Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Collie CJ, Ho JD. Ochronosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skinnontumorochronosis.html. Accessed April 20th, 2024.
Definition / general
- Disorders characterized by blue-gray to black pigmentation due to deposition of ochre colored pigment in connective tissues
- 2 main forms: alkaptonuria / endogenous ochronosis (homogentisate 1,2 dioxygenase deficiency) and exogenous ochronosis (overuse of topical hydroquinone and other medicaments)
Essential features
- Deposition disorder characterized by deposition of homogentisic acid in connective tissue
- May result from an inborn error of metabolism (alkaptonuria) or from overuse of topical hydroquinone or other phenol containing medications (exogenous ochronosis)
- Alkaptonuria presents with hyperpigmentation, arthropathies, kidney disease and heart disease
- Exogenous ochronosis patients primarily present with hyperpigmentation involving the face, neck or upper limbs
- Classical histologic findings in the skin include formation of banana shaped, yellow-brown deposits and heavy elastosis in the superficial dermis
ICD coding
Epidemiology
- Alkaptonuria
- Very rare; prevalence 1:100,000 - 250,000 (J Med Genet 2002;39:E40)
- Exogenous ochronosis
- Little data available
- F > M
- Variable prevalence among ethnicities with dark skinned individuals thought to be the most affected (Indian J Dermatol 2015;60:537)
- U.S. data: 22 cases in 50 years (J Am Acad Dermatol 2007;57:854)
Sites
- Alkaptonuria: skin (ear, face, acral surfaces and axillae), sclera, bone cartilage, kidney and cardiac valves
- Exogenous ochronosis: skin of the malar areas, temples, lower cheeks, neck, forearms and hands
Pathophysiology
- Alkaptonuria
