Table of Contents
Definition / general | Terminology | Epidemiology | Clinical features | Diagnosis | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Differential diagnosisCite this page: Hamodat M. Leprosy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorleprosy.html. Accessed April 19th, 2024.
Definition / general
- Chronic cutaneous infection caused by Mycobacterium leprae and Mycobacterium lepromatosis (CDC: Mycobacterium lepromatosis Lepromatous Leprosy in US Citizen Who Traveled to Disease-Endemic Areas [Accessed 26 November 2018])
Terminology
- Also called Hansen disease
Epidemiology
- Most U.S. cases occur in immigrants
- Worldwide distribution due to travel and migration but endemic in tropics
Clinical features
- Mycobacterium leprae is an obligate intracellular gram positive and weakly acid fast organism
- The complexity of presentation is related to the varied immunologic responses
- The incubation period is usually 3 - 5 years
- Tuberculoid leprosy occurs in individuals with good cell mediated immunity; patients develop granulomatous response
- Lepromatous leprosy occurs in individuals with poor cell mediated immunity; do not develop a granulomatous response
- Borderline leprosy is an intermediate form between tuberculoid and lepromatous leprosy
- Transmitted by nasal discharge and digital impregnation of skin, as bacilli can be carried under nails and are inoculated under the skin by scratching
- Lucio phenomenon is seen in Mexican and Central American patients who present with untreated, diffuse, non nodular lepromatous leprosy with hemorrhagic infarct
- Planter lesions are at increased risk to develop squamous cell carcinoma (Indian J Lepr 1998;70:179)
