Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Important features to report | Diagrams / tables | Microscopic (histologic) images | Positive stains | Sample pathology report | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Srivastava S. Gastritis-features to report. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/stomachgastritisfeatures.html. Accessed April 24th, 2024.
Definition / general
- Features to report by international protocols
- Updated Sydney system (based on topography, morphology and etiology) (Am J Surg Pathol 1996;20:1161)
- Operative link for gastritis assessment (OLGA / OLGIM staging system) (based on atrophy or intestinal metaplasia) (Dig Liver Dis 2011;43:S373)
Essential features
- Chronic and active gastritis should be graded as mild, moderate and marked
- The presence and extent of intestinal metaplasia (IM) should be documented
- H. pylori should be reported as present or absent
- Dysplasia if present should be graded as low or high grade
Terminology
- Chronic gastritis, chronic inflammation, active gastritis, chronic active gastritis
ICD coding
- ICD-11
- DA42 - gastritis
- DA42.0 - autoimmune gastritis
- DA42.1 - Helicobacter pylori induced gastritis
- DA42.2 - eosinophilic gastritis
- DA42.3 - lymphocytic gastritis
- DA42.4 - allergic gastritis
- DA42.5 - gastritis due to duodenogastric reflux
- DA42.7 - gastritis of unknown etiology with specific endoscopic or pathological features
- DA42.8 - gastritis due to external causes
- DA42.9 - gastric phlegmon
- DA42.Y - other specified gastritis
- DA42.Z - gastritis, unspecified
- DA42 - gastritis
Important features to report
- Location / site
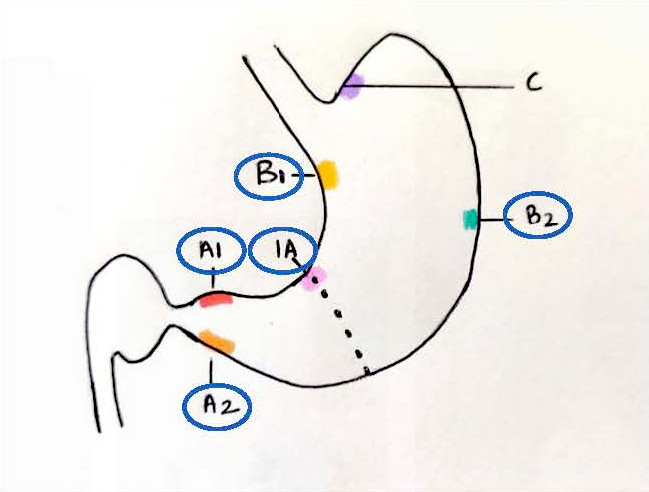
- 5 biopsy specimens are essential
- 2 from antrum (2 - 3 cm from the pylorus, 1 each from the lesser and greater curvature), 2 from the body (8 cm from the cardia, 1 each from the lesser and greater curvature) and incisura angularis
- Biopsies from different sites should be separately identifiable when submitted to the laboratory
