Table of Contents
Definition / general | Terminology | Granulomatous dermatitis | Infections | Lichenoid dermatitis | Panniculitides | Perivascular dermatitis | Psoriasiform dermatitis | Sclerosing dermatitis | Spongiotic dermatitis | Vasculopathic / vasculitic dermatitis | Vesiculobullous dermatitis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Dehner C, Dehner LP. Common terms & patterns. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorcommonterms.html. Accessed April 16th, 2024.
Definition / general
- This topic represents an overview of common terms and microscopic findings of the most frequently seen reaction pattern in dermatopathology
Terminology
- Acantholysis:
- Separation of cell - cell connections (desmosomes) between keratinocytes leading to single, rounded keratinocytes
- Seen in pemphigus variants and related disorders
- Acanthosis:
- Thickening of epidermis
- Elongated rete ridges usually extend into dermis
- Can be regular (all rete pegs at roughly the same level) or irregular (rete pegs at different levels of the papillary dermis)
- Anagen:
- Hair during growth phase
- Anaplasia:
- Atypical nuclei (abnormal in size and shape) and pleomorphism (variation in nuclear characteristics)
- Asteroid body:
- Collections of eosinophilic material in sporotrichosis or star shaped inclusion in sarcoidal giant cells / other granulomatous processes
- Atrophy:
- Epidermal:
- Decreased thickness due to reduced numbers of keratinocytes
- Epidermis may appear flat at its base with loss of rete ridge pattern
- May occur after inflammation / certain topical treatments
- Dermal:
- Thinning of dermal layer due to loss of collagen / elastin
- May occur after steroids and atrophodermas
- Epidermal:
- Banana bodies:
- Yellow-green, banana shaped fibers in the dermis; can be due to exogenous or endogenous causes
- Basal vacuolar degeneration:
- Also known as liquefactive / hydropic degeneration
- Small vacuoles resembling bubbles in the basal layer
- Often associated with individually necrotic keratinocytes
- May or may not have an associated band of infiltrate obscuring the dermoepidermal junction
- Associated with vacuolar / lichenoid interface dermatitis (e.g., cutaneous lupus, erythema multiforme, lichen planus)
- Basement membrane:
- Thin membranous layer of extracellular matrix which is separating the epidermis from the dermis
- Birefringence:
- Optical capacity of a material with a refractive index that depends on polarization and propagation of direction of light
- Blister:
- Fluid filled skin lesions
- May result from separation of keratinocytes (intraepidermal blisters) or loss of adhesion between the epidermis and the underlying dermis (subepidermal blisters)
- Examples of diseases commonly associated with blisters include autoimmune bullous dermatoses, interface dermatitis, spongiotic dermatitis and some viral and bacterial infections
- Bullae:
- Fluid filled lesion > 1 cm (= large blister)
- Calcinosis:
