Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Head and neck mucosal melanoma staging | Genitourinary tract mucosal melanoma staging | Diagnosis | Prognostic factors | Case reports | Clinical images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Deerwester M, Smoller BR. Mucosal melanoma (genital, oral, sinonasal). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumormelanocyticmucosalmelanoma.html. Accessed April 19th, 2024.
Definition / general
- Malignant neoplasm of mucosal melanocytes
- Rare melanoma subtype that originates from melanocytes within sun protected mucous membranes
- Mucosal melanomas share many of the histologic characteristics of cutaneous melanomas and differ mainly in the underlying anatomic sites involved
Essential features
- Mucosal melanoma represents a rare subtype of melanoma, accounting for ~0.8 - 3.7% of all melanomas in Caucasians (Cancer Treat Res 2016;167:295)
- Can arise from any mucosal epithelium within the body, including epithelium from the lower GI tract (26.5%), nasal cavity and paranasal sinuses (23%), gynecological sites (22.5%), oral cavity (15%), urological sites (5%), upper GI tract (5%) and other (e.g., conjunctiva, 3%) (Cancer Treat Res 2016;167:295)
- While the incidence of cutaneous melanomas has increased by ~1.4% every year, the incidence of mucosal melanoma has remained stable (Cancer Treat Res 2016;167:295)
- Mucosal melanoma is one of the most aggressive subtypes of melanoma and carries a significantly worse prognosis than cutaneous melanoma with a 5 year overall survival of < 25%; 23% of patients have metastases at the time of diagnosis (Ann Oncol 2017;28:868)
