Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Endoscopic findings | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Samra H, Mostafa M. Peptic duodenitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/smallbowelduodenitis.html. Accessed April 19th, 2024.
Definition / general
- Histologic findings indicative of duodenal mucosa injury as a result of chronic exposure to increased gastric secretion
Essential features
- Primarily involves proximal duodenum
- Histologic features include gastric foveolar metaplasia and Brunner gland hyperplasia
- Usually mild and regresses with treatment
Terminology
- Also termed chronic nonspecific duodenitis
ICD coding
- ICD-10: K29.80 - duodenitis without bleeding
Epidemiology
- Median age: 58 years (Hum Pathol 2010;41:1593)
- Foveolar metaplasia can be seen in up to 26.3% of patient population (Lab Invest 2016;96 Suppl 1:187A)
Sites
- Duodenum, usually proximal segment
Pathophysiology
- Chronic exposure of the duodenal mucosa to excessive gastric acidity in proportion to duodenal bicarbonate contents, resulting in injury to the lining mucosa (Monogr Pathol 1990;31:69)
Etiology
- Medications (in particular NSAIDs) (Aliment Pharmacol Ther 2012;36:48)
- Helicobacter pylori infection (though recent data suggests H. pylori might not be implicated as much as it was believed) (Hum Pathol 2010;41:1593, Lab Invest 2016;96 Suppl 1:187A)
