Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Salib C, Teruya-Feldstein J. Primary cutaneous diffuse large B cell lymphoma, leg type. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/skintumornonmelanocyticdiffuselargeBcellleg.html. Accessed April 19th, 2024.
Definition / general
- Primary cutaneous large B cell lymphoma (PCLBCL) composed exclusively of centroblasts and immunoblasts, typically arising in the leg
Essential features
- Aggressive B cell neoplasm predominantly affecting older women
- Histologic evaluation shows large neoplastic B cell lymphoma composed exclusively of centroblasts and immunoblasts
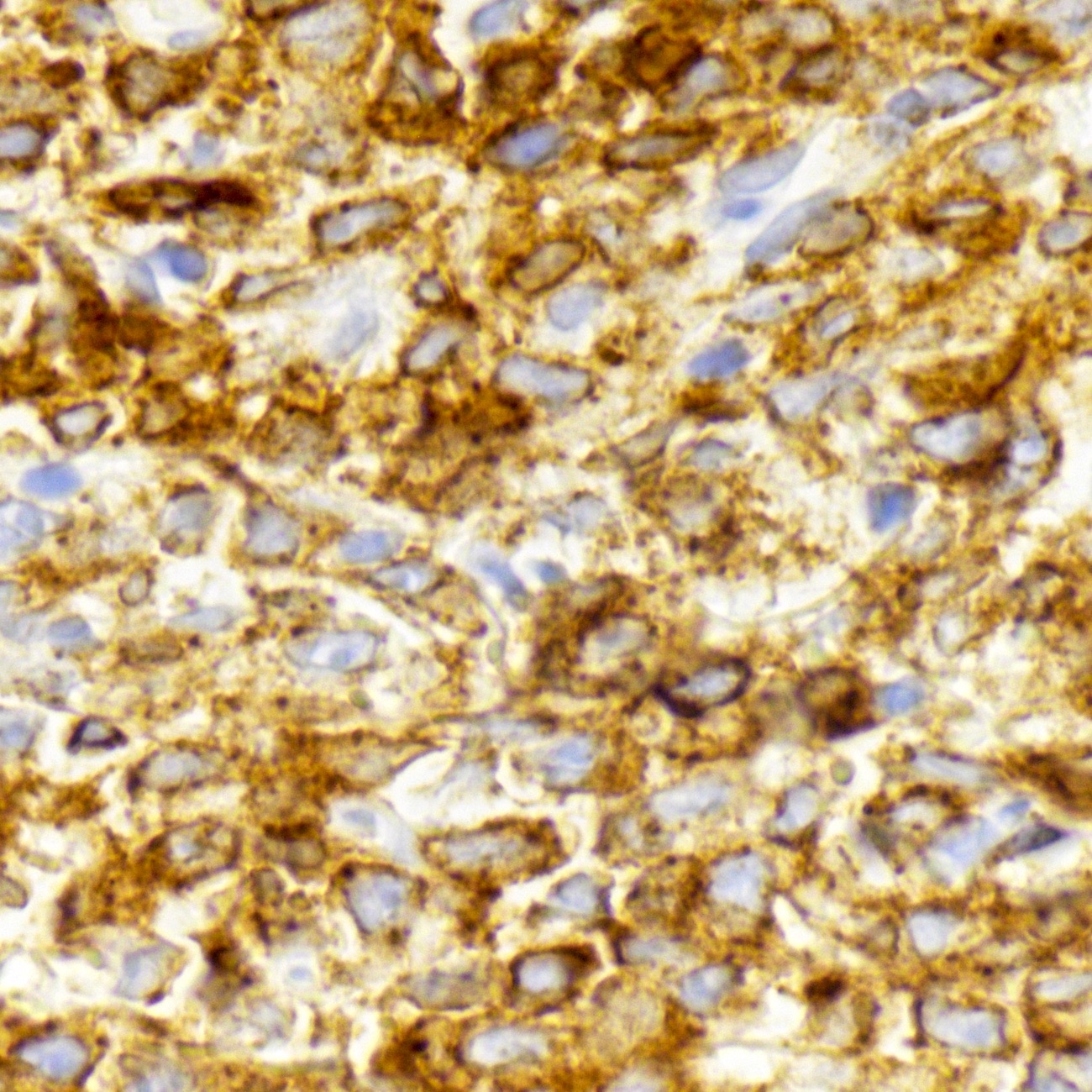
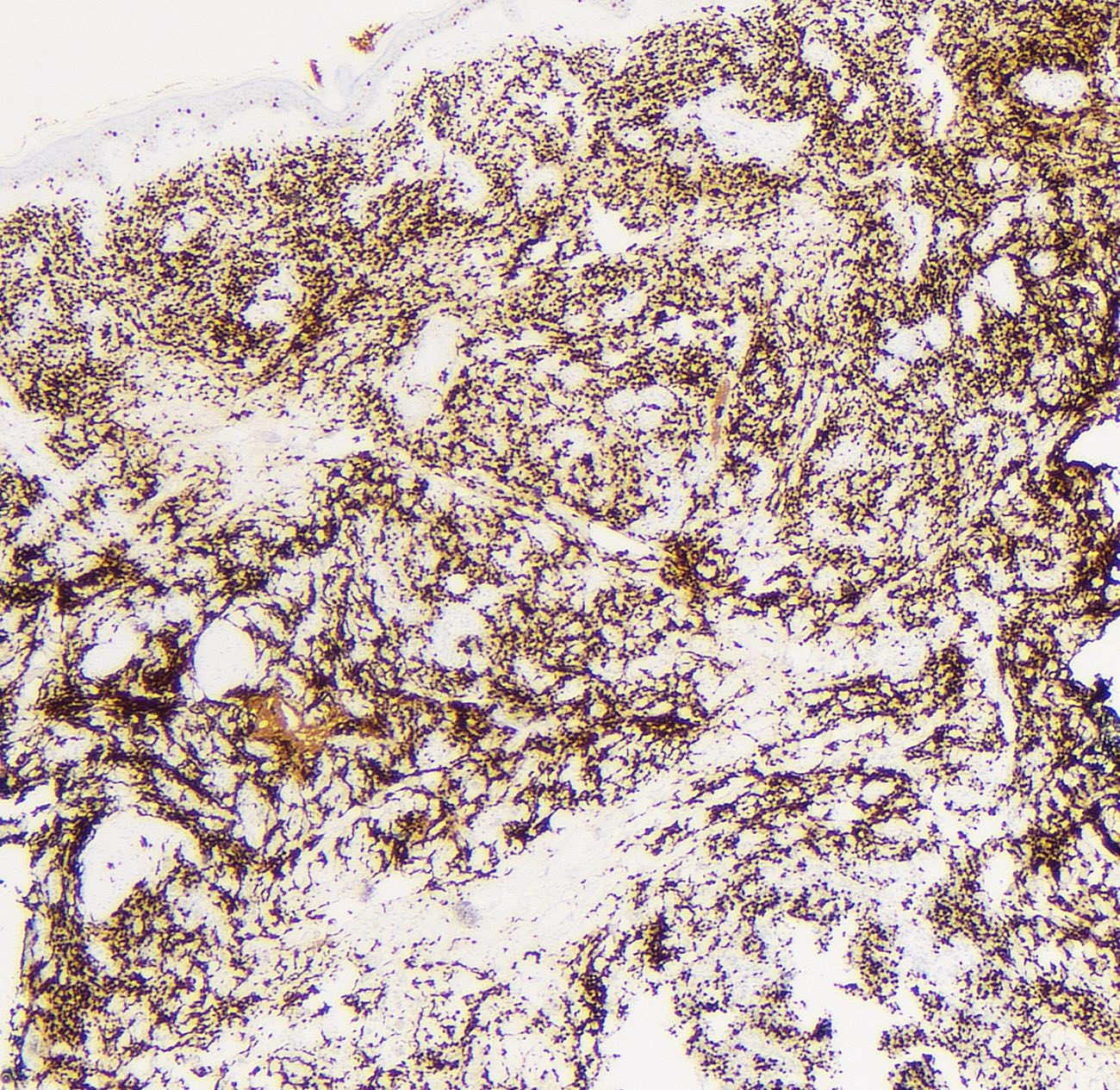
- Neoplastic cells are positive for CD20, CD79a, strong staining for MUM1 and BCL2, while negative for CD10 and EBER
- Treatment involves R-CHOP (rituximab, cyclophosphamide, hydroxydaunomycin, oncovin, prednisone) or local radiotherapy (solitary lesions)
ICD coding
Epidemiology
- 2.6% of all primary cutaneous lymphomas, 20% of all primary cutaneous B cell lymphomas (Arch Dermatol 2007;143:1144)
- M:F = 1:3 (Blood 2019;133:1703)
- Elderly patients, median age is seventh decade of life (Blood 2009;113:5064)