ICD coding
- ICD-10:
- C21.0 - malignant neoplasm of anus, unspecified
- C21.1 - malignant neoplasm of anal canal
- C43.0 - malignant melanoma of lip
- C43.11 - malignant melanoma of right eyelid, including canthus
- C43.12 - malignant melanoma of left eyelid, including canthus
- C43.51 - malignant melanoma of anal skin
- C51.0 - malignant neoplasm of labium majus
- C51.1 - malignant neoplasm of labium minus
- C51.2 - malignant neoplasm of clitoris
- C51.8 - malignant neoplasm of overlapping sites of vulva
- C51.9 - malignant neoplasm of vulva, unspecified
- C60.0 - malignant neoplasm of prepuce
- C60.1 - malignant neoplasm of glans penis
- C60.2 - malignant neoplasm of body of penis
- C60.8 - malignant neoplasm of overlapping sites of penis
- C60.9 - malignant neoplasm of penis, unspecified
Epidemiology
- Unlike cutaneous melanoma, which is estimated to be the fifth most common cancer in the United States among men and the sixth among women, mucosal melanomas are rare
- Mucosal melanomas represent only ~1.4% of all melanomas (all races / ethnicities); however, they have a worse prognosis when compared to cutaneous melanomas
- Mucosal melanoma accounts for ~0.8 - 3.7% of all melanomas in Caucasians; the incidence of mucosal melanomas is higher in Caucasians than other racial groups (Cancer Treat Res 2016;167:295)
- Mucosal melanoma differs by race / ethnicity with regard to the anatomic site
