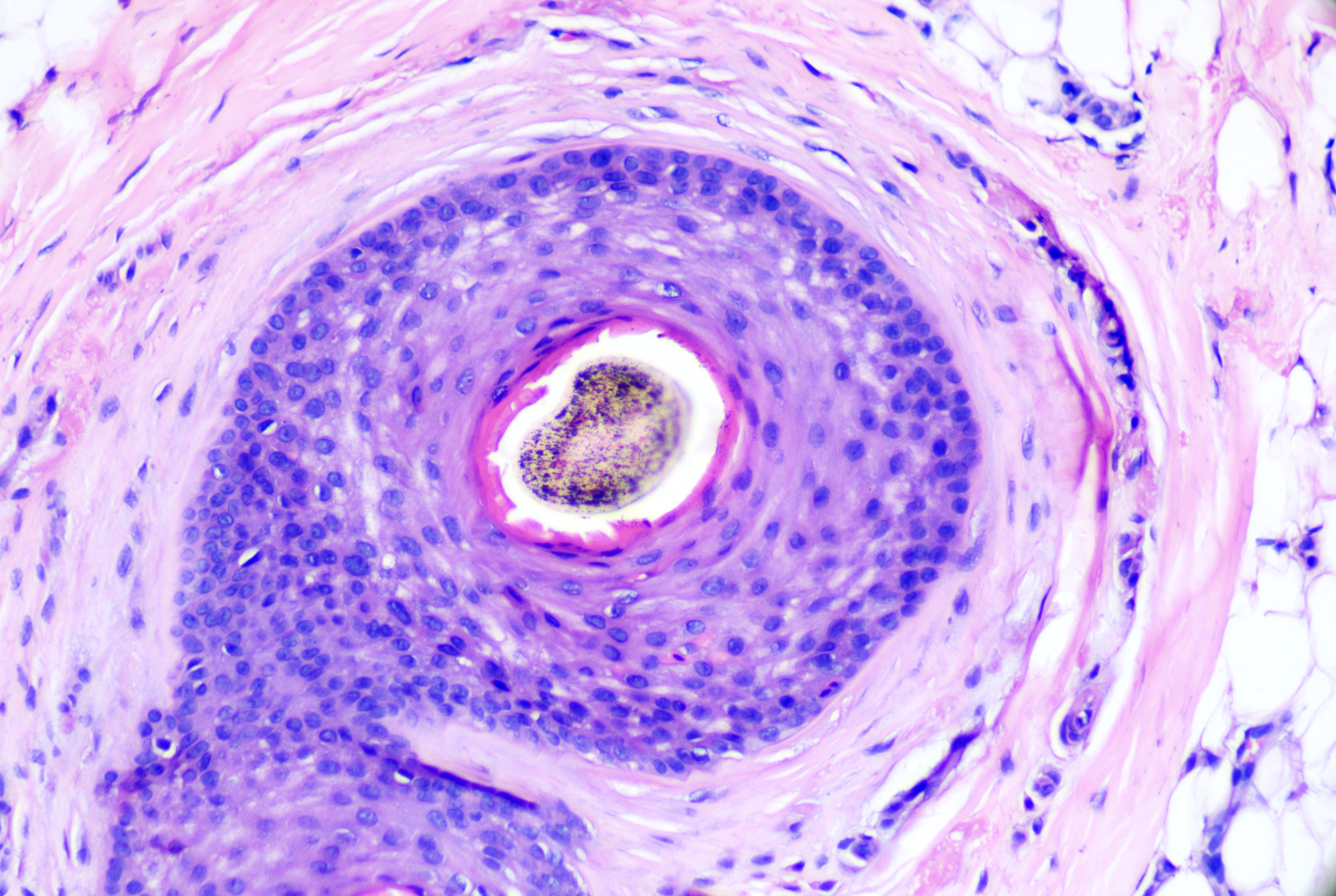
- Premature desquamation of the inner root sheath (IRS) (Clin Cosmet Investig Dermatol 2016;9:175)
- Loss of the inner root sheath below the level of the isthmus
- The level at which sebaceous glands appear indicates the isthmus; thus loss of the inner root sheath in sections prior to their appearance or at the level of the subcutis or eccrine coils indicate premature desquamation (PDIRS)
- May be seen in uninflamed follicles
- Commonly present in but not specific for central centrifugal cicatricial alopecia
- Asymmetric thinning of follicular epithelium
- Follicular density and drop out are inversely proportional to chronicity of alopecia (recall that normal baseline follicular density in persons of African descent may be as low as 21 - 22 hairs/4 mm punch) (Arch Dermatol 1999;135:656)
- No major shift out of anagen
- May exhibit follicular miniaturization (Am J Dermatopathol 2014;36:859)