- Note: it has proven useful to ink the antrum greater curve with red and incisura with black and place antrum lesser and greater curve and incisura on 1 slide, while body greater curve is inked red and placed together with lesser curve biopsy on another slide
- Pathologist should be informed about endoscopic findings, clinical history and medications taken in the previous 2 months, especially NSAIDS and proton pump inhibitors (PPIs)
- Optional additional biopsies from suspected lesions or according to local epidemiological conditions with respect to gastritis type and incidence of gastric cancer
- 5 biopsy specimens are essential
- Morphological variables
- Graded (mild, moderate and marked)
- H. pylori density
- Essential reporting whether H. pylori is present or absent
- Density grading is done for epidemiological associations and should be on the gastric epithelium and not in the intestinal metaplastic areas
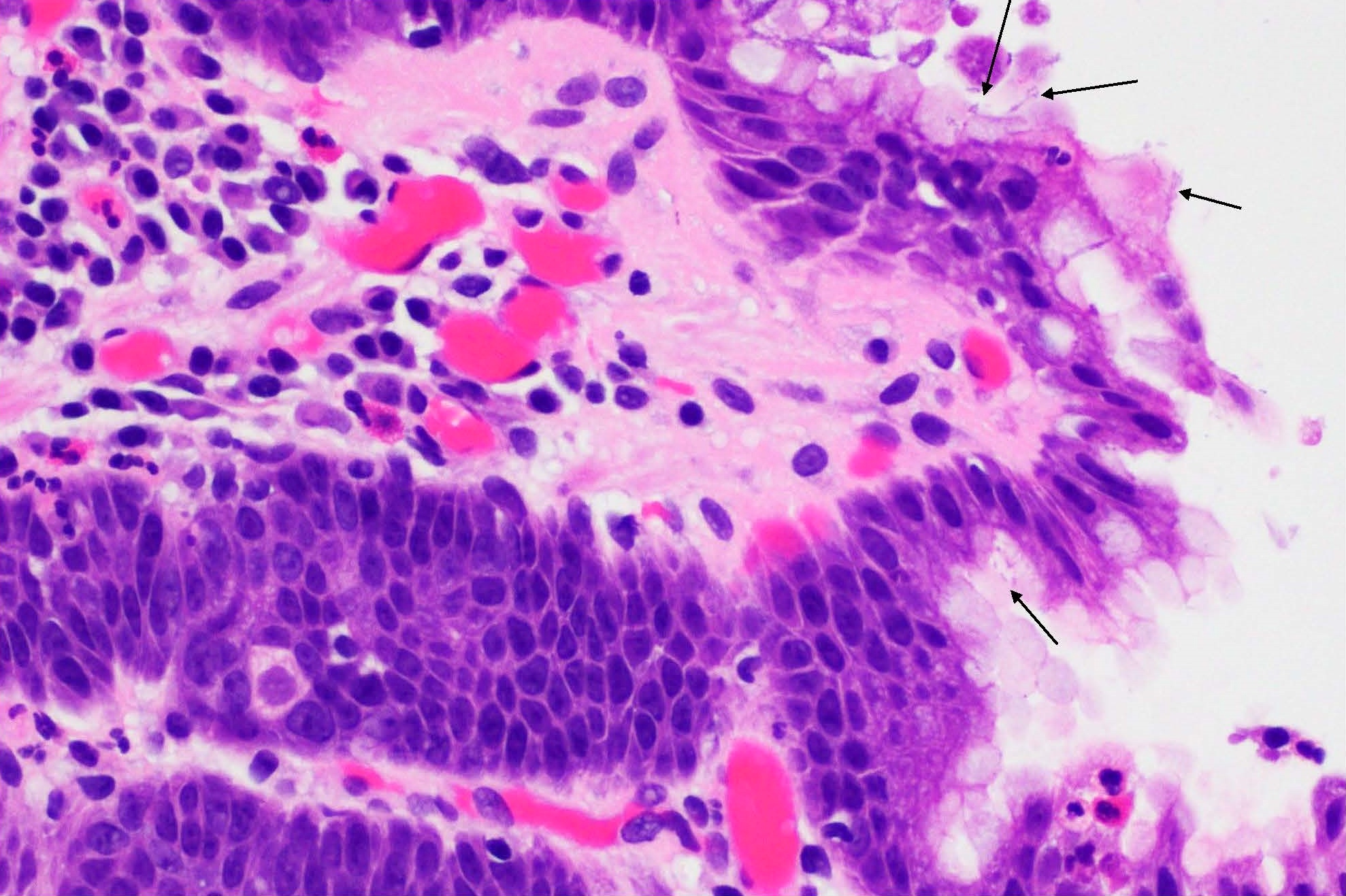
- Neutrophilic activity
- Grading of neutrophilic density is done in context of chronic active gastritis due to H. pylori
- Accumulated in the lamina propria, within the epithelium (glandular neck) and foveolar lumen (pit abscess)
- Density is correlated to the extent of mucosal damage and intensity of H. pylori infection
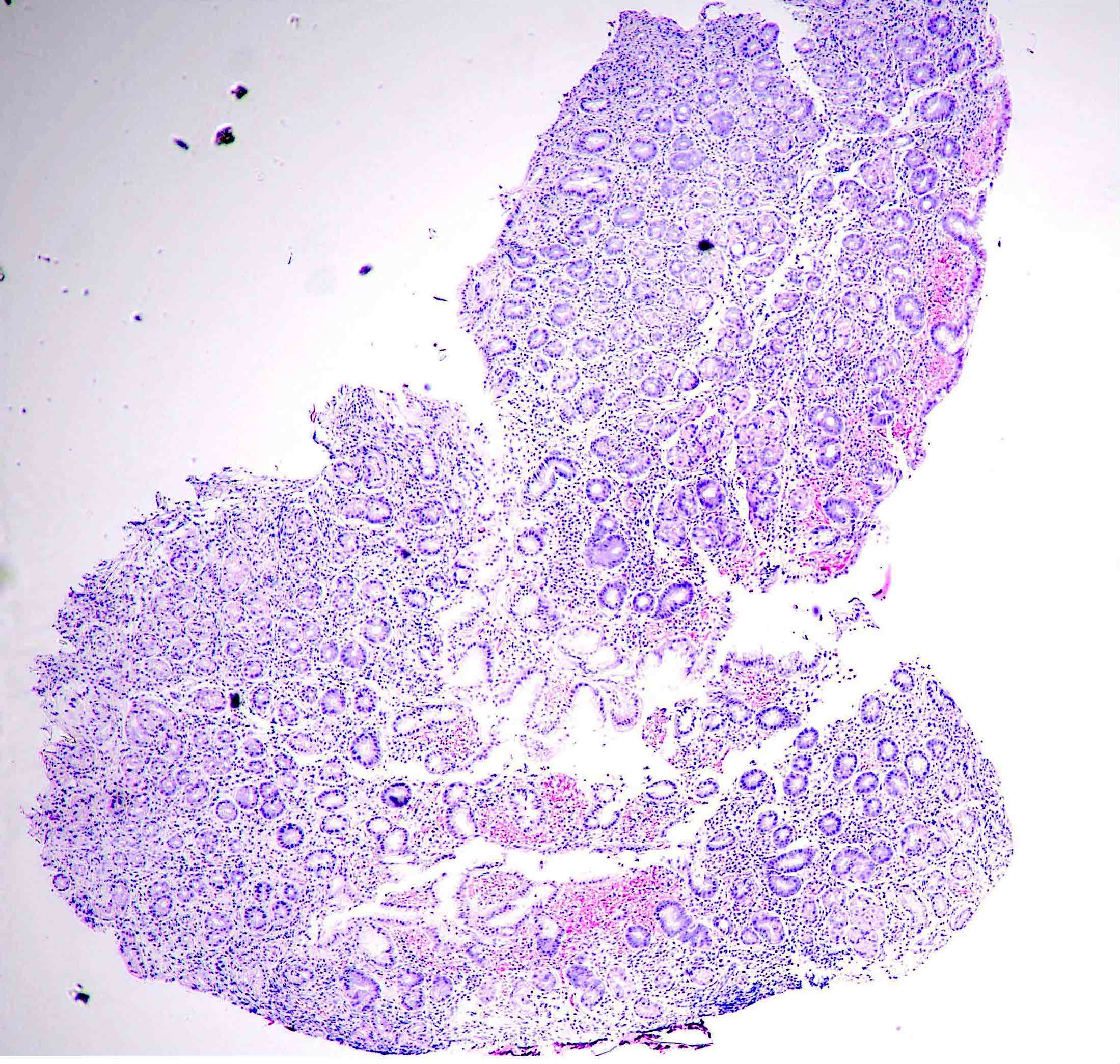
- Chronic inflammation
- Grading of mononuclear leukocytes and plasma cells should be done
- 2 - 5 lymphocytes, plasma cells and macrophages per high power field in the lamina propria or 2 - 3 lymphocytes or plasma cells in between the gastric foveolae is normally seen
- Grading chronic inflammatory cells is important to monitor the pre and post antibacterial treatment, especially H. pylori
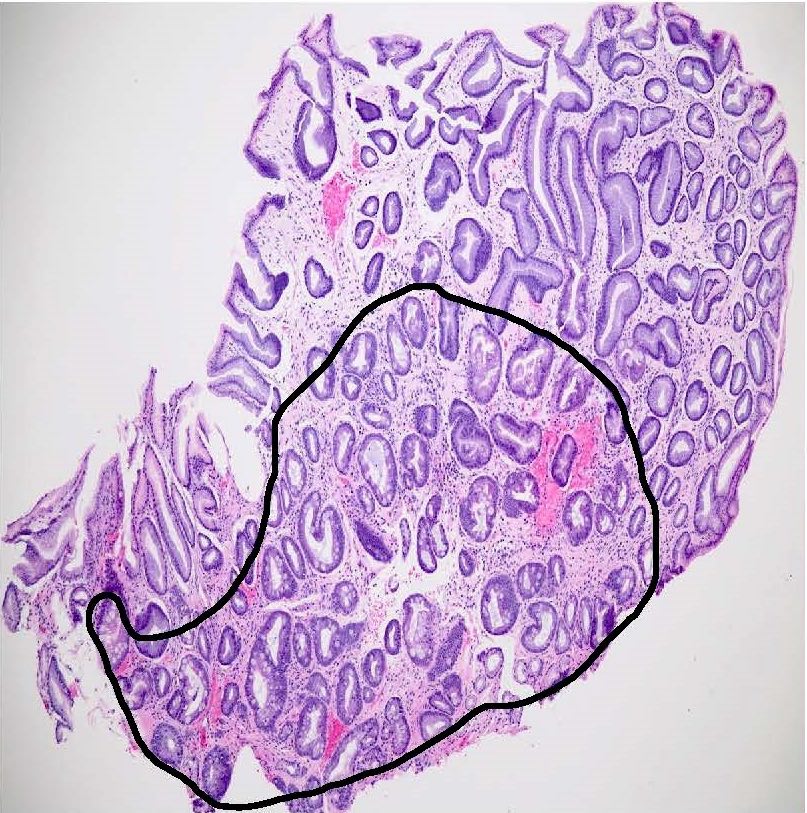
- Atrophy
- Loss of glandular tissue is termed as atrophy; in endoscopic biopsies, it may be challenging to identify atrophy especially in the presence of intestinal or pseudopyloric metaplasia
- Visual analog scale should be followed to grade the atrophy
- Mild < 30%, moderate 31 - 60% and marked > 60% (Dig Liver Dis 2008;40:8)
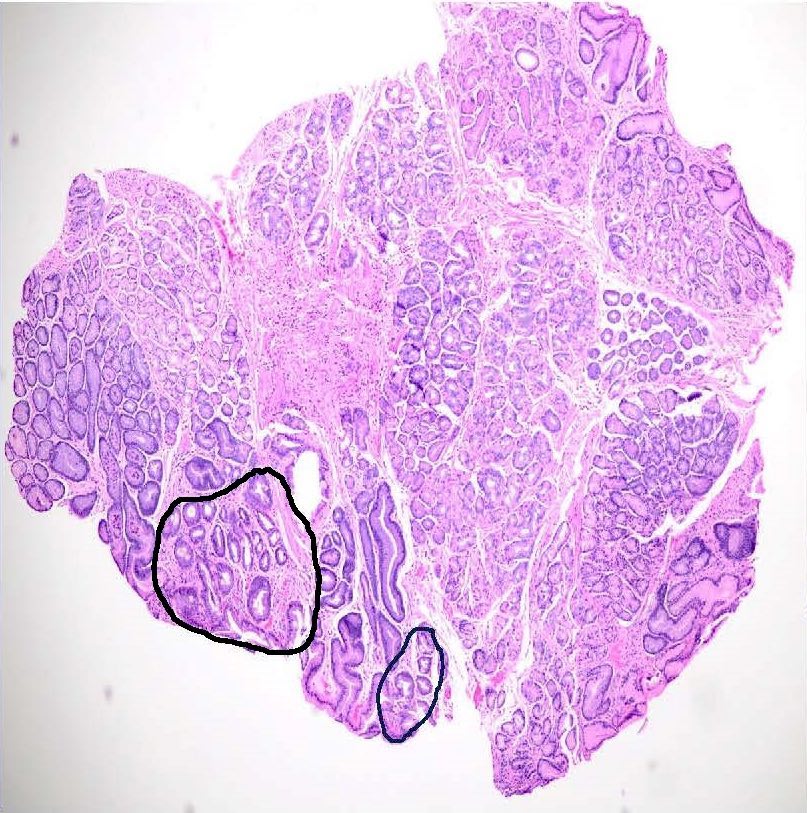