- Non-Hispanic whites have the highest proportion of genitourinary mucosal melanoma, while Asian / Pacific Islanders most commonly have anorectal mucosal melanoma; head and neck tumors are most frequently seen in Hispanics (J Am Acad Dermatol 2017;76:250)
- Mucosal melanoma tends to present in older populations compared to cutaneous melanoma (median age of diagnosis: 70 versus 55 years old) (Cancer Treat Res 2016;167:295)
- Gender disparities within mucosal melanoma exist with the incidence being 2 times higher in women, due to the development of the disease in the genital tract (Cancer Treat Res 2016;167:295)
Sites
- Arises in the head and neck in the following decreasing order of prevalence: nasal cavity, paranasal sinuses and oral cavity
- Larynx
- Esophagus
- Rectum and anal canal
- Vagina
- Cervix
Pathophysiology
- Evolution of mucosal melanoma from precursor lesions is poorly understood but has been associated with some risk factors
- Presence of melanocytes has been demonstrated in many mucosal membranes; however, their function in the mucosa is not well understood
- Many mutations have been associated with mucosal melanomas (see Molecular section) (Front Oncol 2021;11:702287)
Etiology
- Smoking, ill fitting dentures and ingested / inhaled carcinogens, such as tobacco and formaldehyde, are regarded as potential causative factors for oral and sinonasal mucosal melanoma (Front Oncol 2021;11:702287)
- Chronic inflammatory disease, viral infections and chemical irritants are thought to be implicated in vulvar mucosal melanoma