- Inborn error of tyrosine metabolism secondary to autosomal recessive loss of function mutations in HGD / HGO (Nat Genet 1996;14:19)
- Resultant deficiency of homogentisate 1,2 dioxygenase leads to accumulation of homogentisic acid and eventual deposition in collagen rich tissue (Calcif Tissue Int 2017;101:50)
- Long term deposition leads to degenerative arthritis, cardiac valvulopathy, renal disease and oculocutaneous pigmentation (N Engl J Med 2002;347:2111)
- Exogenous ochronosis
- Localized inhibition of homogentisate 1,2 dioxygenase primarily by topical application of phenol containing compounds, particularly hydroquinone (Arch Dermatol 1985;121:1239)
- Deposition and polymerization of homogentisic acid on collagen and elastic fibers (Am J Dermatopathol 2014;36:989, Am J Dermatopathol 2020;42:571)
Etiology
- Alkaptonuria
- Autosomal recessive loss of function mutations in HGD / HGO
- Exogenous ochronosis
- Prolonged use of topical hydroquinone (Dermatol Online J 2019;25:13030/qt5vd7h6xc)
- Less common associations include antimalarials, phenol, resorcinol, quinine injections, mercury and picric acid (Am J Clin Dermatol 2001;2:213, J Am Acad Dermatol 1986;15:357)
Clinical features
- Alkaptonuria
- Blue-gray to black macules and papules on sclera, cheeks, cartilaginous portions of the ear and acral surfaces (N Engl J Med 2002;347:2111)
- Brown discoloration of the axillae (Int J Rheum Dis 2014;17:327)
- Black discoloration of urine if left to stand
- Renal disease, including calculi, tubulointerstitial disease and renal tubular acidosis (Clin Nephrol 2015;84:339, Mod Pathol 1992;5:464, Saudi J Kidney Dis Transpl 2018;29:997)
- Arthritis (N Engl J Med 2002;347:2111)
- Cardiac valvulopathy (J Heart Valve Dis 2006;15:730)
- Exogenous ochronosis