- To date, no reported cases in children (Semin Diagn Pathol 2017;34:85)
Sites
- Unilateral lower limb (80% of cases) (Blood 2019;133:1703)
- 2.0 - 5.0 cm, erythematous to violaceous nodules (Int J Radiat Oncol Biol Phys 2013;87:719)
- Up to 12% of cases arise at other sites, such as the CNS (Blood 2005;106:2491, J Eur Acad Dermatol Venereol 2016;30:186)
Pathophysiology
- Not clearly understood
- B cells undergo aberrant somatic hypermutation; process of affinity maturation of immunoglobulins by somatic hypermutation in regions of the genome that do not encode immunoglobulin genes
- May occur in oncogene containing gene loci
- Loss of high fidelity DNA repair mechanisms
Etiology
- Not clearly understood
- Arises de novo
- Predisposing factors:
- Chronic antigenic stimulation by viral and bacterial infections
- Possible association:
- Hepatitis C virus (HCV) (An Bras Dermatol 2015;90:687)
Clinical features
- Clinically aggressive with a high rate of relapse or dissemination
- Recurrence in 55 - 70% of patients (Semin Diagn Pathol 2017;34:85)
- 5 year overall survival is 50 - 60% (Blood 2019;133:1703)
Diagnosis
- Extensive clinical history (e.g. presence of B symptoms, fever, weight loss, etc.)
