Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Molecular / cytogenetics images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Uddin Z, Ud Din N. Angiomatoid fibrous histiocytoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/softtissuefhangiomatoid.html. Accessed April 18th, 2024.
Definition / general
- Rare mesenchymal tumor of borderline malignant potential and uncertain histogenesis, characterized by solid nodules of epithelioid to spindled cells, blood filled pseudoangiomatous spaces, a fibrous pseudocapsule and a lymphoplasmacytic cuff toward the periphery
Essential features
- Syncytial-like sheets of epithelioid to ovoid cells
- Pseudoangiomatous blood filled spaces
- Peripheral fibrous pseudocapsule and lymphoid tissue
Terminology
- Originally described as angiomatoid malignant fibrous histiocytoma by Franz M. Enzinger in 1979 (Cancer 1979;44:2147)
ICD coding
- ICD-O: 8836/1 - angiomatoid fibrous histiocytoma
- ICD-11: 2F7C & XH9362 - neoplasms of uncertain behavior of connective or other soft tissue & angiomatoid fibrous histiocytoma
Epidemiology
- Relatively rare entity, comprising 0.3% of all soft tissue tumors
- More common in the first 2 decades of life without any sex predilection
- Has been reported in a wide age range, extending from congenital presentation to the ninth decade (Arch Pathol Lab Med 2015;139:674)
- Patients with extrasomatic soft tissue sites show higher mean age
Sites
- Superficial soft tissues of extremities, followed by the trunk and the head and neck
Pathophysiology
- Not known
Etiology