- Diagnosis is by PCR; most skin lesions have no identifiable bacteria (J Lab Physicians 2011;3:21)
- Mitsuda reaction: intradermal injection of an armadilloderived lepra bacilli, is useful for classification
- Description:
- Tuberculoid leprosy has hypopigmented center and raised erythematous border
- Lepromatous leprosy has macules, papules and plaques, but firm nodules may also be seen in the face
- Borderline leprosy has hypopigmented macules
Diagnosis
- 16S ribosomal RNA gene PCR assay (can use paraffin block)
Case reports
- 59 year old white man born in the United States with an extensive travel history presenting with progressive skin lesions, prior peripheral neuropathy and arthritis due to M. lepromatosis (CDC: Mycobacterium lepromatosis Lepromatous Leprosy in US Citizen Who Traveled to Disease-Endemic Areas [Accessed 26 November 2018])
Treatment
- Clarithromycin, rifampin and dapsone
Microscopic (histologic) description
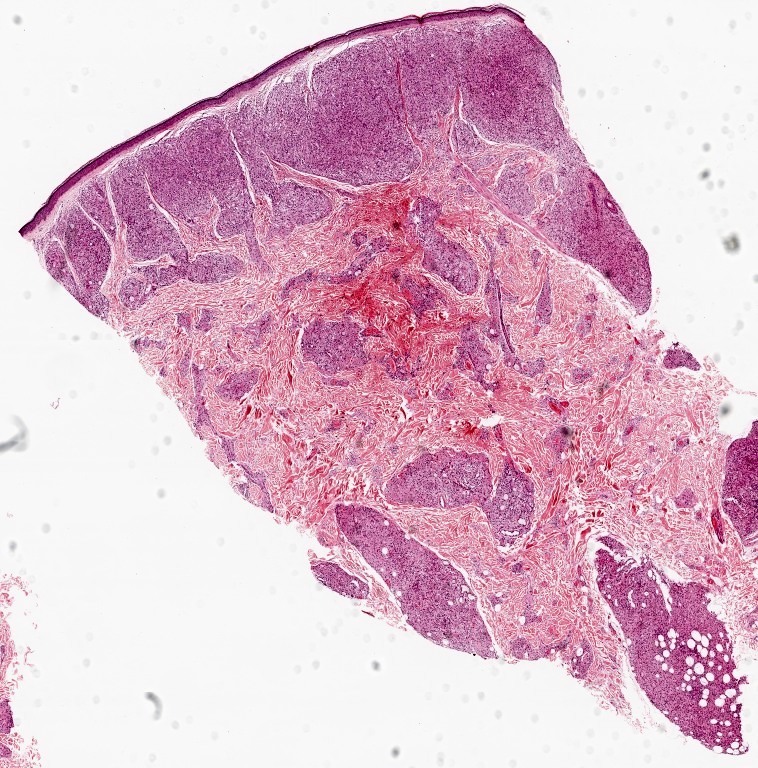
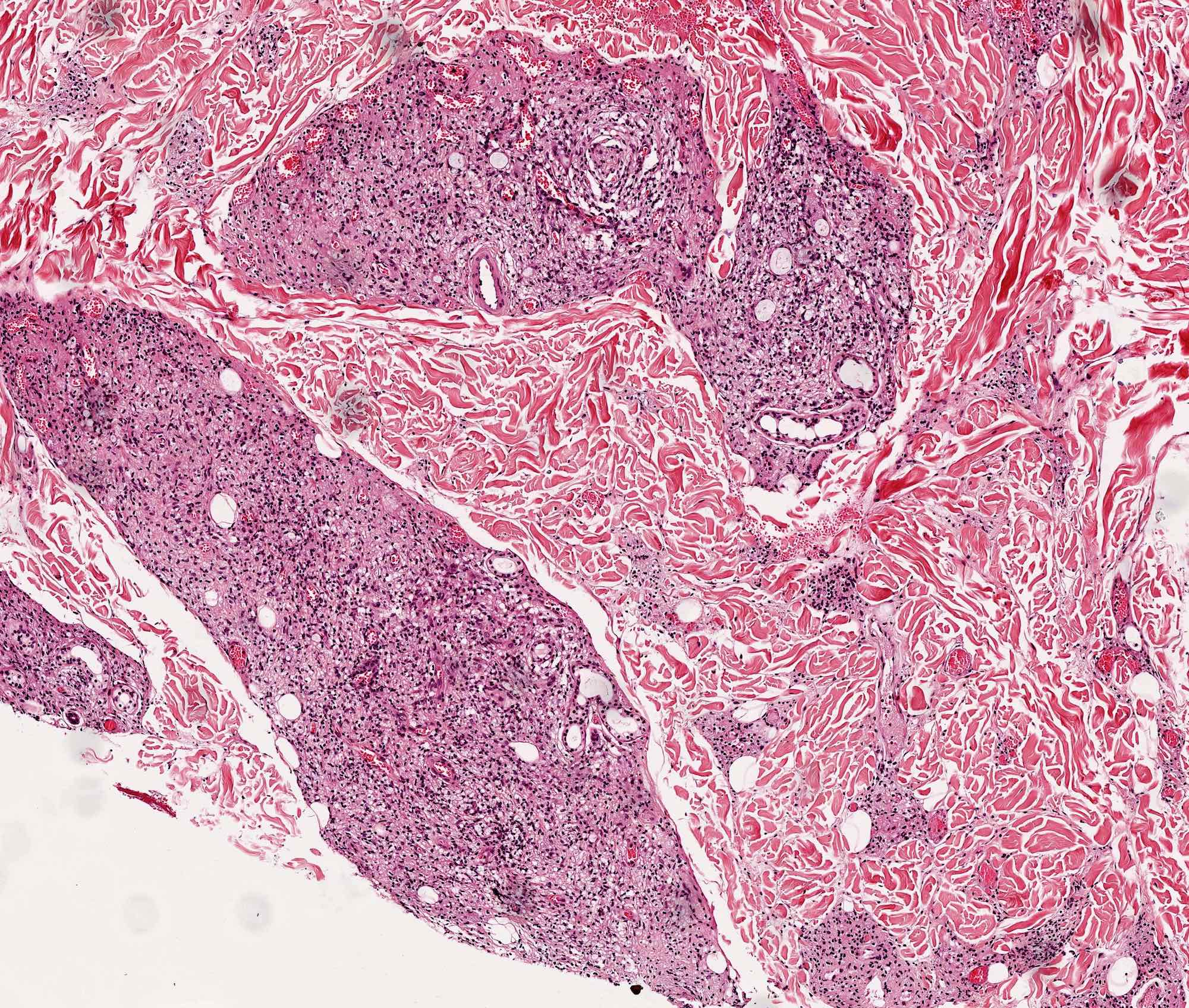
- Tuberculoid leprosy: epithelioid histiocytes surround small cutaneous nerves; Langhans giant cells may be seen but without necrosis; the infiltrate may involve the papillary dermis up to the epidermis; may destroy arrectores pilorum muscle; bacilli are usually scarce
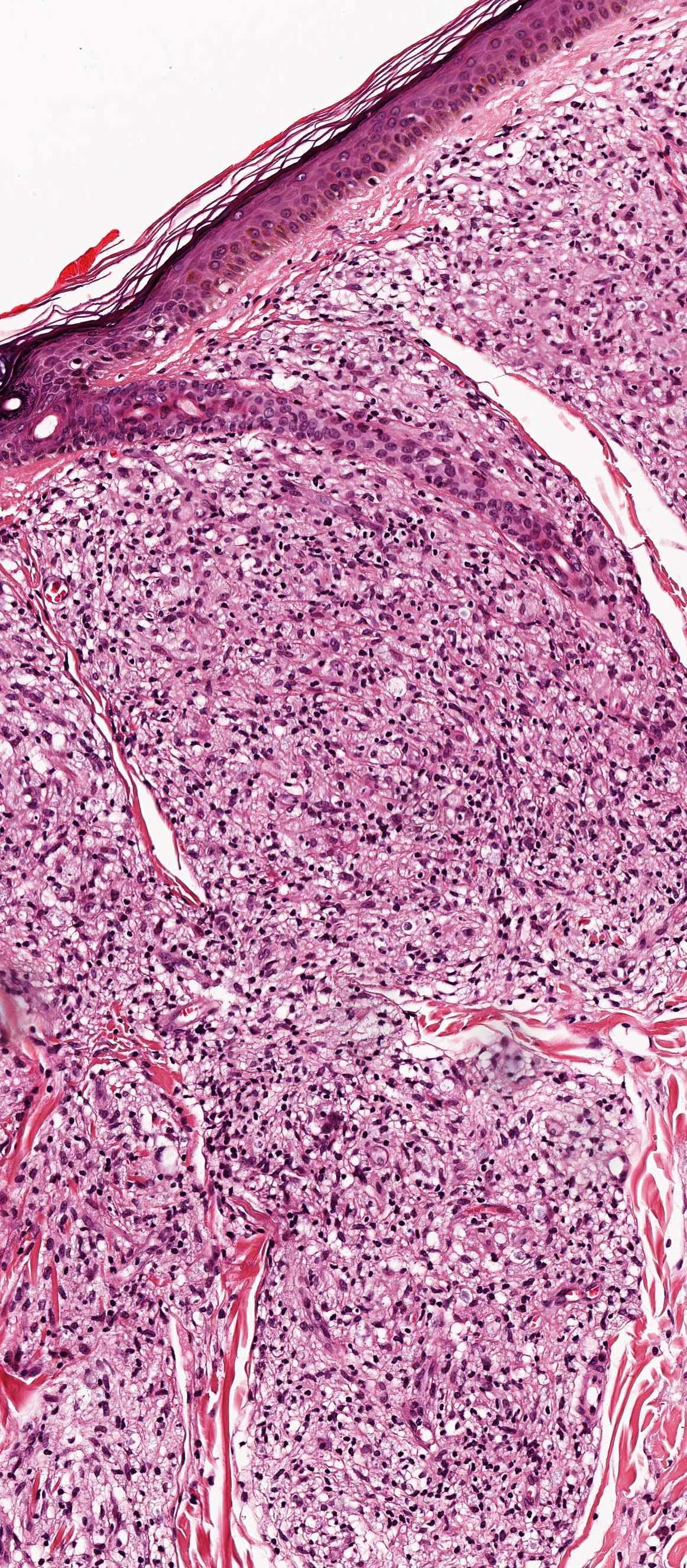
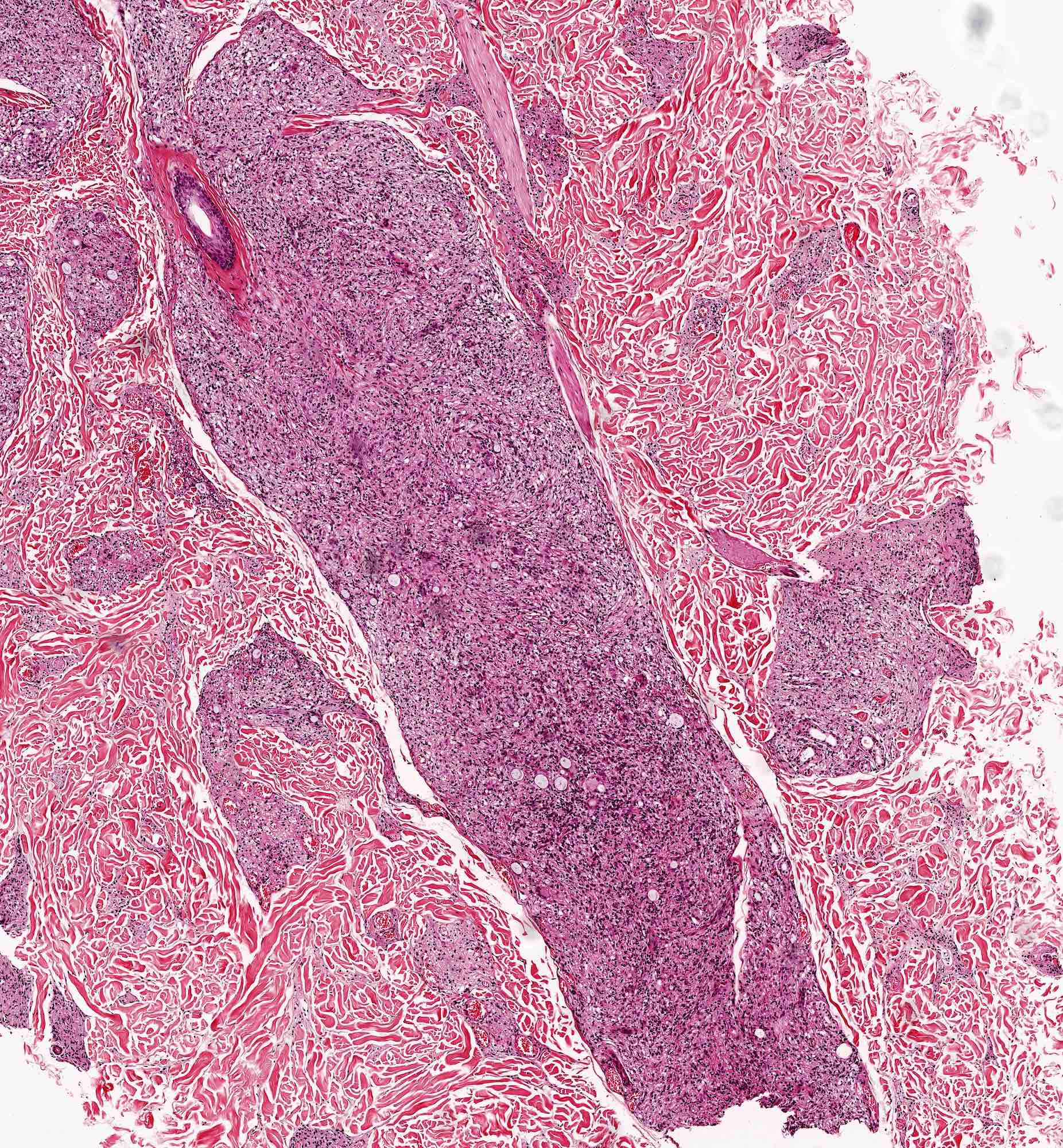
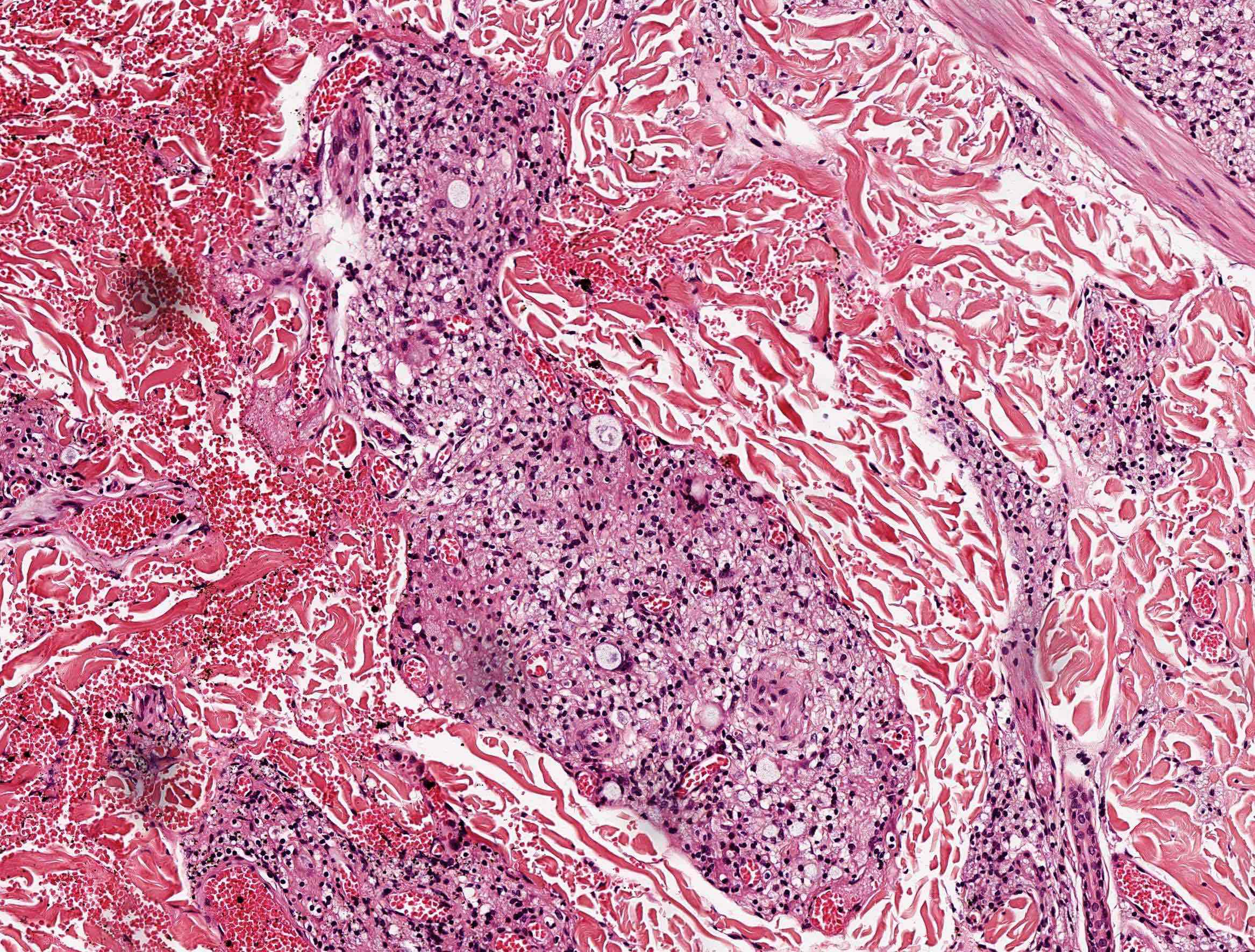
- Lepromatous leprosy: macrophages (Virchow cells, lepra) are found in poorly circumscribed masses in the dermis, with few / no lymphocytes; macrophages may be distended with large groups of leprosy bacilli (globi); bacteria are present in large numbers in cutaneous nerves and in endothelium and media of small and large vessels; may invade arrectores pilorum muscle; may have subcutaneous nodules (erythema nodosum leprorum)
- Borderline leprosy: perineural fibrosis with lamellar or onion skin pattern; more circumscription of the granulomatous response, more lymphocytes and closer relationship to nerves
- Indeterminate leprosy: scanty superficial and deep lymphohistiocytic infiltrate in the dermis with some tendency to localize around appendages; increased mast cells
- Histiocytoid leprosy: spindle cell proliferation with storiform pattern suggestive of fibrous histiocytoma
- Lucio phenomenon: leukocytoclastic vasculitis and epidermal infarction
Microscopic (histologic) images
Positive stains
- Modified Ziehl-Neelsen stain (Wade-Fite) stain
Differential diagnosis