- Thorough physical examination
- Tissue biopsy of skin lesion with ancillary testing (flow cytometry, FISH, mutation next generation sequencing studies)
Laboratory
- Complete blood count with differential (CBC w/ diff):
- Lymphocytosis, atypical lymphocytes (if leukemic involvement)
- Comprehensive blood chemistry (CMP)
- Including liver and kidney analysis
- Lactate dehydrogenase (LDH):
- Elevated (indicator of tumor lysis)
- Serum Beta2 microglobulin:
- Variable (indicator of tumor mass) (An Bras Dermatol 2015;90:687)
Radiology description
- FDG avid and hypermetabolic subcutaneous nodules on FDG-PET imaging (Clin Nucl Med 2016;41:65)
Prognostic factors
- Unfavorable prognosis:
- Multiple skin lesions at diagnosis
- Loss of CDKN2A and CDKN2B gene loci on chromosome 9p21.3 due to promotor methylation or gene deletion (up to 67% of cases)
- MYD88 L265P mutation (Am J Surg Pathol 2018;42:1488)
- Favorable prognosis:
- Solitary skin lesion at diagnosis
- Addition of rituximab to CHOP regimen
Case reports
- 41 year old woman with longstanding history of systemic lupus erythematosus presents with an enlarging, well demarcated 3 x 2 cm firm, multilobed, red violaceous, nontender nodule over the left shoulder (J Cutan Med Surg 2016;20:579)
- 72 year old woman with a solitary, 3 cm upper arm nodule for 1 month duration (J Dermatol 2017;44:608)
- 74 year old woman presenting with a painful, left lower leg lesion that was enlarging over 5 months (Cutis 2018;102:E31)
- 82 year old woman with asymptomatic, growing lesions over the past year (Actas Dermosifiliogr 2014;105:78)
- 83 year old man with history of pleomorphic sarcoma treated with radiotherapy, presents with a large, partially ulcerated cutaneous lesion in the region of prior radiation (J Gen Intern Med 2015;30:371)
- 85 year old woman with disseminated solid nodularities (1 - 2 cm) on the face and upper extremities (Am J Dermatopathol 2017;39:e44)
Treatment
- Local radiation or surgery for solitary lesions (Dermatol Clin 2015;33:835)
- R-CHOP: rituximab, cyclophosphamide, hydroxydaunomycin, oncovin, prednisone
- Bortezomib (NFkB inhibitor)