- Originally described as a fibrohistiocytic tumor; however, WHO classification has kept it in the list of tumors of uncertain differentiation since no convincing ultrastructural or immunohistochemical evidence has been found to support this theory (Arch Pathol Lab Med 2015;139:674)
Clinical features
- Predominantly presents as a slow growing, nontender, superficial, subcutaneous nodule in extremities, followed by the trunk and the head and neck
- In the extremities, almost 66% of these tumors affect lymph node bearing regions, such as popliteal fossa, antecubital fossa, axilla, inguinal area and neck
- Nonsomatic soft tissue sites of origin are increasingly being reported, including mediastinum, lung, bone, brain, gynecological tract, omentum and retroperitoneum (Mod Pathol 2011;24:1560, Br J Neurosurg 2021;35:233)
- Often clinically mistaken with a vascular neoplasm or a hematoma
- Constitutional symptoms are uncommon and are linked to cytokine production by tumor
Diagnosis
- Diagnosis can be challenging due to nonspecific clinical, histological and immunohistochemical features compounded by rarity of this tumor
- Key diagnostic histological features include:
- Thick, fibrous pseudocapsule
- Dense pericapsular cuff of lymphoplasmacytic cells
- Presence of pseudoangiomatous / pseudovascular spaces
- Syncytial proliferation of bland epithelioid to spindle shaped cells
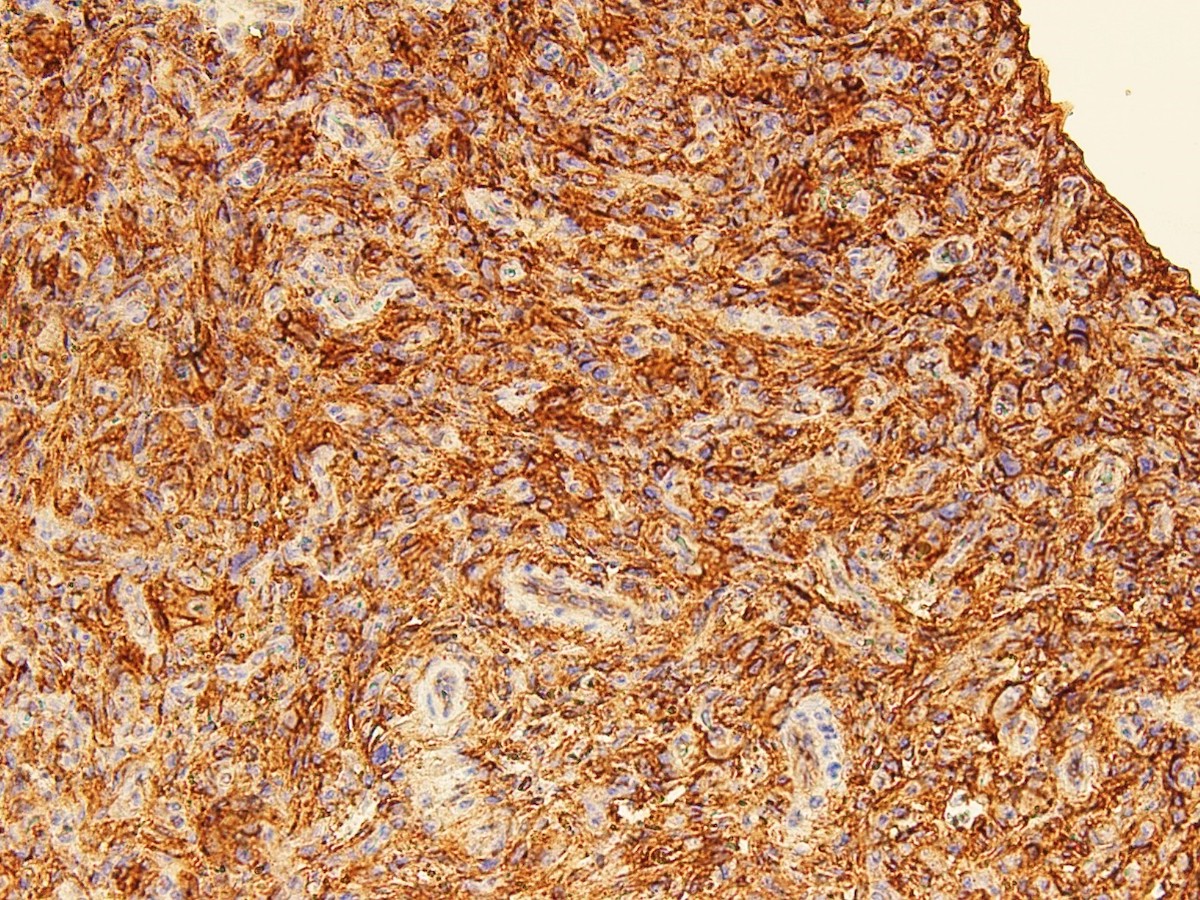
- Supportive immunohistochemical features: desmin+, CD99+, EMA+, CD68+
- Reference: Arch Pathol Lab Med 2015;139:674
Radiology description
- Circumscribed, lobulated mass