- Human immunodeficiency virus (HIV) is associated with anorectal mucosal melanoma
Head and neck mucosal melanoma staging
- The AJCC TNM stages for mucosal melanoma of the head and neck are as follows (Amin: AJCC Cancer Staging Manual, 8th Edition, 2017):
- T1 and T2: omitted due to the poor prognosis of even small and superficial lesions
- T3: mucosal disease
- T4A: moderately advanced disease; tumor involves the cartilage, deep soft tissue or overlying skin
- T4B: very advanced disease; tumor involves one or more of the following:
- Brain
- Dura
- Skull base
- Lower cranial nerves (IX, X, XI, XII)
- Masticator space
- Carotid artery
- Prevertebral space
- Mediastinal structures
Genitourinary tract mucosal melanoma staging
- Urinary tract, female and male genital tracts and anorectal melanomas are staged using the cutaneous melanoma staging system; there is no Union for International Cancer Control (UICC) staging criteria for these melanomas
Diagnosis
- Biopsies should attempt to remove the entire lesion, including a depth adequate to determine an accurate Breslow depth; if limited by large size, representative samples should be obtained
- CT or MRI to assess the primary site of disease (Clin Radiol 2011;66:224)
- CT or PET scan to assess for metastases and lymph node involvement
- MRI with contrast is the modality of choice to detect cerebral metastases with higher sensitivity and specificity than contrast enhanced CT (J Neurooncol 1999;44:275)
- CT is the modality of choice for detecting distant metastases
