Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Srivastava S. Acute gastritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachacutegastritis.html. Accessed April 24th, 2024.
Definition / general
- Acute gastritis is a sudden inflammation or swelling in the lining of the stomach characterized histologically by inflammatory cells in the lamina propria of the gastric mucosa (predominantly polymorphonuclear leukocytes); the leukocytes may also penetrate the glandular lumen or submucosa based on the severity of the lesion
- According to the Kyoto Global Consensus Report, gastritis is best classified based on etiology or atrophic versus nonatrophic gastritis and not based on duration (Curr Treat Options Gastroenterol 2020;18:488)
Essential features
- Sudden inflammation occurring in short interval of time
- Usually associated with polymorphonuclear leukocyte infiltration
- Commonly associated with nonsteroidal anti-inflammatory drugs (NSAIDs), steroid and alcohol usage
- Acute gastritis commonly includes erosive or acute hemorrhagic gastritis, nonerosive gastritis and rarely, acute Helicobacter gastritis and acute suppurative / necrotizing or acute phlegmonous gastritis
Terminology
- Active gastritis
ICD coding
Epidemiology
- No gender predilection
- Strongly associated with alcohol intake, smoking, usage of NSAIDs and steroids
Sites
- Entire stomach with a predilection in antrum
Pathophysiology
- Acute gastritis occurs when the mucosal defense mechanism is disturbed due to inflicting agents like alcohol, NSAIDs, steroids, chemotherapeutic agents, etc.; this weakened mucosal defense allows the acid to further damage the mucosal lining
- In acute phlegmonous gastritis, transmural infection is caused by Staphylococcus, Streptococcus, Clostridium or Escherichia coli
- Acute gastritis could also be caused by infection from H. pylori wherein the bacilli may cause transient hypochlorhydria and epigastric pain; however, it is self limiting and later may present as chronic gastritis and H. pylori infection (World J Gastroenterol 2014;20:5461)