- Cystic change with multiple areas of fluid - fluid levels
- Signal characteristics and enhancement are presumed to be variable subject to the cellular, myxoid, collagenous and vascular content of the lesion
- Heterogeneous intermediate to low signal intensity in T1 weighted image (T1WI) and heterogeneous high signal intensity in T2 weighted / short T1 inversion recovery (STIR) with the hemorrhagic component
- After administration of IV contrast, enhancement of the soft tissue component within the lesion is seen with no enhancement of cystic components (Cureus 2021;13:e16465)
Prognostic factors
- Morphological features of this tumor cannot predict the outcome
- Most behave in an indolent fashion
- Local recurrences have been reported in up to 15% of cases
- Most recurrent cases show positive margins, deeper presentations and extrasomatic locations
- < 5% metastasize, mostly to lymph nodes with exceptional cases of lung, liver and brain metastasis (BMC Musculoskelet Disord 2017;18:31)
Case reports
- 7 year old boy presented with angiomatoid fibrous histiocytoma and Castleman disease (Pediatr Blood Cancer 2021;68:e28590)
- 8 year old boy with left thigh angiomatoid fibrous histiocytoma having arterial vascular channels within the tumor and feeding branch from the left profunda femoris artery (BJR Case Rep 2020;7:20190069)
- 10 year old boy and 11 year old girl with intracranial angiomatoid fibrous histiocytoma presented with history of seizures (World Neurosurg 2020;143:398)
- 10 year old boy with subcutaneous pleomorphic variant of angiomatoid fibrous histiocytoma with multiplication of EWSR1::CREB1 fusion gene (Pathol Oncol Res 2012;18:545)