- Decrease in sebaceous gland number
- Variably dense perifollicular lymphocytic infiltrate affecting the isthmus and lower infundibulum
- Concentric, lamellated, often myxoid perifollicular fibrosis (onion skin-like)
- In cases with progressive fibrosis, lymphocytes may appear to back away from follicle
- Basal layer vacuolation of follicular or interfollicular epithelium is not a feature of central centrifugal cicatricial alopecia
- Marked interfollicular fibrosis is not typical of central centrifugal cicatricial alopecia
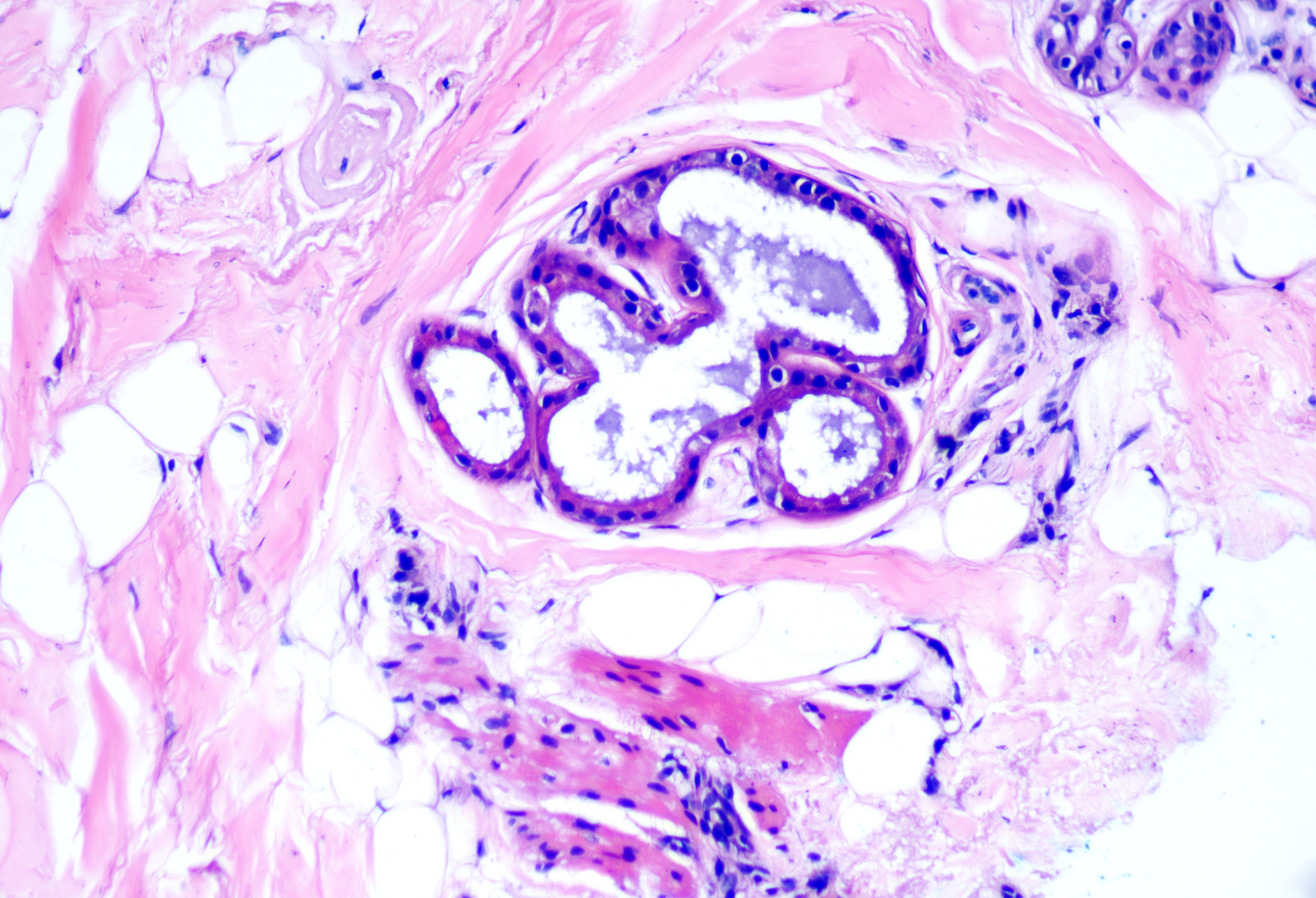
- Follicular destruction may be present with resultant naked hair shafts with or without a foreign body granulomatous reaction (late stage)
- While follicular destruction may result in a more mixed inflammatory cell infiltrate with occasional neutrophils, plasma cells and eosinophils, a heavy mixed inflammatory cell infiltrate should raise the suspicion for folliculitis decalvans