- Speckled blue-gray or brown-black macules on head, neck, upper limbs and hands; more severe on malar areas and other sun exposed skin (Am J Dermatopathol 2019;41:e47)
- Occasional caviar-like papules (Int J Dermatol 2013;52:413)
- Areas of admixed hypopigmentation or erythema occasionally noted
- Dematoscopic examination reveals dark amorphous structures in involved skin with obliteration of follicular ostia (Indian J Dermatol Venereol Leprol 2013;79:819)
Diagnosis
- Alkaptonuria
- Urine gas chromatography mass spectrometry analysis for homogentisic acid (J Chromatogr B Analyt Technol Biomed Life Sci 2014;963:106)
- PCR evaluating for HGD mutations (Clin Genet 2003;63:145)
- Skin biopsy
- Exogenous ochronosis
- High index of suspicion in the correct clinical context
- Thorough medication history
- Examination of cosmetic cream ingredients for hydroquinone
- Skin biopsy
Laboratory
- Increased urinary levels of homogentisic acid on gas chromatography mass spectrometry analysis in alkaptonuria (J Chromatogr B Analyt Technol Biomed Life Sci 2014;963:106)
- Pathogenic biallelic mutations of HGD on molecular testing with PCR (JIMD Rep 2015;24:3)
Radiology description
- Xray findings in alkaptonuric arthropathy include joint space narrowing, osteophyte formation, joint space calcification and reactive sclerosis of articular surfaces (Radiol Med 2005;110:349)
Prognostic factors
- Alkaptonuria
- Normal life expectancy (Rare Dis 2013;1:e27475)
- Arthropathy increases morbidity
- Exogenous ochronosis
- Late diagnosis and extensive hyperpigmentation at time of diagnosis connote poor prognosis
Case reports
- 53 year old man with knee pain (Medicine (Baltimore) 2019;98:e16837)
- 53 year old man with progressively spreading papules on hands, nose and ears (J Dermatol Case Rep 2015;9:42)