- Cutaneous deposition of insoluble calcium in response to damage, metabolic derangements or undetermined etiology
- Catagen:
- Hair during regressive phase
- Caterpillar bodies:
- Eosinophilic bodies present within the roof of the blister formed in porphyric bullous eruptions, such as porphyria cutanea tarda
- Civatte / colloid bodies:
- Globular residue of apoptotic keratinocytes
- Typically pink in color
- Referred to as Civatte bodies when present within the epidermis and as colloid bodies when in the papillary dermis
- Classically described in lichen planus but may be seen in all causes of interface / lichenoid dermatitis
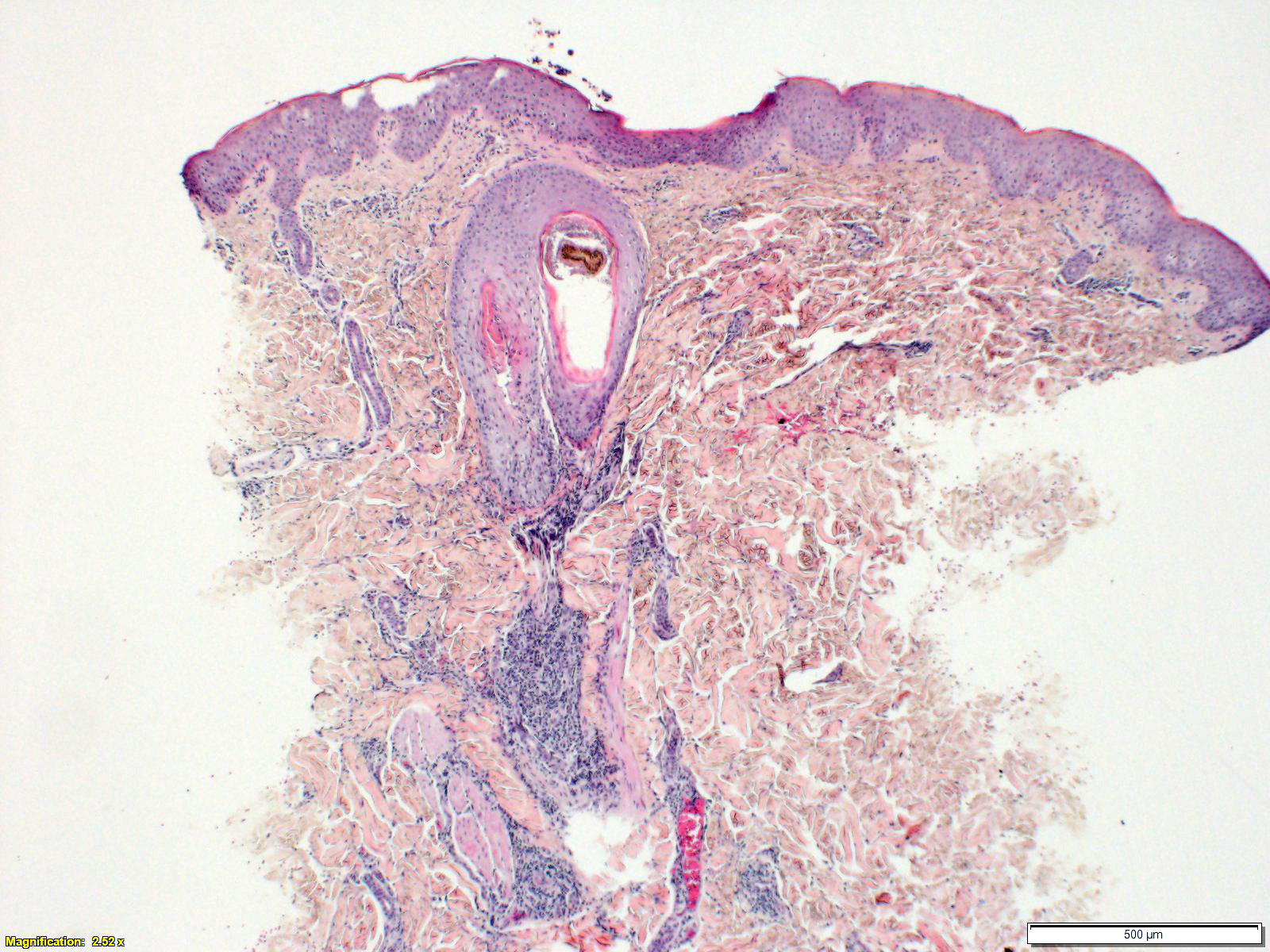
- Comedo:
- Dilated follicular infundibulum filled with keratin, lipid (not visible with standard stains) and often basophilic debris
- Bacterial colonies may be present
- Classical lesion in acne vulgaris
- Cornoid lamellae:
- Layers of parakeratosis often in a ~45° angle overlying an area of diminished granular layer with dyskeratotic cells present at the base
- Classically seen in porokeratosis variants
- Cowdry bodies:
- Cowdry A: intranuclear inclusion in herpes simplex virus
- Cowdry B: intranuclear inclusion in cytomegalovirus, adenovirus, poliovirus
- Crust:
- Hyperkeratosis (often parakeratosis) with inspissated serum with or without Inflammatory cells (= wet scale)
- Cyst:
- Encapsulated cavity or sac lined by true epithelium
- DEJ:
- Dermoepidermal junction
- Dermal papilla (hair):
- Layer that is located at the base of the hair follicle
- Desmosome:
- Adhesion molecule between two cells
- Diffuse infiltrate:
- sheets of inflammatory ells diffusely infiltrating dermis
- Donovan body:
- Rod shaped, oval organisms within histiocytes in granuloma inguinale
- Characteristic bipolar staining pattern gives safety pin appearance
- Highlighted by Warthin-Starry and Giemsa stains
- Dutcher body:
- Spherical, intracytoplasmic immunoglobulin inclusions that appear intranuclear due to folding into the nucleus of plasma cells
- Seen in plasmacytoma
- Dyskeratosis:
- Abnormal, premature keratinization of keratinocytes below granular cell layer
- Often have brightly eosinophilic cytoplasm with or without a pyknotic nucleus
- Effacement:
- Synonymous with consumption of the epidermis
- Refers to thinning of the epidermis / loss of rete ridges
- Commonly seen in melanoma
- Elastolysis:
- Defect in elastic fibers leading to atrophy, skin laxity
- Elastorrhexis:
- Fragmentation of elastic fibers; systematic elastorrhexis seen in pseudoxanthoma elasticum
- Elastosis:
- Degenerative changes in elastic fibers (increase in abnormal elastin) leading to loss of elastic quality of the dermis
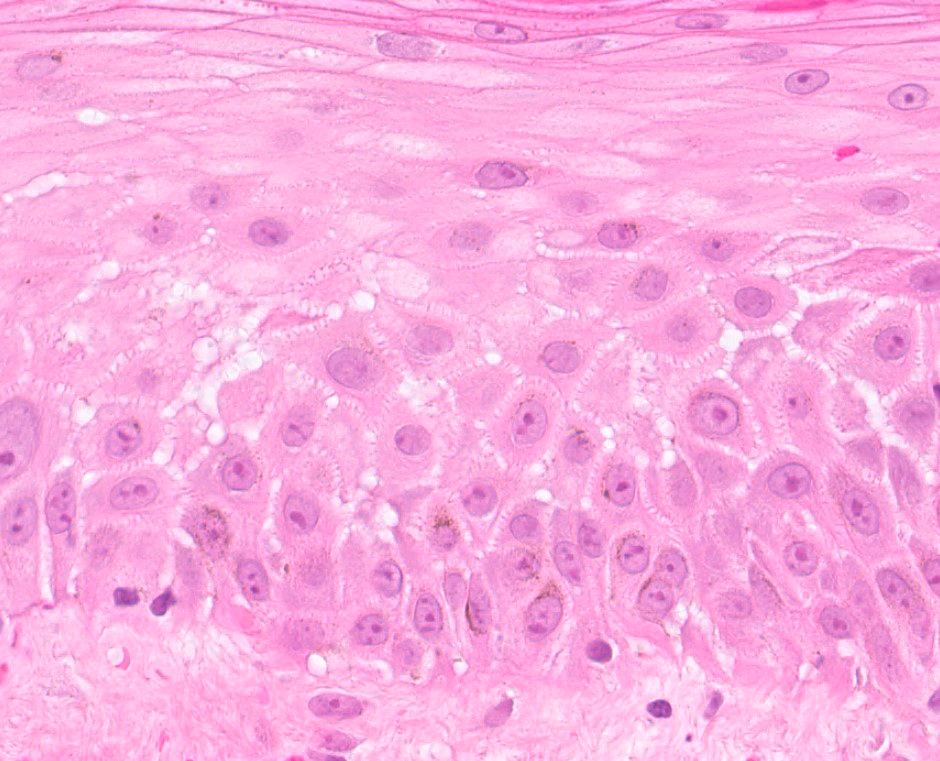
- Epidermolysis:
- Alteration of granular layer with perinuclear clear spaces, swollen and irregular keratohyalin granules, increased thickness of granular layer
- Different from acantholysis
- Classically seen in epidermolytic ichthyosis and keratodermas but may be seen in epidermal nevi, isolated keratoses and incidentally