Etiology
- Drugs (NSAIDs like aspirin, ibuprofen, naproxen), Helicobacter species (H. pylori and H. heilmanii), stress, uremia, ischemia, shock, corrosive agents, sepsis, trauma, alcohol, cocaine, severe burns, major surgery (Dig Liver Dis 2000;32:34)
- Rarely by chemotherapeutic agents like nivolumab, pembrolizumab, cytomegalovirus and Epstein-Barr virus, Staphylococcus, Streptococcus and Clostridium species (Dig Dis Sci 2021;66:2461, Clin J Gastroenterol 2019;12:274)
Clinical features
- Most patients are asymptomatic
- Nonspecific epigastric discomfort, abdominal pain, nausea, vomiting and loss of appetite could be presenting features in some
- May present as upper gastrointestinal bleeding (hematemesis) due to gastric erosions and ulcerations or rarely as melena (black tarry stools)
- Phlegmonous gastritis presents as a medical emergency with severe abdominal pain, nausea, vomiting (Medicine (Baltimore) 2019;98:e17777)
Diagnosis
- By patient history; confirmation by endoscopy and biopsy
Laboratory
- Complete blood count (CBC): elevated white blood cell counts with neutrophilia, with or without low hemoglobin
- Increased lactate dehydrogenase (LDH)
- Stool test for bleeding
- Urease level could be helpful in predicting acute gastritis in patients with dyspepsia (Acta Med Indones 2022;54:42)
Radiology description
- Endoscopic findings: reddish or friable mucosa, edematous mucosa; sometimes digested blood can be seen (J Crit Care Med (Targu Mures) 2018;4:143)
- CT scan: diffuse thickening and edematous stomach wall in phlegmonous gastritis (Medicine (Baltimore) 2018;97:e0629)
Prognostic factors
- Usually resolves by itself within a few days or weeks once the inflammation settles and the causative agents are removed