- 13 year old girl with angiomatoid fibrous histiocytoma on left angle of mandible (Int J Paediatr Dent 2006;16:363)
- 20 year old man presented with angiomatoid fibrous histiocytoma in the cervical spinal canal (Br J Neurosurg 2020 Dec 7 [Epub ahead of print])
- 50 year old woman with a falcine angiomatoid fibrous histiocytoma having diffuse rhabdoid morphology and focal high mitotic activity mimicking rhabdoid meningioma (Brain Tumor Pathol 2021;38:138)
Treatment
- Wide local excision with follow up is the treatment of choice
- Irresectable and recurrent cases may be treated by adjuvant radiotherapy and or chemotherapy (Arch Pathol Lab Med 2015;139:674)
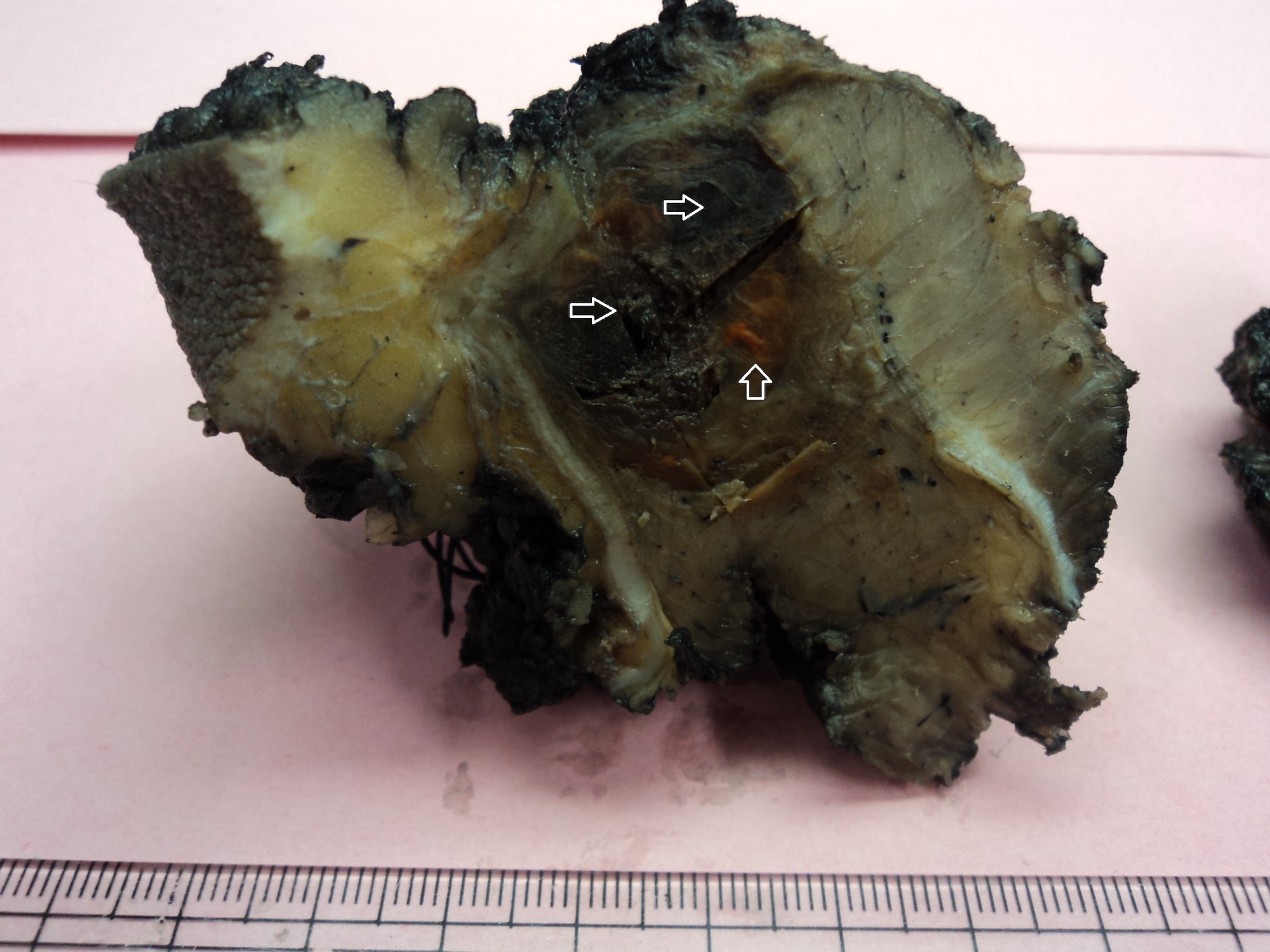
Gross description
- Nodular and multicystic masses having grayish white to yellow cut surface with hemorrhagic areas / blood filled cysts
- Median size is 2 cm (size range: 0.7 - 12 cm)
- Reference: BMC Musculoskelet Disord 2017;18:31
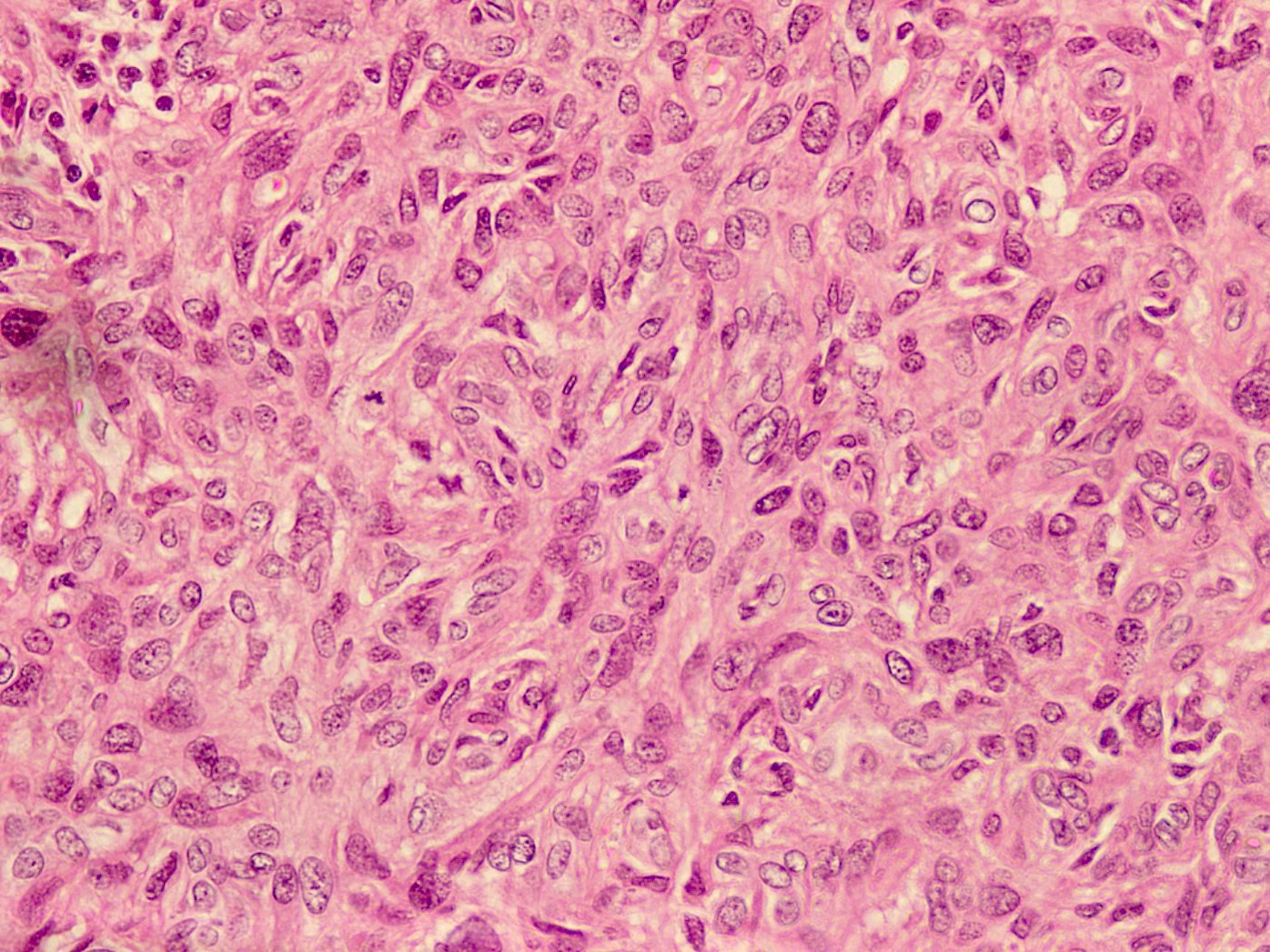
Microscopic (histologic) description
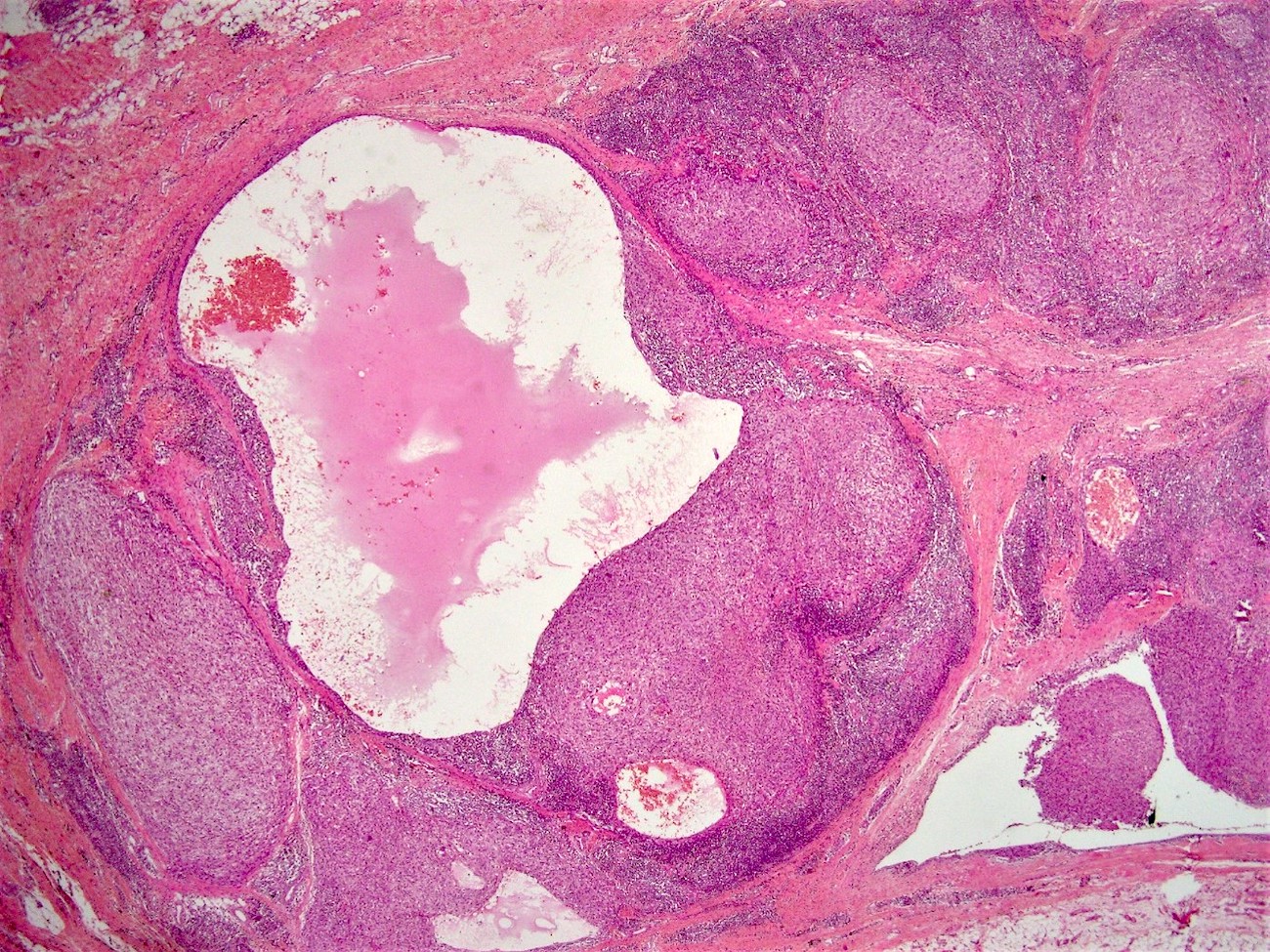
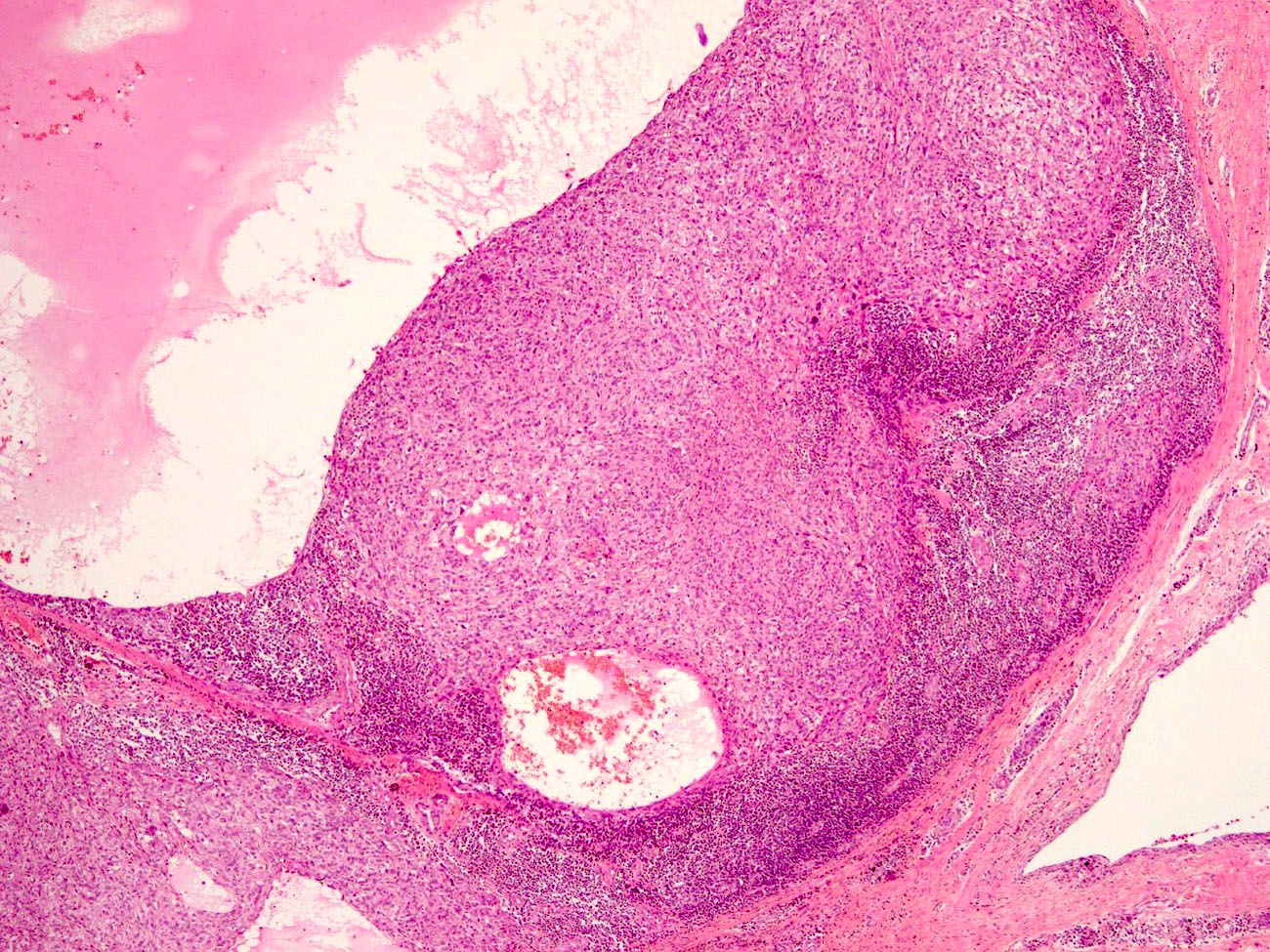
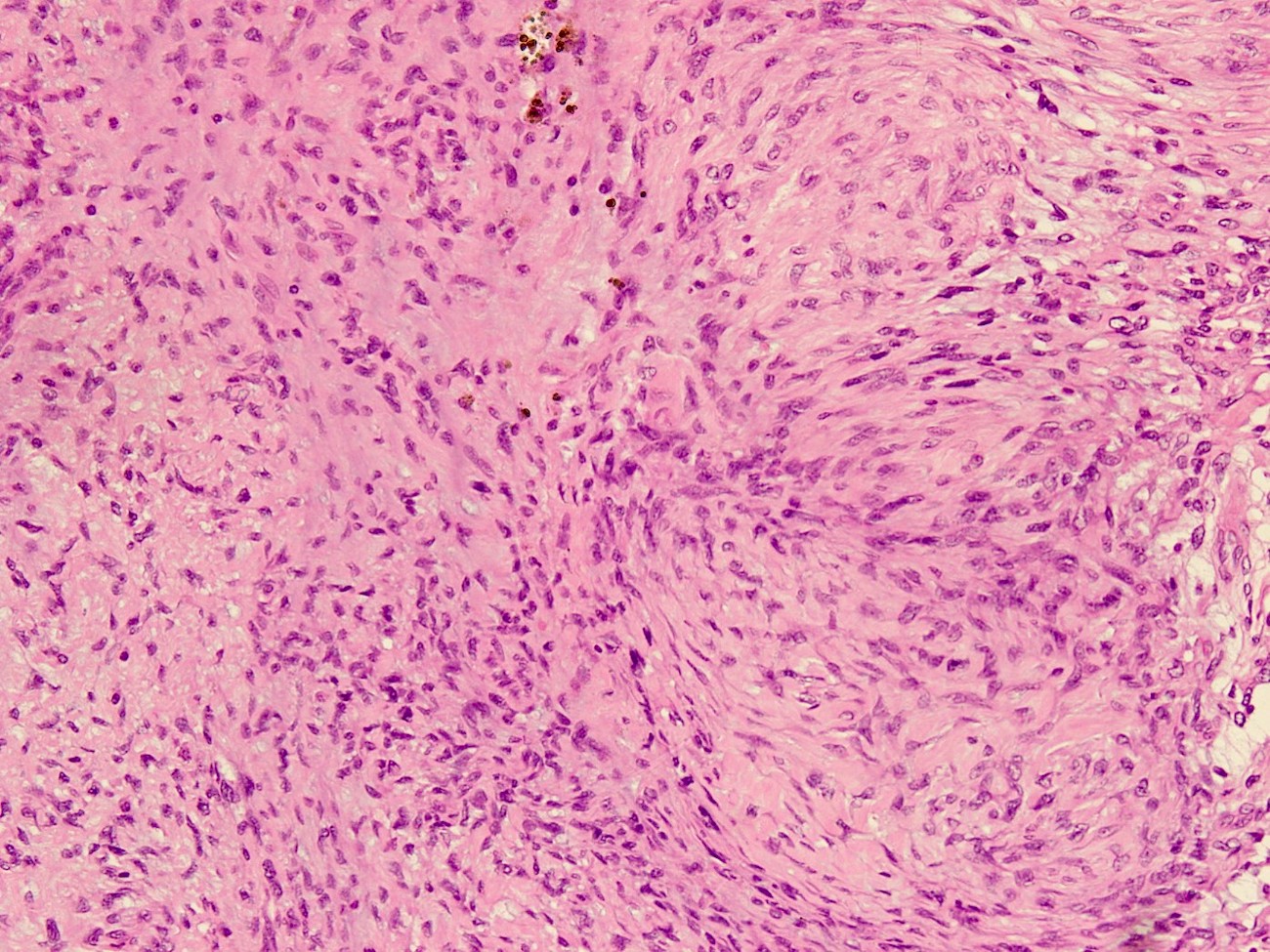
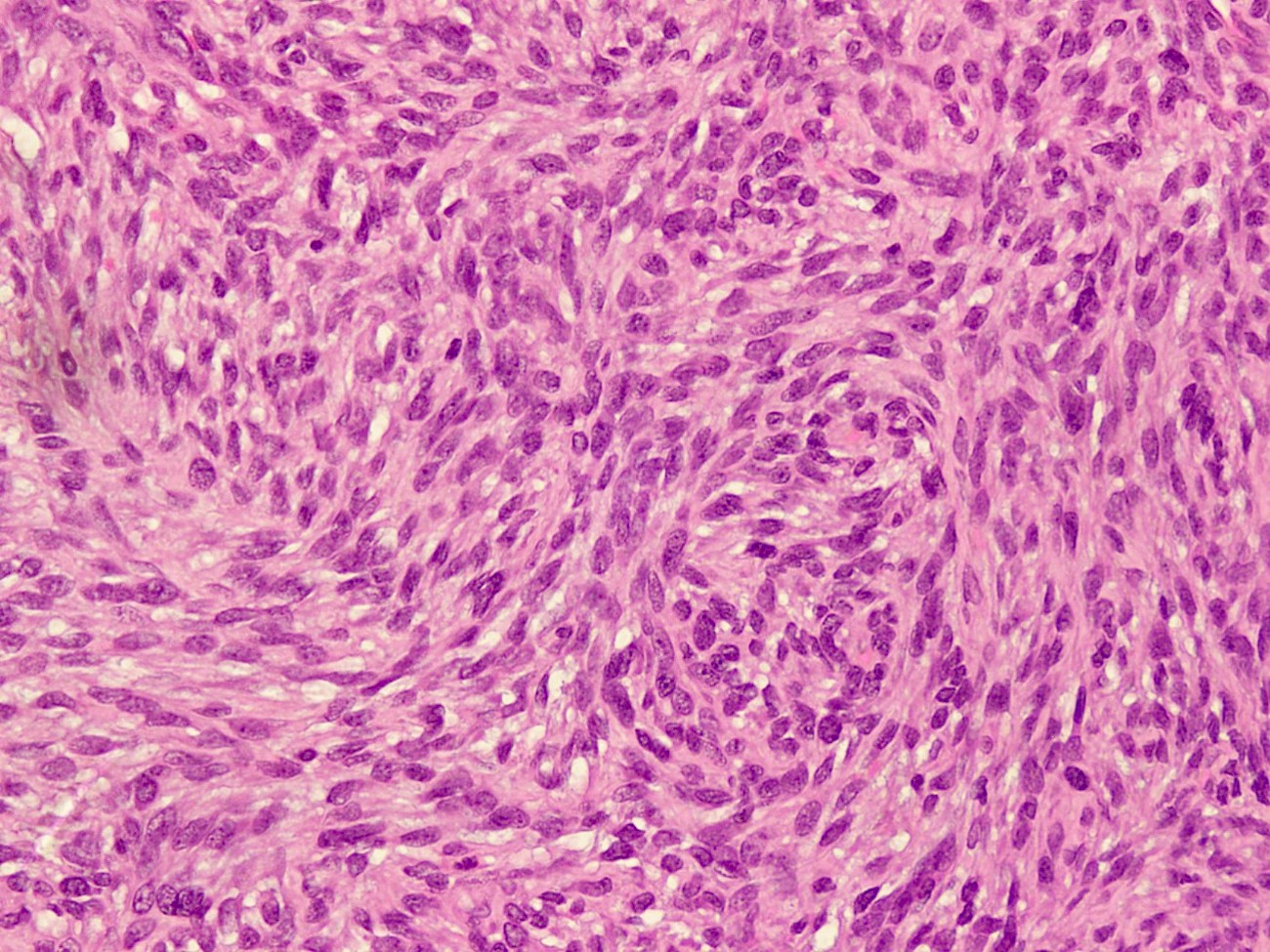
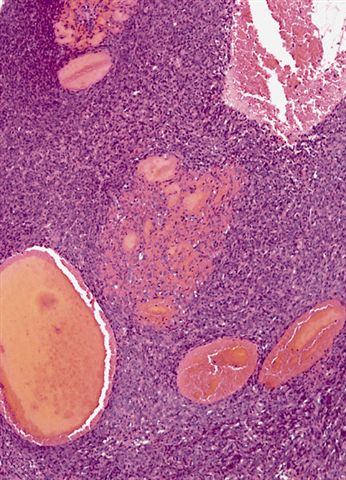
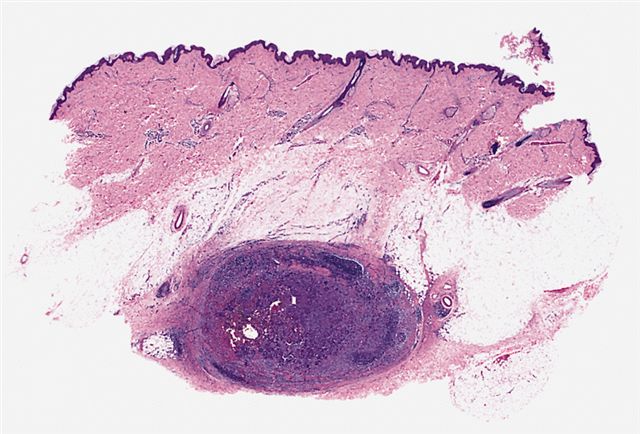
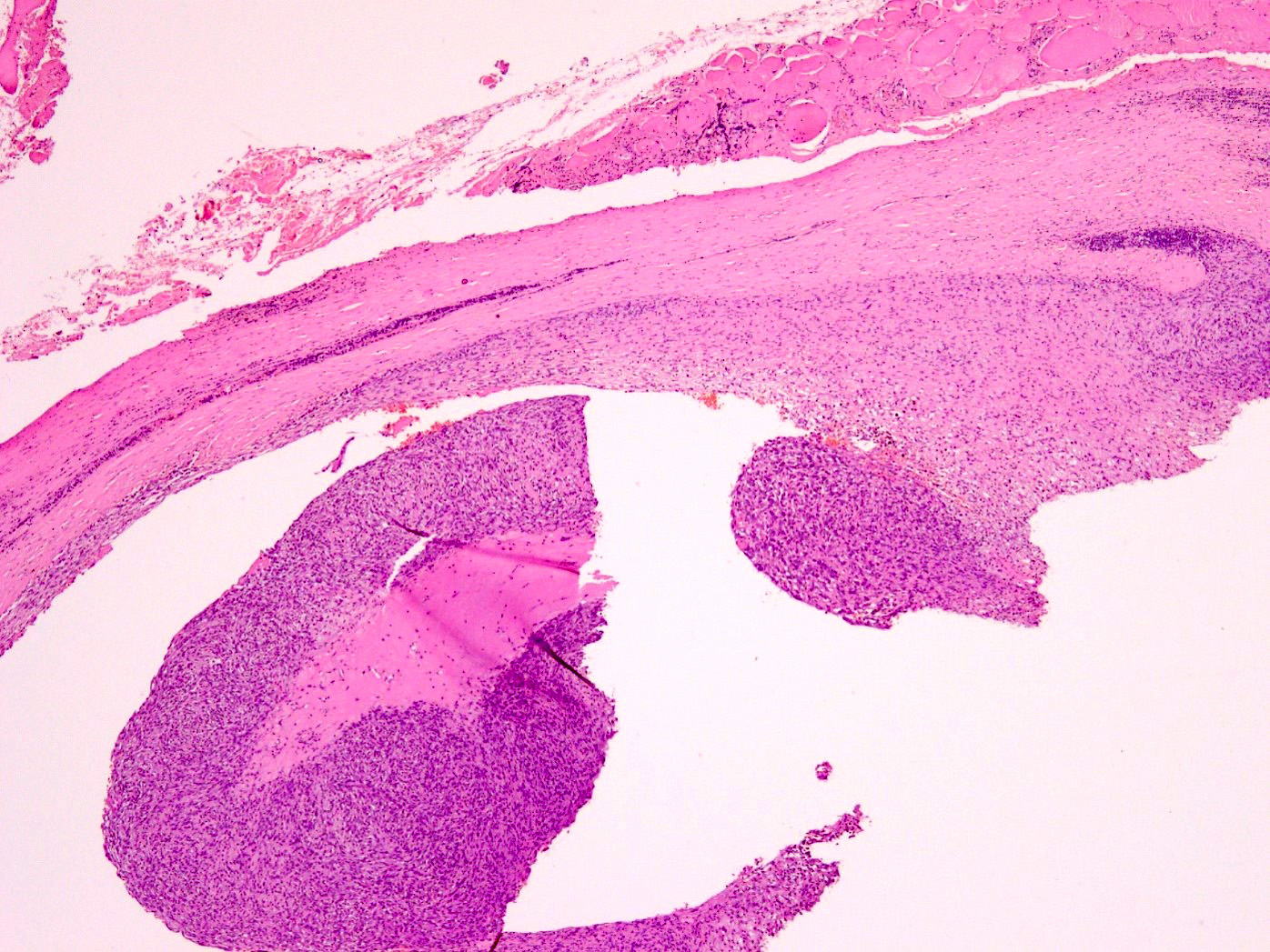
- Thick, fibrous pseudocapsule with a dense pericapsular cuff of lymphoplasmacytic cells (with or without lymphoid follicles), seen in up to 80% of cases