- Epidermotropism:
- Atypical individual cells present in epidermis without significant spongiosis
- Most commonly refers to atypical lymphocytes in cutaneous T cell lymphomas but can be seen in other malignant neoplasms, including melanoma and metastatic deposits
- Erosion:
- Discontinuity of skin causing partial loss of epidermis
- Excoriation:
- Deep scratch with abrupt loss of epidermis without full thickness loss at an ulcer
- Excoriation may result in partial or full thickness epidermal loss (erosion versus ulcer)
- Often self induced
- Exocytosis:
- Inflammatory cells migrating into the epidermis (commonly seen in spongiotic dermatitis)
- Lymphocytes, neutrophils and eosinophils most commonly seen
- Festooning:
- Undulating pattern of the dermal papillae
- Commonly seen underneath bullae / blisters (e.g. in porphyria cutanea tarda / subepidermal autoimmune bullous diseases)
- Fibrinoid necrosis:
- Necrosis associated with vascular damage
- Fibrosis:
- Increased amount of fibroblasts forming a scar or skin thickening
- Flame figure:
- Deposition of eosinophil granules from degranulated eosinophils and nuclear debris on dermal collagen fibers with or without surrounding histiocytes
- Classically seen in Wells syndrome (eosinophilic cellulitis) but may be seen in a variety of eosinophil rich diseases
- Foam cell:
- Histiocyte whose cytoplasm is replaced by variably sized lipid vacuoles
- Commonly seen in xanthoma variants, lipidized dermatofibromas and some histiocytoses
- Follicular plugging:
- Process of abundant hyperkeratotic material plugging up follicular ostia
- Globi:
- Amphophilic collection of mycobacteria, classically seen in leprosy
- Granuloma:
- Collection of macrophages forming a cluster / round structure in response to certain types of inflammation (foreign material, microorganisms, etc.)
- Grenz zone:
- Thin layer of uninvolved dermis directly beneath the epidermis, separating it from an inflammatory cell infiltrate or tumor
- Grenz zones classically seen in granuloma faciale, leukemia cutis, dermatofibromas, lepromatous leprosy and solar elastosis
- Hemidesmosome:
- Adhesion molecule between cell and basal lamina
- Henderson-Patterson body:
- Cytoplasmic viral inclusion bodies often filling cup shaped cavity space in molluscum contagiosum (molluscum bodies)
- Horn (cutaneous horn):
- Massive vertically oriented hyperkeratosis (parakeratotic, orthokeratotic or mixed) most commonly overlying a keratinocytic neoplasm
- Importance lies with the lesion which underlies the horn which may be malignant in a significant minority
- Horn cyst:
- Hyperkeratotic epithelial structure presumably due to abrupt complete keratinization
- Hypergranulosis:
- Thickening of the stratum corneum
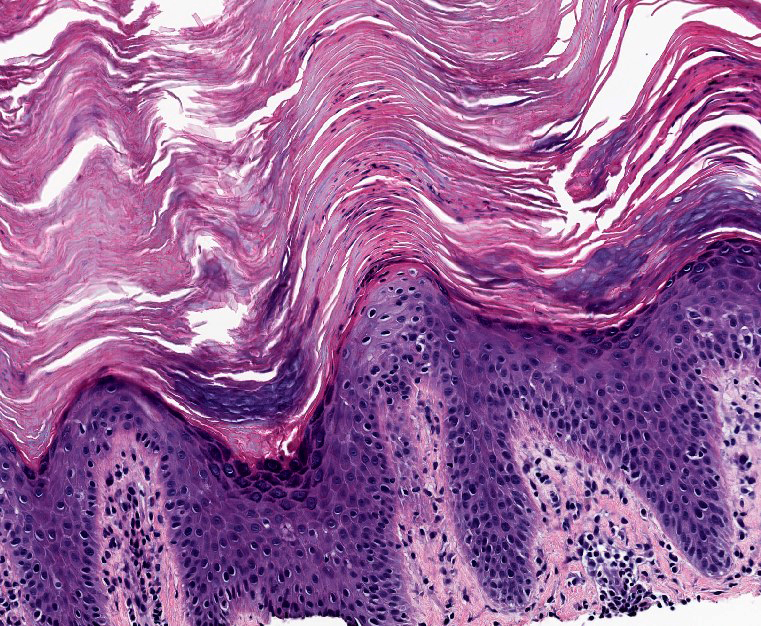
- Hyperkeratosis:
- Thickened cornified layer (stratum corneum)
- Keratin may be abnormal
- Either orthokeratotic (typically compact keratin with no nuclei) or parakeratotic (nuclei in cornified layer)
