Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Satturwar S, Aly FZ. Thyroid follicular nodular disease (multinodular goiter). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidnodular.html. Accessed April 24th, 2024.
Definition / general
- Most common disease of thyroid gland
- Diffuse or nodular enlargement with distorted outer surface
- Grossly visible mass / nodule in 10% of thyroid glands at autopsy but microscopic nodularity is present in 40%
- 3 - 5% risk of thyroid cancer, predominantly follicular variant of papillary thyroid carcinoma or up to 17.5% with papillary microcarcinoma (S Afr J Surg 2014;52:5, Int J Surg Open 2018;15:18)
Essential features
- Majority asymptomatic and euthyroid
- Asymmetric diffuse or nodular enlargement of thyroid gland with distorted outer surface
- Iodine deficiency is most common cause worldwide; however, in the U.S., most goiters are due to autoimmune thyroiditis (i.e. Hashimoto disease) (Endotext: Multinodular Goiter [Accessed 23 December 2020])
- Histologically, multiple variably sized dilated follicles lined by flattened to hyperplastic epithelium, with or without degenerative changes
Terminology
- Goiter is clinical term meaning enlarged thyroid, which can be either diffuse or nodular (e.g. multinodular or solitary / dominant nodule)
- Appropriate morphological term is nodular / multinodular hyperplasia
- Synonyms: adenomatous / adenomatoid hyperplasia / nodule, colloid goiter, simple goiter, colloid / hyperplastic nodule
- Simple goiter: also called diffuse nontoxic goiter or colloid goiter
- Thyroid gland usually 40 g or more
- Eventually converts into multinodular goiter
- Multinodular goiter: irregular enlargement of thyroid gland due to repeated episodes of hyperplasia and involution (degeneration) of simple goiter
- Thyroid gland often 100 g or more; may resemble a neoplasm, particularly if a single firm dominant nodule is present
- Nodules are clonal or polyclonal and are due to heterogeneous responses of follicular epithelium to TSH
- Nontoxic goiter: no hyperthyroidism present
ICD coding
- ICD-10: E04.2 - nontoxic multinodular goiter
Epidemiology
- 90% of those affected are women (F > > > M)
- Variable age; develops more frequently during adolescence and pregnancy