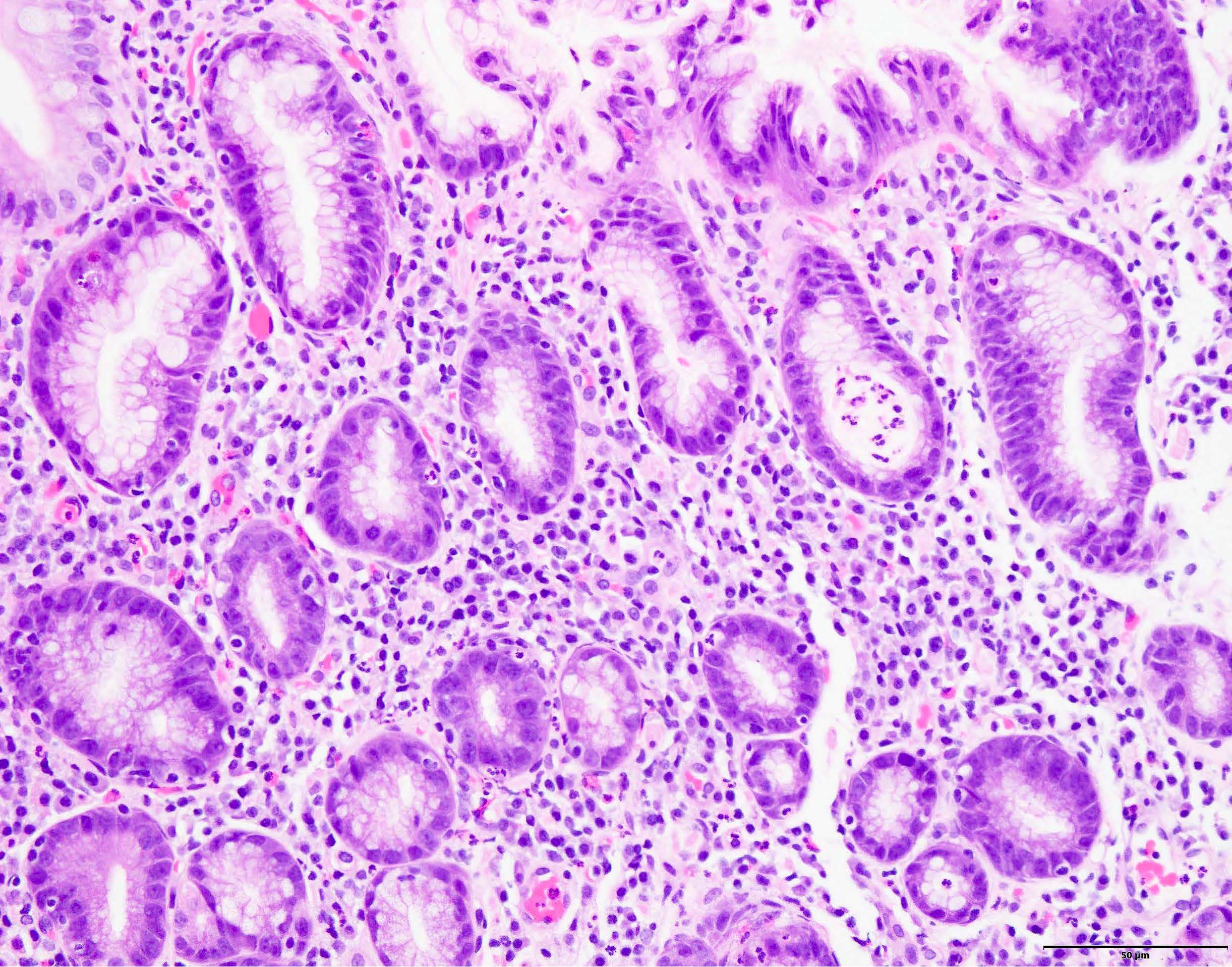
- Intestinal metaplasia
- Presence of intestinal type epithelium replete with goblet cells, with or without brush border, Paneth cells and columnar cells is known as IM
- Routine subtyping of IM is not recommended in clinical set up and should be confined to research settings only
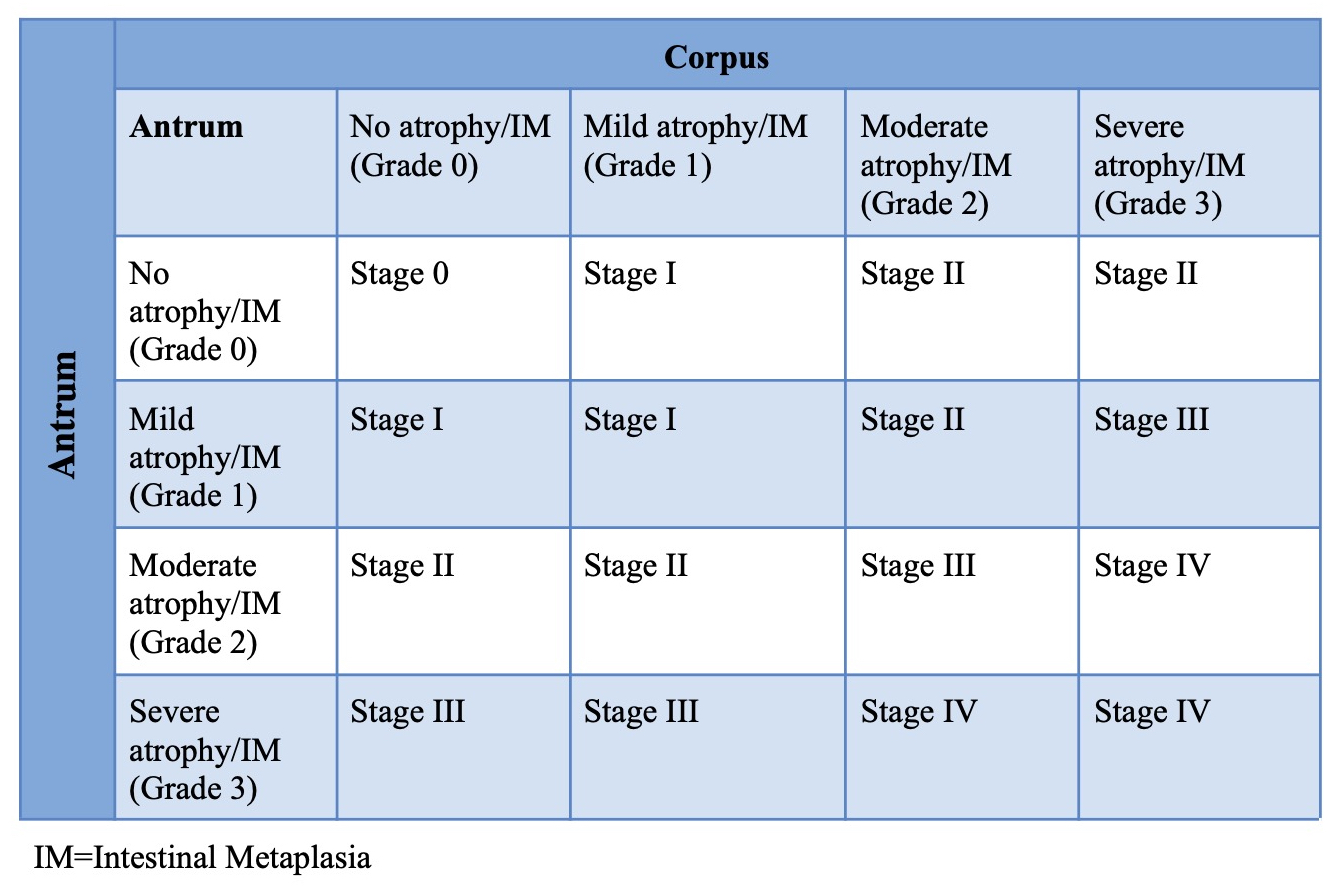
- Operative link on gastritis assessment (OLGA) / operative link on intestinal metaplasia assessment (OLGIM)
- Recently histological classification known as OLGA (operative link on gastritis assessment) was proposed to grade gastritis into stages with corresponding risks for gastric cancer (GC) (Dig Liver Dis 2008;40:8)
- Due to poor interobserver agreement in grading atrophy, IM is currently being used to grade gastritis (OLGIM) (Gastrointest Endosc 2010;71:1150)
- OLGA / OLGIM utilizes the percentage of atrophy / IM given by Sydney protocol in all of the 5 biopsies
- Average sum of percentages of atrophy / IM in incisura angularis and antrum (lesser and greater curves) is regarded as cumulative atrophy / IM grade in antrum
- While the average sum of percentages of atrophy / IM in the body (lesser and greater curves) is regarded as cumulative atrophy / IM grade in the body
- Stages III and IV are associated with gastric cancer
- European Society of Gastrointestinal Endoscopy (ESGE) 2019 and Academy of Medicine, Singapore clinical guidelines recommends endoscopic surveillance every 3 years for patients with OLGA / OLGIM stage III and IV (Endoscopy 2019;51:365, Ann Acad Med Singap 2022;51:417)
- Average sum of percentages of atrophy / IM in incisura angularis and antrum (lesser and greater curves) is regarded as cumulative atrophy / IM grade in antrum
- Dysplasia, if present, should be documented as low or high grade according to the Vienna classification (Gut 2002;51:130)
- H. pylori density
- Nongraded
- Surface epithelial damage, mucus depletion and erosion especially in the context of H. pylori infection should be noted