- 56 year old man with blue-gray pigmentation of external ear (ScientificWorldJournal 2010;10:1530)
- 60 year old man with rheumatoid arthritis and new onset facial pigmentation with use of hydroxychloroquine (Eur J Rheumatol 2018;5:206)
- 63 year old woman with ochronosis; reflectance confocal microscopic, dermoscopic and electron microscopic features (Arch Dermatol 2010;146:1021)
Treatment
- Alkaptonuria
- Dietary reduction of phenylalanine and tyrosine
- Cardiac valve replacement
- Arthroplasty
- Oral nitisinone (Metabolism 2005;54:719)
- Oral ascorbic acid (Ann Clin Biochem 2003;40:108)
- Exogenous ochronosis
- Discontinuation of causative agent
- Sunscreen
- Q switch alexandrite laser (Dermatol Surg 2004;30:555)
Clinical images
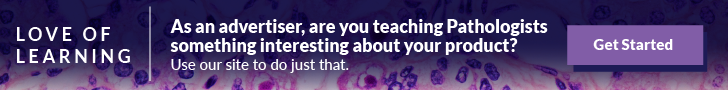
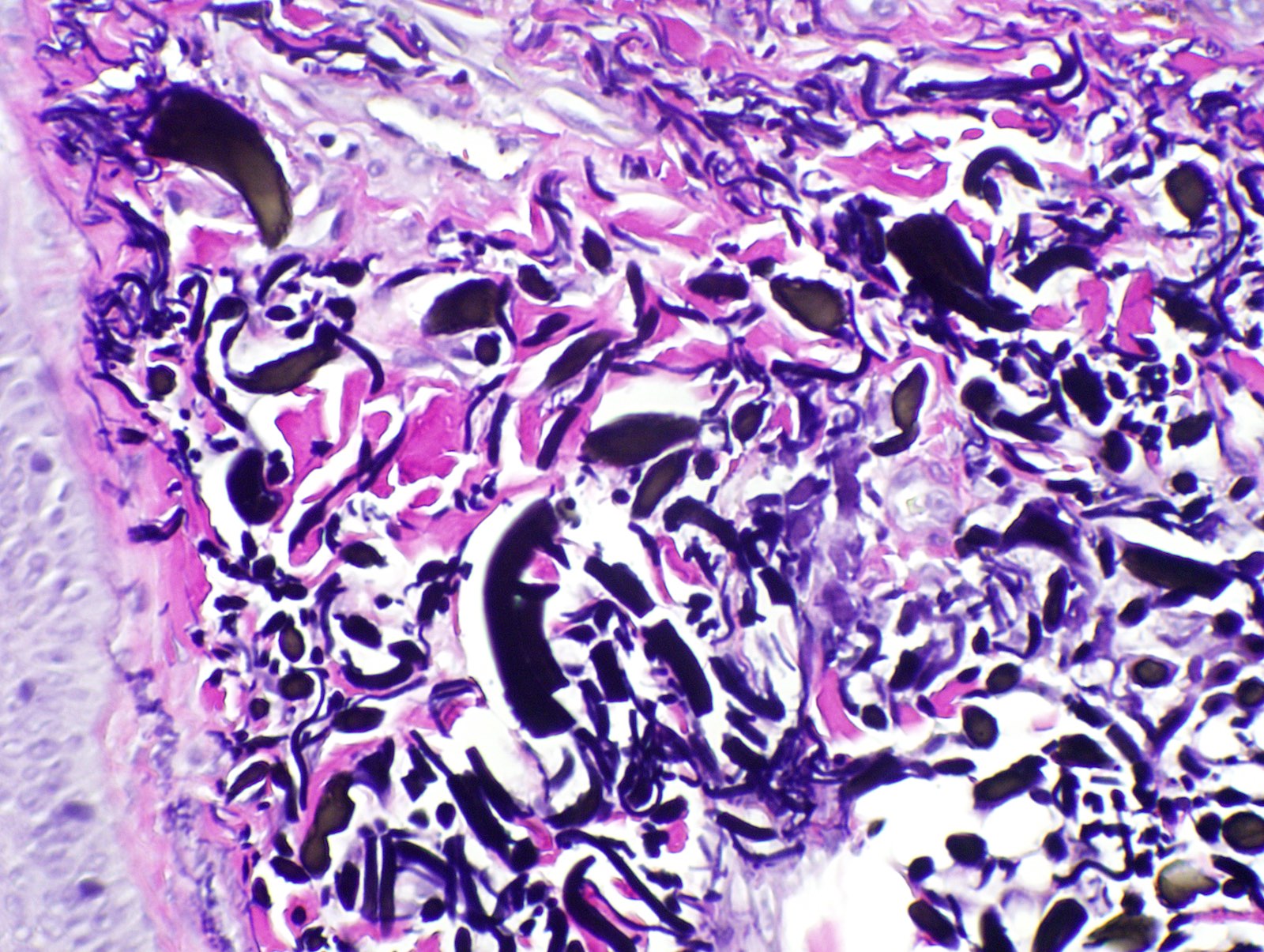
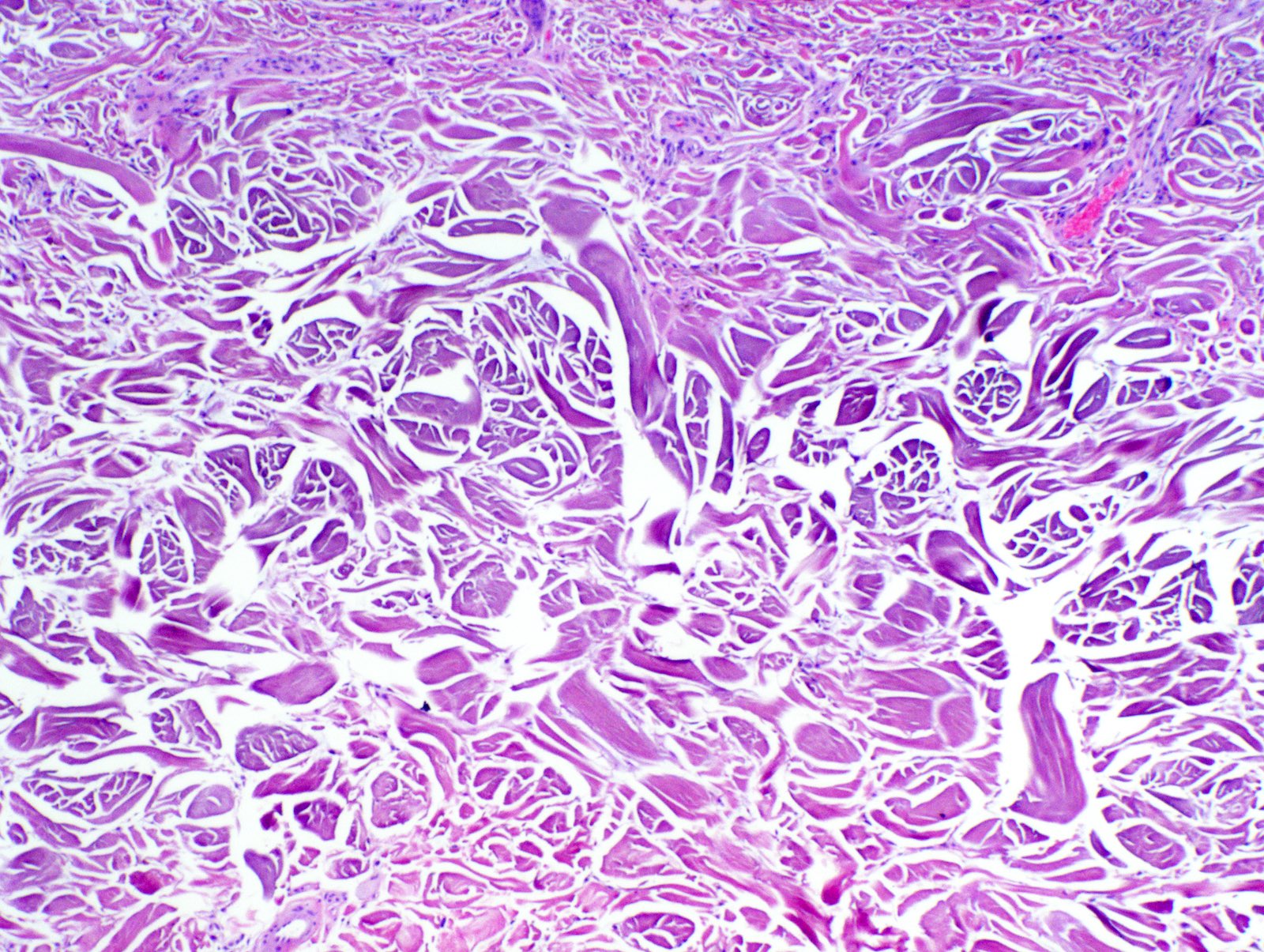
Microscopic (histologic) description
- Features of ochronosis are similar in both alkaptonuria and exogenous ochronosis
- Early changes include homogenization of collagen and degenerating elastotic fibers (Am J Dermatopathol 2014;36:989, Am J Dermatopathol 2019 Nov 12 [Epub ahead of print])
- Yellow-brown, banana shaped, sickled or round ochronotic bodies deposit in the connective tissue
- Occasional bodies may be seen in direct continuity with collagen or elastic fibers (Am J Dermatopathol 2019 Nov 12 [Epub ahead of print])
- Exogenous ochronosis
- Extensive solar elastosis-like change is noted in an interfollicular distribution
- Decreased basal keratinocyte pigmentation
- Occasionally, ochronotic bodies are seen in association with colloid milium and are designated pigmented colloid milium (J Dermatol Case Rep 2015;9:42)
- Granulomatous reaction has also been reported (J Cutan Pathol 1990;17:236)