- Lungs and pleura are most frequently affected, followed by the liver
- Lesions may be hypervascular on CT in the arterial phase and hypodense in the portal phase
- Rim enhancement and central necrosis is common
- High signal is often noted on noncontrast T1W liver MRI
- PET CT is 98% sensitive and 94% specific for detecting metastatic melanoma (Radiology 2007;244:566)
Prognostic factors
- Mucosal melanomas have a worse prognosis than cutaneous melanoma
- 5 year survival of mucosal melanoma patients is < 25%; 23% of patients have metastases at the time of diagnosis (Ann Oncol 2017;28:868)
- Mucosal melanoma patients have a median survival of 9 months and the worst prognosis compared with other melanoma subgroups such as uveal, acral, nonacral cutaneous and unknown primary melanoma (Ann Oncol 2017;28:868)
Case reports
- 53 year old man with mucosal melanoma of eustachian tube (J Int Adv Otol 2022;18:455)
- 56 year old postmenopausal woman who presented with intermittent vaginal bleeding and passage of dark clots (Cureus 2020;12:e10536)
- 60 and 67 year old women with malignant amelanotic melanoma of the female genital tract (Melanoma Res 2009;19:267)
- 65 year old with mucosal melanoma of paranasal sinuses (Int J Surg Case Rep 2021;87:106450)
- 80 year old woman with oral mucosal melanoma (J Dent Sci 2020;15:556)
- 84 year old postmenopausal woman with a suspicious vaginal lesion (BMJ Case Rep 2020;13:e232200)
Clinical images
Frozen section description
- Intraoperative consultation is not recommended