- Distinguish true erosions (fibrin deposits, neutrophilic infiltrate and regenerative changes) from detachment of surface epithelium due to mishandling and processing
- Lymphoid aggregates are hallmarks of H. pylori infection; hence, not graded
- Presence of lymphoid aggregates in the absence of H. pylori indicates either overlooking the presence of the bacterium, sampling error or H. pylori infection that has cleared
- Irregular or large lymphoid aggregates or dense aggregates of lymphocytes warrant the diagnosis of mucosa associated lymphoid tissue (MALT)
- Foveolar hyperplasia
- Characterized by increased length and tortuosity of foveolae along with the expansion of the proliferative zone and increased nuclear size
- It is most prominent in chemical gastritis
- Pseudopyloric metaplasia (spasmolytic polypeptide expressing metaplasia)
- These are metaplastic glands resembling pyloric glands that are observed in the body of the stomach
- Pseudopyloric glands must be differentiated from the true antral glands especially if the location of the biopsy is not confirmed
- True antral glands have G or the gastrin cells while these are absent in the pseudopyloric glands
- Note: IHC staining for gastrin can be performed to ascertain the site in cases with pseudopyloric metaplasia
- Pseudopyloric glands also secrete pepsinogen I and II and have enterochromaffin cells while the antral glands secrete only pepsinogen I
- Pancreatic metaplasia
- Characterized by replacement of the gastric glands by the pancreatic acinar cells
- Pancreatic metaplasia is associated with IM and gastritis
- Endocrine cell hyperplasia
- Enterochromaffin-like cell hyperplasia is seen in autoimmune gastritis (AIG)
- Hypochlorhydria or achlorhydria drives the G cells which secretes excessive gastrin, which in turn leads to the hyperplasia of the histamine producing enterochromaffin-like cells
- Special stains such as Gromelius, IHC for chromogranin A and synaptophysin can be used to detect the enterochromaffin-like cell hyperplasia
- Surface epithelial damage, mucus depletion and erosion especially in the context of H. pylori infection should be noted