- Ibrutinib (oral tyrosine kinase pathway inhibitor)
Clinical images
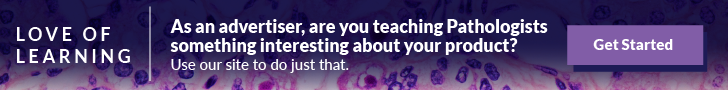
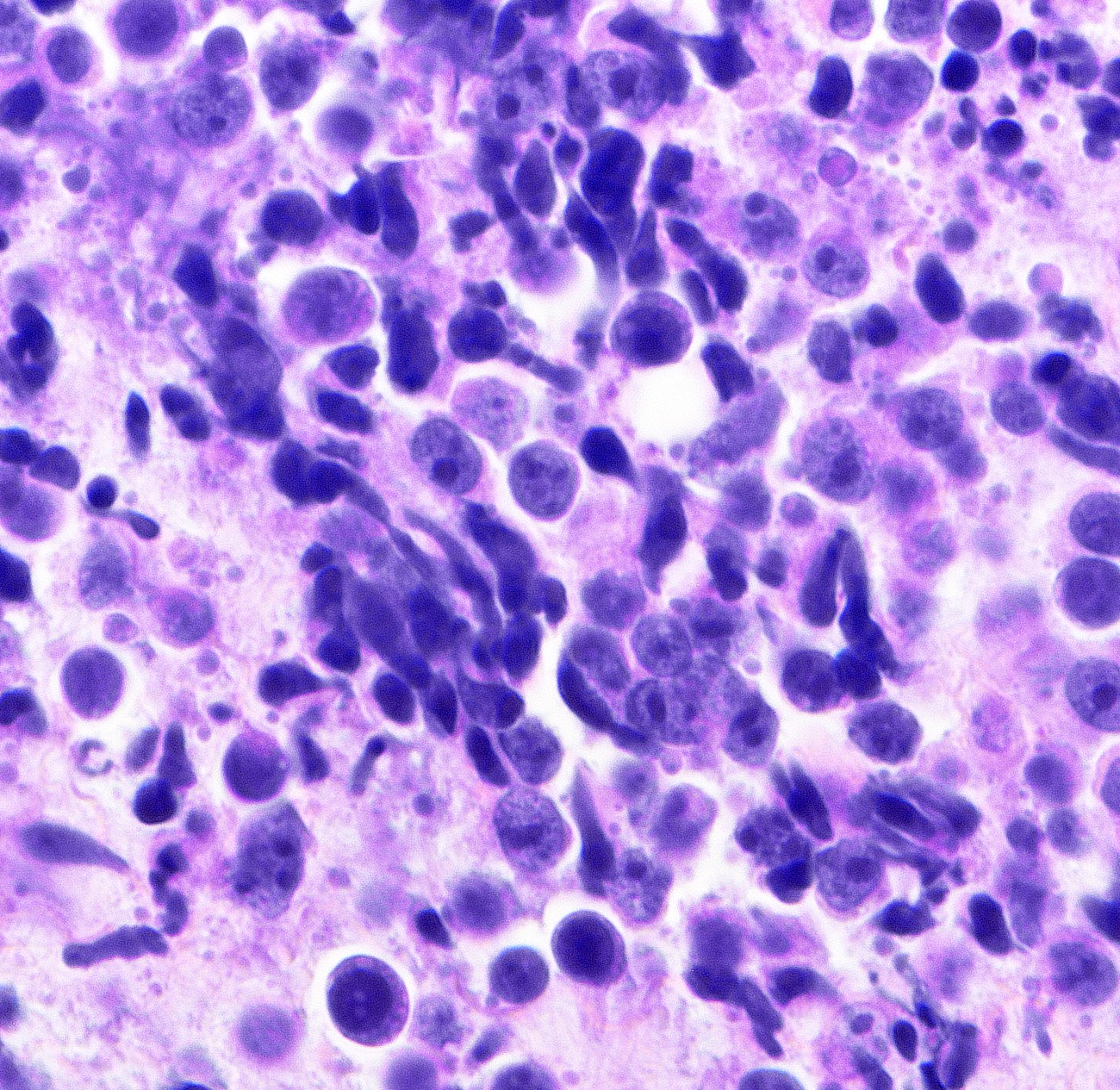
Microscopic (histologic) description
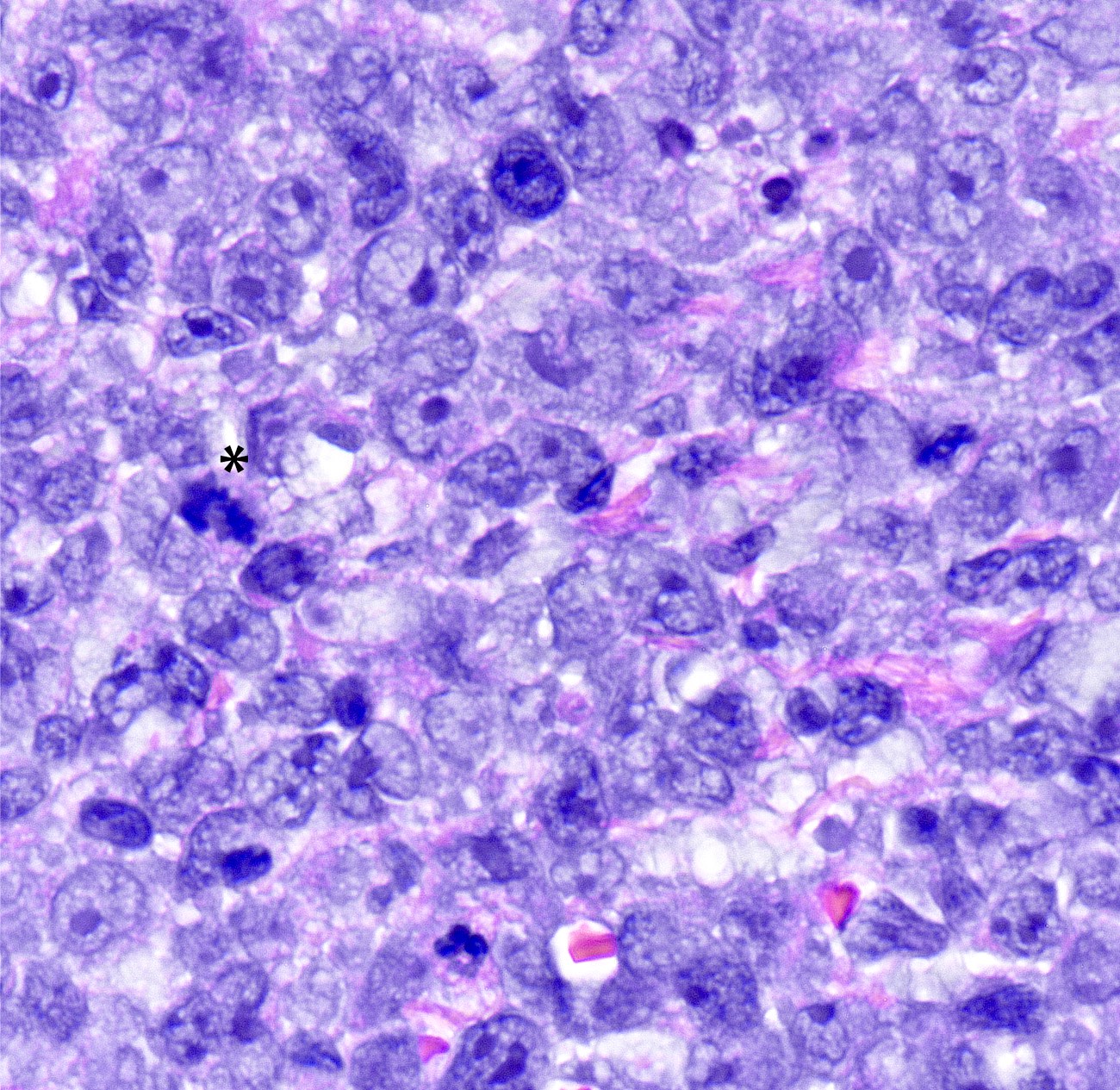
- Superficial and deep dermal involvement by intermediate to large, monotonous, diffuse sheets of centroblasts (round, noncleaved nuclei with vesicular chromatin and one to multiple small nucleoli) and immunoblasts (large, oval nuclei with vesicular chromatin and one prominent nucleolus) (Semin Diagn Pathol 2017;34:85)
- Epidermis spared (may be ulcerated)
- Brisk mitotic activity frequently seen (Histopathology 2019;74:1067)
- Apoptosis, karyorrhexis, cytoplasmic fragments (Am J Surg Pathol 2018;42:1488)
- Small B cells and follicular dendritic cell meshworks (CD21+ / CD35+) are often absent
- Rare reactive, perivascular T cells may be present
Microscopic (histologic) images
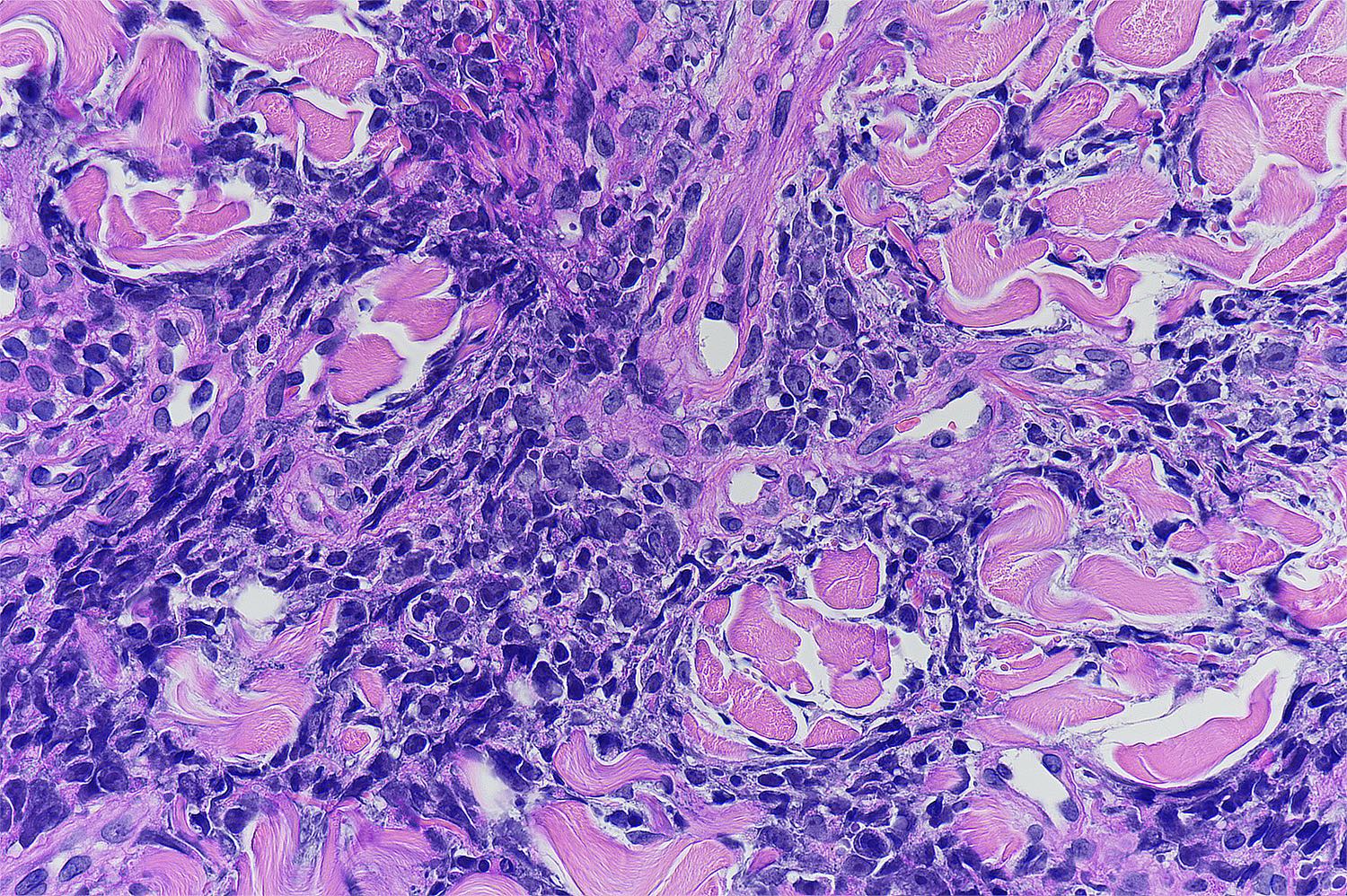
Cytology description
- Neoplastic B cells resemble normal B cells that give rise to them
- Centroblasts and immunoblasts cells