Sites
- Involves entire thyroid gland
Etiology
- Increase in TSH secretion is the main cause in iodine deficiency related goiter and in autoimmune (Hashimoto) thyroiditis; in persons with normal TSH, oxidative damage to follicular cells and then damage to DNA leads to hyperplasia
- In individuals with normal TSH, thyroid enlargement is caused by multiple growth factors, including TSH
- Genetic factors:
- DICER1 syndrome: germline mutations in DICER1 gene in familial and childhood multinodular goiter (J Clin Endocrinol Metab 2016;101:1, Head Neck 2013;35:E369); patients also at increased risk of Sertoli-Leydig cell tumor, cystic nephroma and pleuropulmonary blastoma
- PTEN hamartoma tumor syndrome: autosomal dominant disorder with germline mutation of PTEN tumor suppressor gene manifesting as multiple carcinomas and hamartomas in variety of organs, including thyroid, presenting with multinodular goiter (J Clin Endocrinol Metab 2011;96:34, Thyroid 2011;21:135)
- Promoter hypermethylation of tumor suppressor gene RASSF1A: (Ras association domain family 1 isoform A) is a tumor suppressor gene whose inactivation is implicated in the development of many human cancers
- Promoter hypermethylation leads to loss of function of RASSF1A
- Other ways it can get inactivated is by gene deletion or point mutations (JAMA Surg 2014;149:1146)
- Some nodules eventually become autonomous due to activating mutations in the TSH receptor or G proteins within the thyroid follicular cells
- Drug induced goiter: sulfonamides and phenylbutazone inhibit organification of iodine
- Iodine containing drugs such as amiodarone interfere with thyroglobulin proteolysis
- Iodine or lithium interfere with thyroglobulin breakdown and release of T3 / T4
- Goitrogens: cassava, cabbage, cauliflower, Brussels sprouts and turnips interfere with T3 / T4 synthesis
- Cassava contains a thiocyanate which inhibits iodide transport within the thyroid
- Hereditary: see dyshormonogenetic goiter
- Plummer syndrome: hyperfunctioning thyroid nodule within a goiter, without ophthalmopathy or dermopathy of Graves disease
- Plummer-Vinson (Paterson-Kelly) syndrome: iron deficiency anemia, glossitis, esophageal dysphasia related to webs, may have thyroid enlargement (Orphanet J Rare Dis 2006;1:36)