- Graded (mild, moderate and marked)
- Topography
- Recommendations
- Patterns of chronic gastritis should be documented as diffuse (both antrum and corpus), antral predominant or corpus predominant
- Patterns of atrophy and IM should be categorized as multifocal or diffuse (multifocal atrophy and IM are characterized by patchy glandular loss and IM alternating with well preserved glandular layer)
- Antrum usually exhibits 1 grade higher prominent gastritis than the corpus
- Corpus predominant gastritis is usually the result of autoimmune and lymphocytic gastritis
- Multifocal atrophic gastritis is mostly caused by H. pylori infection and increases the risk for gastric cancer
- Recommendations
- Etiology
- If H. pylori is found in the biopsy, then it should be incorporated in the report as it is the major cause of gastritis; however, if the organism cannot be found in the specimen but has a positive serology test or urea breath test, then a diagnosis of chronic gastritis without any further qualification is warranted
- Corpus predominant gastritis and atrophy without any accompanying metaplasia or atrophy in the antrum favors the diagnosis of autoimmune gastritis; however, final diagnosis should be confirmed with a clinicopathological correlation
- Acute gastritis
- Usage of the term acute gastritis is discouraged because of the confusion between acute and active gastritis
- Special forms of gastritis
- Chemical or reactive gastritis
- Foveolar hyperplasia, mucosal oedema, smooth muscle proliferation in lamina propria with a minor increase in the inflammatory cells
- Clinical information is required to make a diagnosis (e.g., bile reflux induced gastritis, NSAID associated chemical gastritis)
- Lymphocytic gastritis
- Characterized by > 25 intraepithelial lymphocytes per 100 cells
- Usually associated with varioliform gastritis, Menetrier disease and celiac disease
- Granulomatous gastritis
- Granulomas can be seen in cases of Crohn's disease, tuberculosis, histoplasmosis, anisakiasis, sarcoidosis, etc.