- Idiopathic (Aliment Pharmacol Ther 2013;38:946)
Clinical features
- May be asymptomatic (incidental finding) or cause dyspepsia, abdominal pain, hematemesis
- In advanced cases: symptoms related to gastric outlet obstruction or acute abdominal pain (clinical features of peritonitis) secondary to duodenal perforation
Diagnosis
- Endoscopy with biopsy
Laboratory
- Negative celiac sprue serology (antitissue transglutaminase, endomysial antibodies, deamidated gliadin peptide)
Endoscopic findings
- Mucosal erythema
- Mucosal nodularity (Mod Pathol 2005;18:1134)
- Mucosal erosion and ulceration
Prognostic factors
- Good prognosis as most cases regress with treatment
Case reports
- 56 year old man with foveolar gastric metaplasia of atypical appearance (J Med Case Rep 2016;10:355)
- 72 year old man with duodenal obstruction secondary to Brunner gland hyperplasia (Pathologica 2017;109:414)
- 80 year old man with carcinoma arising from gastric foveolar metaplasia in the duodenum after 9 years of observation (Clin J Gastroenterol 2018;11:391)
Treatment
- Stop the offending medication
- Proton pump inhibitors
- Treat underlying infection, like H. pylori (Histopathology 2006;48:417)
- Surgical intervention for perforated peptic duodenitis or gastric outlet obstruction