- Inferior follicle:
- Inferior segment of the follicle from the bulge to the base of the follicle
- Infundibulum:
- Upper segment of the hair follicle
- Interface dermatitis:
- Pattern of inflammatory dermatitis characterized by basal layer vacuolation with or without a band of inflammation obscuring the dermoepidermal junction
- When band-like lymphocytic infitlrate present, referred to as lichenoid interface or lichenoid dermatitis
- Isthmus:
- Segment between the sebaceous gland duct opening and the hair bulge
- Kamino bodies:
- Eosinophilic bodies associated with spitz nevi
- Koilocyte:
- Keratinocyte that underwent structural changes due to viral infection
- Lentiginous:
- Linear pattern of melanocytic proliferation within epidermal basal cell layer
- Leukocytoclasis:
- Vascular karyorrhexis of degenerating neutrophils is a feature of neutrophilic vasculitis (also called leukocytoclastic vasculitis)
- Leukocytoclastic vasculitis:
- Inflammatory reaction of blood vessels including fibrinoid changes within the vessel walls
- Lichenification:
- Thick, rough skin with prominent skin markings usually due to repeated rubbing
- Associated with hyperkeratosis
- Lichenoid dermatitis:
- Inflammatory pattern characterized by basal vacuolar change and a band of inflammatory cells at the dermo - epidermal junction
- Lichenoid infiltrate:
- Band-like lymphocytic infiltrate at the dermoepidermal junction
- Macule:
- Flat lesion less than 1.0 cm
- Medlar body:
- Also known as sclerotic bodies
- Brown, round fungal cell in between yeast and hyphal state with the appearance of copper pennies
- Diagnostic for chromoblastomycosis
- Michaelis-Gutmann body:
- Round, calcified structures located within the cytoplasm of histiocytes in malakoplakia
- Stain with Perls stain for iron and von Kossa for calcium
- Mikulicz cells:
- Large foamy histiocytes containing rods of klebsiella rhinosclermomatis in rhinoscleroma
- Munro microabscess:
- Neutrophilic collections in the stratum corneum
- Classically seen in psoriasis
- Necrobiosis:
- Altered / necrotic collagen
- Seen in granuloma annulare and other necrobiotic lesions
- Nevus:
- Often used to refer to a benign tumor of melanocytes but may also refer to a hamartomatous lesion of any component of the skin (epidermis, dermis, blood vessels etc.)
- Nodular inflammation:
- Inflammatory cells forming nodular collections
- Nodule:
- Solid lesion (> 1 cm) whose vertical dimension is greater than its horizontal
- Oncholysis:
- Separation of the nail plate from the underlying nail bed
- Associated with psoriasis, trauma, onychomycosis, thyrotoxicosis and phototoxic drug ingestion
- Owl eye inclusion:
- Term used to describe a cells infected by cytomegalovirus
- Pagetoid spread:
- Single malignant cells involving the epidermis
- Panniculitis:
- Lobular:
- Inflammation of fat involving predominantly the fat lobules (e.g., erythema induratum, pancreatic panniculitis, etc.)