- Similar ochronotic bodies are seen in the connective tissues of cardiac, scleral and bony tissue when involved
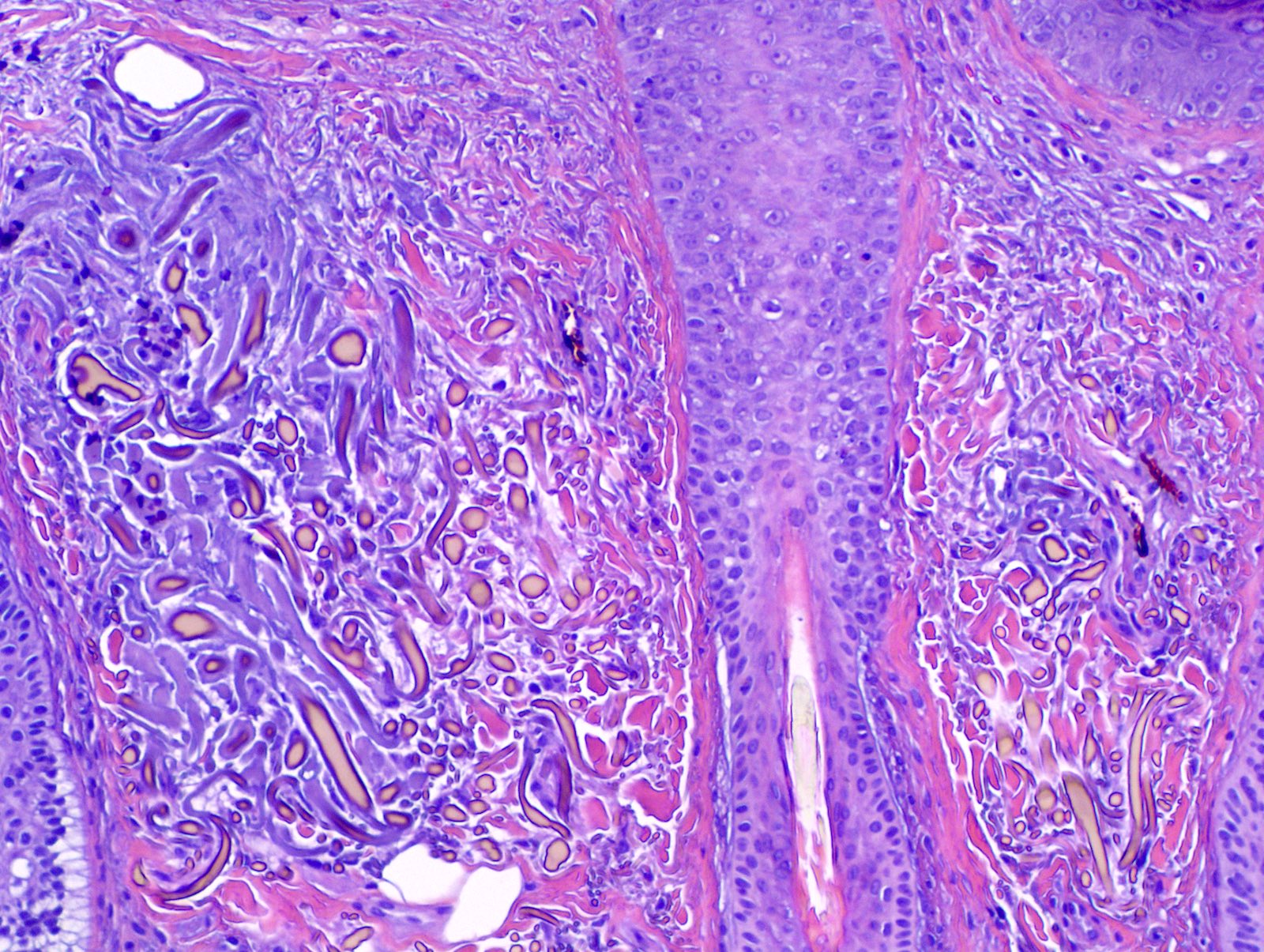
Microscopic (histologic) images
Positive stains
- Methylene blue (Indian J Dermatol Venereol Leprol 2015;81:623)
- Variable Verhoeff van Gieson (Am J Dermatopathol 2019 Nov 12 [Epub ahead of print])
Negative stains
Electron microscopy description
- Electron dense material within elastic fibers
- Degeneration of elastic fibers with fragmentation, clearing and a moth eaten appearance
- Reference: Arch Dermatol 2010;146:1021
Molecular / cytogenetics description
- Numerous HGD mutations reported in alkaptonuria
- Reference: JIMD Rep 2012;4:55
Sample pathology report
- Right cheek, punch biopsy:
- Ochronosis (see comment)
- Comment: The specimen exhibits extensive elastosis in an interfollicular distribution and scattered yellow-brown, banana shaped deposits in the superficial dermis in keeping with exogenous ochronosis.
Differential diagnosis
- Melasma:
- Increased keratinocyte melanization, which may involve all layers of the epidermis
- Variable papillary dermal melanophages
- Solar elastosis
- Telangiectasia
- Increased mast cells
- Acquired bilateral nevus of Ota-like macules (Hori nevus):
- Scattered dendritic melanocytes in the superficial dermis
- Cells typically heavily pigmented and express melanocyte markers
- Argyria:
- Fine, black granules deposited on the basement membrane of blood vessels and skin adnexa
- Lichen planus pigmentosus:
- Subtle interface dermatitis (active lesion)
- Focal band-like lymphocytic infiltrate (active lesion)
- Band-like or perivascular heavily pigmented melanophages (active and burnt out lesions)
- Facial acanthosis nigricans:
- Hyperkeratosis
- Papillomatosis
- Only subtle increase in basal keratinocyte pigmentation