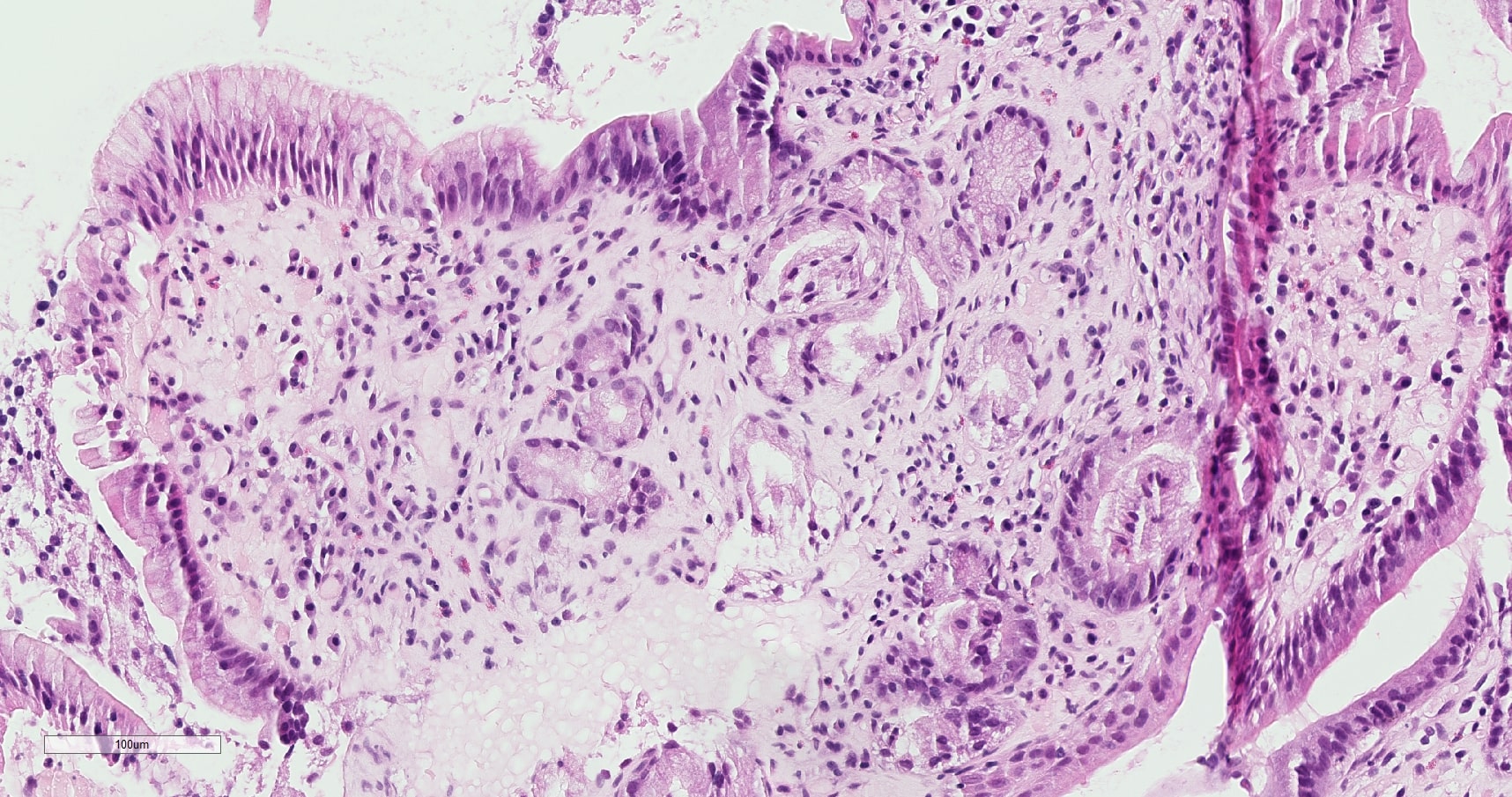
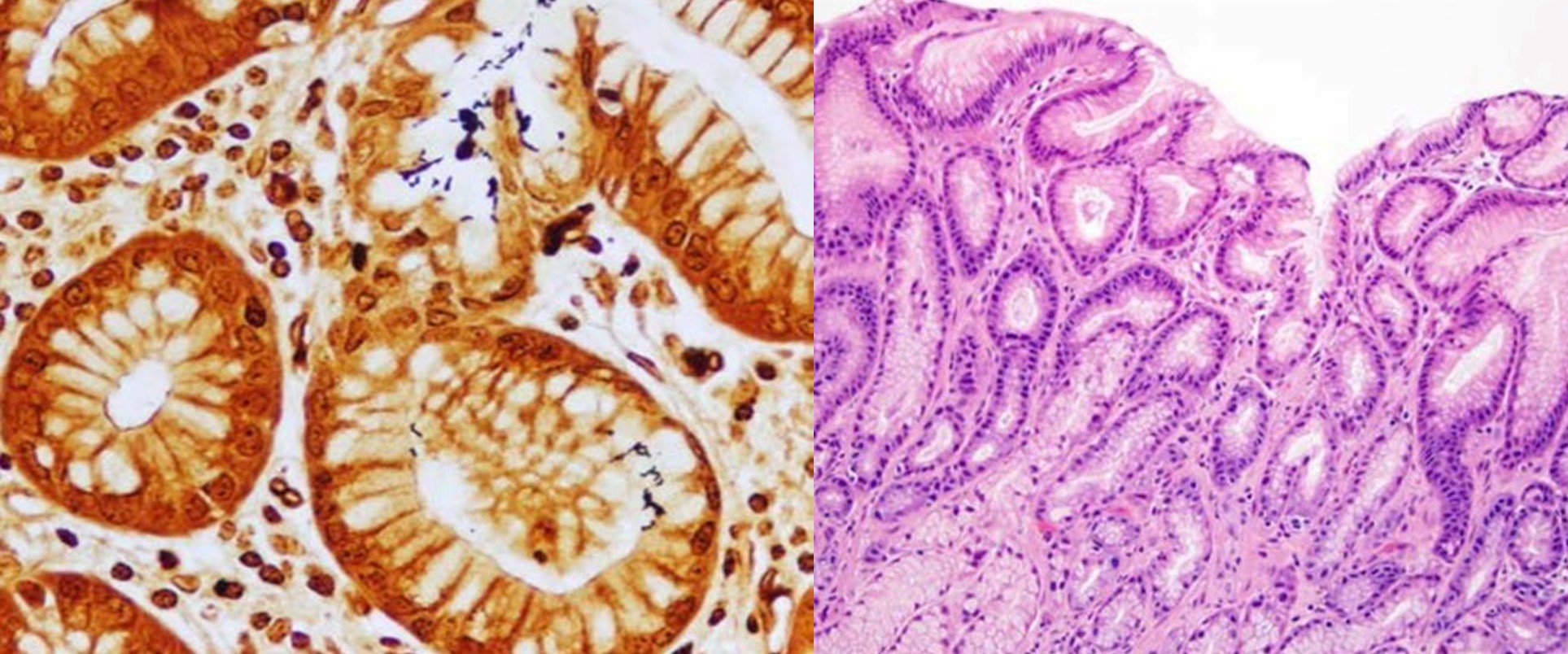
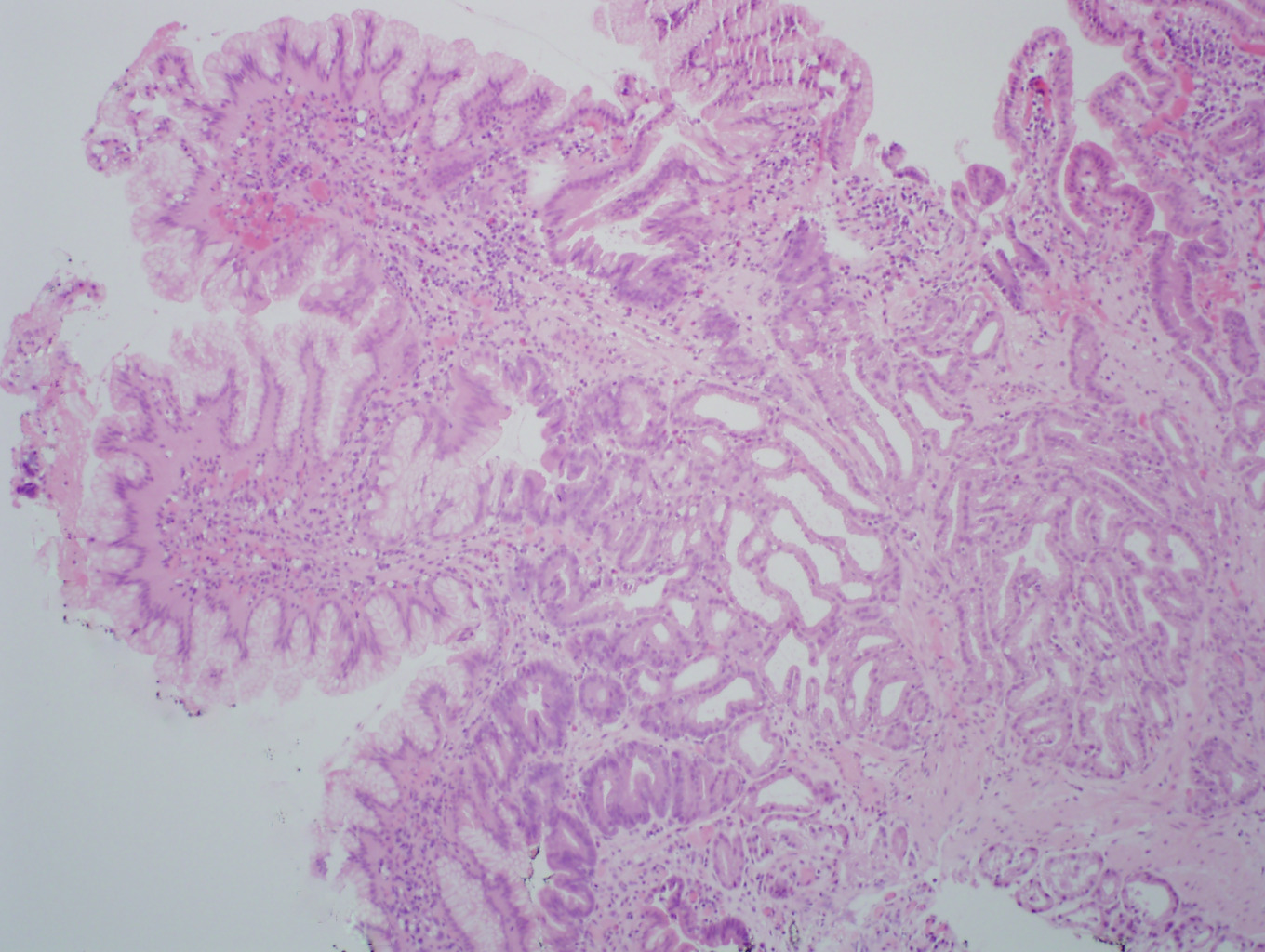
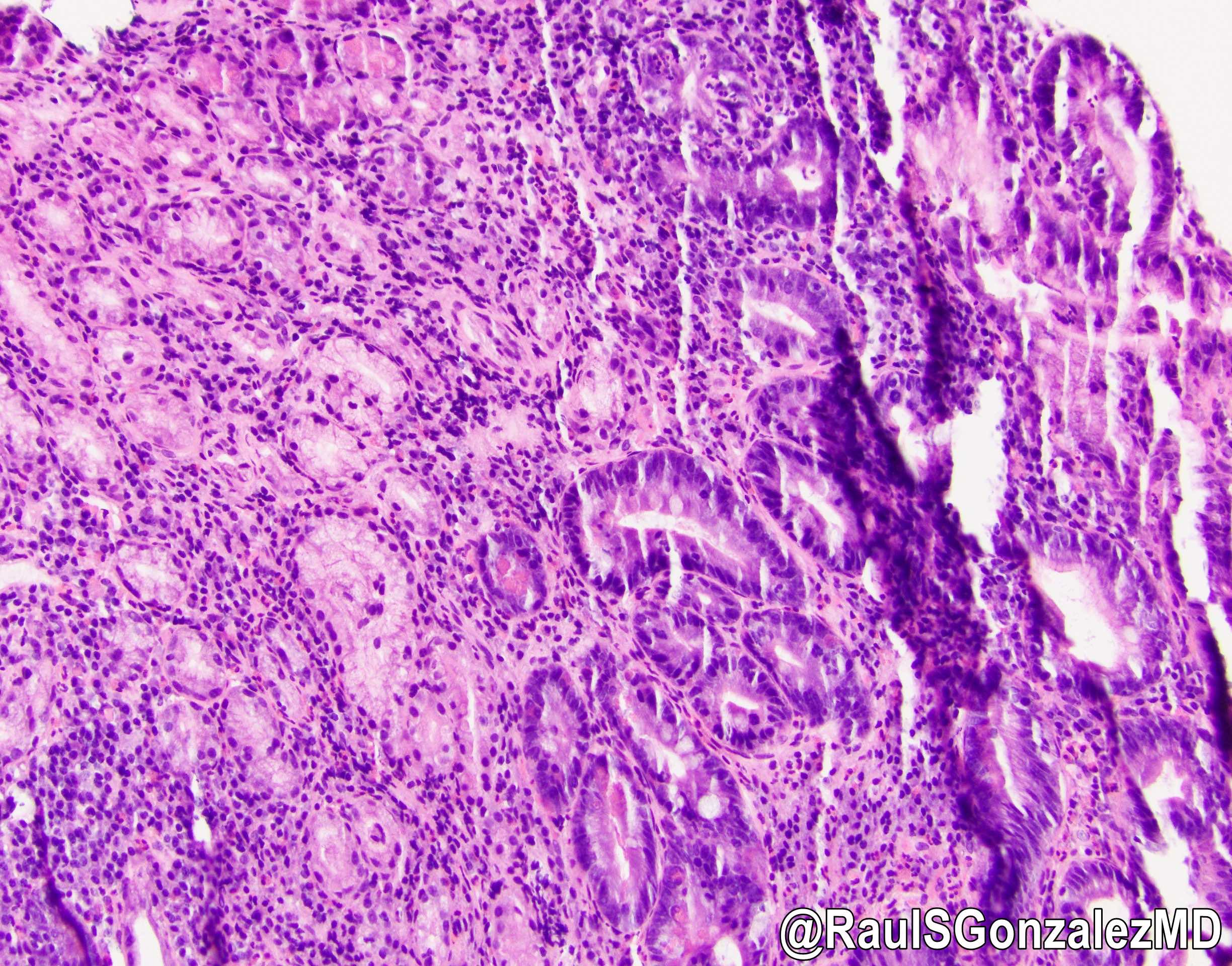
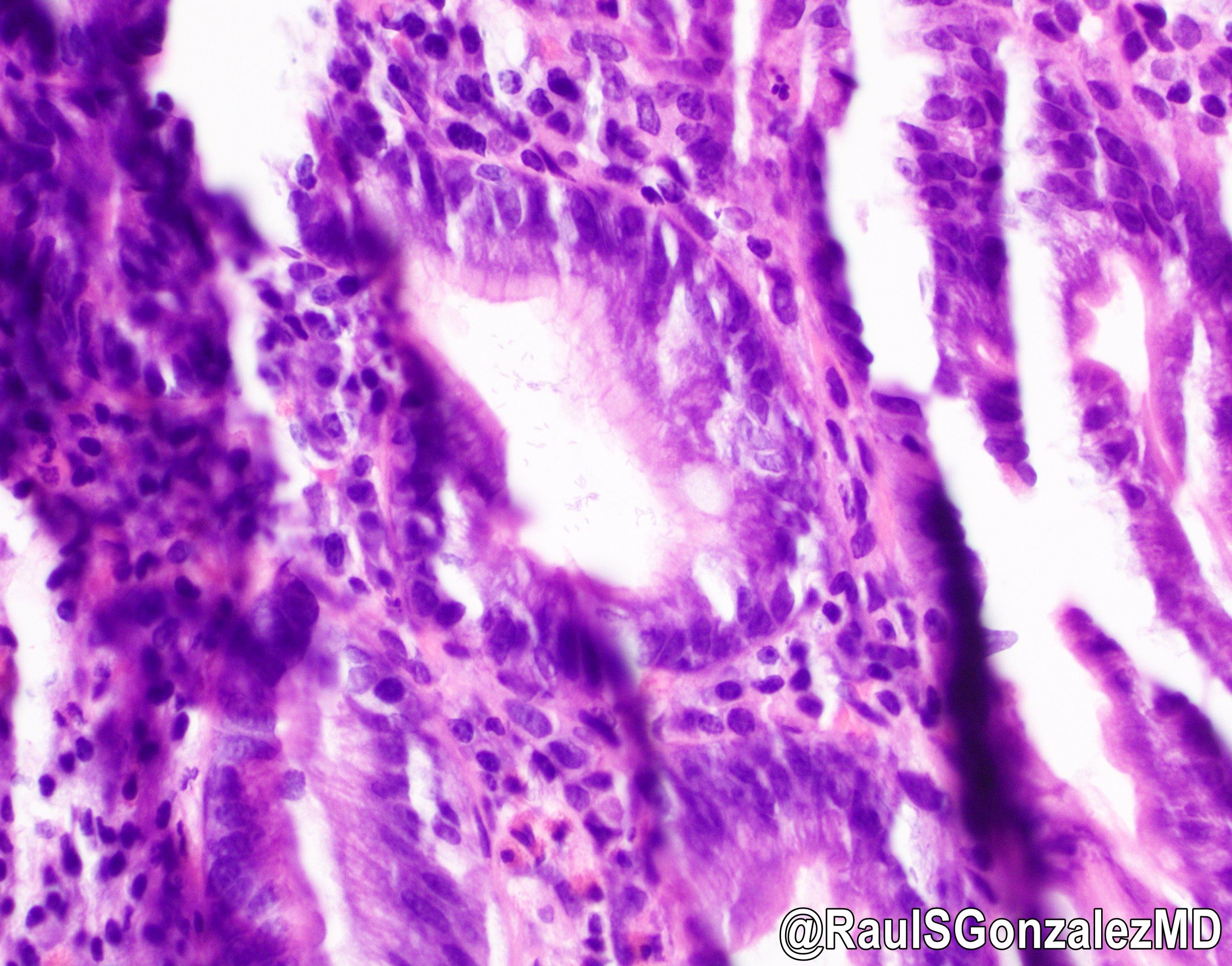
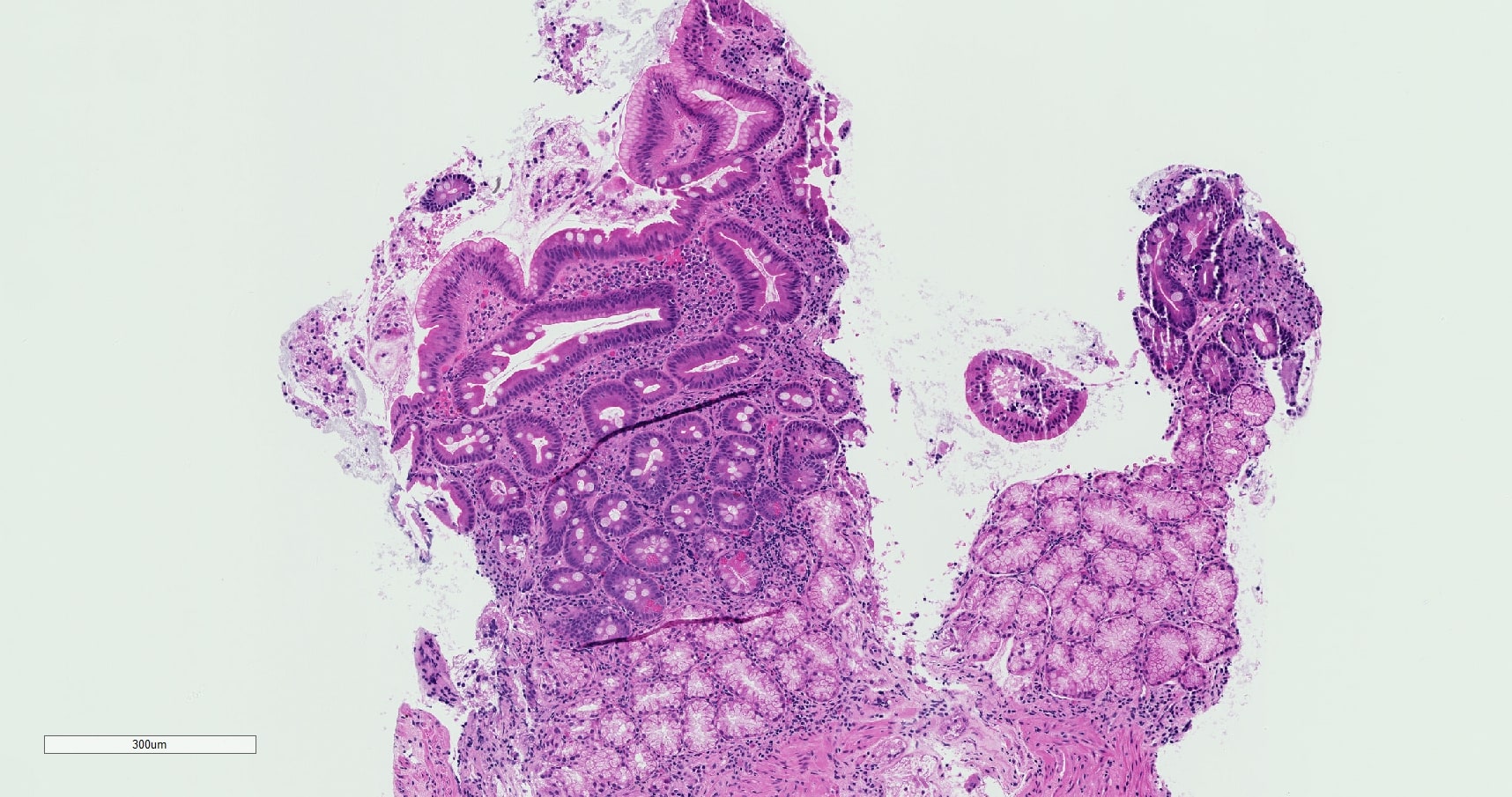
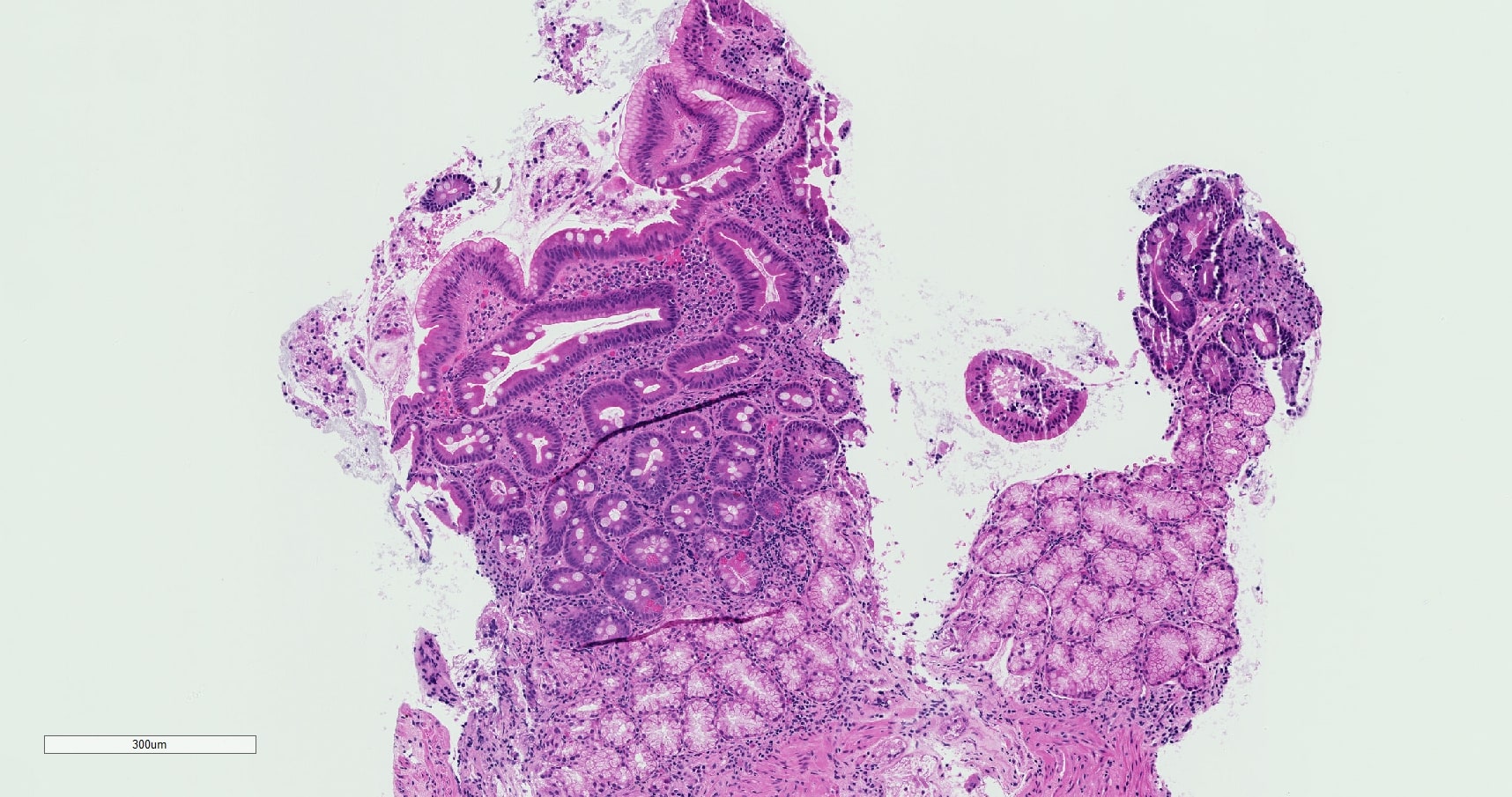
Microscopic (histologic) description
- Foveolar metaplasia of the surface duodenal epithelium
- Brunner gland hyperplasia (Brunner glands seen above the muscularis mucosae)
- Expansion of the lamina propria by mixed inflammatory cell infiltrate, including few neutrophils that usually do not infiltrate the epithelium
- Mildly increased intraepithelial lymphocytes, usually corresponding to Marsh 1 lesion (Mod Pathol 2005;18:1134)