- Eosinophilic gastritis
- Eosinophils are the dominant cell type with little or no increase in any other cell types
- Stomach is the most common site and infiltration is highest in antrum
- Collagenous gastritis
- Thick band of collagen beneath the surface epithelium is seen in this gastritis
- Radiation gastritis
- Characterized by necrosis of fundal glands, edema and mononuclear infiltration
- Infectious gastritis
- Mycobacterium avium intracellulare, commonly seen in HIV patients, is diagnosed by accumulation of foamy histiocytes in lamina propria and ill defined granulomas without necrosis
- Syphilitic gastritis, also seen commonly in HIV patients, is characterized by prominent mixed inflammatory infiltrate, with abundant plasma cells, mucosal ulcerations, mononuclear vasculitis of larger vessels in submucosa and muscularis mucosa
- H. heilmanii gastritis
- Rare compared with H. pylori gastritis
- More commonly seen in children as compared with adults
- Histologically shows fewer lymphoid aggregates and lesser neutrophils as compared with H. pylori
- H. heilmanii is 3.5 - 7.5 microns in size with long tight spirals
- Cytomegalovirus (CMV) gastritis
- Commonly seen in immunocompromised patients and children
- Gastric mucosa may appear normal or show erosion or shallow ulcers or pseudotumor (grossly nodular mucosa)
- Depending on the host's immune response, patients may show numerous CMV inclusions in epithelial cells, endothelial cells and macrophages with little or no inflammatory response
- Sometimes intense eosinophilic infiltration is seen, suggesting an allergic response
- Fungal gastritis
- Seen in immunocompromised subjects especially in HIV patients
- Gastric candidiasis appears as erosions with fungal hyphae lying at the base of ulcer
- Drug induced gastritis
- Iron pill gastritis due to iron intake in iron deficiency anemia shows crystalline brown pigmented material deposition, erosion, ulceration and granulation tissues