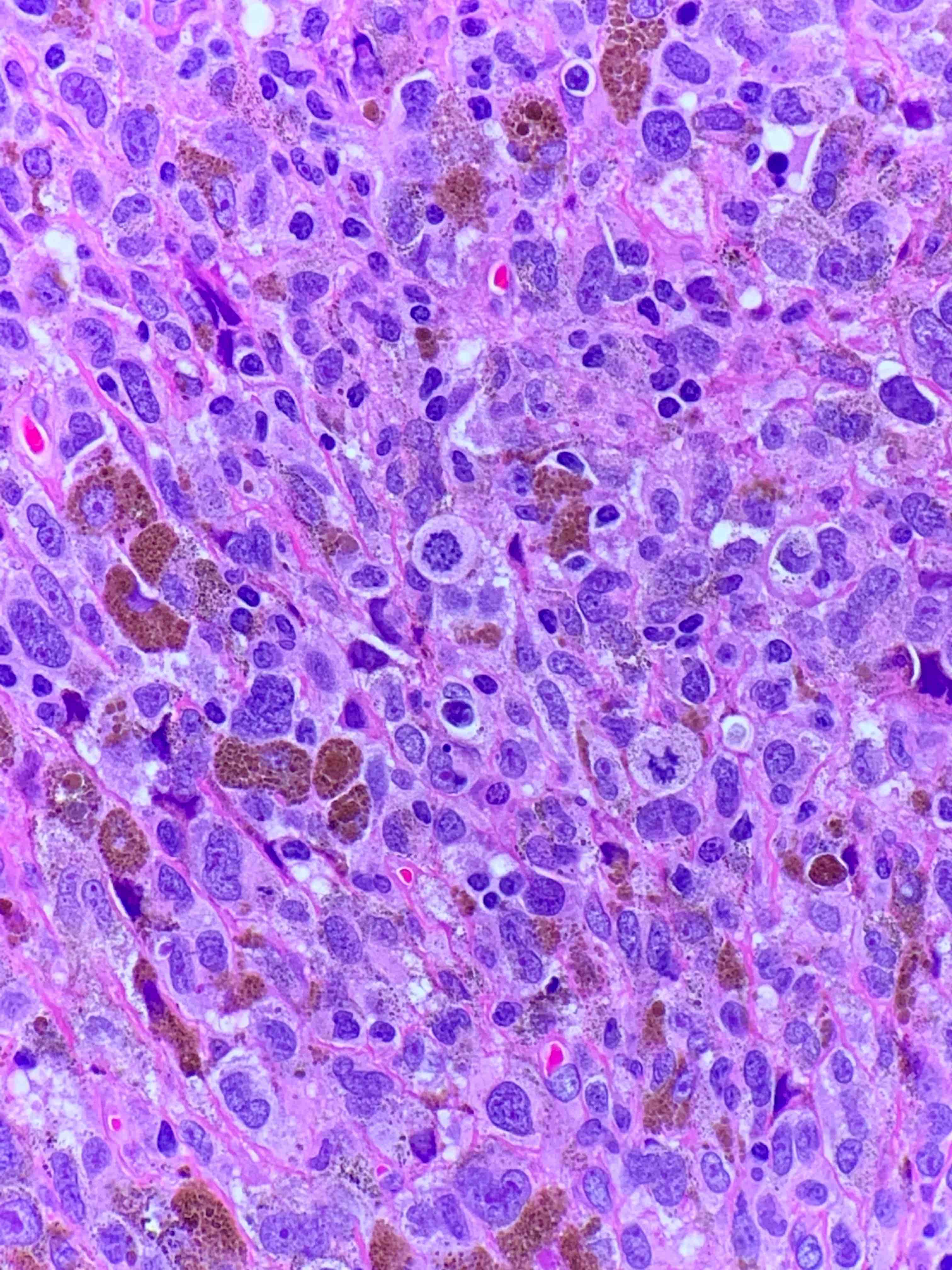
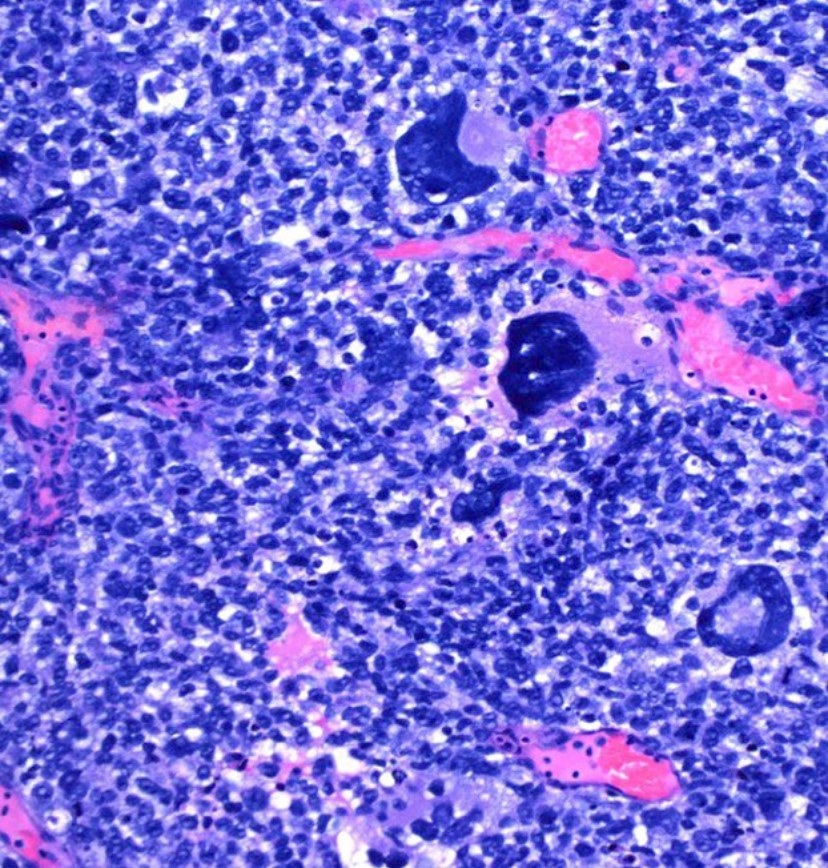
Microscopic (histologic) description
- Arising upon the mucosal surfaces, the intraepithelial component demonstrates a proliferation of melanocytes as single cells and nests, beginning within the basal layer
- Ulceration is frequently encountered
- There is pagetoid involvement of the epidermis
- Lesion is often asymmetric with lack of maturation and cytological atypia
- Cells are often large and epithelioid, with abundant eosinophilic cytoplasm
- Histologic features can vary widely from spindled, epithelioid and pleomorphic to rhabdoid, plasmacytoid and undifferentiated
- Prominent nucleoli and mitotic figures are often seen
- Approximately 50% of mucosal melanomas are amelanotic (or minimal pigmentation) leading to overlapping features and diagnostic challenges in differentiating mucosal melanomas from other small cell / undifferentiated sinonasal tumors (Head Neck Pathol 2017;11:110)
- Reference: Dermatopathology (Basel) 2018;5:41
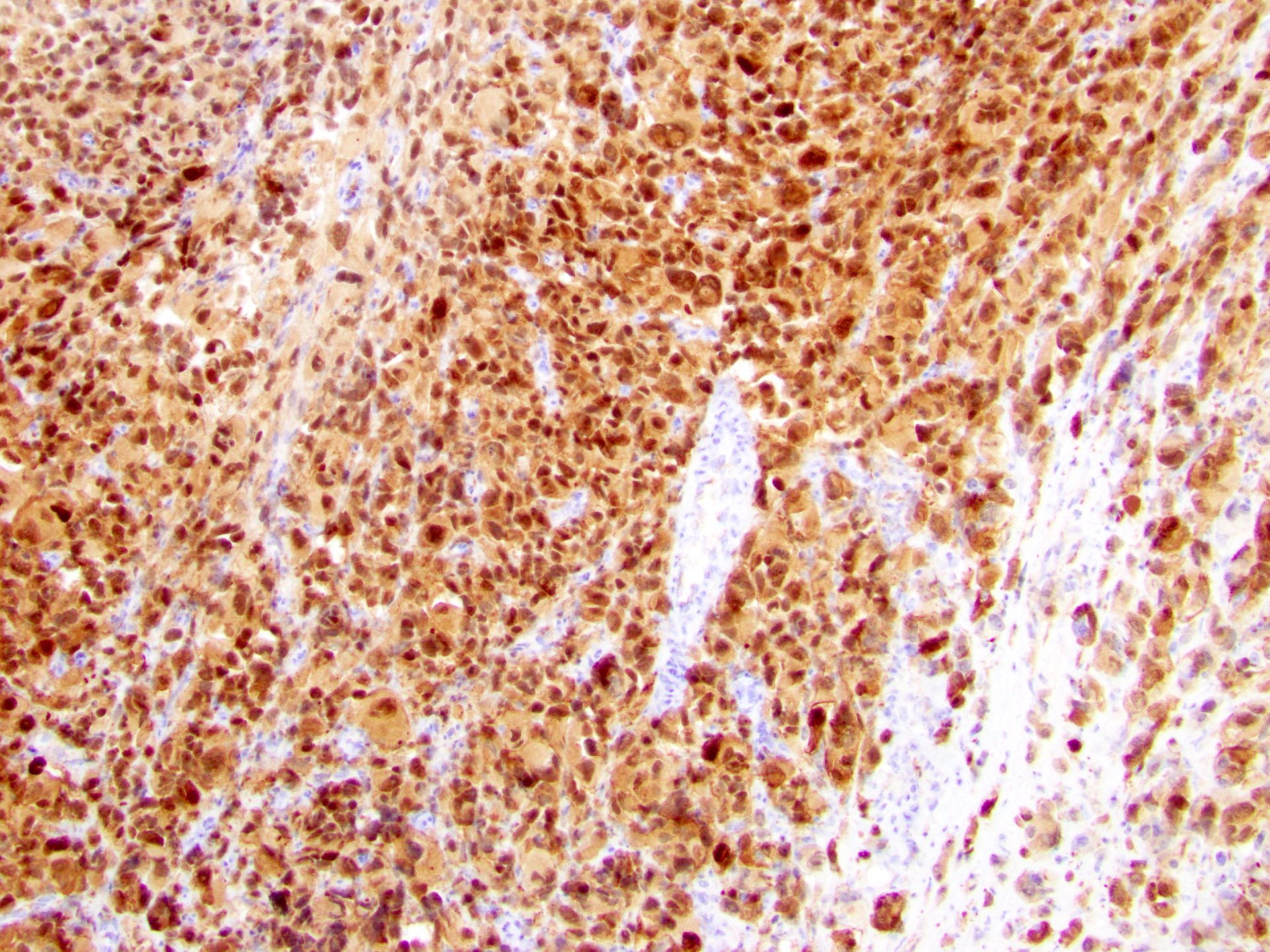
Microscopic (histologic) images
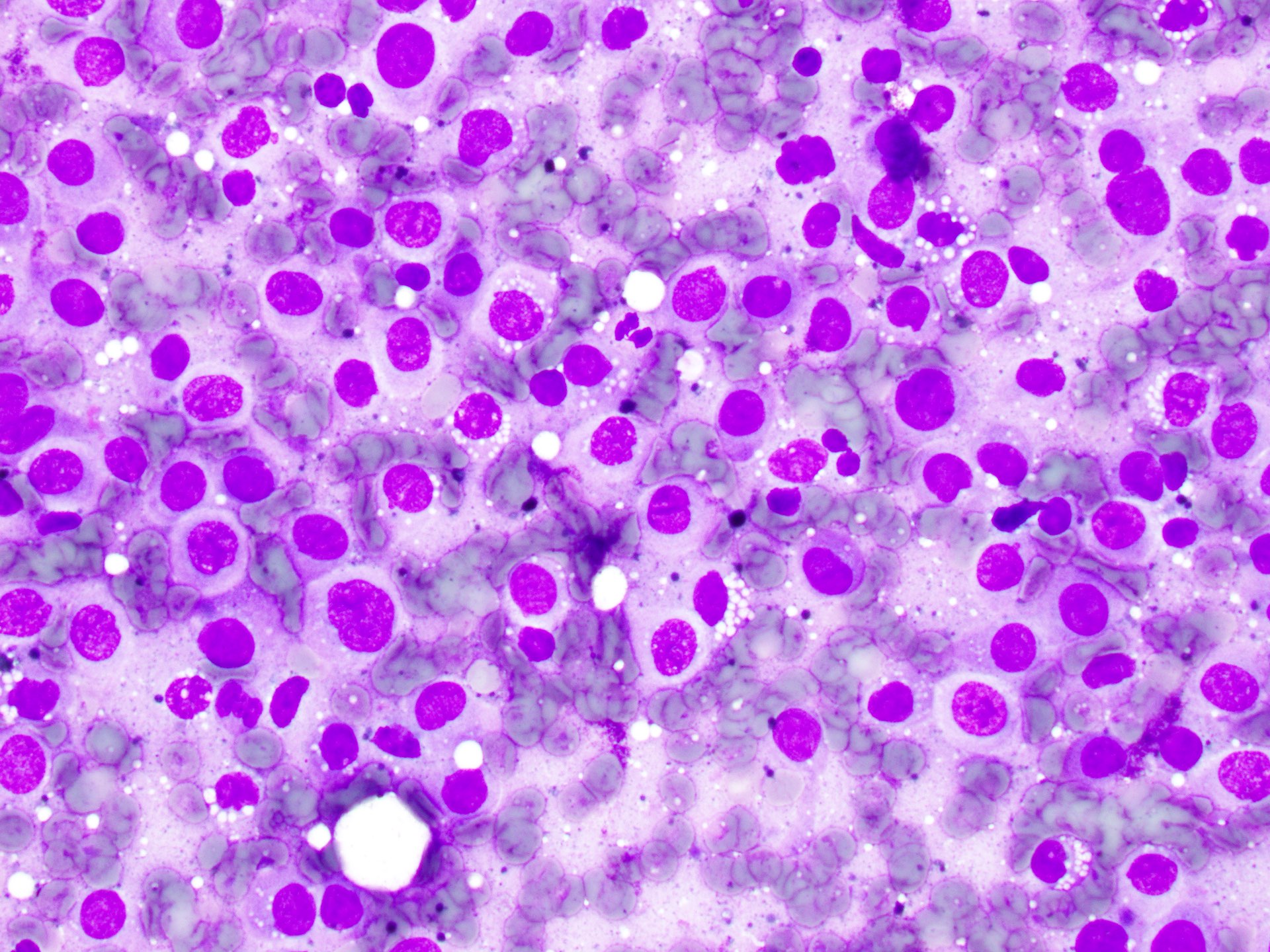
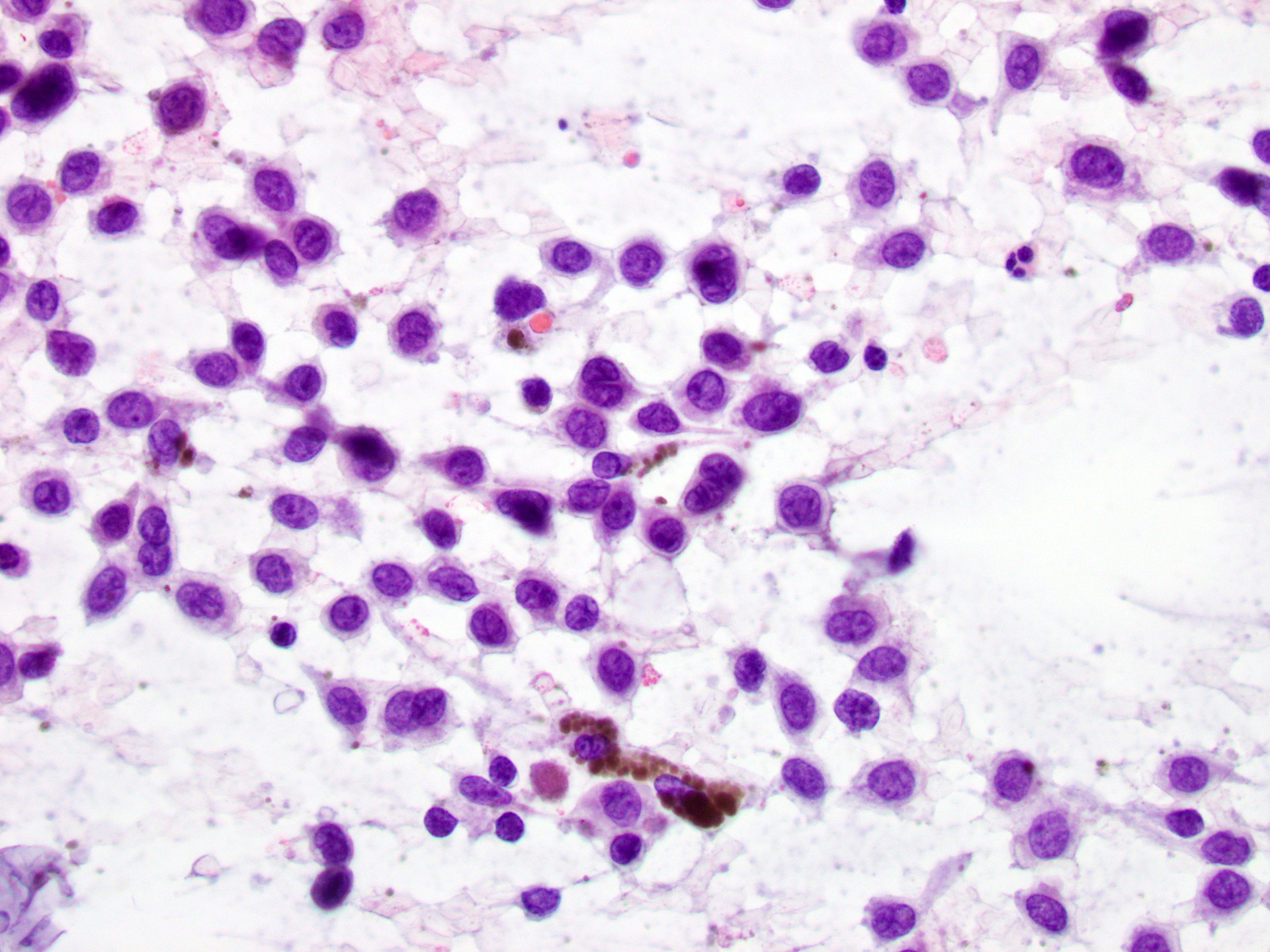
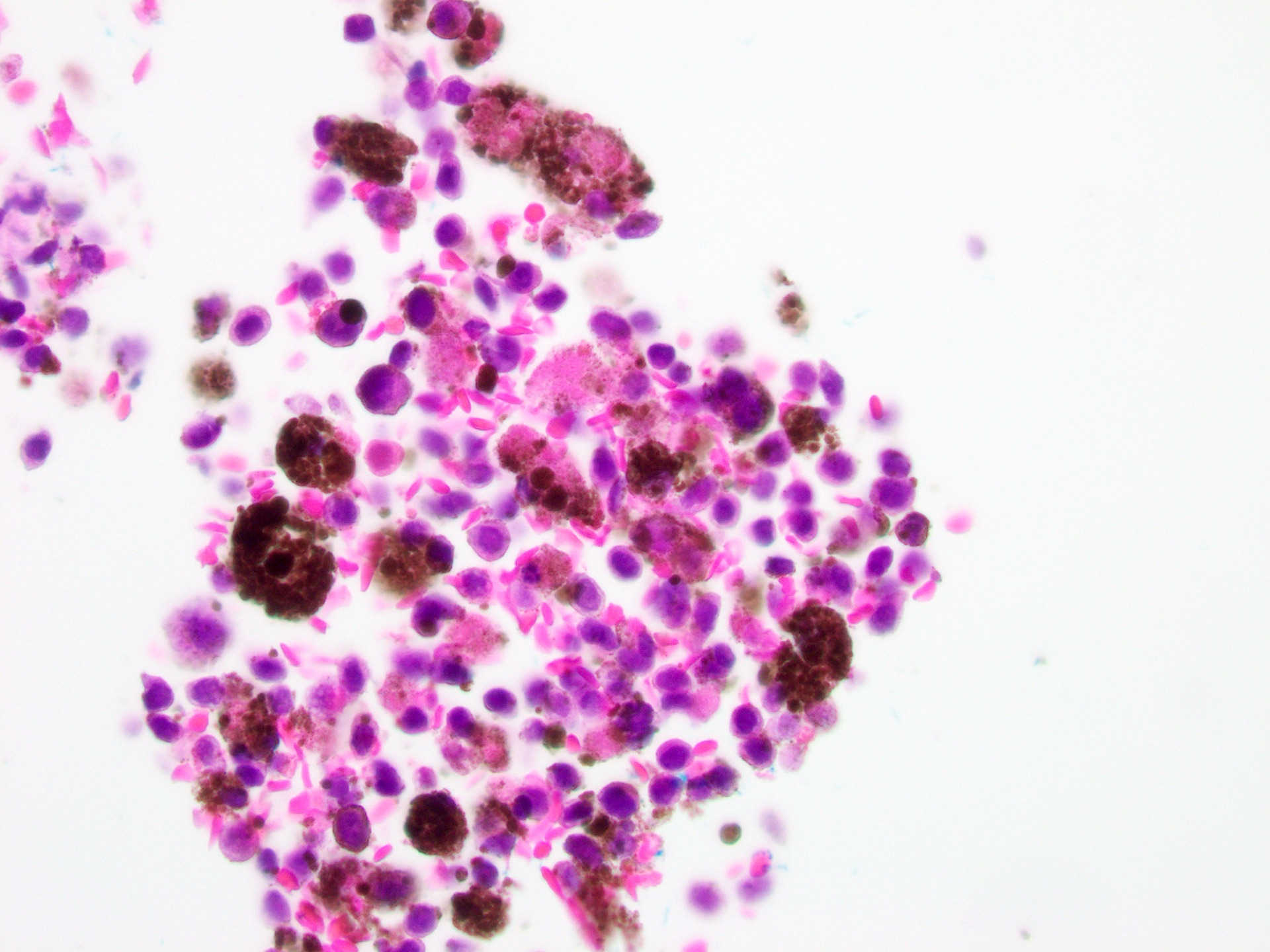
Cytology description
- Limitations:
- Variability in cytological presentation
- Can mimic any malignant tumor
- Cytologic features:
- Discohesive epithelioid, plasmacytoid, spindle cells or giant cells
- Can be multinucleated
- Sometimes microvacuolized cytoplasm
- Dispersed and finely granular pigment