Clinical features
- Thyroid enlargement (goiter); neck mass
- Majority asymptomatic and euthyroid
- Hypothyroidism due to decreased production of T3 and T4 hormones
- Hyperthyroidism due to autonomous transformation
- Pressure symptoms due to compression of trachea and esophagus (uncommon since enlargement is mainly towards strap muscle and subcutaneous tissue); compression of recurrent laryngeal nerve with hoarseness, phrenic nerve paralysis and Horner syndrome
- Subacute obstructive symptoms with or without pain due to secondary hemorrhage into a nodule
- Exertional dyspnea when tracheal diameter is less than 8 mm with stridor or wheezing when the diameter is less than 5 mm
- References: Otolaryngol Clin North Am. 2003;36:35, BMC Emerg Med 2019;19:18, J Endocrinol Invest 2016;39:357
Diagnosis
- Clinical examination
- Thyroid function tests: TSH, T3, T4
- Thyroid peroxidase antibodies
- Thyroid ultrasound
- CT or MRI to evaluate extent of goiter
- Fine needle aspiration is indicated if:
- History of rapid growth
- Pain or tenderness
- Unusually firm areas in the nodule
- Suspicious sonographic features
Laboratory
- Usually normal T3 / T4, TSH, normal radioactive iodine uptake, thyroglobulin may be elevated
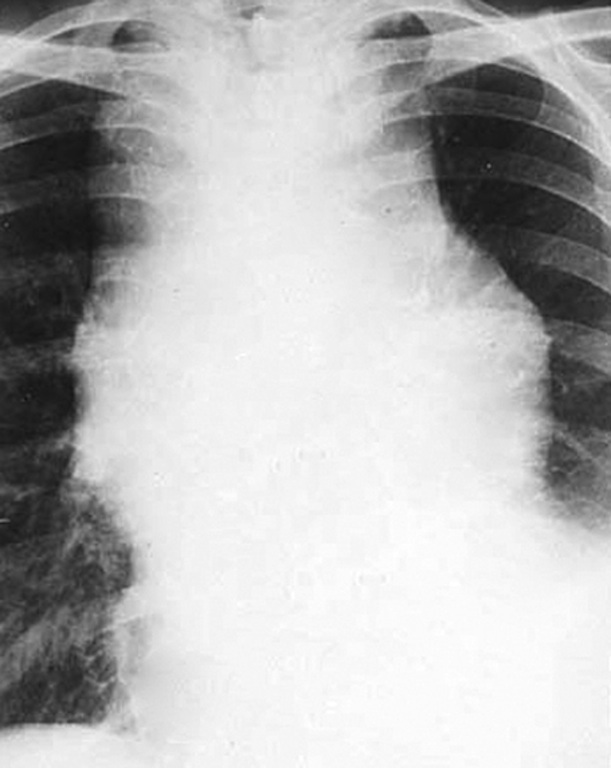
Radiology description
- Upper limits of normal for thyroid gland volume:
- Adult men: 25 mL
- Adult women: 18 mL
- 13 - 14 years: 8 - 10 mL
- 3 - 4 years: 3 mL
- Neonate: 0.8 - 1.5 mL
- Ultrasound:
- Wide variety of appearances which include:
- Enlarged iso / hyperechoic gland with surrounding hypoechoic halo
- Sponge-like / honeycomb pattern
- Anechoic areas may contain colloid
- Internal calcification
- Wide variety of appearances which include:
- Nuclear medicine:
- 99mTc pertechnetate or radioiodine (123I) demonstrate an enlarged gland, with heterogeneous uptake
- References: Horm Metab Res 2004;36:645, Clin Endocrinol (Oxf) 1987;26:273
Prognostic factors
- Size
- Excellent prognosis with either surgery or radioiodine therapy, depending on comorbidities
Case reports
- 31 year old pregnant woman with cervical goiter developing acute respiratory failure (BMC Emerg Med 2019;19:18)
- 48 year old woman with rapid enlargement of a preexisting goiter due to disseminating tuberculosis (Case Rep Endocrinol 2018;2018:4369531)