- Septal:
- Inflammation of fat involving predominantly the septae in between the fat lobules (e.g., erythema nodosum)
- Lobular:
- Papillary dermal edema:
- Extracellular accumulation of fluid leading to thinning of the dermis
- Papillary mesenchymal body:
- Structures associated with follicular differentiation; can serve as helpful clue in follicular type adnexal neoplasms, such as trichoepithelioma / trichoblastoma
- Papillomatosis:
- Finger-like undulation of the epidermis with upward expansion of dermal papillae
- May have associated epidermal hyperplasia
- Papule:
- Raised lesion < 1 cm
- Parakeratosis:
- Retention of nuclei in the stratum corneum
- Normal for mucous membranes without stratum granulosum
- Parasitized macrophages:
- Macrophages infected by parasites present within their cytoplasm (e.g., in leishmaniasis)
- Patch:
- Flat lesion > 1 cm
- Pautrier microabscess:
- Collections of atypial lymphocytes involving the epidermis; seen in mycosis fungoides
- Periadnexal inflammation:
- inflammatory cells predominantly surrounding the adnexal structures
- Perivascular inflammation:
- Inflammatory cells predominantly surrounding vasculature
- Plaque:
- Raised, relatively flat topped lesion > 1 cm
- Poikiloderma:
- Combination of atrophy, telangiectasia and pigmentary changes
- Pseudoepitheliomatous hyperplasia:
- Exaggerated acanthosis of the epidermis mimicking squamous cell carcinoma
- Commonly seen in the epidermis overlying prior procedure sites, chronic inflammation, granular cell tumor, blastomycosis
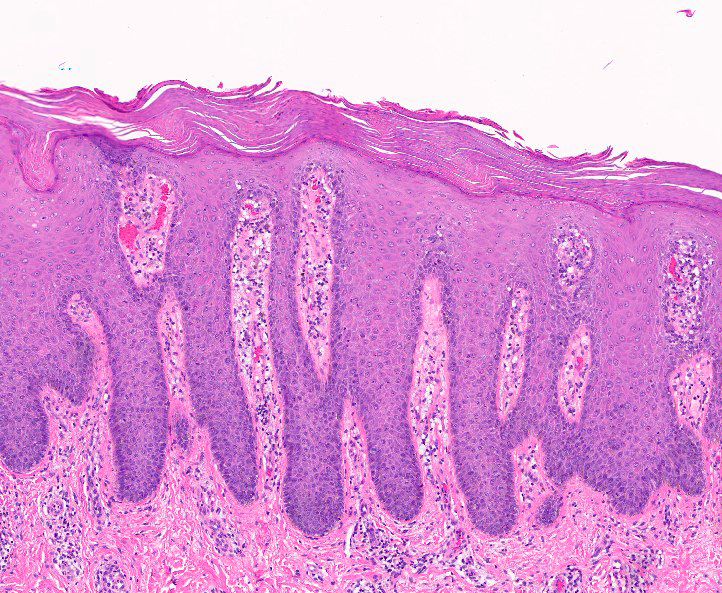
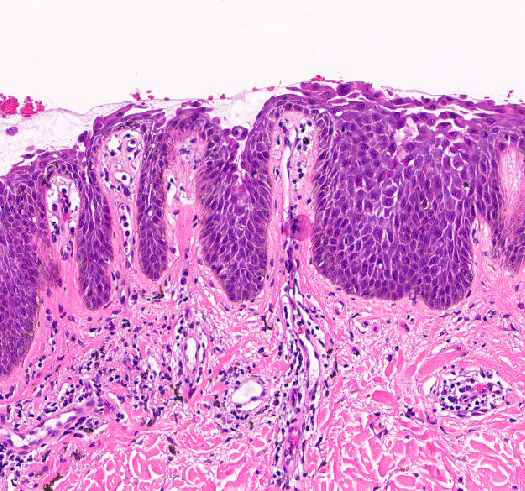
- Psoriasiform epidermal hyperplasia:
- Acanthosis of the epidermis with regular elongation the rete ridges
- Purpura:
- Extravasation of red blood cells into the skin or mucous membranes with or without inflammation
- Pustule:
- Intraepidermal or subepidermal vesicle or bullae filled with neutrophils
- Scale:
- Dry, horny, plate-like excrescence corresponding to hyperkeratosis
- Usually due to imperfect cornification
- Schaumann body:
- Laminated calcified structure
- Seen in sarcoidosis but rare in skin lesions
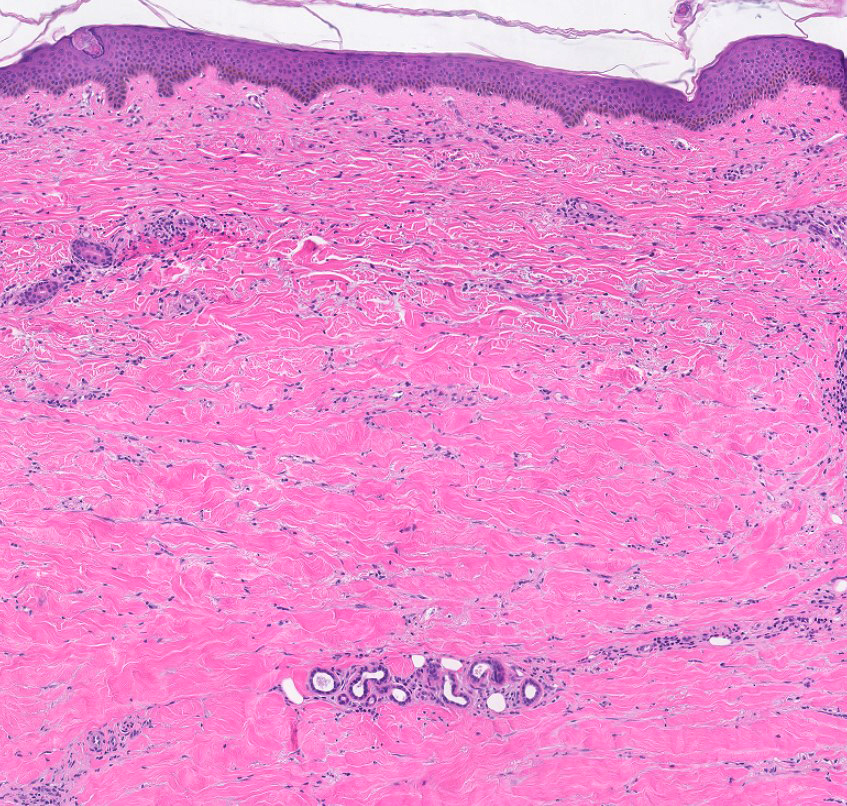
- Sclerosis:
- Excess connective tissue with decreased amount of fibroblasts
- Shadow cells:
- Cells without a nucleus due to prior cell death
- Sinus:
- Tract connecting cavities to each other or to the surface
- Spongiform pustule of Kogoj:
- Collection of neutrophils within the stratum spinosum
- Associated with spongiosis at the periphery (e.g. seen in psoriasis)
- Seen in psoriasis, including pustular variants
- Spongiosis:
- Intraepidermal edema causing splaying apart of keratinocytes in stratum spinosum (resembling a sponge)
- Intercellular adhesion proteins (desmosomes) often visible
- Vesicles due to shearing of desmosomes
- Squamous eddies:
- Whorled profiles composed of keratinocytes (e.g. seen in inverted follicular keratoses)
- Storiform:
- Growth pattern consisting of spindle cells arranged in a cartwheel-like pattern
