Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Qasim S, Raghavan S. Lipodermatosclerosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorlipodermatosclerosis.html. Accessed April 18th, 2024.
Definition / general
- Lipodermatosclerosis (hypodermitis sclerodermiformis and sclerosing panniculitis) presents as a chronic fibrosing disease commonly associated with venous insufficiency, arterial ischemia or thrombophlebitis
- It is known to affect the subcutis of the lower extremities, commonly in obese, white women, older than 60
- Hypodermitis sclerodermiformis was described in 1955 by Huriez et al. as a scleroderma-like hardening of the legs thought to result from infection of venous ulcers
- In 1980, Burnand et al. used the term venous lipodermatosclerosis, which was characterized by changes in the skin and subcutaneous changes commonly known as postphlebitic leg (Arch Dermatol 1982;118:312)
Essential features
- Lipodermatosclerosis is a chronic inflammatory condition characterized by subcutaneous fibrosis and hardening of the skin on the lower extremities due to venous insufficiency
- Lipodermatosclerosis is also known as venous stasis panniculitis or hypodermitis sclerodermaformis
Terminology
- Venous stasis panniculitis
- Hypodermitis sclerodermiformis and sclerosing panniculitis
- Chronic panniculitis with lipomembranous changes
ICD coding
- ICD-10: I83.10 - varicose veins
Epidemiology
- Common, middle aged or older people (J Am Acad Dermatol 2010;62:1005)
- Women, associated with immobility and a high body mass index (obesity)