- Immune therapy induced gastritis is relatively rare but is increasingly being reported in the last 2 - 3 years
- It is most caused by anti-PD1 drugs like pembrolizumab and nivolumab administered as a single agent or in combination
- Histologically diffuse chronic active gastritis with increased lymphocytic infiltration, apoptosis are seen (Front Oncol 2023:13:1164236)
- Chemical or reactive gastritis
Diagrams / tables
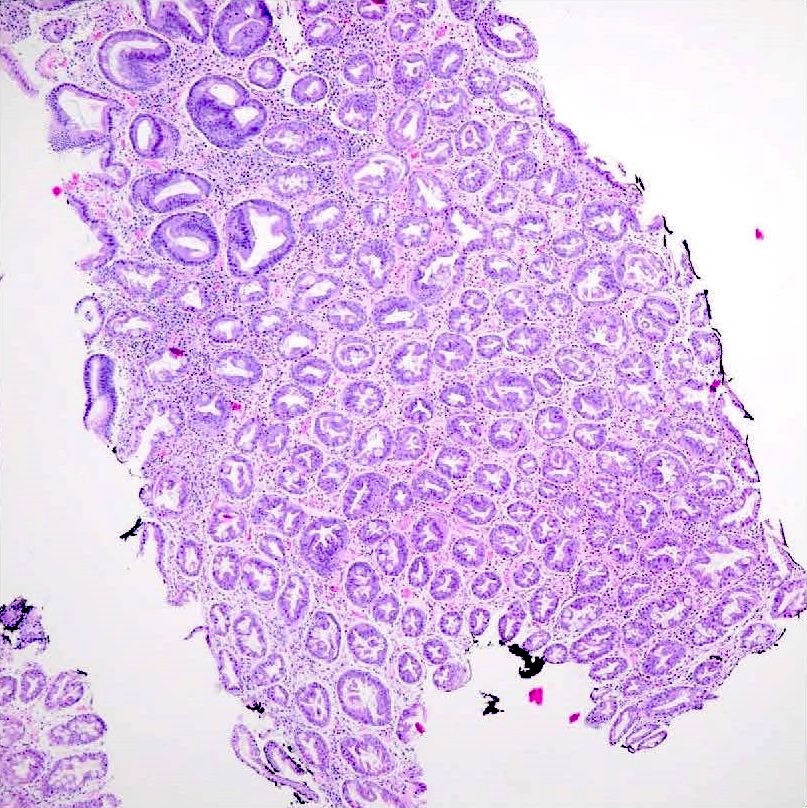
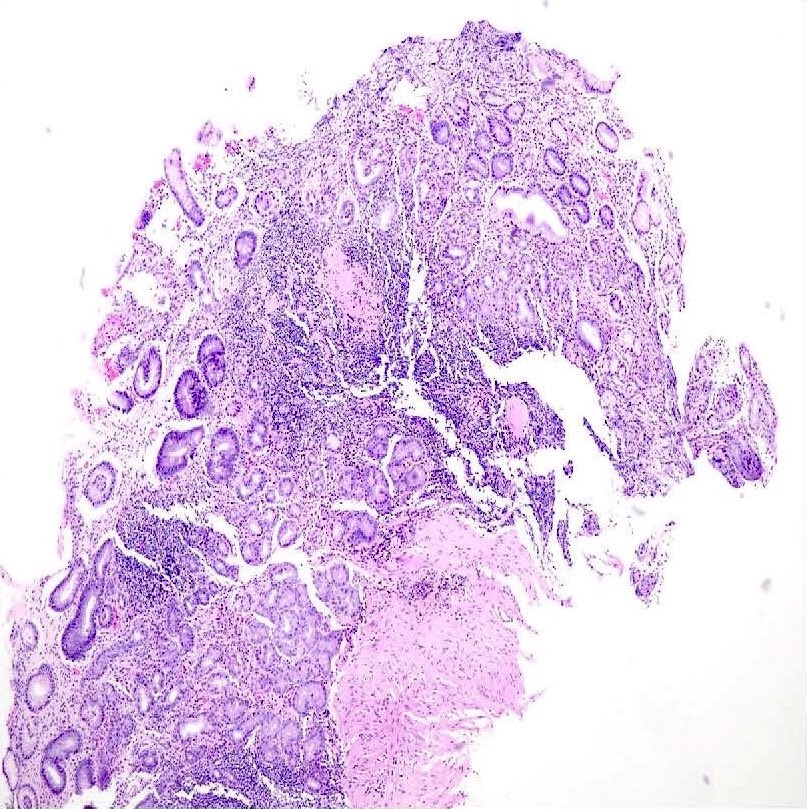
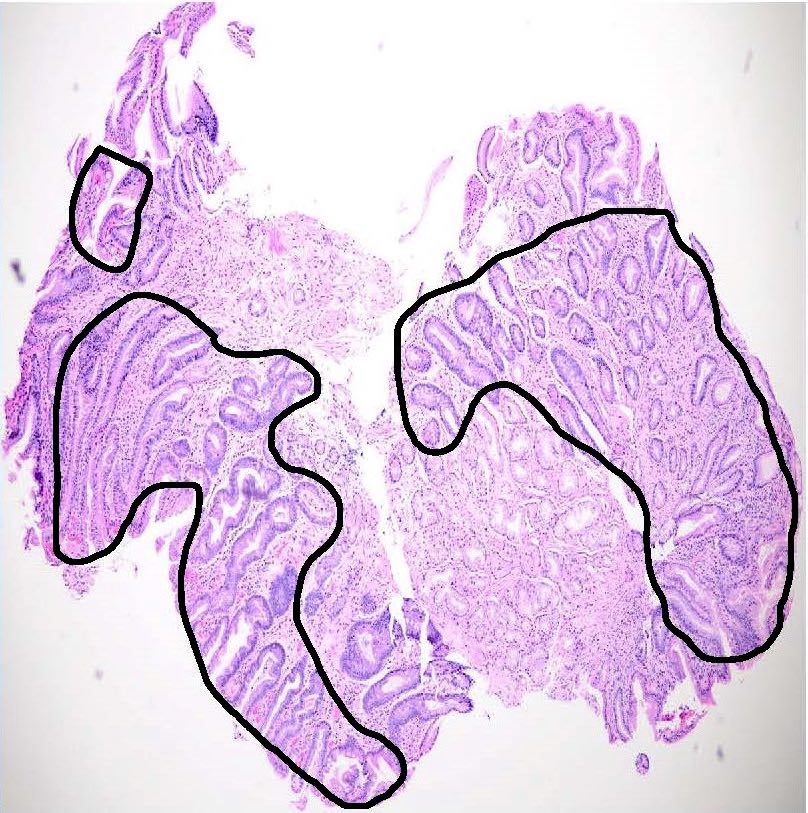
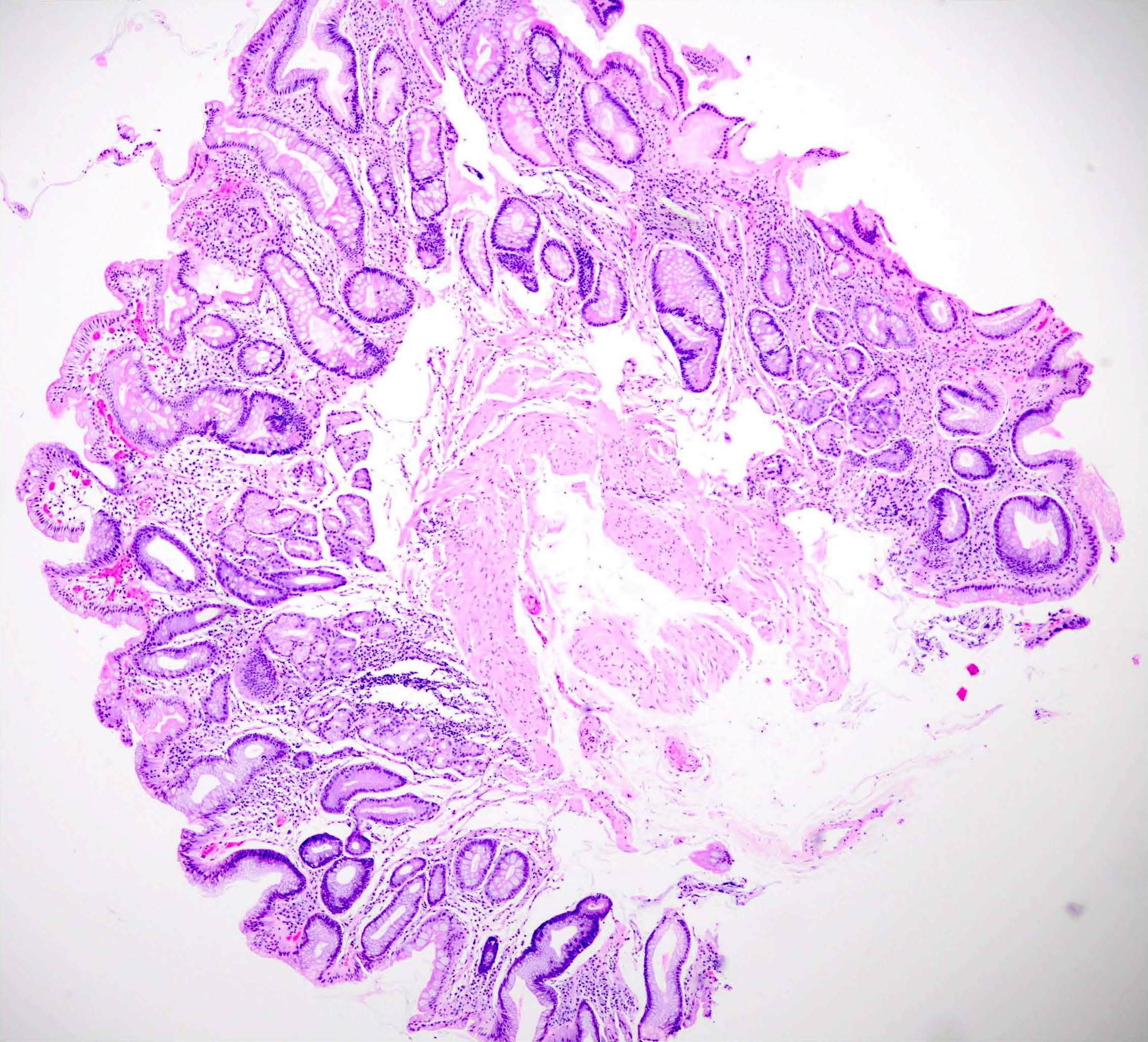
Microscopic (histologic) images
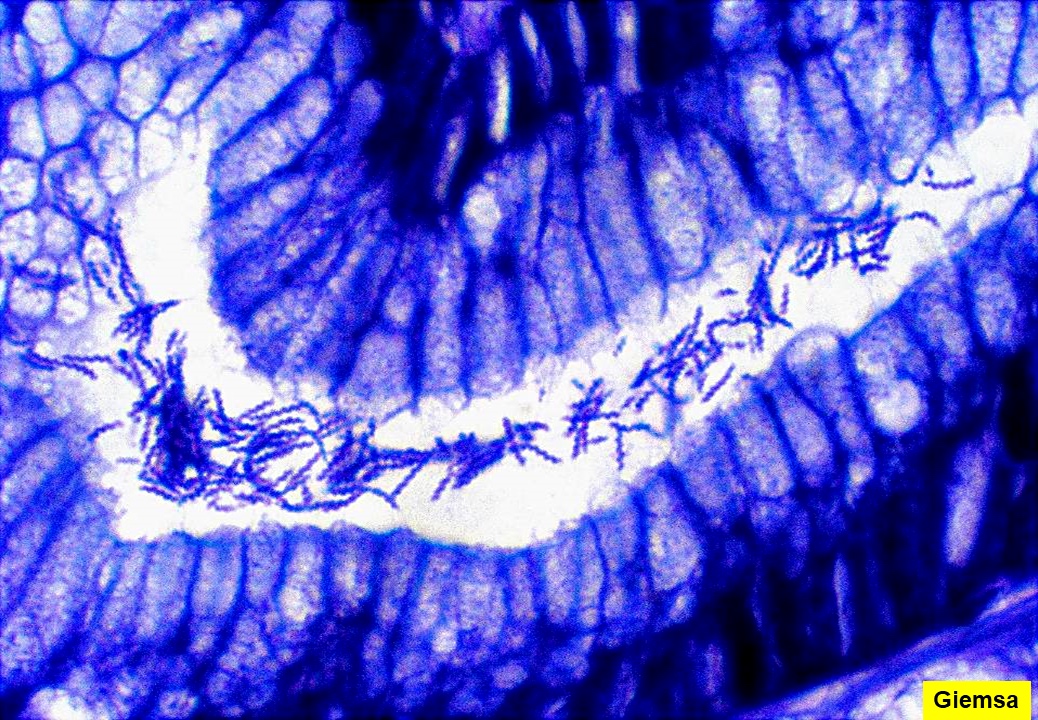
Positive stains
- Alcian blue at pH 2.5: diagnostic stain, however not routinely needed as gastric intestinal metaplasia can be readily identified in H&E; Alcian blue stains goblet cells bright blue in color due to the presence of sialomucins
- IHC for H. pylori detection offers better sensitivity and specificity than the traditional histochemical stains (Adv Anat Pathol 2020;27:193)
- Giemsa, modified Giemsa and Warthin-Starry for H. pylori and H. heilmanii detection
- Synaptophysin and chromogranin A for neuroendocrine hyperplasia
Sample pathology report
- Stomach, antral and body biopsy:
- Mild chronic gastritis with intestinal metaplasia (see comment)
- Comment: Antrum greater curve (red inked) shows mild chronic gastritis with moderate intestinal metaplasia; no evidence of H. pylori, dysplasia or malignancy. Antrum lesser curve shows mild chronic gastritis with marked intestinal metaplasia; no evidence of H. pylori, dysplasia or malignancy. Incisura (black inked) shows mild chronic gastritis with mild intestinal metaplasia; no evidence of H. pylori, dysplasia or malignancy. Body greater curve (red inked) shows mild chronic gastritis; no evidence of intestinal metaplasia, H. pylori, dysplasia or malignancy. Body lesser curve shows mild chronic gastritis with mild intestinal metaplasia; no evidence of H. pylori, dysplasia or malignancy.