Positive stains
Negative stains
Molecular / cytogenetics description
- Similar gene expression profile as DLBCL, activated B cell-like type (Blood 2005;105:3671)
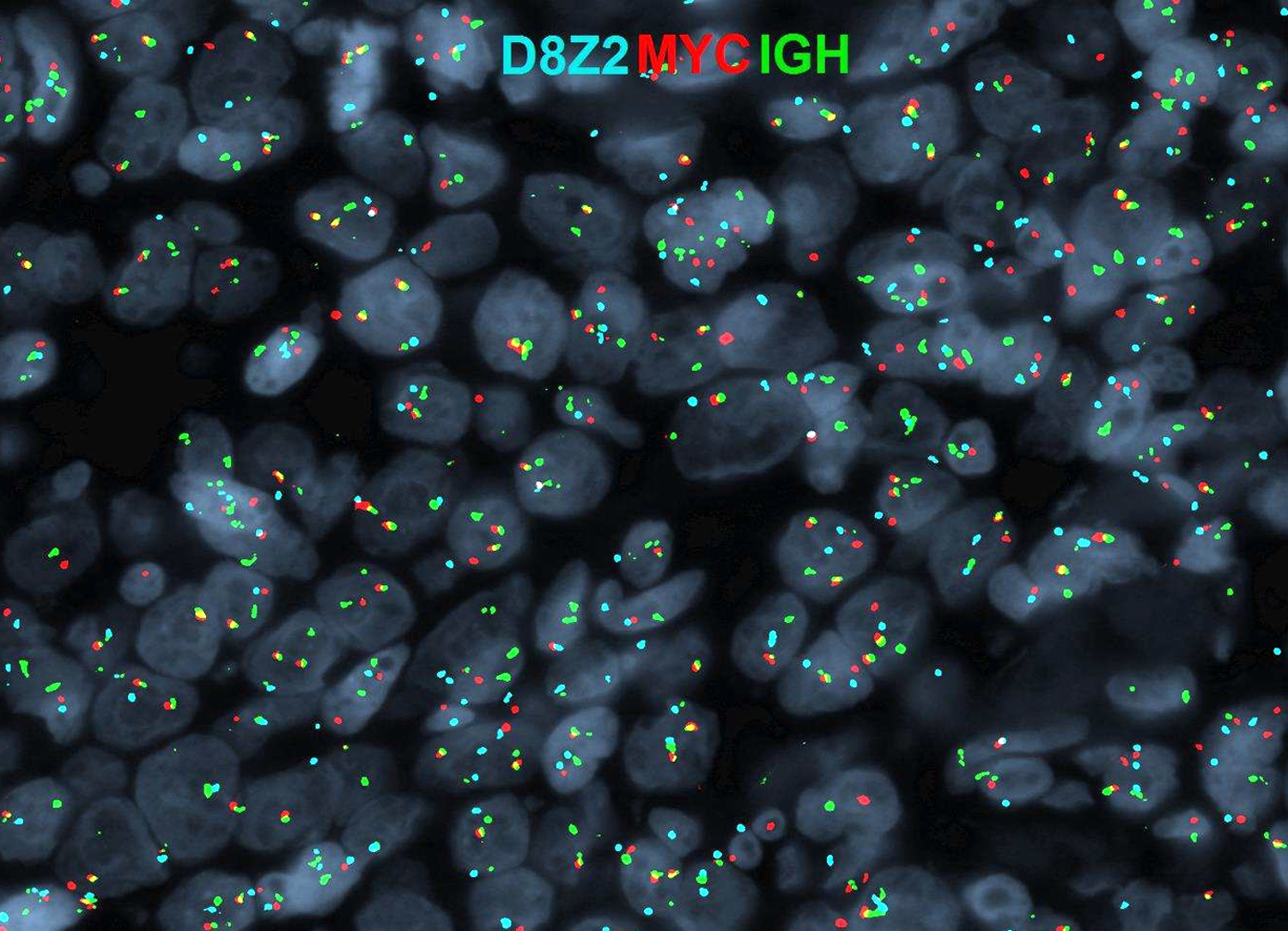
- Interface FISH: translocation of IGH genes with MYC or BCL6
- DNA amplification of 18q21.31-21.33, including BCL2 and MALT1 genes, are identified in 67% of cases by array comparative genomic hybridization and FISH (J Clin Oncol 2006;24:296)
- Loss of CDKN2A and CDKN2B gene loci on chromosome 9p21.3 due to promoter methylation or gene deletion (up to 67% of cases)
- Other mutations: MYD88 L265P (60%), TNFAIP3 (40%), CD79B (20%), CARD11 (10%)
Sample pathology report
- Left thigh, biopsy:
- Primary cutaneous diffuse large B cell lymphoma, leg type; nongerminal center, double expressing (BCL2+ MYC+) involving superficial and deep dermis
- Microscopic description and additional studies:
- H&E sections reveal diffuse sheets of an atypical lymphocyte population infiltrating the dermis while sparing the epidermis. The atypical cells are medium to large in size