- Classically seen in dermatofibrosarcoma protuberans (DFSP)
- Telogen:
- Hair during resting phase
- Ulceration:
- Discontinuity of skin causing complete loss of epidermis and possible loss of dermis with accompanying surface fibrin deposition or exudate with or without granulation tissue response
- Verocay body:
- Structure composed of 2 nuclear palisades with central eosinophilic cytoplasmic processes
- Classically seen in schwannoma
- Vesicle:
- Fluid filled lesion < 1 cm
- Von Hansemann cells:
- Large macrophages containing Michaelis-Gutmann bodies seen in malakoplakia
- Wheal:
- Itchy, transient, elevated area with variable blanching and erythema
- Due to dermal edema
Granulomatous dermatitis
- Similar pattern seen in various clinical settings
- Sarcoidosis
- Necrobiosis lipoidica (associated with diabetes mellitus)
- Granuloma annulare (localized, generalized, etc.)
- Palisaded neutrophilic and granulomatous dermatitis
- Granulomatous reaction to foreign material
Contributed by Carina Dehner, M.D., Ph.D.
Infections
- Bacterial
- Impetigo:
- Nonbullous or bullous forms
- Gram positive cocci are the trigger
- Staphylococcus scalded skin syndrome:
- Sterile subcorneal split of epidermis
- Driven by toxins from certain Staphylococcus aureus strains
- Rhinoscleroma:
- Diffuse inflammatory infiltrate underlying submucosa, Mikulicz cells present
- Trigger: Klebsiella pneumoniae
- Erythrasma:
- Erythematous intertriginous patches
- Triggered by Corynebacterium minutissimum infection
- Impetigo:
- Viral
- Herpes virus:
- Multinucleated keratinocytes with chromatin margination and molding
- Mucosal sites (HSV1 / 2) or dermatome distribution (varicella zoster virus)
- Epstein-Barr virus (EBV):
- Infectious mononucleosis, oral hairy leukoplakia, Gianotti-Crosti syndrome
- EBV virus can be detected by in situ hybridization
- Cytomegalovirus:
- Large, intranuclear inclusions with halo
- Molluscum contagiosum:
- Molluscum bodies
- Trigger: poxvirus
- Herpes virus:
- Spirochetes
- Syphilis:
- Psoriasiform hyperplasia, mixed pattern dermatitis
- Treponema pallidum
- Syphilis:
- Fungal
- Dermatophytosis:
- Neutrophils in stratum corneum sandwich sign: parakeratosis or compact orthokeratosis underlying basket weave type stratum corneum
- Majocchi granuloma:
- T. rubrum
- Fungi surrounding degenerate hair shafts
- Pityriasis (tinea) versicolor:
- Malassezia
- Need to see spores and hyphae in stratum corneum
- Blastomycosis:
- May induce pseudoepitheliomatous hyperplasia
- Dermatophytosis:
- Arthropods / parasites
- Demodex:
- Commonly seen, mostly incidental
- If exuberant, can induce pathologic changes leading to dry eye, chalazion, etc.
- Scabies:
- Potassium hydroxide preparation (KOH prep) can be done on bed site
- Itchy for years
- Demodex:
Contributed by Carina Dehner, M.D., Ph.D.
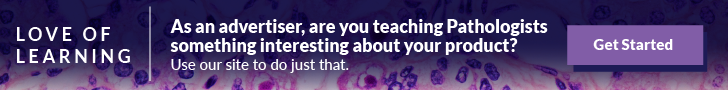
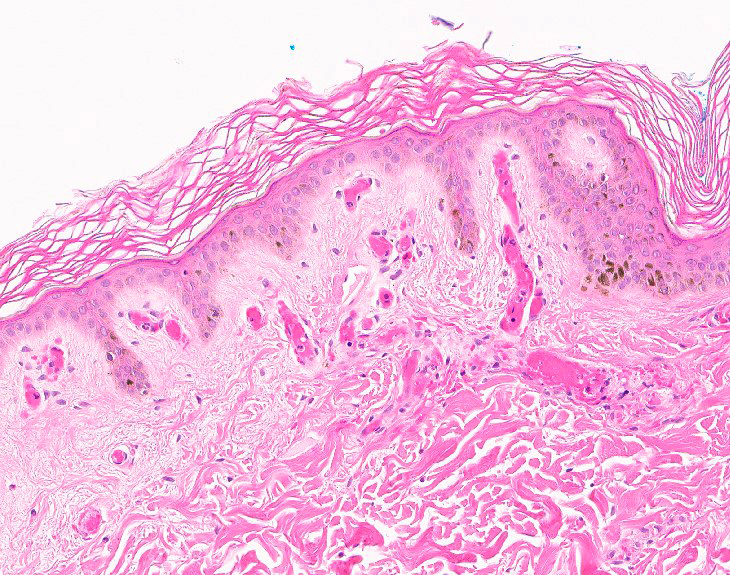
Lichenoid dermatitis
- Lichenoid dermatitis, with or without interface
- Band-like inflammation and basal vacuolar degeneration (lichen planus, etc.)