- 51 year old woman with intrathoracic goiter who needed sternotomy for excision (Asian Cardiovasc Thorac Ann 2016;24:207)
- 56 year old woman with airway obstruction (Tokai J Exp Clin Med 2016;41:181)
- 63 year old woman with hemorrhage of goiter causing acute respiratory distress (Medicine (Baltimore) 2016;95:e2777)
- 78 year old man with giant goiter (J Endocr Soc 2018;2:290)
Treatment
- Asymptomatic, euthyroid patients with multinodular goiters (< 80 mL): monitor by annual neck exam, TSH level and thyroid ultrasound as required
- For very large goiters (> 80 - 100 mL) or goiters that continue to grow: thyroidectomy
- Nontoxic goiters that continue to grow in poor surgical candidates or those who prefer to avoid surgery: radioiodine therapy
- References: J Endocrinol Invest 2016;39:357, World J Surg 2008;32:1301, Endokrynol Pol 2015;66:301, J Endocrinol Invest 2001;24:820
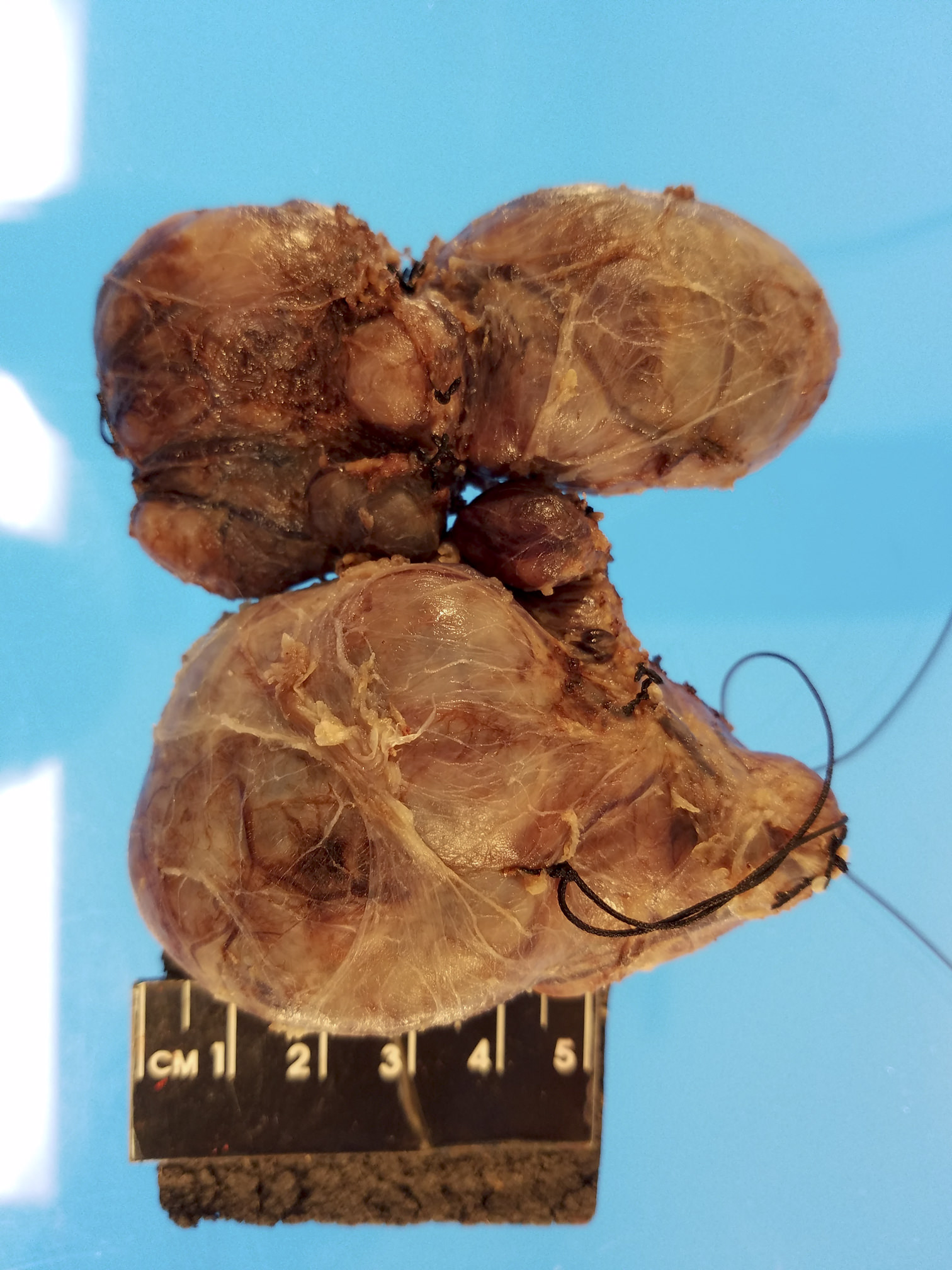
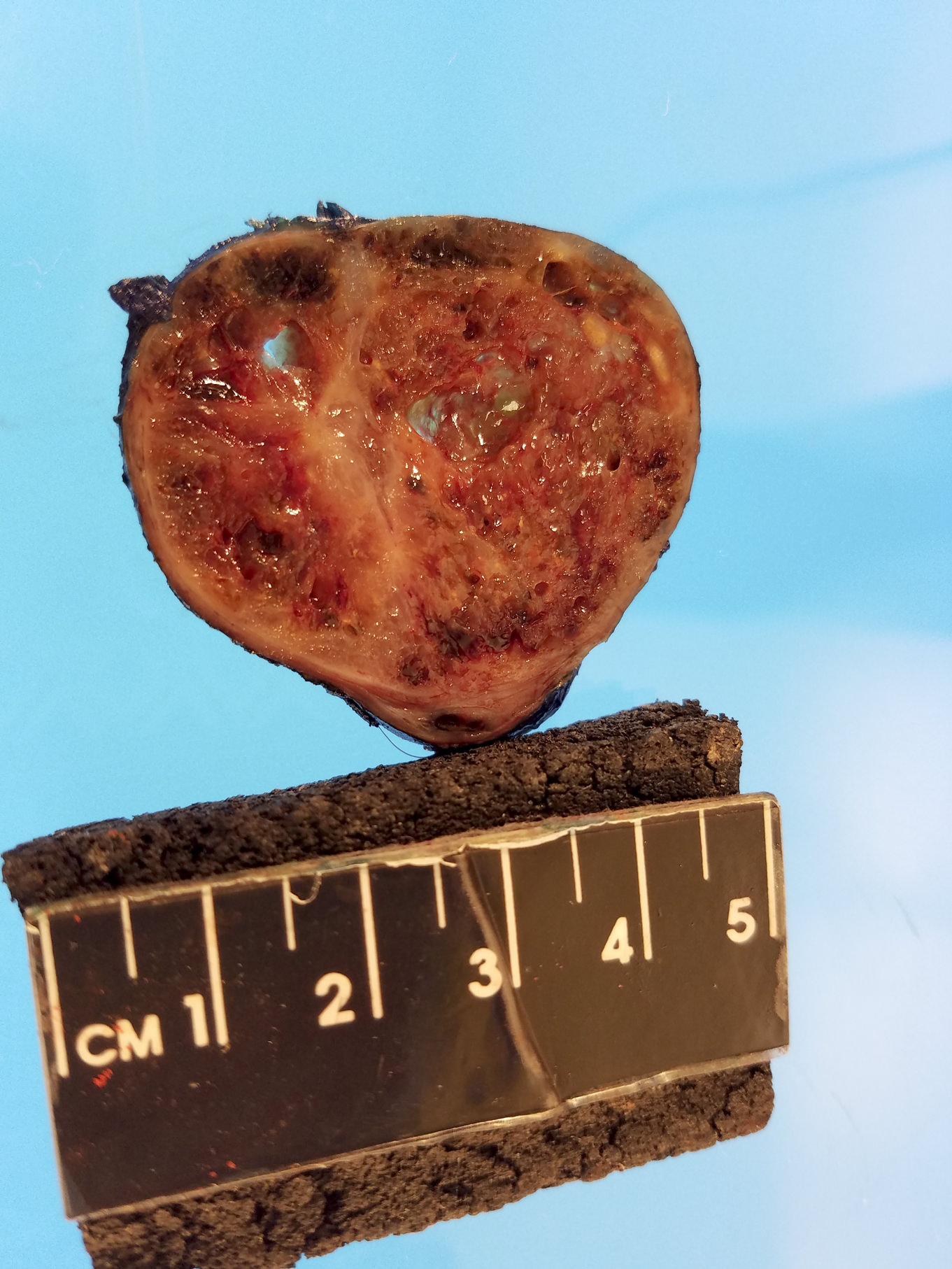
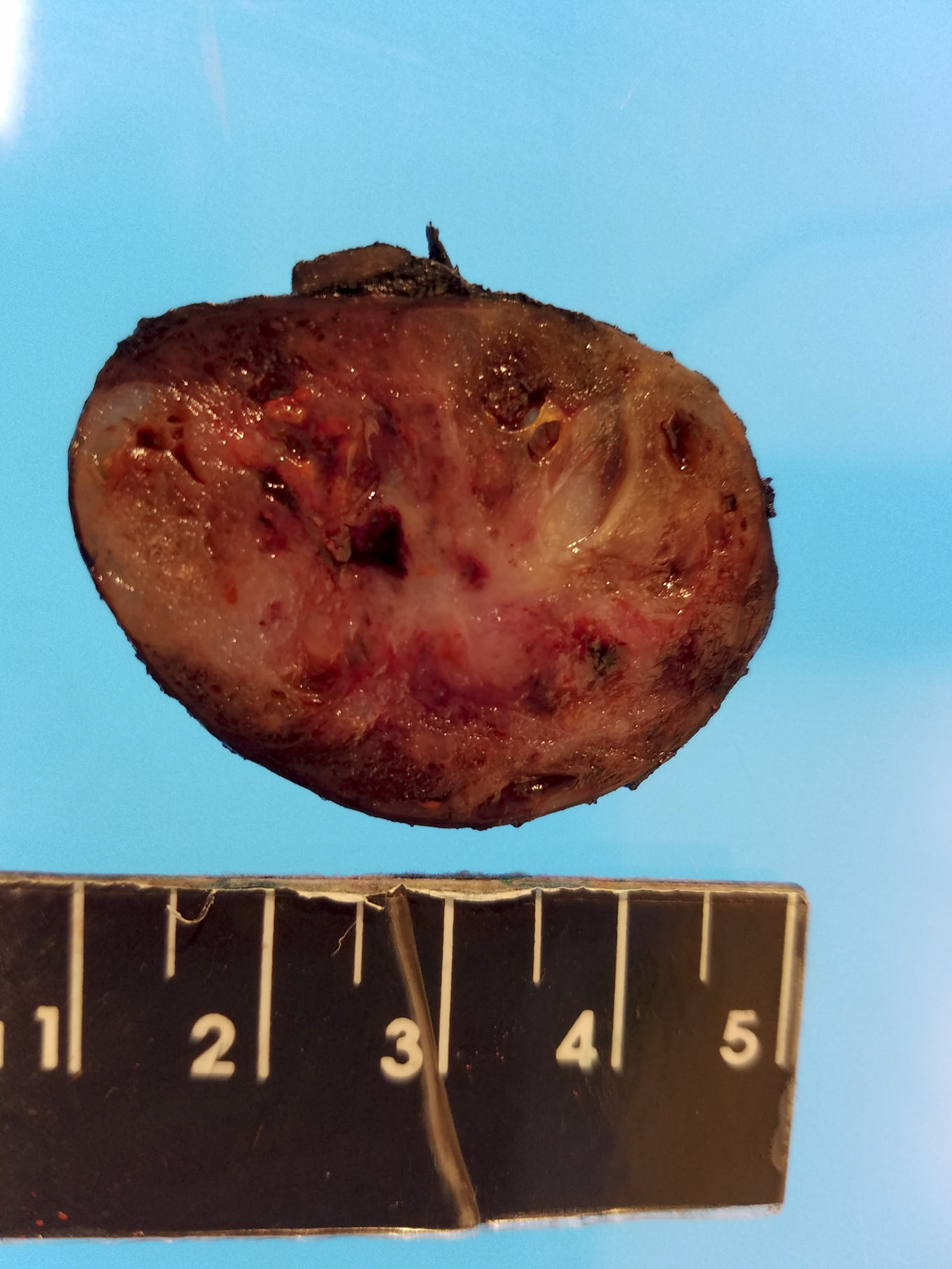
Gross description
- Simple goiters are usually firm with amber cut surface