- Compound follicles in groups of 2 - 3 hairs may be seen; compound follicles with ≥ 4 hairs should raise suspicion for a neutrophilic scarring alopecia
- In advanced disease, complete loss / marked reduction in follicular density with follicular dropout and deep fibrous tracts
- Multiple dilated eccrine glands (Am J Dermatopathol 2019;41:871)
- Overlying epidermis is unremarkable
- Features of a second, concomitant alopecia (e.g., traction alopecia) may be present (J Cutan Pathol 2016;43:483)
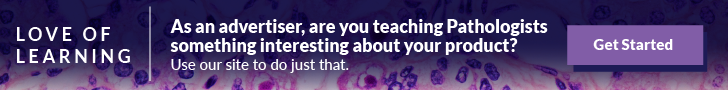
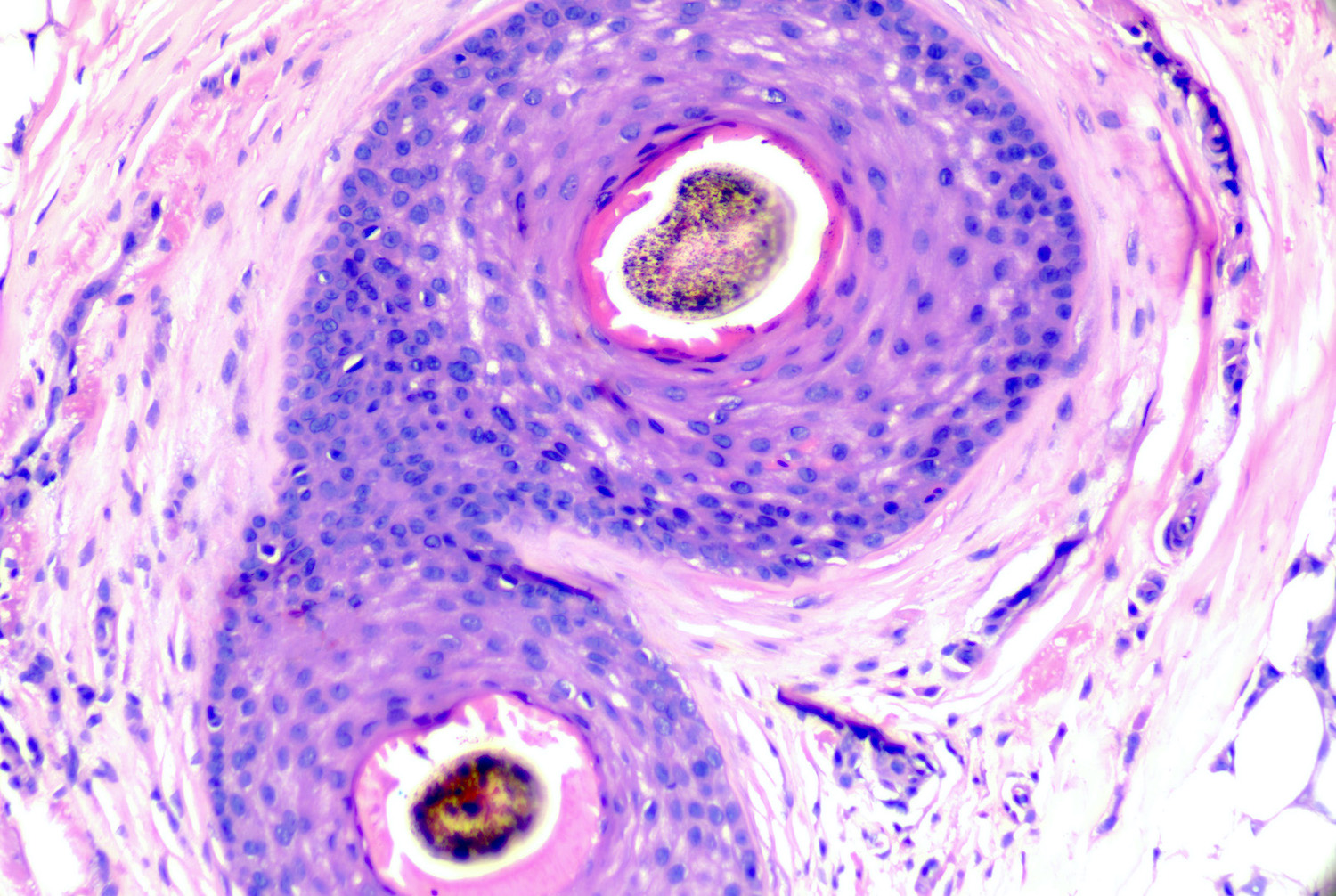
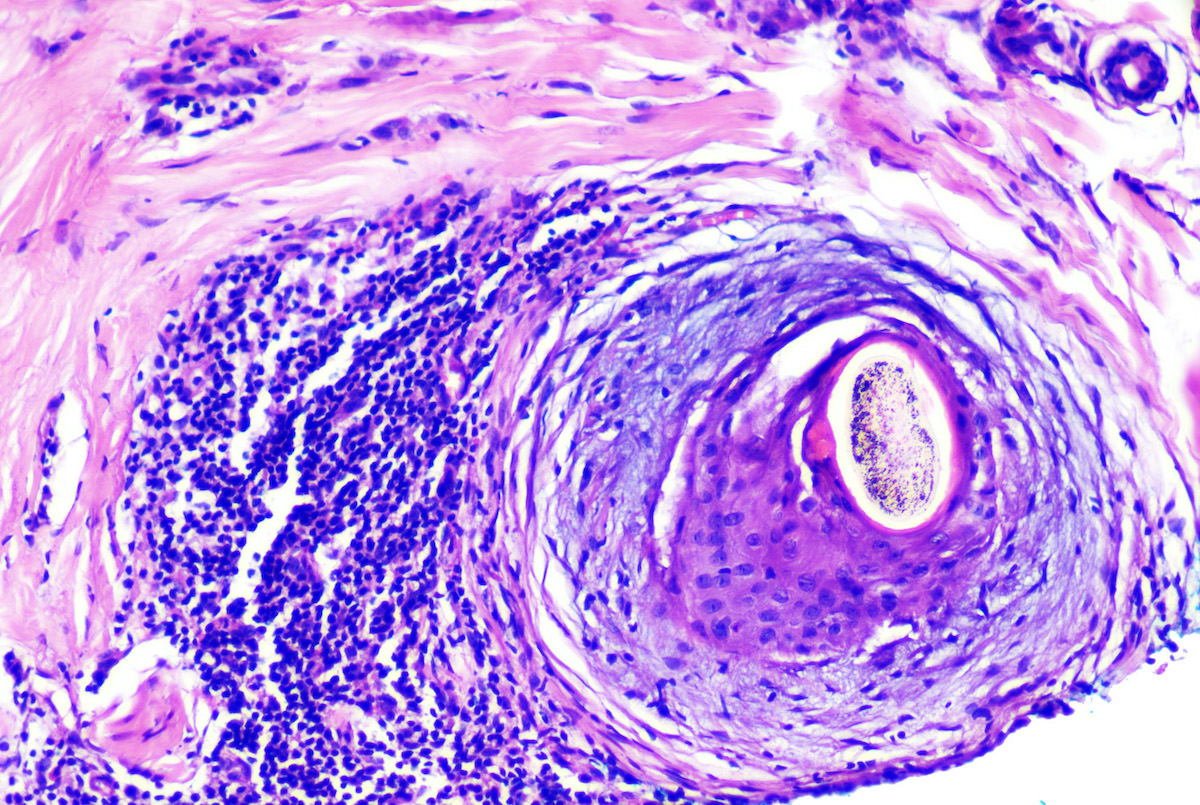
Microscopic (histologic) images
Positive stains
- Verhoeff-van Gieson (VVG) stain reveals tree trunk-like fibrosis if concomitant vertical sections available (Skinmed 2020;18:365)
- PAS stain is useful to exclude tinea capitis; spores in the infundibula or stratum corneum represent Malassezia sp. and are not currently thought to be pathogenic
Sample pathology report
- Skin, scalp, punch biopsy:
- Lymphocytic scarring alopecia consistent with central centrifugal cicatricial alopecia (see comment)
- Comment: Transverse sections reveal 17 hairs, in anagen and terminal in size. Sebaceous glands are reduced in number. There is a mild to moderately dense perifollicular lymphocytic infiltrate at the level of the isthmus and concentric perifollicular fibrosis. Premature desquamation of the inner root sheath, deep fibrous tracts and naked hair shafts are present at deeper levels. Compound follicles in groups of 2 - 3 hairs are identified. The overlying epidermis is unremarkable. PAS stain is negative for fungal elements. It should be noted that lichen planopilaris may exhibit overlapping histopathologic features; however, given the clinical setting (patient of African descent with alopecia at the vertex), central centrifugal cicatricial alopecia is favored.