- Pseudocapsule imparts a low power resemblance to a lymph node involved by a metastatic tumor; absence of subcapsular sinus helps differentiate it from a lymph node
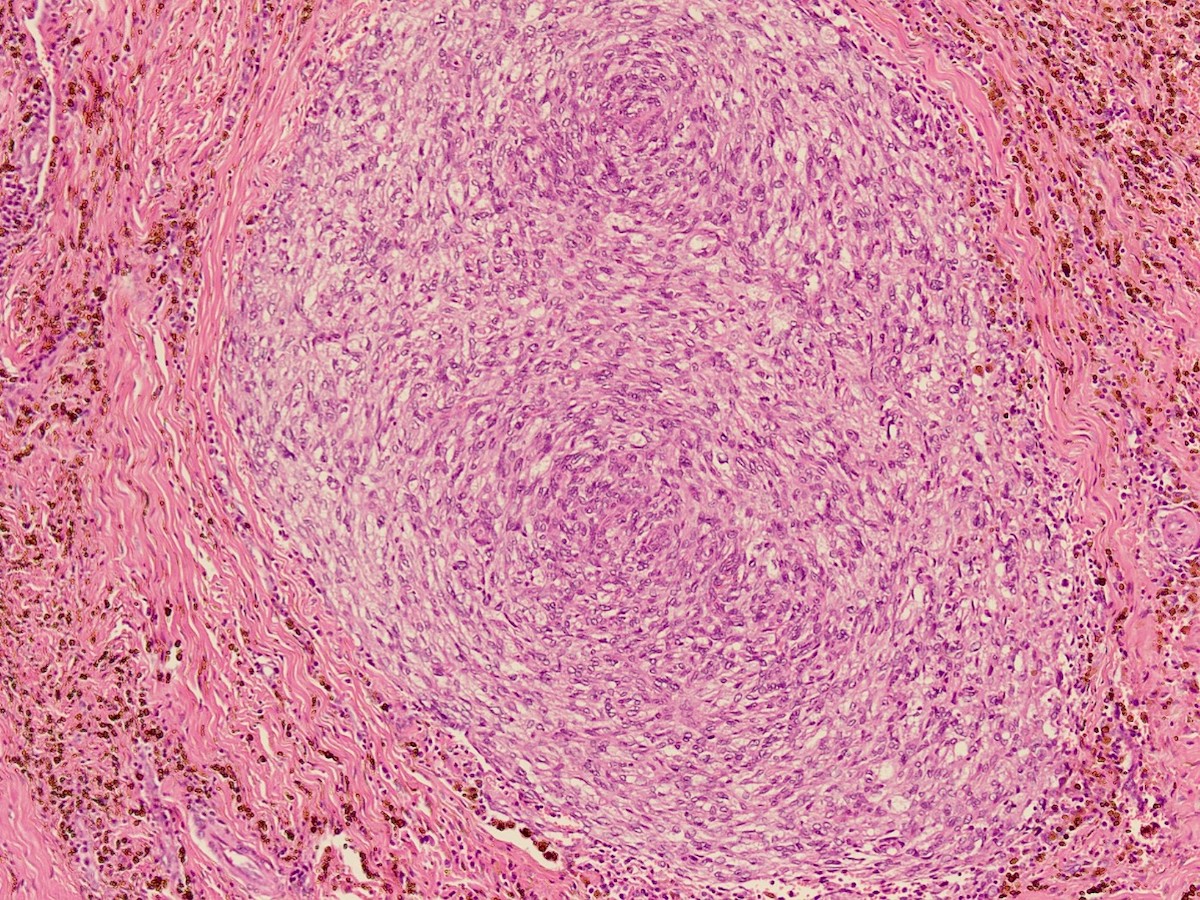
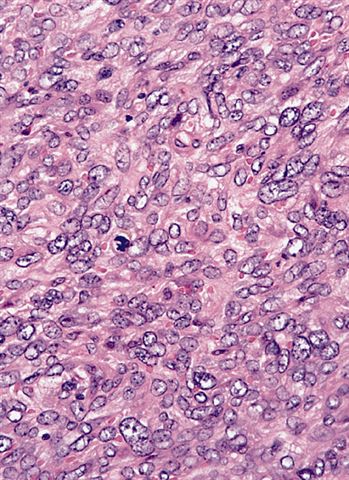
- Circumscribed, often lobulated with syncytial sheets, short fascicles or whorls of epithelioid (histiocyte-like) to spindle shaped cells with moderate amount of eosinophilic cytoplasm, mildly pleomorphic vesicular nuclei and inconspicuous nucleoli
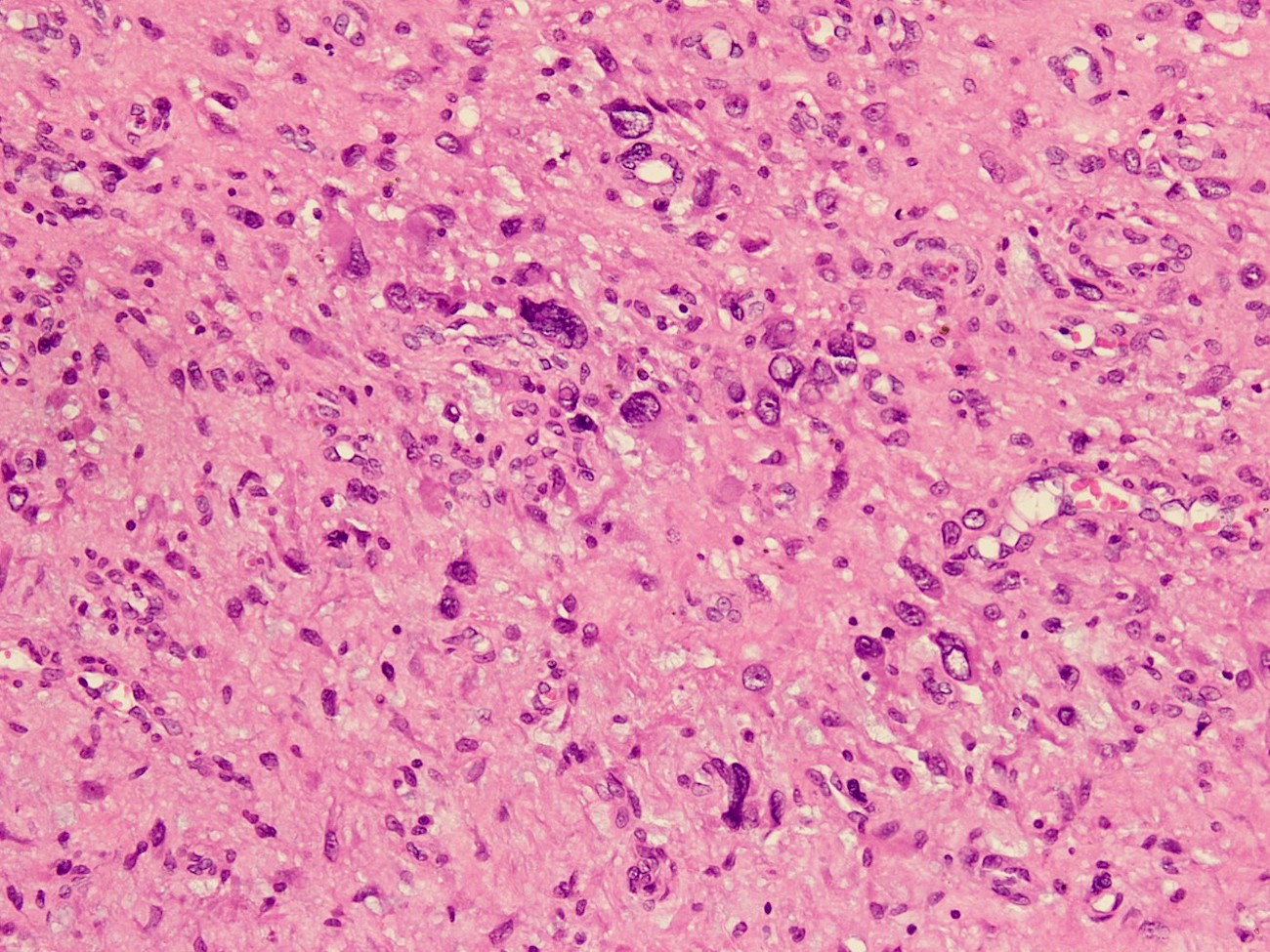
- Presence of pseudoangiomatous / pseudovascular spaces or blood filled lakes lined by tumor cells is an important diagnostic feature but may be absent in up to 33% of cases showing a solid growth (Arch Pathol Lab Med 2015;139:674)
- Mitotic activity is usually low
- Interspersed inflammatory cells are commonly seen
- Hemosiderin deposition may be prominent
- May have areas of nuclear pleomorphism and atypical mitoses
- Morphological variations:
- Small round blue cell tumor-like morphology
- Myxoid change particularly in intracranial ones (World Neurosurg 2019;126:113)
- Pulmonary edema-like pattern
- Microcystic pattern
- Myxoid chondrosarcoma-like pattern (cord-like arrangement against myxoid stroma)
- Marked sclerosis
- Amianthoid fibers
- Rhabdoid features (Brain Tumor Pathol 2021;38:138)
- Schwannoma-like features (nuclear palisading and hyalinized vessels)
Microscopic (histologic) images
Contributed by Nasir Ud Din, M.B.B.S. and AFIP images
Cytology description
- Cytological diagnosis of angiomatoid fibrous histiocytoma is challenging due to its rarity and nonspecific features