- Interface changes without lichenoid inflammation (discoid lupus, erythema multiforme)
- Basal vacuolar degeneration and dyskeratotic keratinocytes only (erythema multiforme)
- Basal vacuolar degeneration and dyskeratotic keratinocytes at the dermoepidermal junction + superficial and deep perivascular, periadnexal inflammation and increased dermal mucin (discoid lupus erythematosus)
Contributed by Carina Dehner, M.D., Ph.D.
Panniculitides
- Septal panniculitis
- Erythema nodosum
- Lobular panniculitis: diverse group associated with rheumatoid arthritis, gout (Arch Dermatol 1998;134:501)
- Pancreatic panniculitis: lobular fat necrosis with saponification and ghost cells
- Erythema induratum: prominent fat necrosis, histiocytes, giant cells, granulomas, vasculitis
- Lupus panniculitis: may show lymphoid follicles
- Sclerosing panniculitis (lipodermatosclerosis)
Contributed by Carina Dehner, M.D., Ph.D.
Perivascular dermatitis
- Wide spectrum of diagnoses
- Superficial: dermal hypersensitivity with or without eosinophils, urticaria
- Superficial and deep: arthropod bite, connective tissue diseases
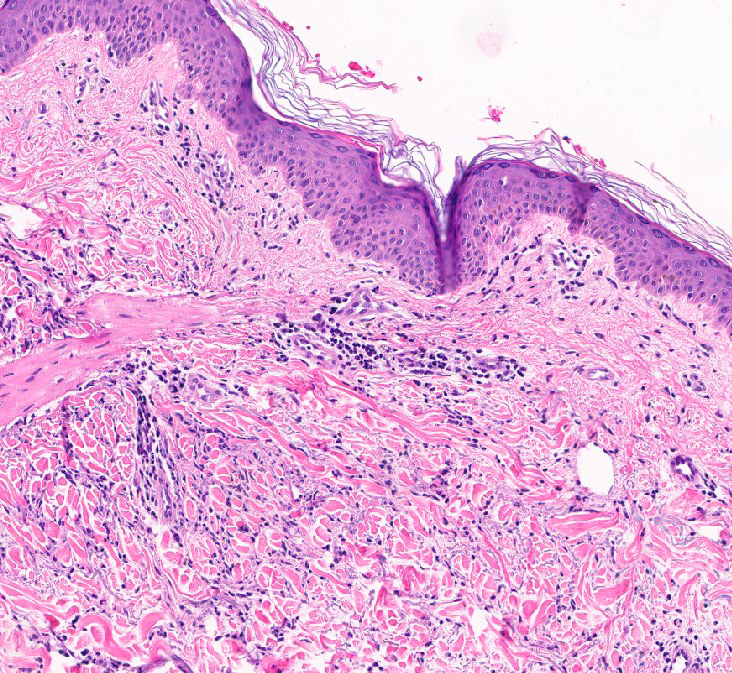
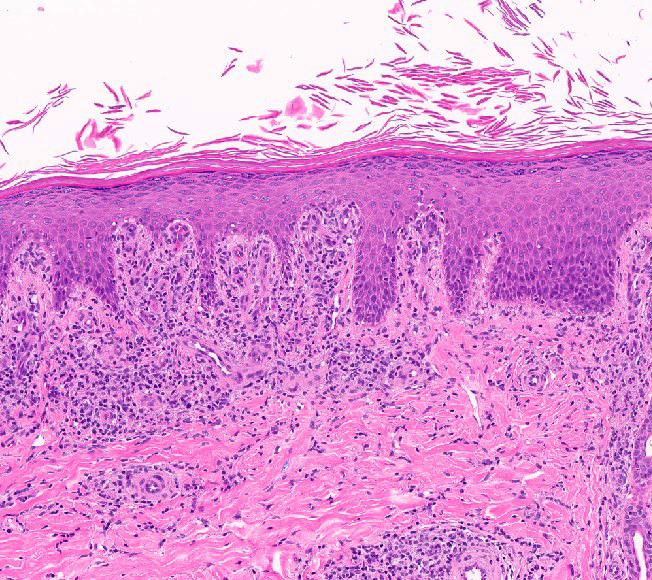
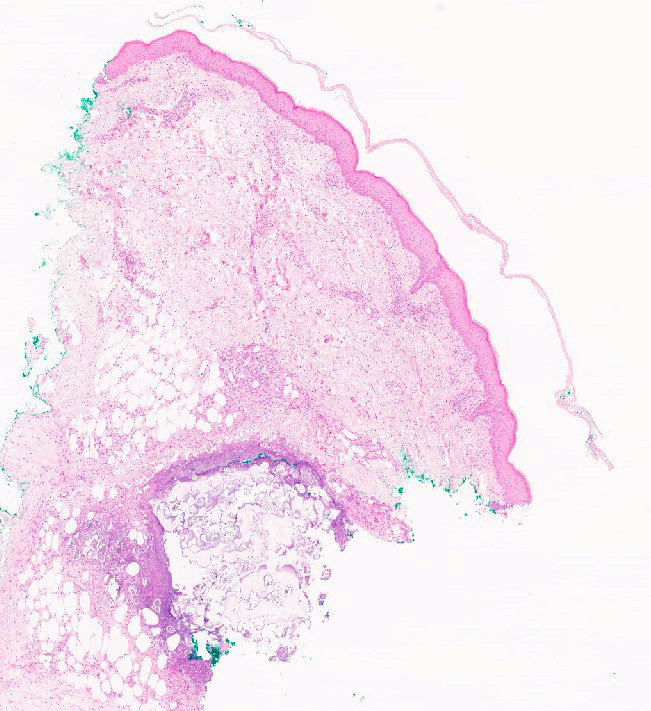
Psoriasiform dermatitis
Sclerosing dermatitis
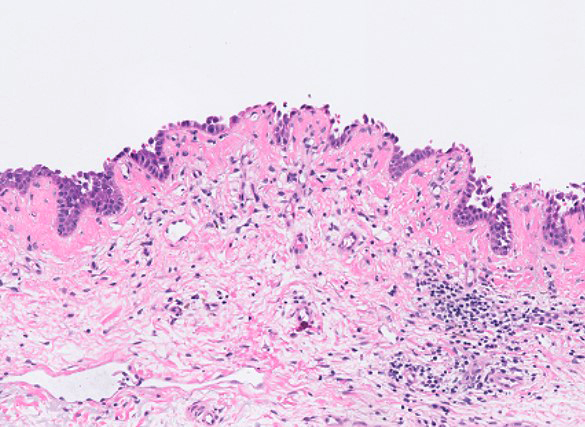
Spongiotic dermatitis
- Spongiosis: accumulation of fluid leading to intercellular edema in the epidermis
- Acute: wet scale + extreme spongiosis (= intraepidermal vesicles) + eosinophils in the inflammatory infiltrate
- Subacute: hyperkeratosis with little parakeratosis + mild acanthosis + mild spongiosis
- Chronic: mild hyperkeratosis + marked acanthosis + minor spongiosis
Contributed by Carina Dehner, M.D., Ph.D.
Vasculopathic / vasculitic dermatitis
- Leukocytoclastic vasculitis: associated with infections, drugs, autoimmune diseases, etc.
- Granuloma faciale: form of leukocytoclastic vasculitis, Grenz zone
- Erythema elevatum diutinum