Sites
- Lower extremities
- Pretibial or medial aspect of the leg
Pathophysiology
- Result of venous insufficiency, triggered by:
- Incompetent venous valves
- Venous outflow obstruction
- Dysfunction of the calf muscle pump (Am Fam Physician 2019;100:298)
- Resulting venous hypertension leads to an increase of leukocytes in the veins, which migrate to surrounding tissue
- Leukocytes are activated, releasing proinflammatory cells and cytokines, inducing a chronic inflammatory state
- Increased collagen production leads to the fibrosis of subcutaneous fat
Etiology
- Vascular damage, venous incompetence / hypertension and to a lesser extent, arterial ischemia
- Abnormal fibrinolytic activity
- Histologically shows an increase in dermal fibroblast proliferation and procollagen gene expression, suggesting involvement of these factors
- Reference: Dermatol Ther 2010;23:375
Clinical features
- Acute phase
- Similar to cellulitis, with induration, erythema, pain, itching and swelling
- Chronic phase
- Subcutaneous fibrosis, resulting in narrowing of the distal lower limb, causing the leg to have the classical upside down champagne bottle appearance; hard, wood-like appearance, which becomes circumferential in well developed lesions (Semin Cutan Med Surg 2013;32:169)
- Overlying ulceration or crusting
- Hyperpigmentation of the skin from hemosiderin deposition, varicose veins, venous eczema
Diagnosis
- Biopsy
Case reports
- 61 year old woman with oxandrolone treatment for acute lipodermatosclerosis (J Vasc Bras 2019;18:e20190031)