- Smears are usually moderately cellular and show spindle shaped to ovoid (histiocyte-like to fibroblast-like) cells in cohesive clusters or dispersed cells (Diagn Cytopathol 2021;49:E36)
- Nuclei show mild to moderate pleomorphism with vesicular chromatin
- Nuclear grooves or intranuclear inclusions may be present
- Background shows blood with lymphocytes and plasma cells
Positive stains
Negative stains
- Smooth muscle actin (14%), calponin (12%), caldesmon (3%) (Hum Pathol 1999;30:1336)
- Myogenin, MyoD1, CD34, CD35, ERG, S100, cytokeratin (Arch Pathol Lab Med 2015;139:674)
Molecular / cytogenetics description
- Most cases show FET family gene rearrangement (mostly EWSR1 or less commonly FUS gene rearrangement)
- FISH for EWSR1 rearrangement is useful diagnostically
- Partner gene is mostly from the CREB family (CREB1, ATF1 or CREM)
- Any of the following 3 characteristic translocations can be seen:
- t(2;22)(q33;q12) creating EWSR1::CREB1 fusion gene (90% cases)
- t(12;22)(q13;q12) creating EWSR1::ATF1 fusion gene (more common in extrasomatic tumors); identical translocation also seen in clear cell sarcoma of soft tissue
- t(12;16)(q13;p11) creating FUS::ATF1 fusion gene (least common) (Genes Chromosomes Cancer 2007;46:1051, Clin Cancer Res 2007;13:7322, Hum Pathol 2011;42:1359)
- Some intracranial myxoid spindle cell tumors with EWSR1::CREB family gene fusion are described, which lack the features typical of angiomatoid fibrous histiocytoma; it is not clear whether they are subtypes of angiomatoid fibrous histiocytoma or belong to a novel entity (Brain Pathol 2018;28:183)