- Can progress to chronic gastritis if not treated; in case of Helicobacter pylori infection, it usually leads to chronic gastritis, which further increases the risk of atrophic gastritis and sometimes gastric cancer
Case reports
- 6 year old boy admitted for hematemesis, abdominal pain and loss of appetite (J Crit Care Med (Targu Mures) 2018;4:143)
- 14 year old girl presented with acute generalized abdominal pain and attack of nonbilious vomiting (BMJ Case Rep 2019;12:e229102)
- 32 year old woman presented with gastric ulcers caused by pressure from trauma (Intractable Rare Dis Res 2016;5:306)
- 33 year old man of mixed phenotype acute leukemia developed acute phlegmonous gastritis during the neutropenia phase (Medicine (Baltimore) 2019;98:e17777)
- 47 year old man presented in the hospital with abdominal pain, high fever and vomiting (Medicine (Baltimore) 2018;97:e0629)
Treatment
- Self limiting and usually resolves upon removal of the causative factors
- Proton pump inhibitor therapy and H2 antagonists
- Eradication therapy in cases of acute H. pylori gastritis (lansoprazole, clarithromycin, amoxicillin and rebapemide) (J Gastroenterol Hepatol 2000;15:1377)
- Broad spectrum antibiotics in cases of phlegmonous or suppurative gastritis
Gross description
- Superficial erosive lesions
- Swollen edematous stomach wall, with or without pus accumulation in acute phlegmonous gastritis
Gross images
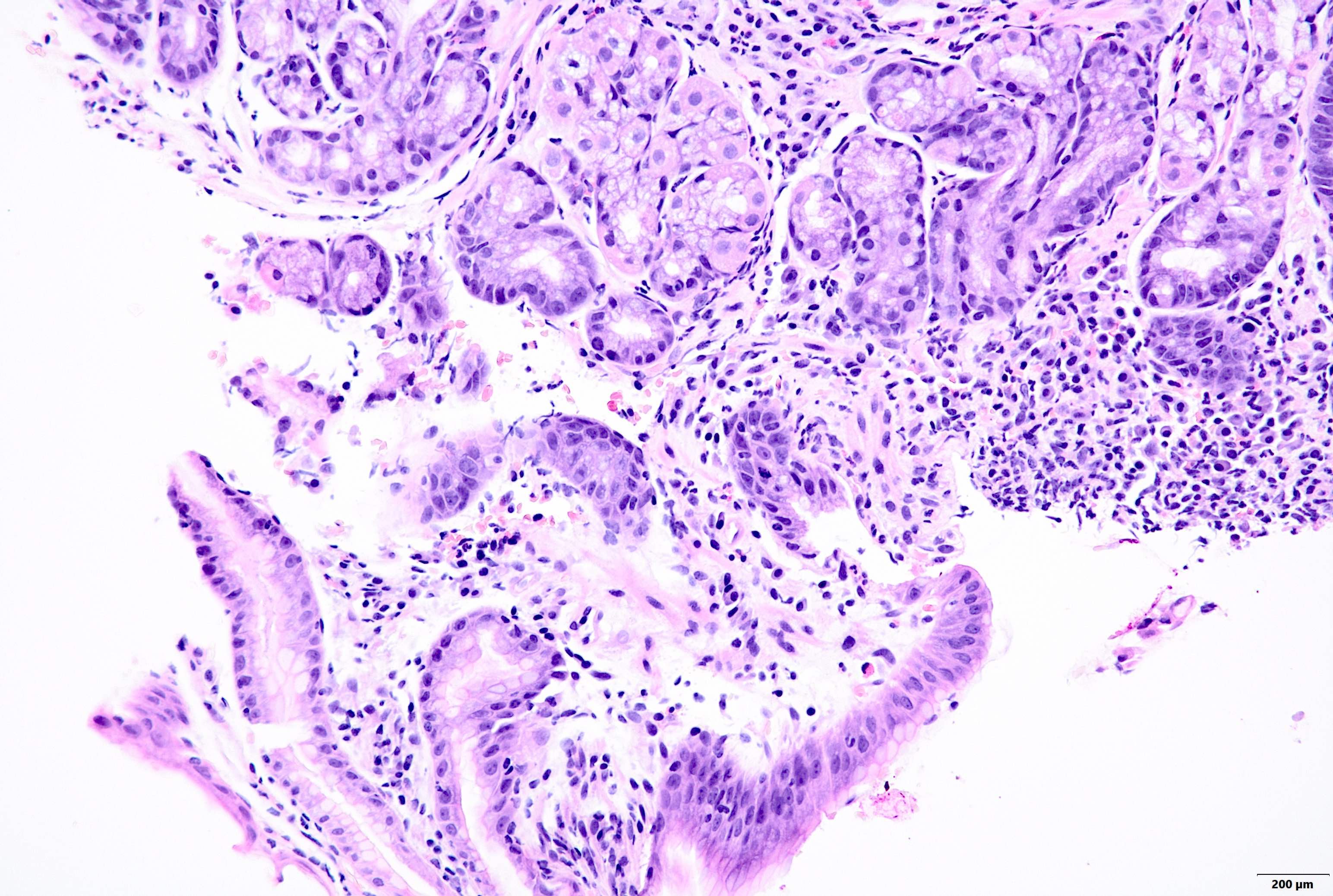
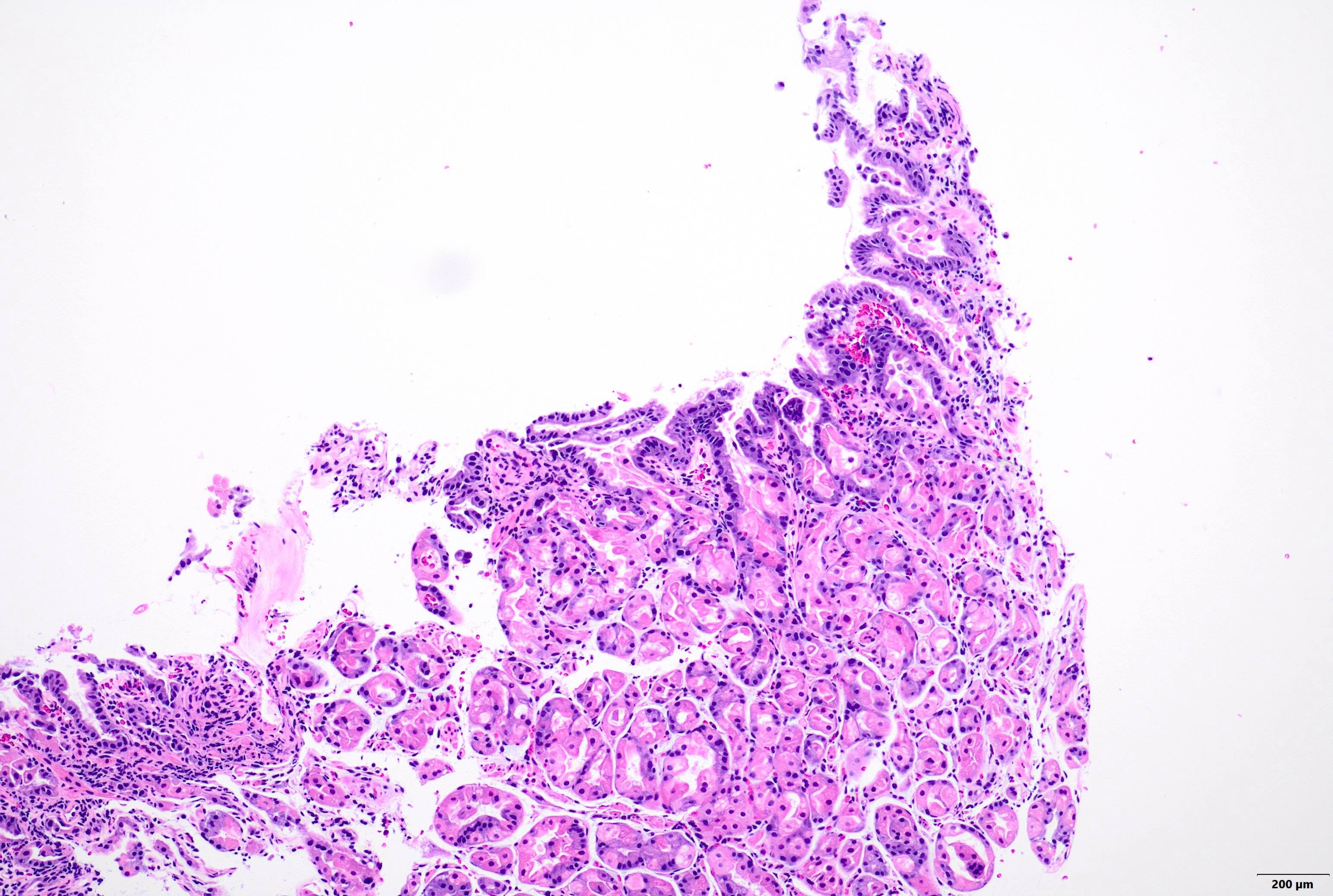
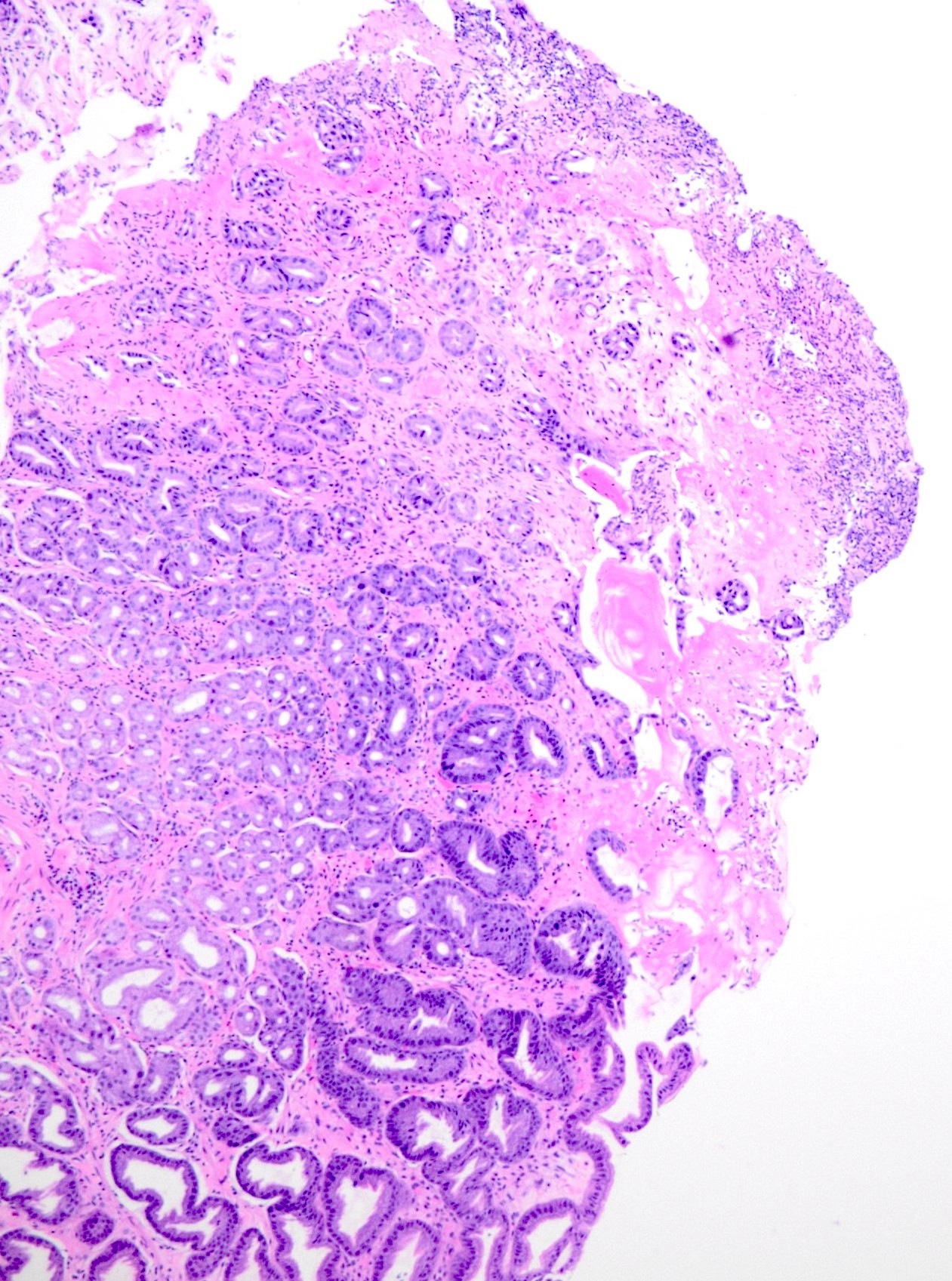
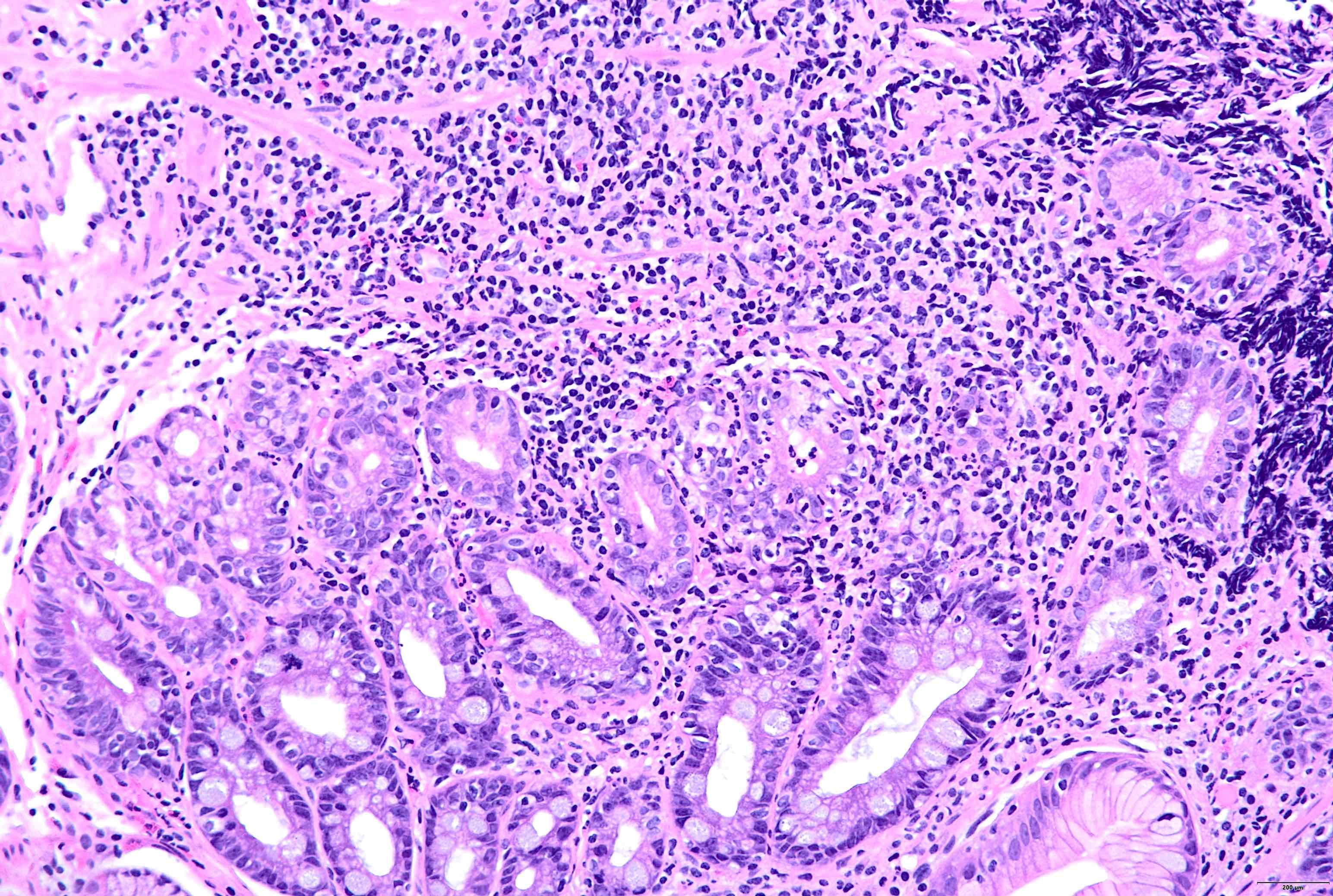
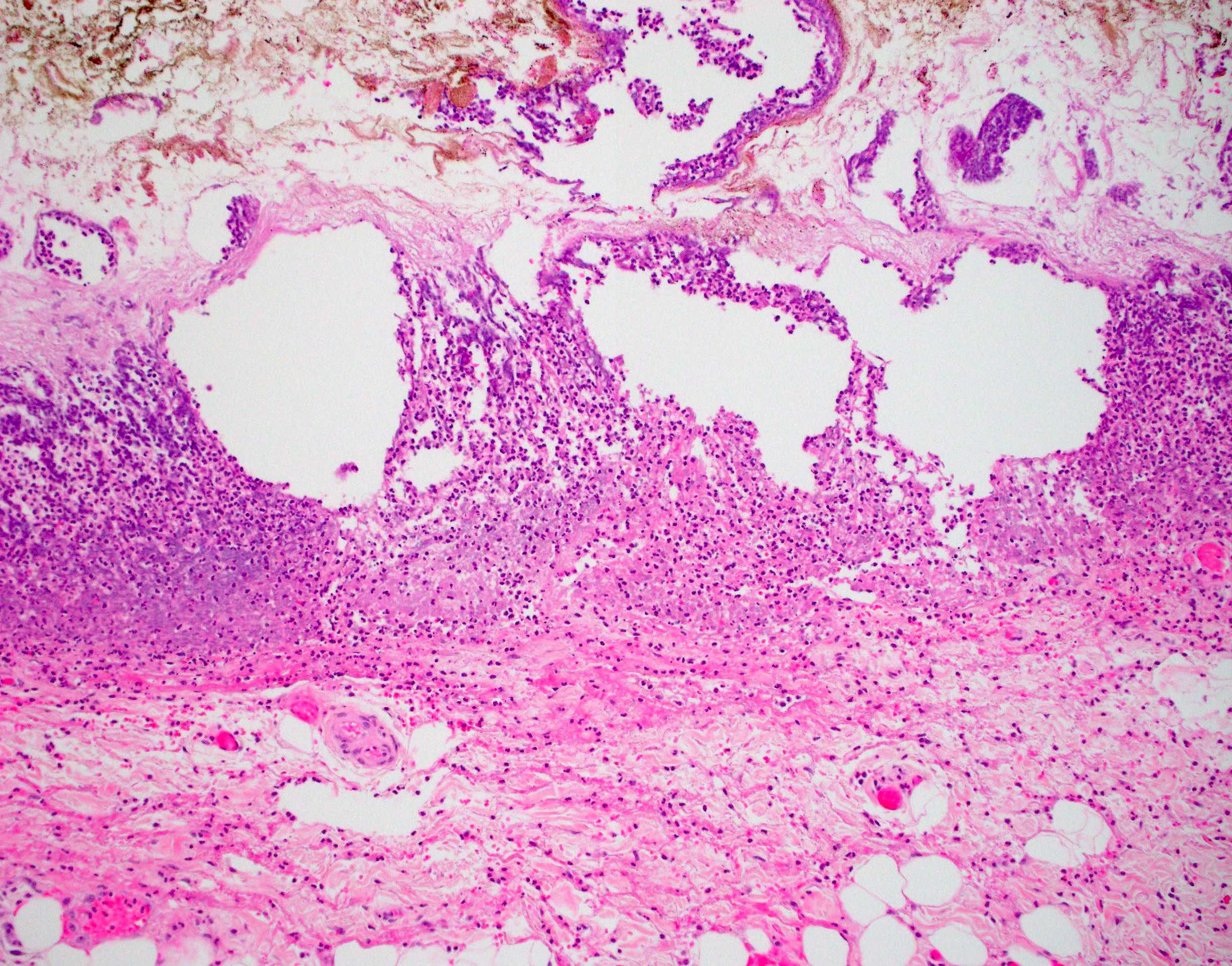
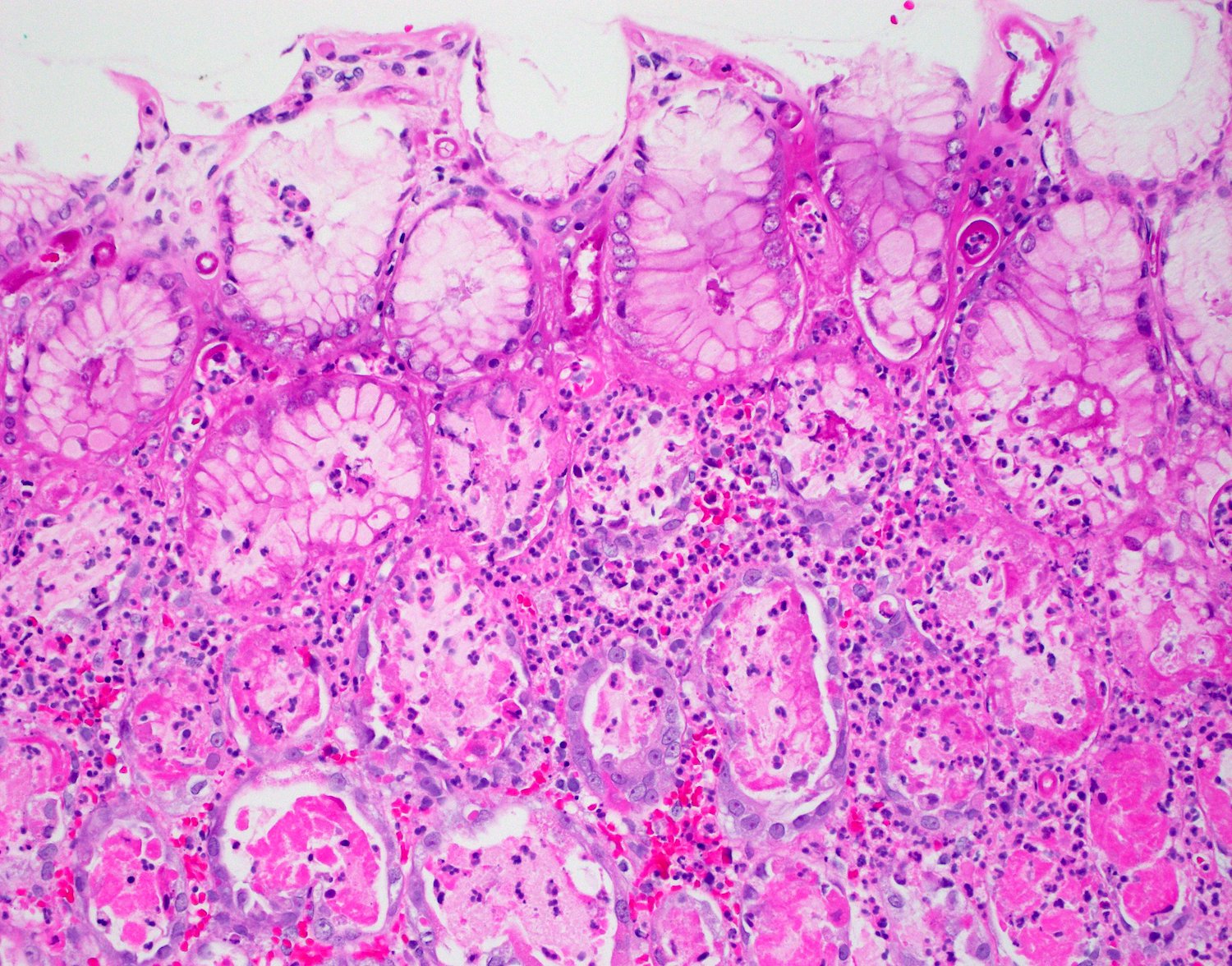
Microscopic (histologic) description
- For alcoholic, stress related or NSAID induced gastritis, initially all the segments of the stomach are involved, followed by predominance in antrum
- Diffuse edema in lamina propria, capillary congestion and interstitial hemorrhage in varying degrees
- Erosions may or may not be present, with regenerative epithelium as the only evidence
- A few neutrophils are present (Am J Surg Pathol 1996;20:1161)
- Acute phase of Helicobacter (though rarely encountered) shows marked degenerative changes in mucus epithelium including mucus depletion, cellular exfoliation and syncytial regenerative changes
- Neutrophilic infiltration on the surface and foveolar epithelium along with pit abscesses can be seen (Am J Surg Pathol 1996;20:1161)
- In acute phlegmonous gastritis, there is diffuse necrosis in the stomach wall extending from submucosa to muscularis layer to the serosa; there is an accumulation of pus and extensive infiltration of neutrophils (Medicine (Baltimore) 2018;97:e0629)
Microscopic (histologic) images
Positive stains
- Giemsa and silver stain if H. pylori is the cause of acute gastritis
Sample pathology report
- Stomach, antral biopsy:
- Stomach biopsy shows acute erosive gastritis (see comment)
- Comment: No evidence of intestinal metaplasia, H. pylori, dysplasia or malignancy.