- Occlusive vasculopathy: fibrin thrombi filling venules and capillaries
Contributed by Carina Dehner, M.D., Ph.D.
Vesiculobullous dermatitis
- Subcorneal split:
- Pemphigus foliaceus:
- Intercellular IgG, C3 on direct immunofluorescence (DIF)
- Sparing of basal layer
- Acute generalized exanthematous pustulosis (AGEP):
- Neutrophils, eosinophils in dermal infiltrate
- Negative DIF
- Pemphigus foliaceus:
- Suprabasal split:
- Pemphigus vegetans:
- Neutrophilic abscesses
- Intercellular IgG, C3 on DIF
- Pemphigus vulgaris:
- Eosinophils, neutrophils, tombstone appearance
- Intercellular IgG, C3 on DIF
- Darier disease:
- Acantholysis and dyskeratosis
- Negative DIF
- Pemphigus vegetans:
- Intraepidermal split:
- Bullous arthropod bite:
- Spongiotic edema, eosinophils
- Negative DIF
- Bullous arthropod bite:
- Subepidermal split:
- Dermatitis herpetiformis:
- Neutrophils in the dermal papillae
- Granular IgA on DIF
- Porphyria cutanea tarda:
- Cell poor split
- IgG around superficial dermal vessels on DIF
- Bullous pemphigoid:
- Eosinophil rich
- Linear IgG and C3 at the dermoepidermal junction on DIF
- Linear IgA bullous dermatosis:
- Neutrophil rich
- Linear IgA at the dermoepidermal junction on DIF
- Dermatitis herpetiformis:
Contributed by Carina Dehner, M.D., Ph.D.
Additional references
Board review style question #1
What is a Majocchi granuloma?
- Deeper fungal infection in which fungi surround degenerate hair shafts
- Necrotizing granuloma seen in infectious diseases, such as tuberculosis
- Nonnecrotizing granuloma seen in diseases such as sarcoidosis
- Palisaded histiocytic granulomatous process with central fibrin, seen in rheumatoid nodule
- Palisaded histiocytic granulomatous process with central mucin, seen in granuloma annulare
Board review style answer #1
A. Majocchi granuloma is a deep fungal infection involving hair follicles caused by dermatophytes, such as T. rubrum
Comment Here
Reference: Common terms & patterns
Comment Here
Reference: Common terms & patterns