Videos
Brief overview of morphology
Sample pathology report
- Right upper thigh, wide local excision and inguinal lymph node dissection:
- Angiomatoid fibrous histiocytoma (see comment)
- Tumor size: 5 x 4 x 2.5 cm
- Lymphovascular invasion: absent
- Margins of excision: all margins of excision are tumor free (give distances from each margin)
- Skin: tumor free
- Lymph nodes: all 06 lymph nodes are tumor free
- Comment: Angiomatoid fibrous histiocytoma is considered as a borderline malignancy of uncertain histogenesis. It may recur in up to 15% cases and rarely can metastasize. Clinical follow up at adequate interval is advised.
- FISH studies to detect EWSR1 rearrangement may be helpful for confirmation of diagnosis (optional comment for difficult cases)
Differential diagnosis
- Organized hematoma:
- No atypical spindle cells
- No pseudocapsule or lymphoplasmacytic cuff
- Negative for desmin
- Nodal metastasis:
- Metastatic melanoma in particular can mimic angiomatoid fibrous histiocytoma
- Arises in regions populated by lymph nodes
- True nodal architecture present
- Subcapsular and medullary sinuses
- History of malignancy may or may not be present
- Relevant IHC may help
- Granulomatous inflammation in a lymph node:
- Lacks solid growth pattern of angiomatoid fibrous histiocytoma
- Granulomas are usually dispersed and discrete or irregular and confluent
- Large granulomas often show central necrosis and lack cystic hemorrhage
- May contain foreign body type giant cells
- Predisposing factors may be noted clinically (exposure to infectious agents, etc.)