- 62 year old woman with pancreatic carcinoma diagnosed with gemcitabine related acute lipodermatosclerosis (J Oncol Pharm Pract 2019;25:1271)
Treatment
- Lifestyle: weight reduction, physical activity
- Preventive measures: compression therapy and elevation
- Medical treatment: stanozolol, pentoxifylline, hydroxychloroquine (Am Fam Physician 2019;100:298)
- Ultrasound therapy
- Ultraviolet radiation (UVA1)
- Surgical treatment
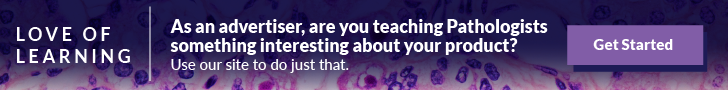
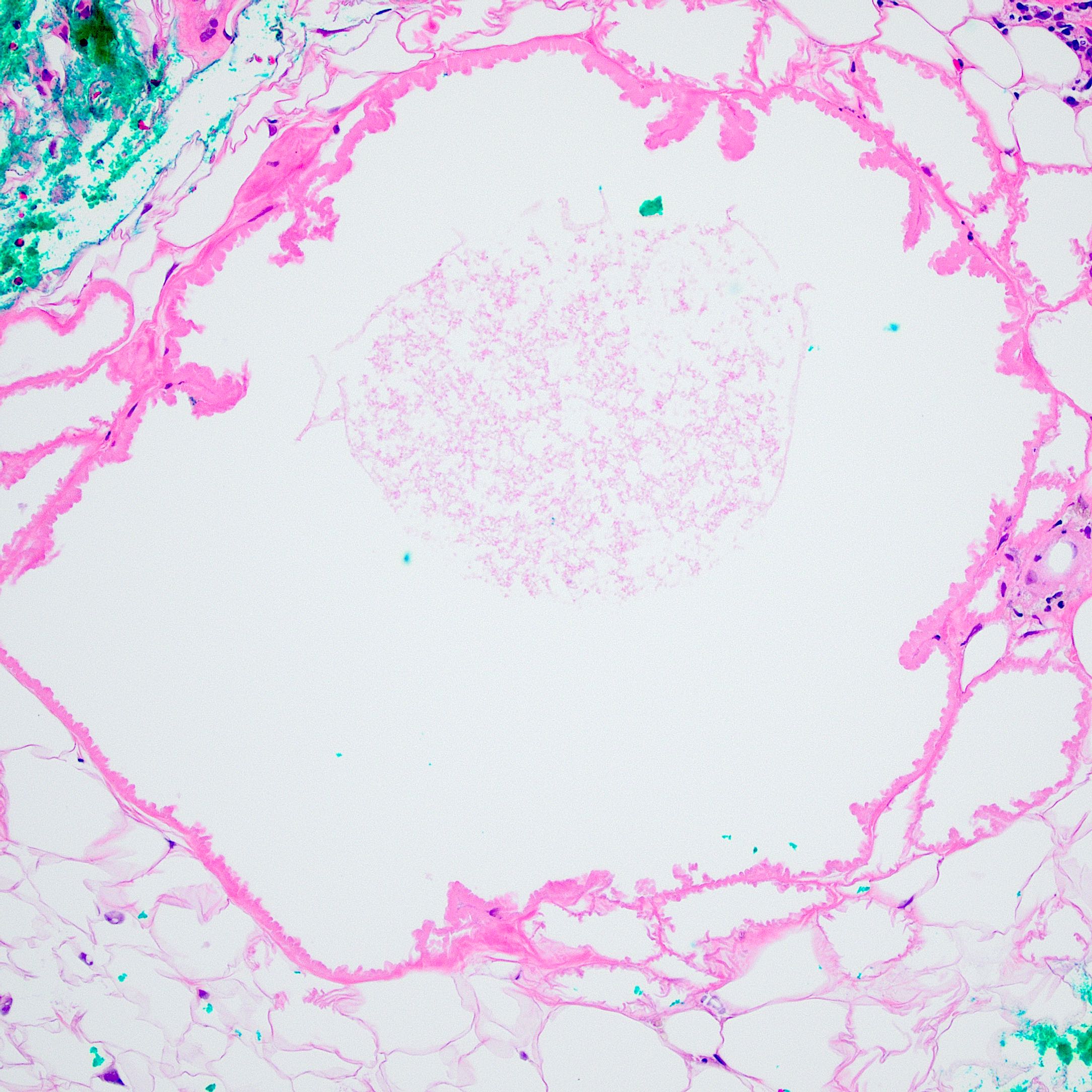
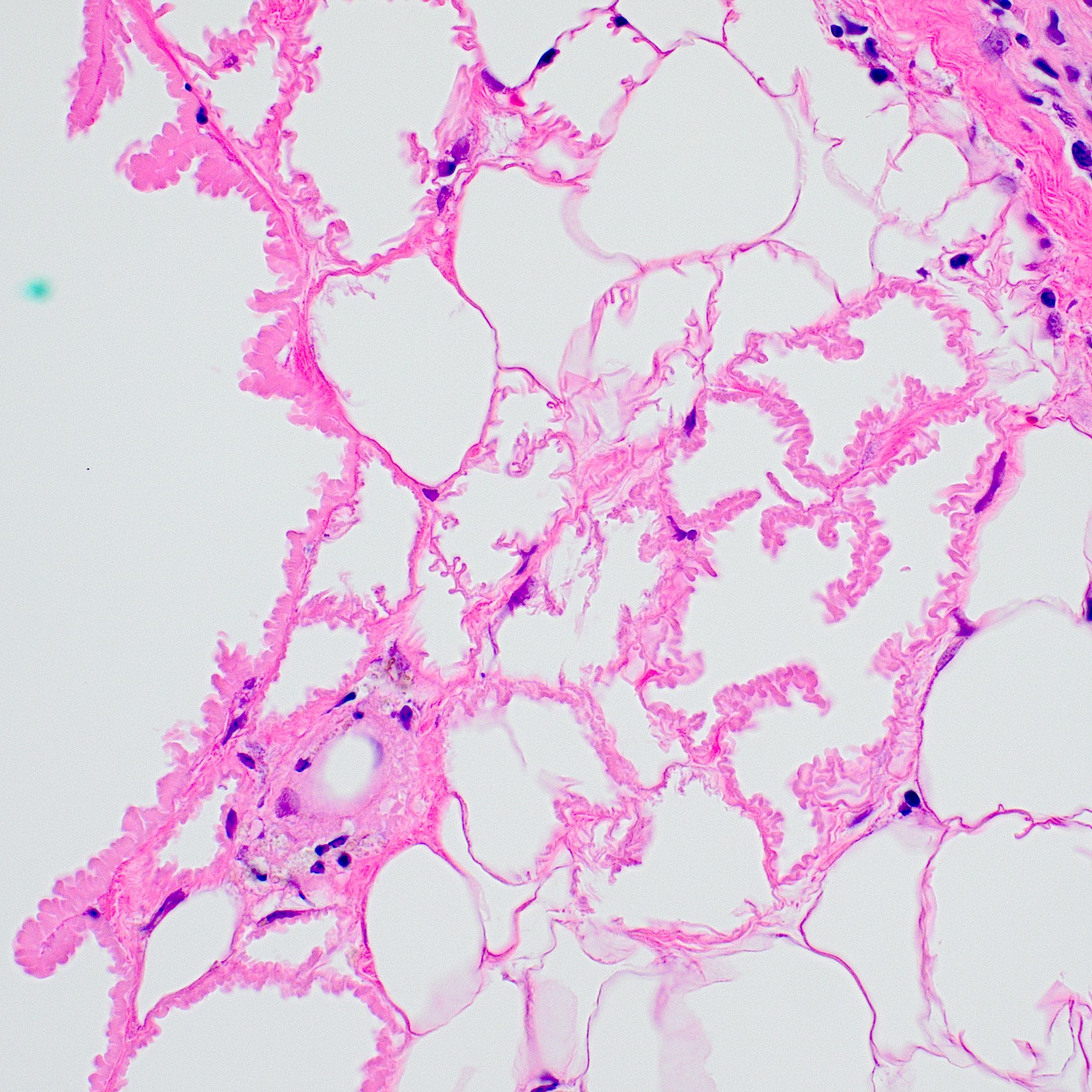
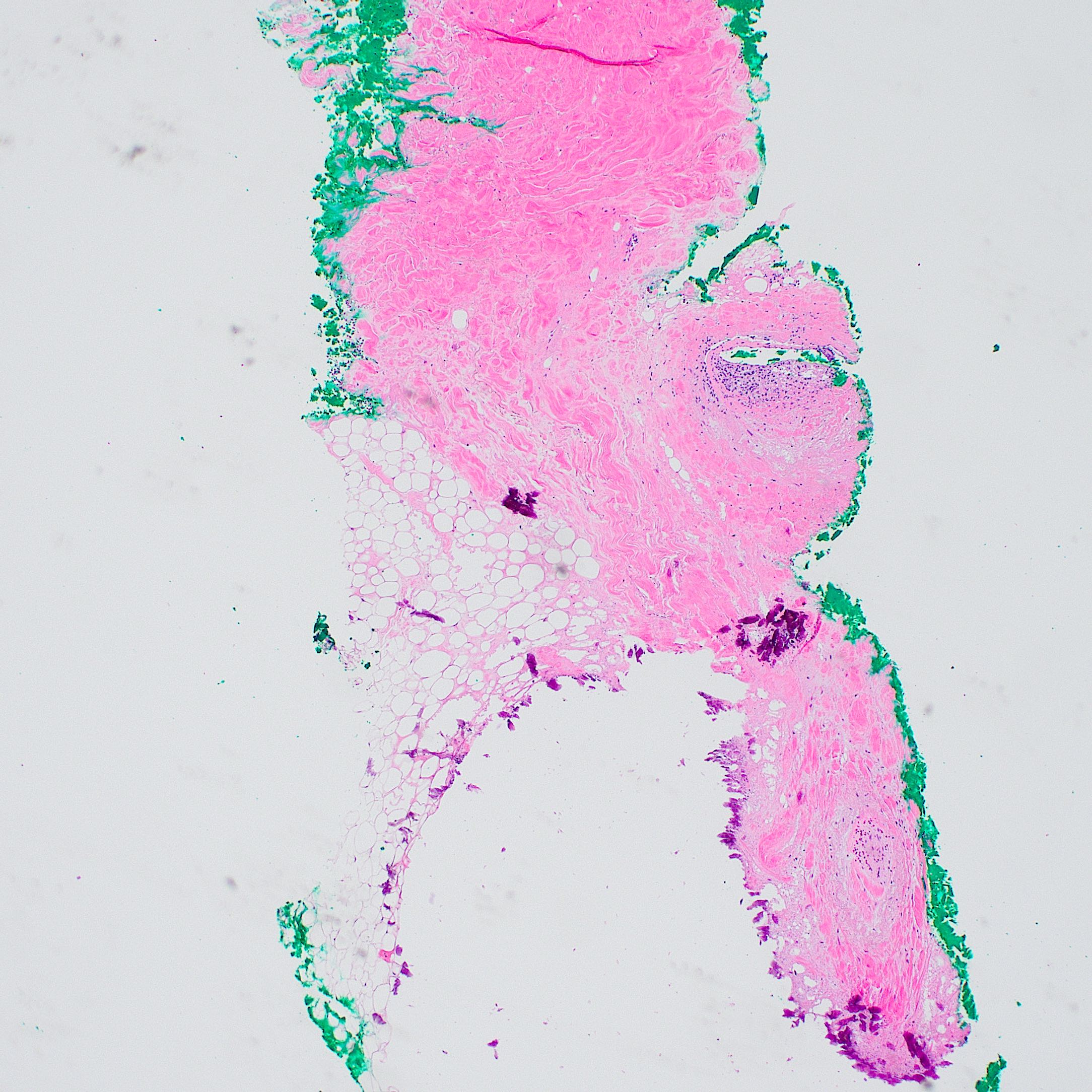
Microscopic (histologic) description
- Lobular and septal involvement of the subcutaneous tissue, fat necrosis, macropseudocyst and micropseudocyst formation and calcification of adipocytes
- Lipomembranes (crenated appearance, eosinophilic feathery anuclear lining of cystic adipocytes) classic but not definitive for the diagnosis
- Pseudoxanthoma elasticum-like septal elastosis with calcification is a consistent finding
- Reference: Int J Dermatol 2016;55:303
Microscopic (histologic) images
Sample pathology report
- Skin, left leg, biopsy:
- Lipodermatosclerosis
Differential diagnosis
- Erythema nodosum:
- Septal panniculitis with a mixed cellular infiltrate of lymphocytes, histiocytes, giant cells and occasional eosinophils, and a characteristic absence of vasculitis
- Morphea (localized scleroderma):
- Atrophic epidermis
- Thickened, hyalinized collagen, with possible loss of appendageal structures
- Inflammatory cell infiltrate (lymphocytes with or without plasma cells)