Board review style question #1
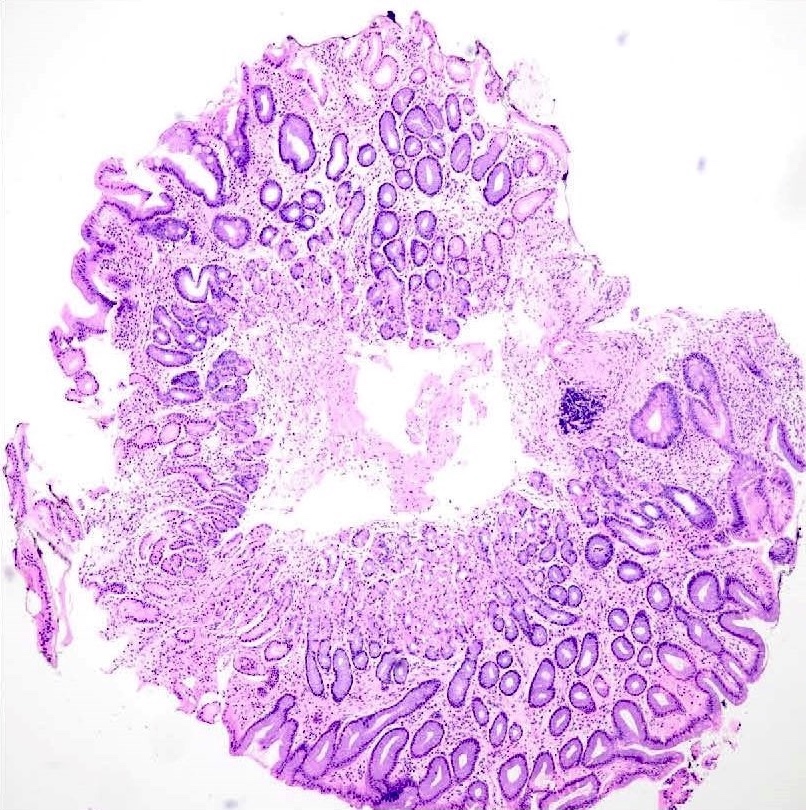
A 50 year old female working professional visited the general practitioner with complaints of fatigue, malaise and gastritis. In addition, she gave a history of diabetes since childhood. The general practitioner referred her to a gastroenterologist for endoscopic guided biopsy, which showed the picture above in the corpus. The antrum (lesser and greater curve) and incisura angularis showed features of mild chronic gastritis only. What could be the most likely diagnosis?
- Autoimmune gastritis
- Eosinophilic gastritis
- Lymphocytic gastritis
- Reactive gastropathy
Board review style answer #1
A. Autoimmune gastritis. In this context, histology likely shows features of autoimmune gastritis induced by the autoantibodies against the parietal cells and intrinsic factor leading to marked intestinal metaplasia (IM) in the body only. In addition, the patient shows features of anemia (fatigue and malaise) and associated autoimmune disorder (type 1 diabetes) which are features associated with autoimmune gastritis. Further laboratory work up is warranted to confirm the diagnosis. Answer C is incorrect because lymphocytic gastritis occurs in association with celiac disease and shows increased intraepithelial lymphocytes with expanded lamina propria. Answer B is incorrect because eosinophilic gastritis is associated with allergies, hay fever and often eczema with > 30 eosinophils per high power field. Answer D is incorrect as reactive gastropathy shows foveolar hyperplasia with corkscrew appearance of the gastric glands.
Comment Here
Reference: Gastritis-features to report
Comment Here
Reference: Gastritis-features to report
Board review style question #2
A 58 year old man had symptoms of reflux and a dull pain in the epigastrium for the past few days. He went to the general practitioner who referred him to a gastroenterologist for endoscopy and biopsy. Histology showed marked intestinal metaplasia (IM) (80%, 65% and 70%) in antrum lesser, greater curve and incisura respectively and mild IM (25%) in the body lesser curve. What would be the OLGIM stage for this patient?
- OLGIM I
- OLGIM II
- OLGIM III
- OLGIM IV
Board review style answer #2
C. OLGIM III. Answers A, B and D are incorrect because the stage in this patient is OLGIM III.The average intestinal metaplasia (IM) in antrum is (80+65+70/3) 72%. Average IM in body is (0+25/2) 12.5%. Using the OLGIM chart, the patient has marked IM (grade 3) in antrum and mild IM (grade I) in body; hence, he has stage III OLGIM. Patients with OLGIM stage III or IV have a higher risk of progression to gastric cancer. The ESGE 2019 and Academy of Medicine, Singapore clinical guidelines recommend endoscopic surveillance every 3 years for such patients.
Comment Here
Reference: Gastritis-features to report
Comment Here
Reference: Gastritis-features to report