with moderate amount of cytoplasm, enlarged round nuclei with vesicular chromatin. Some cells show a single prominent nucleolus (immunoblasts-like) while others display multiple smaller nucleoli (centroblasts-like). Brisk mitotic activity is noted (up to 4/hpf). No areas of geographic necrosis is present. No granulomas seen on sections examined.
- Immunochemistry show atypical large lymphoid cells are positive for CD45 (LCA), CD20, CD79a, MUM1, BCL6, BCL2 (> 95%), MYC (weak 40%), MIB1/Ki67 proliferative fraction of 80 - 90% while negative for CD3, CD10, P53 (< 3%), CD99, CD30 (< 1%), CHR, KER903, S100, TTF1, CK20, SYNAP.
- In situ hybridization for EBV encoded viral RNA (EBER) is NEGATIVE.
- PAS, GMS and AFB stains are negative for microorganisms.
- Karyotype: nuc ish(BCL6x2),(D8Z2x2)(MYC,IGH)x3(MYC con IGHx2),(IGHx3,BCL2x2),(MYCx2)(5'MYC sep 3'MYCx1).
- Report: Multiplex FISH x4 was performed on paraffin embedded tissue: nuc ish(BCL6x2) [191/200], (D8Z2x2)(MYC,IGH)x3(MYC con IGHx2) [130/200], (IGHx3,BCL2x2) [123/200], (MYCx2)(5'MYC sep 3'MYCx1) [124/200].