- Necrobiosis lipoidica:
- Layered inflammatory process and alternating zones of necrobiosis involving the full thickness of the dermis (stacked lasagne type appearance)
- Histiocytic infiltrate with multinucleated giant cells surrounds these areas and accompanying inflammatory infiltrate is predominantly lymphocytic with plasma cells and occasional eosinophils
- Cellulitis:
- Neutrophil predominant perivascular inflammation
Board review style question #1
Board review style answer #1
D. Pseudocyst formation. The biopsy shows classical findings of lipodermatosclerosis, including fat necrosis, pseudocyst formation, calcification of adipocytes and the presence of lipomembranes (eosinophilic feathery anuclear lining of cystic adipocytes) are diagnostic; however, neutrophil infiltration, predominant histiocytic infiltrate and granuloma formation are not historically associated with lipodermatosclerosis.
Comment Here
Reference: Lipodermatosclerosis
Comment Here
Reference: Lipodermatosclerosis
Board review style question #2
Which of the following is the underlying major pathophysiology for lipodermatosclerosis?
- Allergic reaction
- Bacterial infection
- Chronic venous stasis
- Repeated microtrauma
Board review style answer #2
C. Chronic venous stasis. Lipodermatosclerosis is an inflammatory skin condition resulting from underlying venous insufficiency, which is caused by incompetent venous valves, venous outflow obstruction or dysfunction of the calf muscle pump.
Comment Here
Reference: Lipodermatosclerosis
Comment Here
Reference: Lipodermatosclerosis