Differential diagnosis
- Lichen planopilaris (LPP) and frontal fibrosing alopecia (FFA):
- May be impossible to differentiate based on pathologic findings alone (J Cutan Pathol 2020;47:128)
- Significant basal layer vacuolation involving follicular epithelium or interface / lichenoid dermatitis affecting the overlying interfollicular epidermis favor lichen planopilaris / frontal fibrosing alopecia (Int J Dermatol 2006;45:375)
- Narrow wedge shaped fibrosis rather than broad tree trunk fibrosis on vertical sections (VVG stain) favors lichen planopilaris over central centrifugal cicatricial alopecia
- Clinicopathologic correlation required for accurate diagnosis
- Clinical setting is crucial:
- Black patients with vertex predominant alopecia = central centrifugal cicatricial alopecia
- Scattered patches of scarring alopecia in a footprints in the snow / sand appearance = lichen planopilaris
- Scarring alopecia primarily affecting frontal hairline, eyebrows, sideburns with or without limbs = frontal fibrosing alopecia
- Clinical setting is crucial:
- Fibrosing alopecia in a pattern distribution (FAPD):
- Combination of lymphocytic scarring alopecia and pattern hair loss
- Inflammation should primarily affect miniaturized hairs or both miniaturized and terminal hairs
- Interface change involving the follicular epithelium of miniaturized hairs favors fibrosing alopecia in a pattern distribution over other lymphocytic scarring alopecias
- Discoid lupus erythematosus:
- When active, has the densest inflammation of the lymphocytic scarring alopecias
- Typically exhibits dense superficial and deep perivascular, perifollicular and perieccrine lymphocytic infiltrate with or without scattered plasma cells
- Perifollicular fibrosis, miniaturization or total obliteration of follicles may be seen
- Overlying epidermis demonstrates features of interface dermatitis (active or old), often with follicular hyperkeratosis (plugging) and PAS positive thickening of the basement membrane zone
- Direct immunofluorescence demonstrating a positive lupus band test may be useful in distinguishing burnt out discoid lupus erythematosus from other late stage scarring alopecias
Additional references
Board review style question #1
A 56 year old woman of African descent presents with hair loss involving the vertex of the scalp. She has a history of tight hair styles and weaves and complains of an itching sensation. A punch biopsy demonstrates the features shown in the associated photomicrograph. What is the most likely diagnosis?
- Central centrifugal cicatricial alopecia
- Female pattern hair loss
- Frontal fibrosing alopecia
- Lichen planopilaris
- Traction alopecia
Board review style answer #1
A. Central centrifugal cicatricial alopecia. The biopsy demonstrates perifollicular lymphocytes, concentric (onion skin-like) fibrosis, asymmetry of the follicular epithelium and absence of sebaceous glands consistent with a lymphocytic scarring alopecia. While there are overlapping features among this group, in a female patient of African descent with hair loss affecting the vertex, the most likely diagnosis is central centrifugal cicatricial alopecia (CCCA).
Comment Here
Reference: Central centrifugal cicatricial alopecia
Comment Here
Reference: Central centrifugal cicatricial alopecia
Board review style question #2
A 45 year old woman of African descent with alopecia affecting the crown has a biopsy consistent with central centrifugal cicatricial alopecia. The associated photomicrograph is taken at the level of the eccrine coils / subcutis. What finding is shown in the image?
- Asymmetry of follicular epithelium
- Deep fibrous tract
- Dilated eccrine coil
- Onion skin-like perifollicular fibrosis
- Premature desquamation of the inner root sheath
Board review style answer #2
E. Premature desquamation of the inner root sheath. At this deep level (eccrine coils and fat), there should be a well formed inner root sheath but instead the image demonstrates an absence of this structure. While all the answer options are seen in central centrifugal cicatricial alopecia, premature desquamation of the inner root sheath is demonstrated in the photomicrograph.
Comment Here
Reference: Central centrifugal cicatricial alopecia
Comment Here
Reference: Central centrifugal cicatricial alopecia