- Interpretation: Interphase FISH results are consistent with a 65% of cells showing MYC-IGH [t(8;14)] fusion POSITIVE signal pattern. Cells were IGH-BCL2 fusion negative and BCL6 (3q27) gene rearrangement was NOT detected. Although the hallmark of Burkitt lymphoma is the presence of MYC-IGH rearrangement, approximately 10% of DLBCL cases will contain a MYC rearrangement and an aggressive clinical course (Arch Pathol Lab Med 2015;139:602).
- Next generation mutation studies show:
- Biomarker findings
- Microsatellite status - MS-stable
- Tumor mutational burden - TMB-intermediate (7 Muts/Mb)
- CDKN2A/B loss
- ETV6 rearrangement exon 4
- MED12 R817H
- MLL2 H313fs*20
- MYD88 L265P
- PRDM1 splice site 291+1G > T
Differential diagnosis
- Primary cutaneous follicle center lymphoma:
- Marginal zone lymphoma:
- Mantle cell lymphoma, blastoid variant:
- Primary cutaneous T cell lymphoma:
- EBV+ large B cell lymphomas of skin:
- Positive for EBV
- Lymphomatoid granulomatosis (LyG):
- Positive for EBV
- Plasmablastic lymphoma:
- Positive for EBV, may lack B cell markers
- Intravascular DLBCL:
- Intravascular neoplastic cells rather than diffuse infiltration
- Skin involvement of B cell acute lymphoblastic lymphoma (B-ALL):
- Venous leg ulcers:
- Lower extremity ulcerated lesions with mixed inflammatory infiltrate, no evidence of clonality
- Granuloma annulare:
- Dermal lymphophistiocytic infiltrate with mucin deposition, no overlying skin changes, associated with diabetes
- Necrobiosis lipoidica:
- Palisading, necrobiotic granuloma with histiocytes, eosinophils and giant cells in dermis and subcutaneous fat, plasma cells almost always present
- Sarcoidosis:
- Nonnecrotizing granulomatous reaction with lymphocytes, eosinophils and plasma cells
- Erythema nodosum:
- Perivascular and periadnexal inflammatory infiltrate (lymphocytes, histiocytes, neutrophils) with nonnecrotizing granulomatous inflammation (giant cells)
- Lupus erythematosus
- Leprosy (lepromatous):
- Macrophage localized in ill defined dermal aggregates, few lymphocytes, caused by Mycobacterium leprae
- Drug reaction
Additional references
Board review style question #1
- A 78 year old woman with no known clinical history presents with a solitary, violaceous, 4.3 cm papule on her left shin. Patient denies any history of recent travel, allergies or sexually transmitted infections. Biopsy reveals sheets of large round cells with vesicular chromatin and 1 to multiple prominent nucleoli infiltrating the dermis. The tumor cells are positive for CD20, MUM1 and BCL6, while negative for EBV, CD4, CD5, CD30 and ALK. What additional immunohistochemical stain will help differentiating this diagnosis from primary cutaneous follicle center lymphoma?
- BCL1 (cyclin D1)
- BCL2
- CD19
- CD23
- CD79a
Board review style answer #1
B. BCL2. The clinical, morphologic and immunohistochemical presentation are most suggestive of a large B-cell lymphoma. Differential considerations include de novo diffuse large B-cell lymphoma, leg type vs. secondary involvement of DLBCL from a different site (less likely, given no prior history of lymphoma) vs. primary cutaneous follicle center lymphoma (PCFCL). Primary cutaneous follicle center lymphoma are essentially follicular lymphomas arising from/associated with skin hair follicles, with neoplastic B-cell expressing germinal center markers (i.e. CD10, BCL6). Unlike follicular lymphomas however, the classic t(14;18)(BCL2-IGH) translocation is seen in only 20-30% of cases (Mod Pathol 2001;14:913) and generally lack expression of BCL2 protein. These two markers (CD10+, BCL2-) can be used to differentiate PCFCL from DLBCL, leg type, which is typically CD10-, BCL2+.
Comment Here
Reference: Diffuse large B cell lymphoma - leg
Comment Here
Reference: Diffuse large B cell lymphoma - leg
Board review style question #2
- Which of the following factors can be used as a predictor of an unfavorable prognosis for the above lymphoma entity?
- EBV positivity
- Gender
- Lack of MYD88 L265P mutation
- Presence of multifocal lesions
- Presence of t(14;18)(q32;q21) translocation
Board review style answer #2