- Mild villous blunting can be seen (World J Gastroenterol 2005;11:686)
- Severe cases may show mucosal erosion, ulceration or regenerative changes, like mucin depletion, nuclear hyperchromasia and increased mitotic activity
- H. pylori very rarely present in metaplastic epithelium
Microscopic (histologic) images
Sample pathology report
- Duodenum (D1 / D2), biopsy:
- Duodenal mucosa with preserved villous architecture and gastric metaplasia, suggestive of peptic injury
Differential diagnosis
- Celiac sprue:
- Positive celiac serology
- Marked increased intraepithelial lymphocytes and prominent villous blunting
- Improvement with gluten elimination
- May also show concomitant peptic injury / gastric metaplasia
- Crohn’s disease:
- Nonnecrotizing granulomas
- Involvement of other locations in the gastrointestinal tract
Additional references
Board review style question #1
Which of the following histologic findings are most likely to be encountered in peptic duodenitis?
- Cryptitis and crypt abscess formation
- Lamina propria expansion and nonnecrotizing granulomas
- Marked intraepithelial lymphocytosis and moderate villous blunting
- Scattered lymphoid follicles in the lamina propria
- Surface foveolar metaplasia and Brunner gland hyperplasia
Board review style answer #1
E. Surface foveolar metaplasia and Brunner gland hyperplasia
Comment Here
Reference: Peptic duodenitis
Comment Here
Reference: Peptic duodenitis
Board review style question #2
Regarding peptic duodenitis, which one of the following is true?
- Affects primarily duodenal mucosa distal to ampulla of Vater
- Always associated with Helicobacter pylori gastritis
- Histologic findings result from excessive bile reflux
- Medication is always a culprit
- Presents with mild symptoms and regresses with treatment
Board review style answer #2
E. Presents with mild symptoms and regresses with treatment
Comment Here
Reference: Peptic duodenitis
Comment Here
Reference: Peptic duodenitis