- CD68+, CD168+
- Negative for desmin
- Aneurysmal benign fibrous histiocytoma:
- Morphologic variant of benign fibrous histiocytoma (dermatofibroma)
- Dermal localization, often with overlying epidermal changes
- No pseudocapsule or lymphoplasmacytic cuff
- Peripheral collagen trapping often present
- Mixed cell population, including chronic inflammatory cells, siderophages and giant cells
- Negative for desmin
- Follicular dendritic cell sarcoma:
- Kaposi sarcoma (nodular):
- Spindle cell hemangioma:
- Inflammatory myofibroblastic tumor:
- Intranodal palisaded myofibroblastoma:
Additional references
Board review style question #1
A 13 year old boy presented with a left axillary swelling, gradually increasing in size over the period of 6 months. No other symptoms were reported. On examination, a 3 cm subcutaneous, cystic, freely mobile, nontender lump was identified in the medial wall of axilla. The lump was excised and sent for histopathology. The H&E and immunohistochemistry slides of this lump are shown above. What is the most likely diagnosis?
- Angiomatoid fibrous histiocytoma
- Follicular dendritic cell sarcoma of lymph node
- Inflammatory myofibroblastic tumor
- Kaposi sarcoma
- Spindle cell rhabdomyosarcoma
Board review style answer #1
Board review style question #2
Which of the following is true regarding angiomatoid fibrous histiocytoma?
- Associated with immunodeficiency
- Considered as a borderline malignancy
- Does not carry a risk of metastases
- Has a characteristic immunohistochemical profile
- More common in abdominal cavity
Board review style answer #2