- Variable cell shape and size
- Large irregular nuclei
- Prominent eosinophilic nucleoli
- Nuclear pseudoinclusions
- Melanophages
- Reference: Cancer Cytopathol 2022;130:18
Cytology images
Negative stains
Electron microscopy description
- Melanosomes
- Premelanosomes
- No longer used in clinical practice
Electron microscopy images
Molecular / cytogenetics description
- Significantly mutated genes are NRAS, BRAF, NF1, KIT, SF3B1, TP53, SPRED1, ATRX, HLA-A and CHD8 (Nat Commun 2019;10:3163)
- SF3B1 mutations occur more commonly in female genital and anorectal melanomas
- CTNNB1 mutations implicate a role for WNT signaling defects in the genesis of some mucosal melanomas (Nat Commun 2019;10:3163)
- TERT aberrations and ATRX mutations are associated with alterations in telomere length (Nat Commun 2019;10:3163)
- Oral mucosal melanomas have shown mutations as follows: KIT in 14.6%, BRAF in 7%, NRAS in 5.6% (J Stomatol Oral Maxillofac Surg 2022;123:e425)
Sample pathology report
- Vulva, left, radial vulvectomy:
- Malignant melanoma (see comment)
- Comment:
- Depth: 1.8 cm. (18 mm) (Breslow)
- Level: IV (Clark)
- Ulceration: present
- Mitoses (per mm2): 5
- Regression: not identified
- Angioinvasion: not identified
- Neural invasion: present
- Lymphocytic infiltrate: absent
- Microsatellites: not identified
- Margins: negative
- Lymph nodes: 2/2
- Pathologic stage: pT4b N2
Differential diagnosis
- Benign melanocytic nevus and its histological variants:
- Dysplastic nevus:
- No asymmetry
- No pagetoid spread