Additional references
Board review style question #1
A 40 year old Afro-Caribbean woman with a history of long term use of skin lightening products presents with an asymptomatic hyperpigmented eruption involving the face. A punch biopsy reveals yellow-brown, banana shaped deposits in the superficial dermis. What is the most likely diagnosis?
- Acanthosis nigricans
- Argyria
- Exogenous ochronosis
- Lichen planus pigmentosus
- Melasma
Board review style answer #1
C. Exogenous ochronosis. This image shows extensive elastosis with the formation of banana bodies / ochronotic bodies. These findings are diagnostic of ochronosis. The association with skin lightening agents favor exogenous ochronosis rather than heritable ochronosis.
Comment Here
Reference: Ochronosis
Comment Here
Reference: Ochronosis
Board review style question #2
A 60 year old man presents for hip replacement. On preoperative evaluation, black discoloration of the sclera and ear cartilage are noted and a diagnosis of alkaptonuria is entertained. What enzyme is deficient in patients with alkaptonuria?
- Fumarylacetoacetate hydrolase
- Homogentisate 1,2 dioxygenase
- Tyrosinase
- Tyrosine aminotransferase
- 4-hydroxyphenylpyruvate dioxygenase
Board review style answer #2
B. Homogentisate 1,2 dioxygenase. Alkaptonuria is an inborn error of tyrosine metabolism secondary to autosomal recessive loss of function mutations in HGD / HGO, resulting in a deficiency of homogentisate 1,2 dioxygenase. This leads to the accumulation of homogentisic acid with deposition in collagen rich tissue. Longterm tissue deposition leads to degenerative arthritis, cardiac valvulopathy, renal disease and oculocutaneous pigmentation
Comment Here
Reference: Ochronosis
Comment Here
Reference: Ochronosis