Differential diagnosis
- Peptic ulcer disease:
- Peptic ulcer disease presents as round or oval ulcer / crater in the gastric mucosa, while acute gastritis usually presents with redness, superficial erosions or shallow ulcers
- Duration of disease is another important differentiating feature between peptic ulcer disease and acute gastritis
- Chronic gastritis:
- Longstanding duration
- Presence of chronic inflammatory infiltrate like plasma cells and lymphocytes
- Chronic H. pylori gastritis:
- Chronic inflammatory infiltrate with plasma cells and lymphocytes and neutrophils
Board review style question #1
A 40 year old working professional woman visited her general practitioner with complaints of abdominal pain, nausea and loss of appetite. On eliciting her clinical history, the general practitioner found that she had some deadlines to meet in her office and was working overtime; in addition, she was taking ibuprofen for her body pain during the past few days. The general practitioner referred her to a gastroenterologist for an endoscopy. What could be the possible endoscopic finding?
- 2 cm friable lesion in the fundus of the stomach
- 5 cm ulcer at lesser curvature with irregular margins
- Superficial mucosal erosion with erythema
- Thickened and tortuous mucosal folds
Board review style answer #1
C. Superficial mucosal erosion with erythema. In this context, this endoscopy most likely shows features of acute gastritis induced by the frequent usage of ibuprofen along with overproduction of gastric acid due to anxiety and stress. Answer D is incorrect because thickened and tortuous folds are usually seen in chronic gastritis, Menetrier disease or malignancy. Answers A and B are incorrect because they are characteristic features of malignant ulcers.
Comment Here
Reference: Acute gastritis
Comment Here
Reference: Acute gastritis
Board review style question #2
A 52 year old woman with 4 weeks of acute bacterial sinusitis was treated with a course of doxycycline combined with aggressive nasal lavage. She then developed dyspepsia. Upper endoscopy was performed and found patches of mild erythema in the antrum and body; additionally, there were areas of pale yellow mucosa in the cardia and fundus. Biopsy was performed to rule out H. pylori, intestinal metaplasia, dysplasia or malignancy. What would be the most likely diagnosis of this patient?
- Acute gastritis
- Chronic active gastritis
- Chronic gastritis
- Signet ring cell carcinoma
Board review style answer #2
A. Acute gastritis. This is a typical case of doxycycline induced acute gastritis. In the representative image, notice neutrophil infiltrates and superficial mucosal capillaries with characteristic eosinophilic degenerative changes. Answer C is incorrect because chronic gastritis features lymphoplasmacytic infiltrates more than neutrophils. Answer B is incorrect because chronic active gastritis is usually seen in patients with Helicobacter pylori infection. The cells are degenerative looking rather than dysplasia. Answer D is incorrect because there are no atypical cells or signet ring cell carcinoma in this biopsy.
Comment Here
Reference: Acute gastritis
Comment Here
Reference: Acute gastritis