- No confluence of expansile nests
- No epidermal consumption / ulceration
- Cytological maturation of dermal melanocytes
- Melanocytic nevi of special sites:
- A small degree of cytological and architectural atypia is acceptable (Am J Dermatopathol 2016;38:867)
- Dysplastic nevus:
- Metastatic melanoma:
- Personal history of melanoma
- Absence of lymphocytic infiltrate
- Absence of junctional component
- Merkel cell carcinoma:
- Neuroendocrine markers (synaptophysin, chromogranin)+
- CK20+ (perinuclear dot-like positivity)
- Anaplastic lymphoma (ALK positive / ALK negative):
Additional references
Board review style question #1
What is the most common location for mucosal melanoma of the head and neck?
- Larynx
- Nasal cavity
- Oral cavity
- Paranasal sinuses
- Pharynx
Board review style answer #1
B. Nasal cavity, followed by paranasal sinuses and oral cavity. About 80% of head and neck mucosal melanomas involve the nasal cavity or septum and maxillary sinus. In the oral cavity, most cases arise in the maxillary gingiva and palate. Tumors arising in other paranasal sinuses, pharynx and larynx are rare.
Comment Here
Reference: Mucosal melanoma (genital, oral, sinonasal)
Comment Here
Reference: Mucosal melanoma (genital, oral, sinonasal)
Board review style question #2
Board review style answer #2
D. 80%. The recurrence rate is 80% in vaginal melanomas and 60% in vulvar melanomas.
Comment Here
Reference: Mucosal melanoma (genital, oral, sinonasal)
Comment Here
Reference: Mucosal melanoma (genital, oral, sinonasal)