- Multinodular goiters are asymmetric, large, 200 - 700 g (up to 2 kg)
- Increased size: lobe 8 - 15 cm, dominant nodules up to 10 cm
- Nodular and bumpy outer surface and variegated cut surface, cystic and hemorrhagic with brown gelatinous colloid nodules with focal calcification
- Reference: Diagn Cytopathol 2007;35:579
Gross images
Contributed by Swati Satturwar, M.D. and Andrey Bychkov, M.D., Ph.D.
AFIP images
Images hosted on other servers:
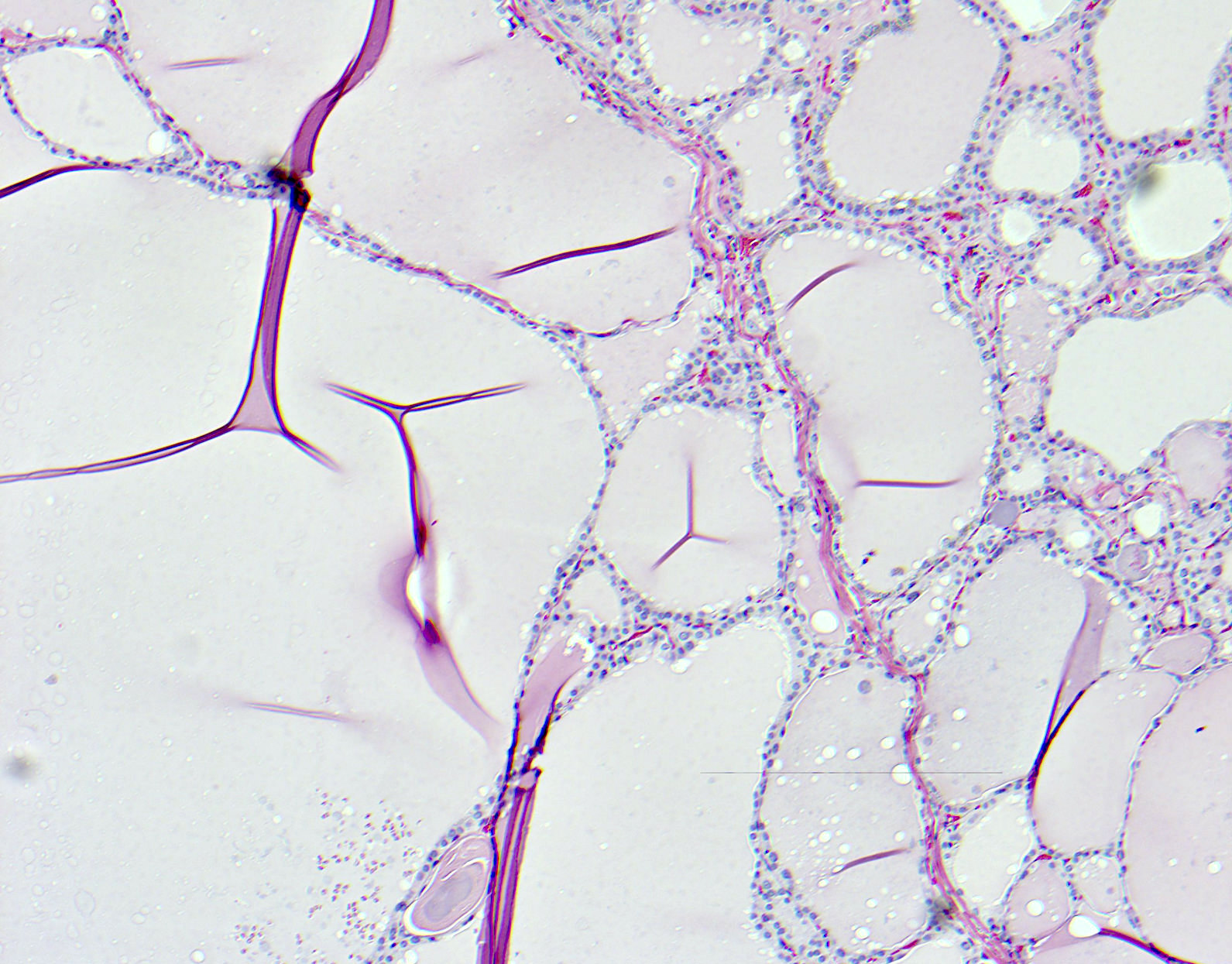
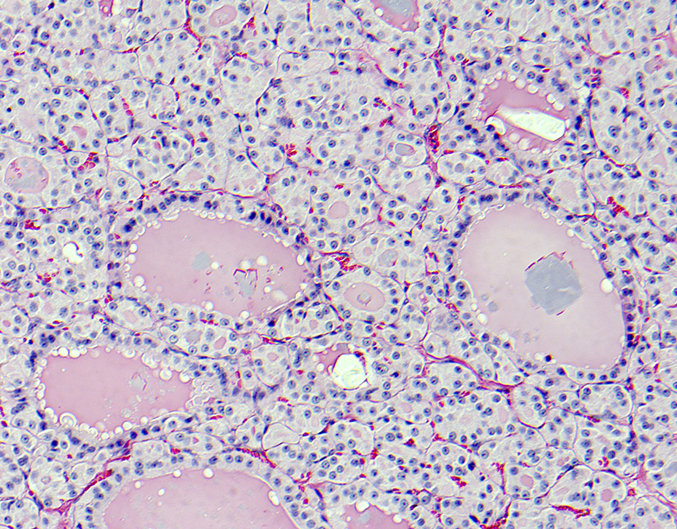
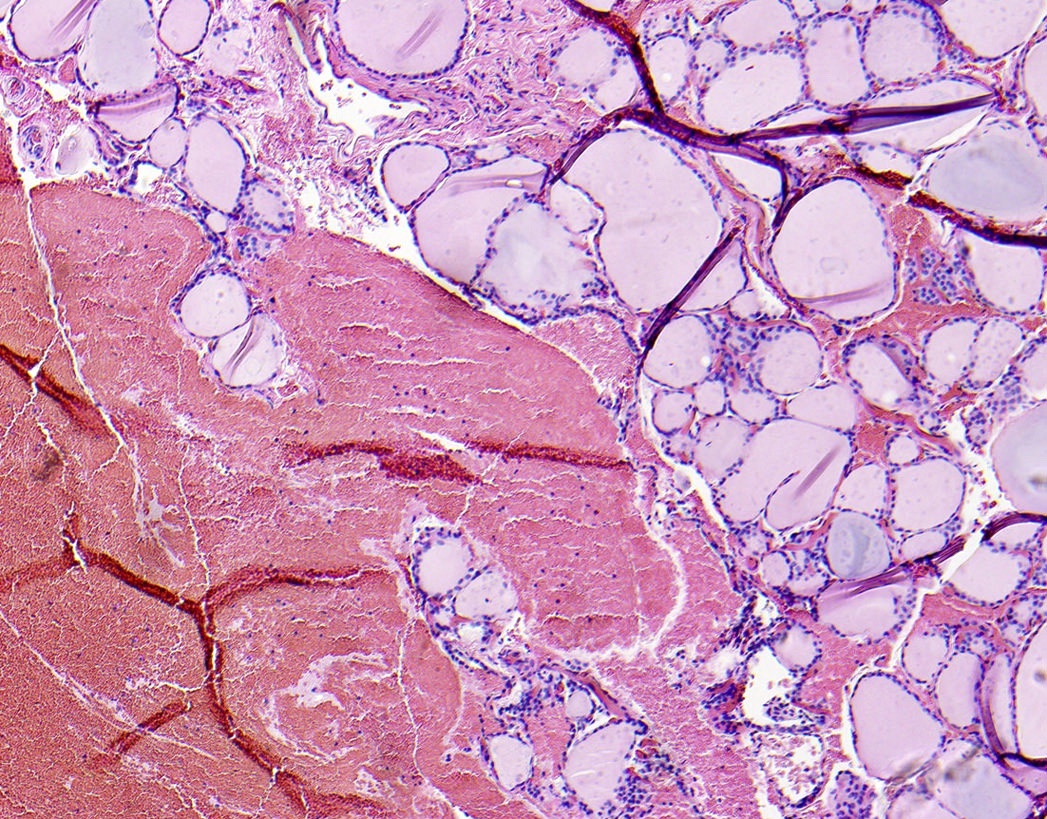
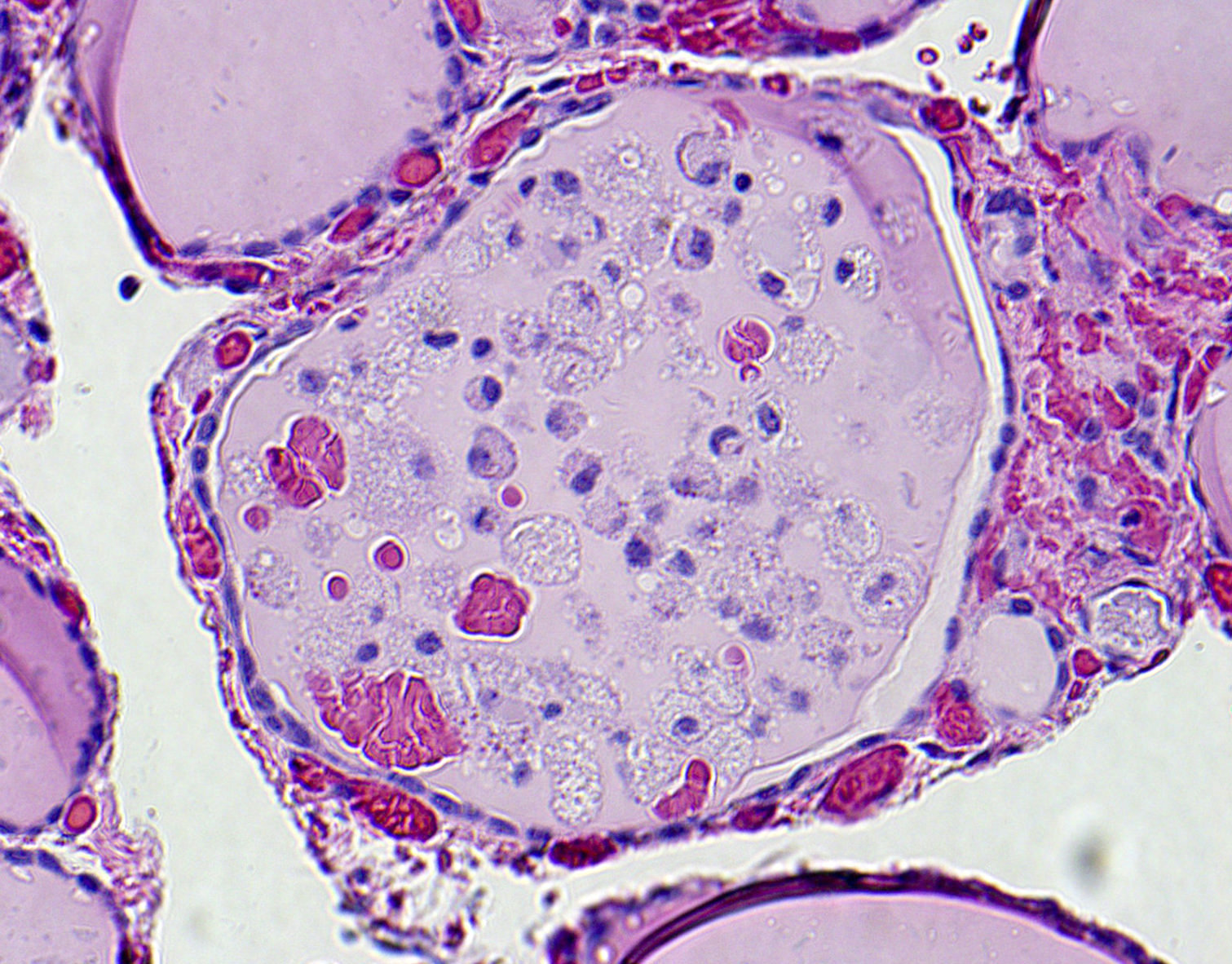
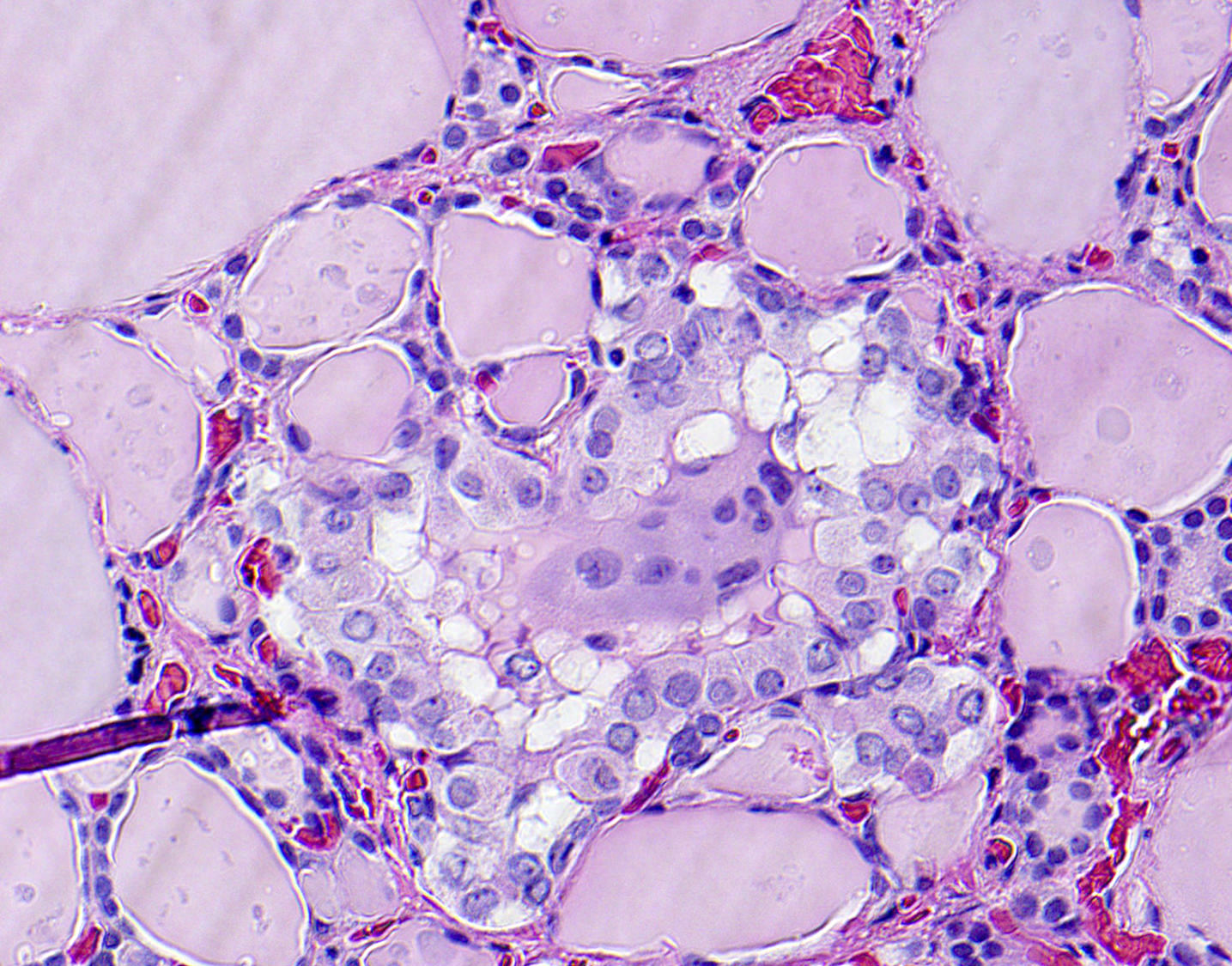
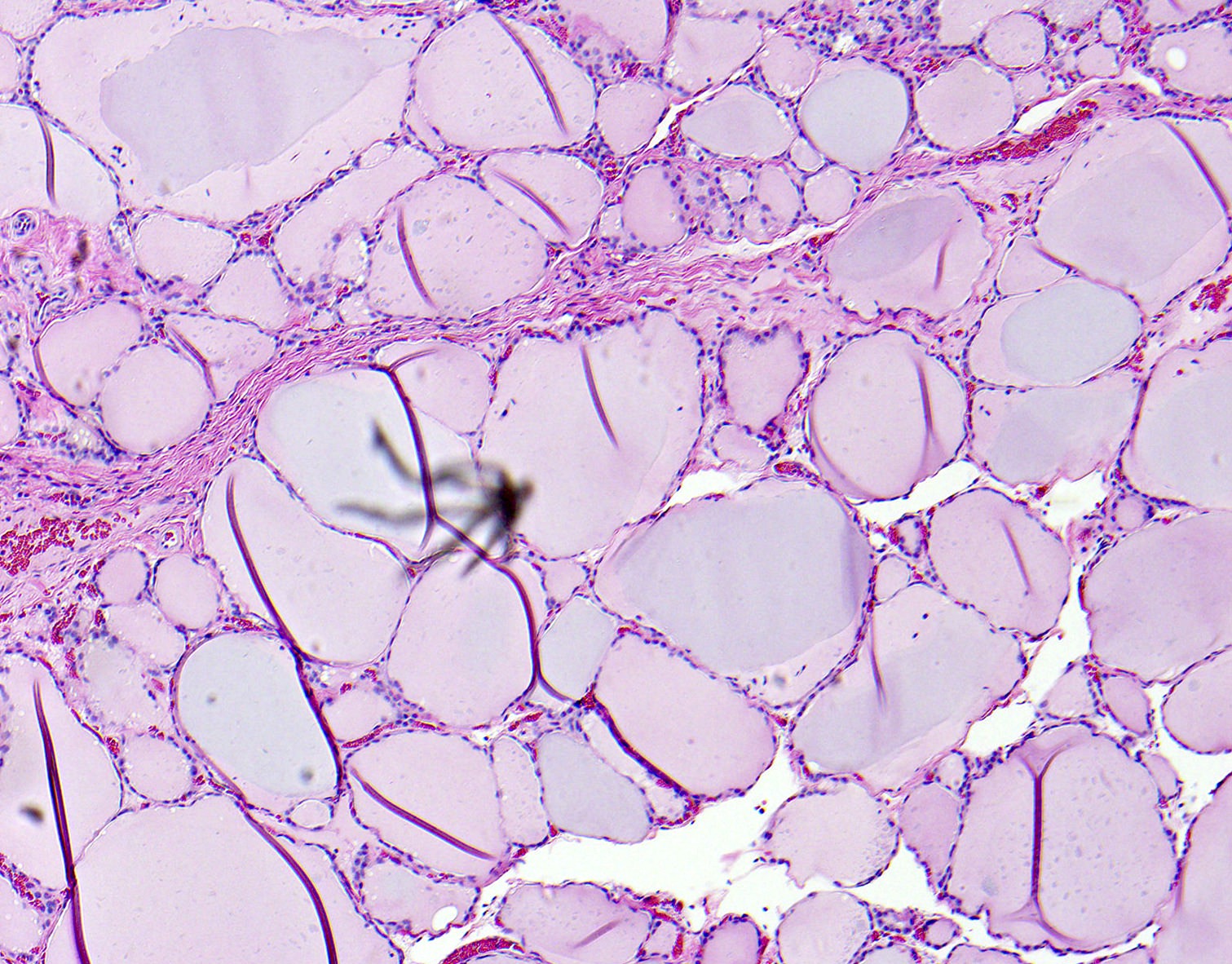
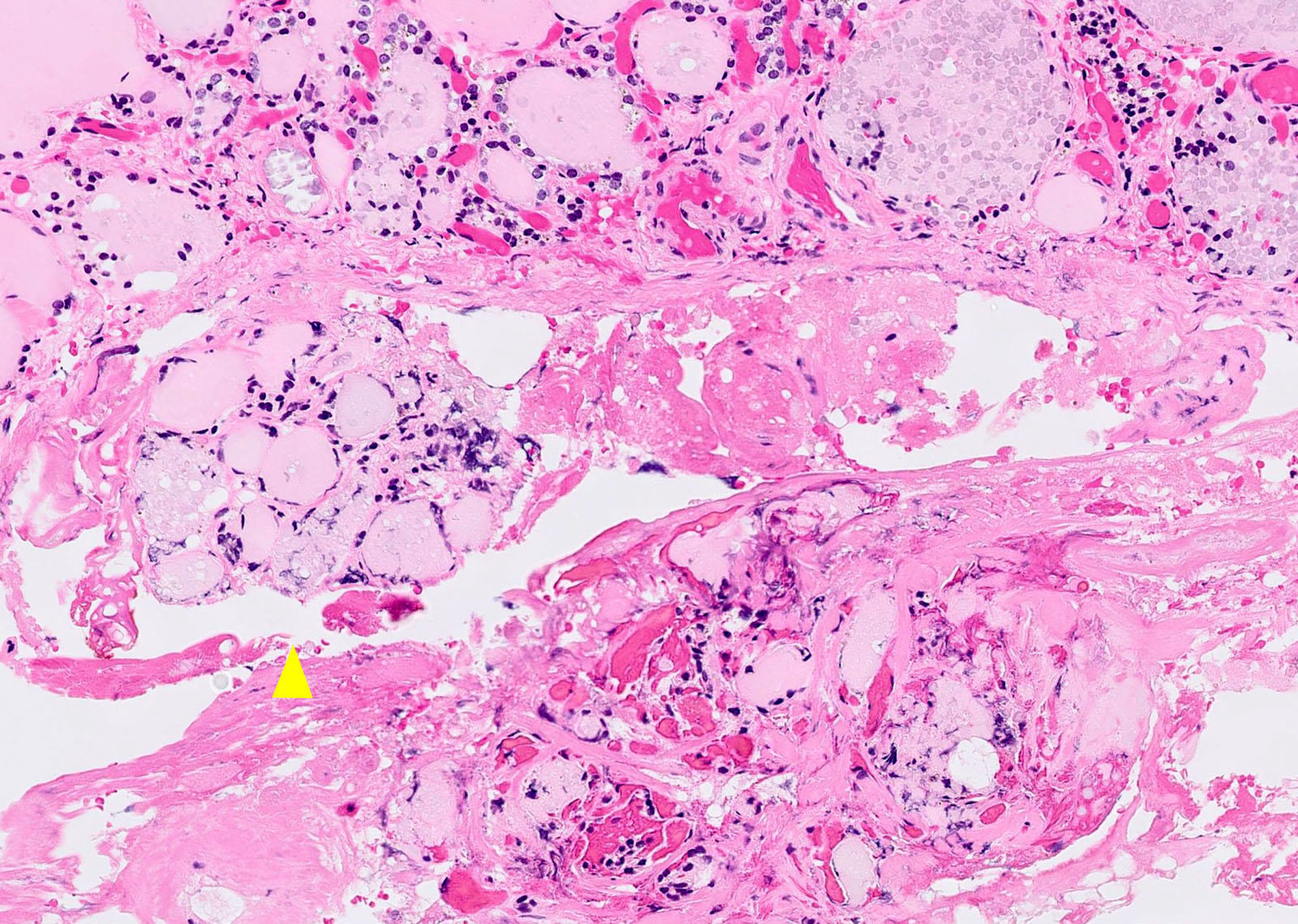
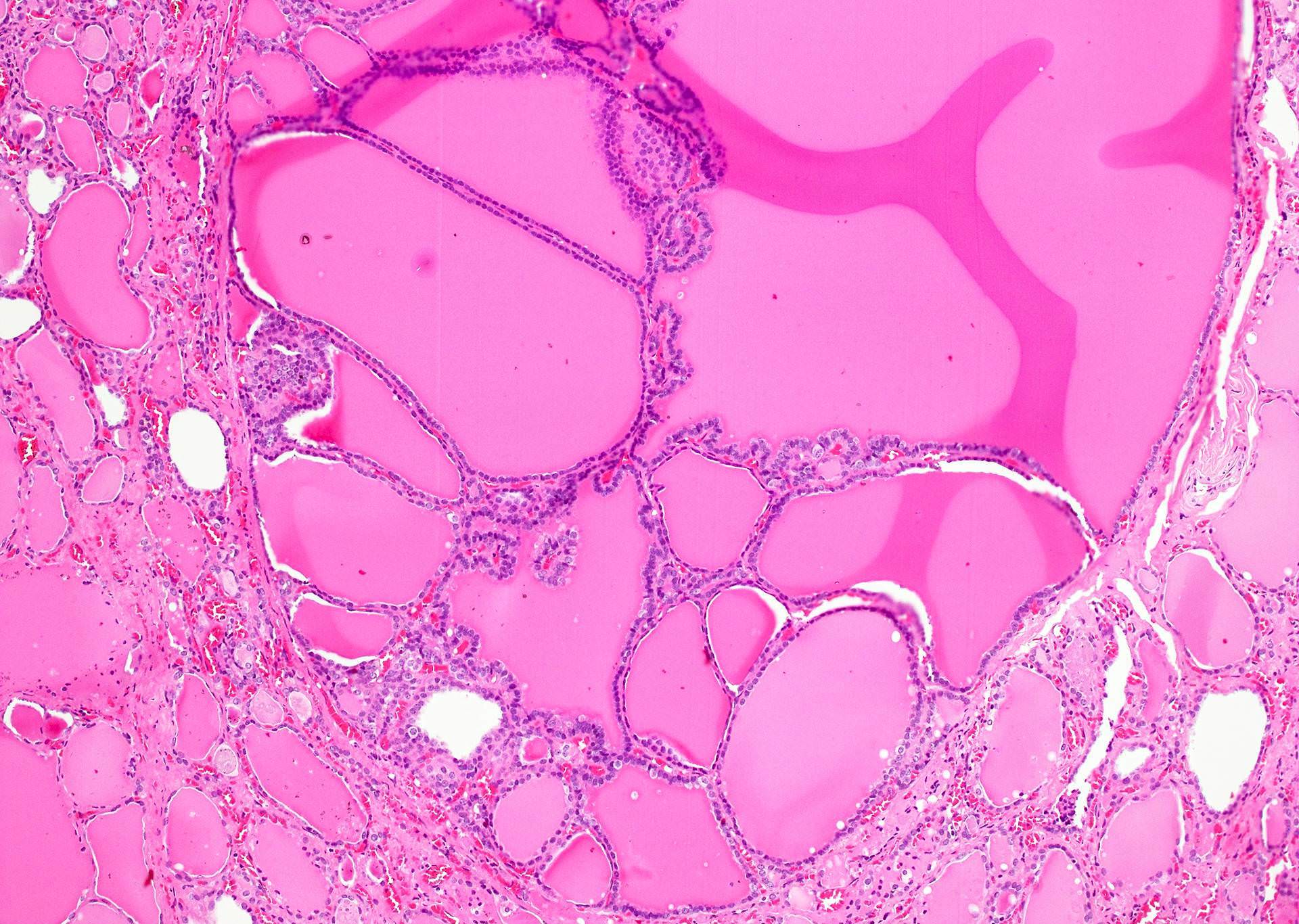
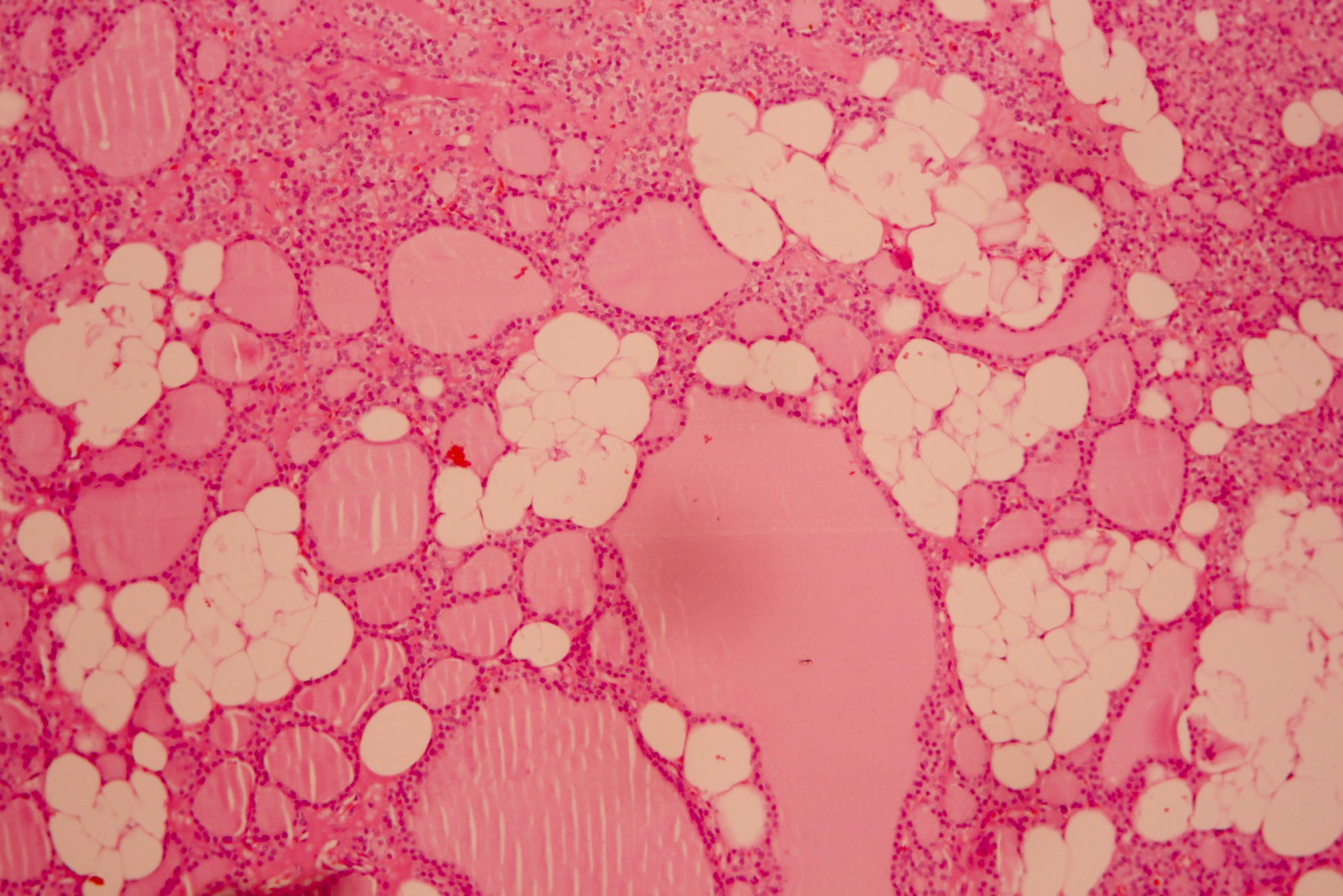
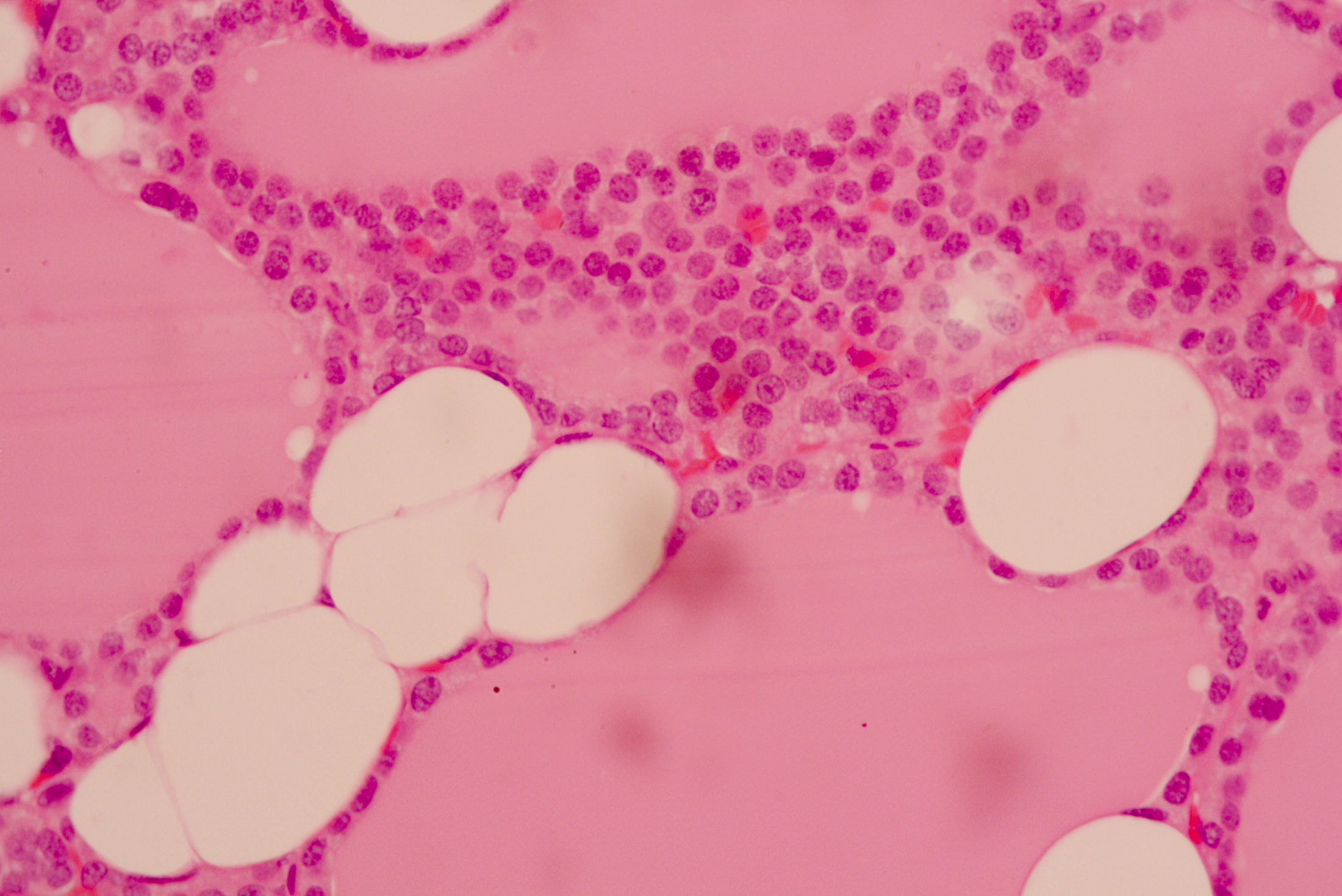
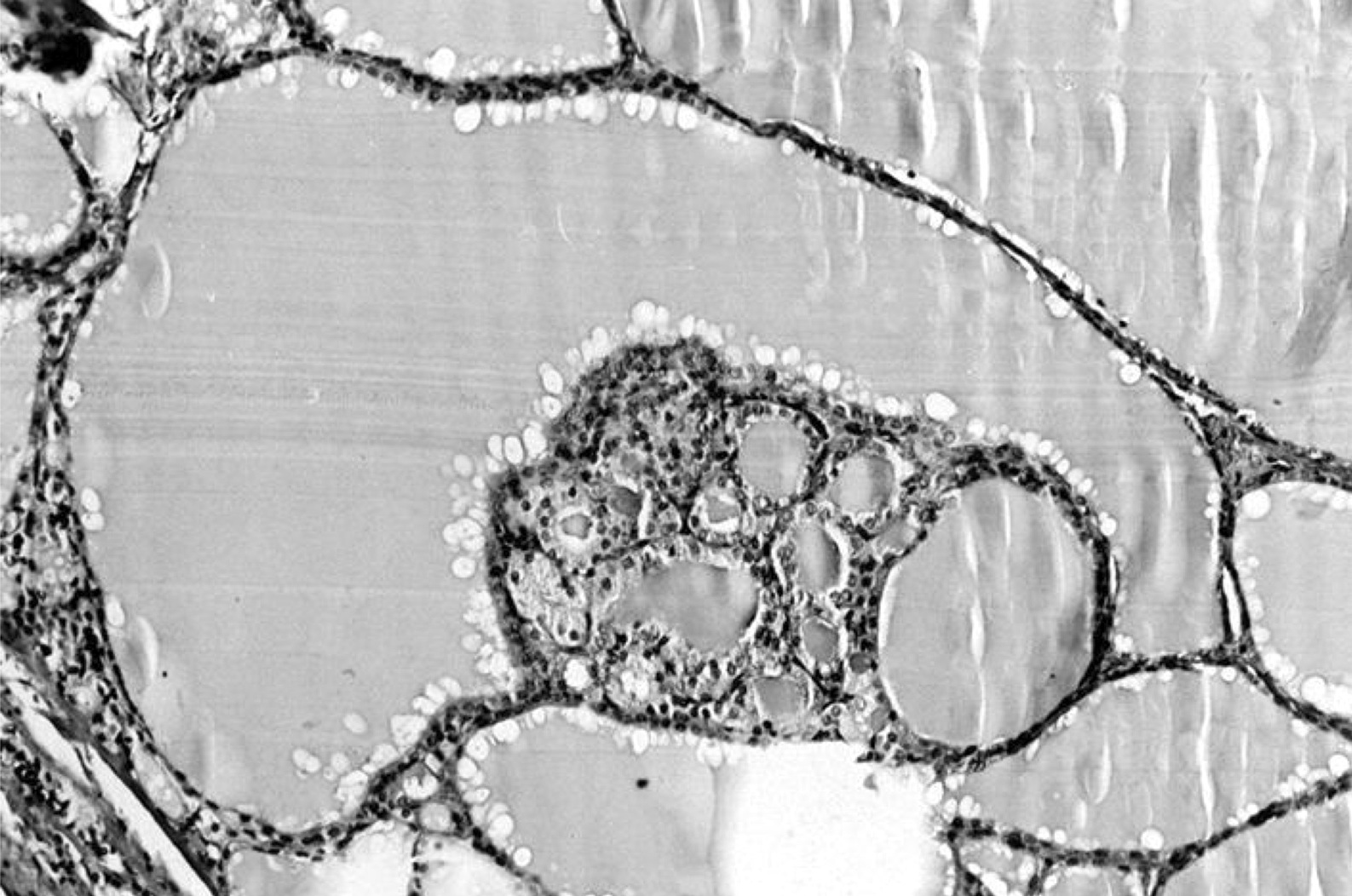
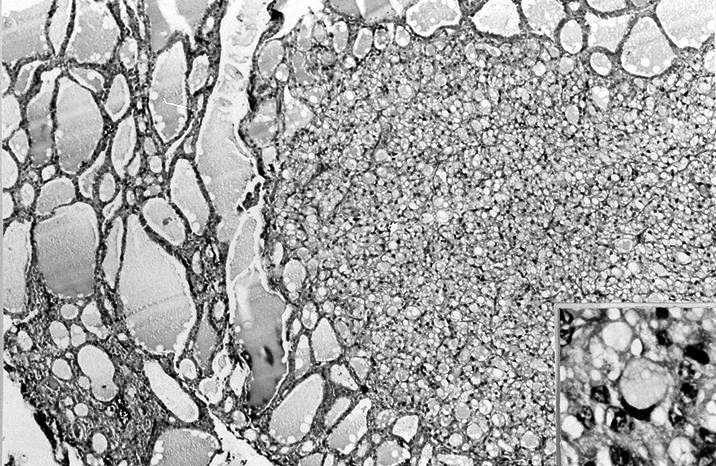
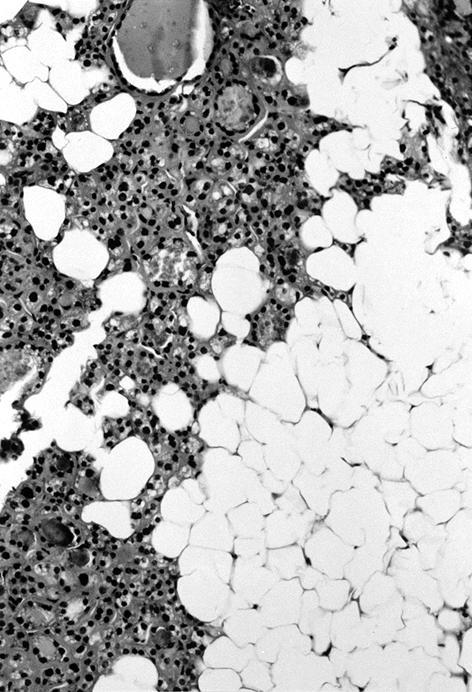
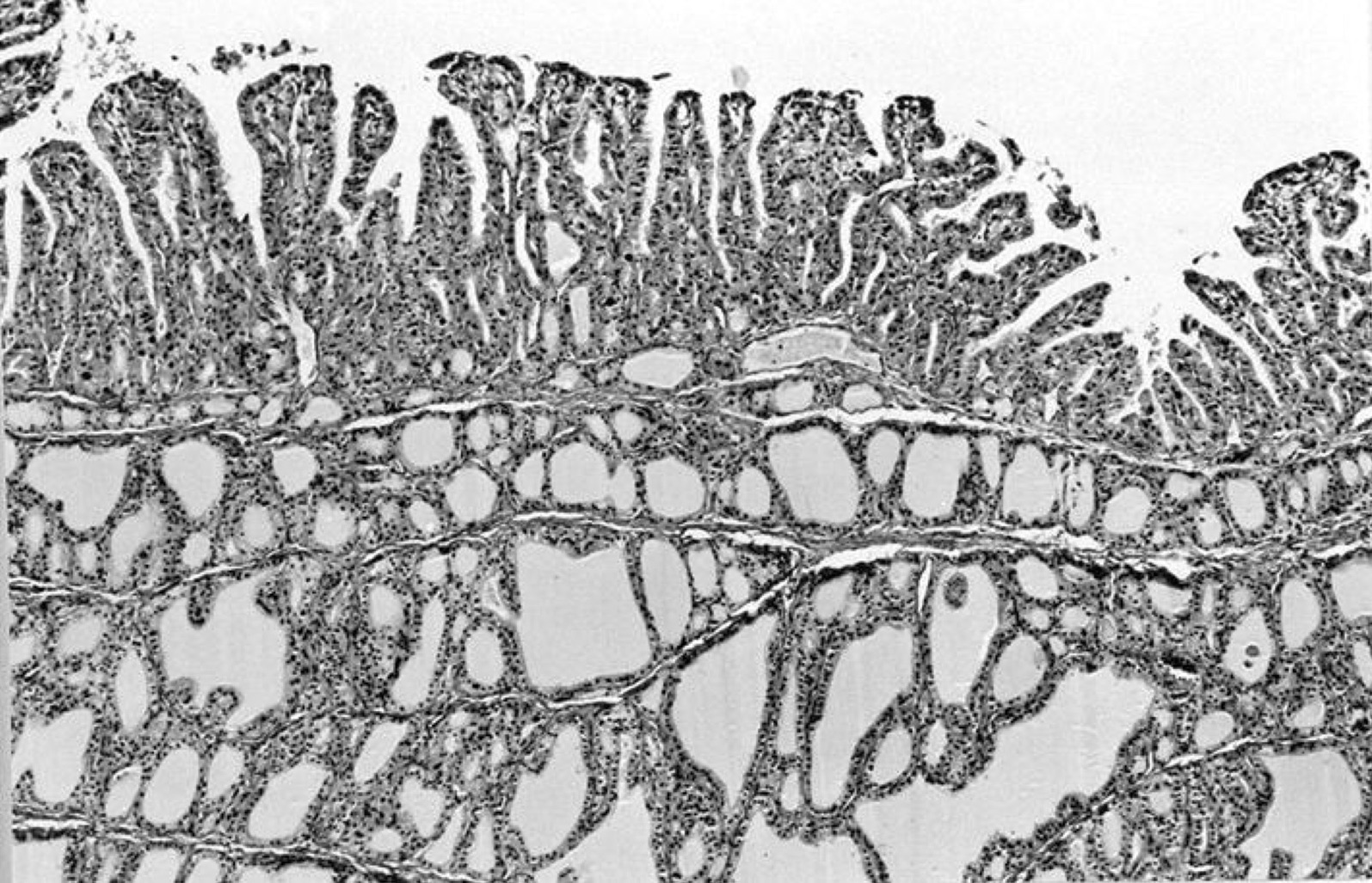
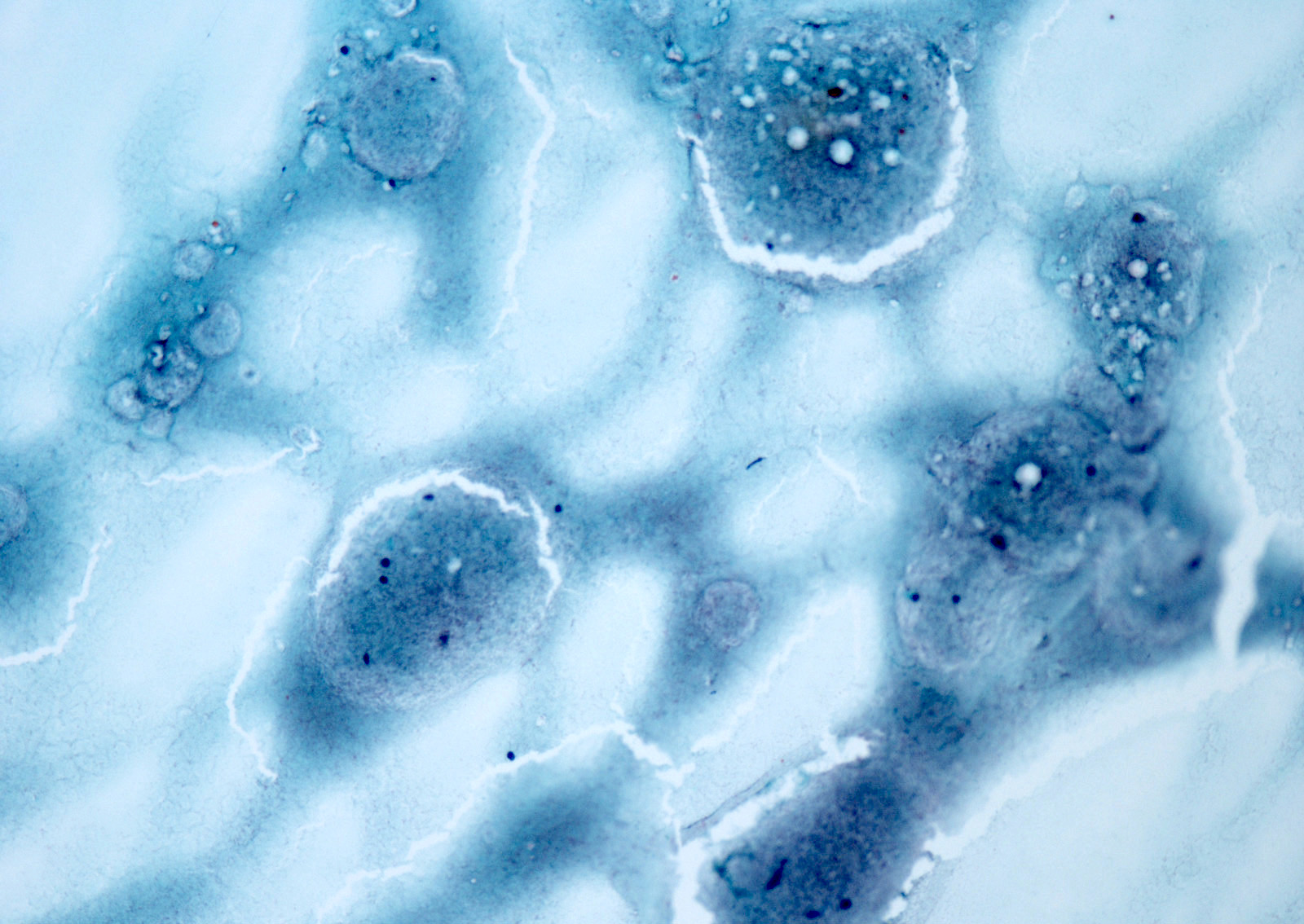
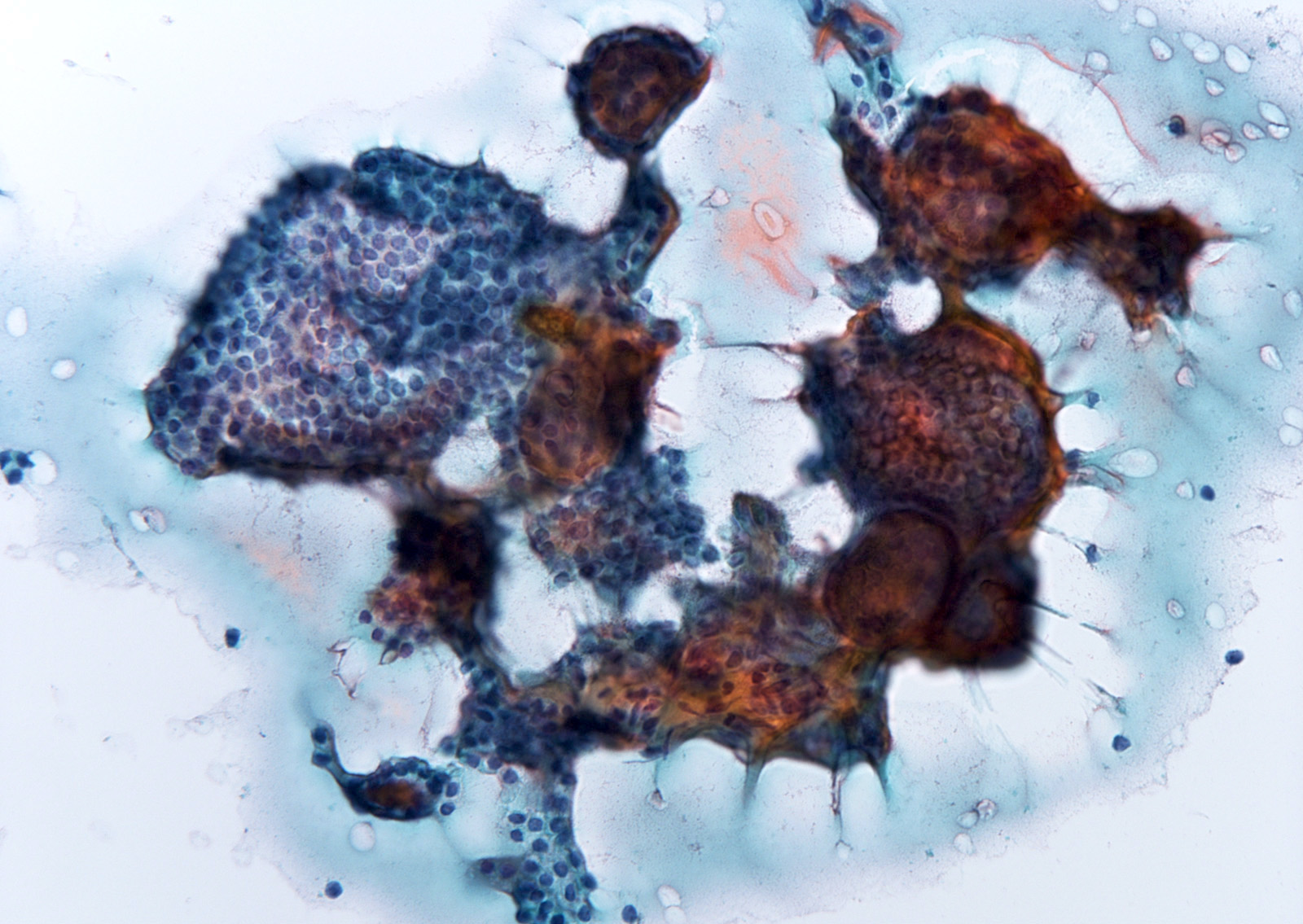
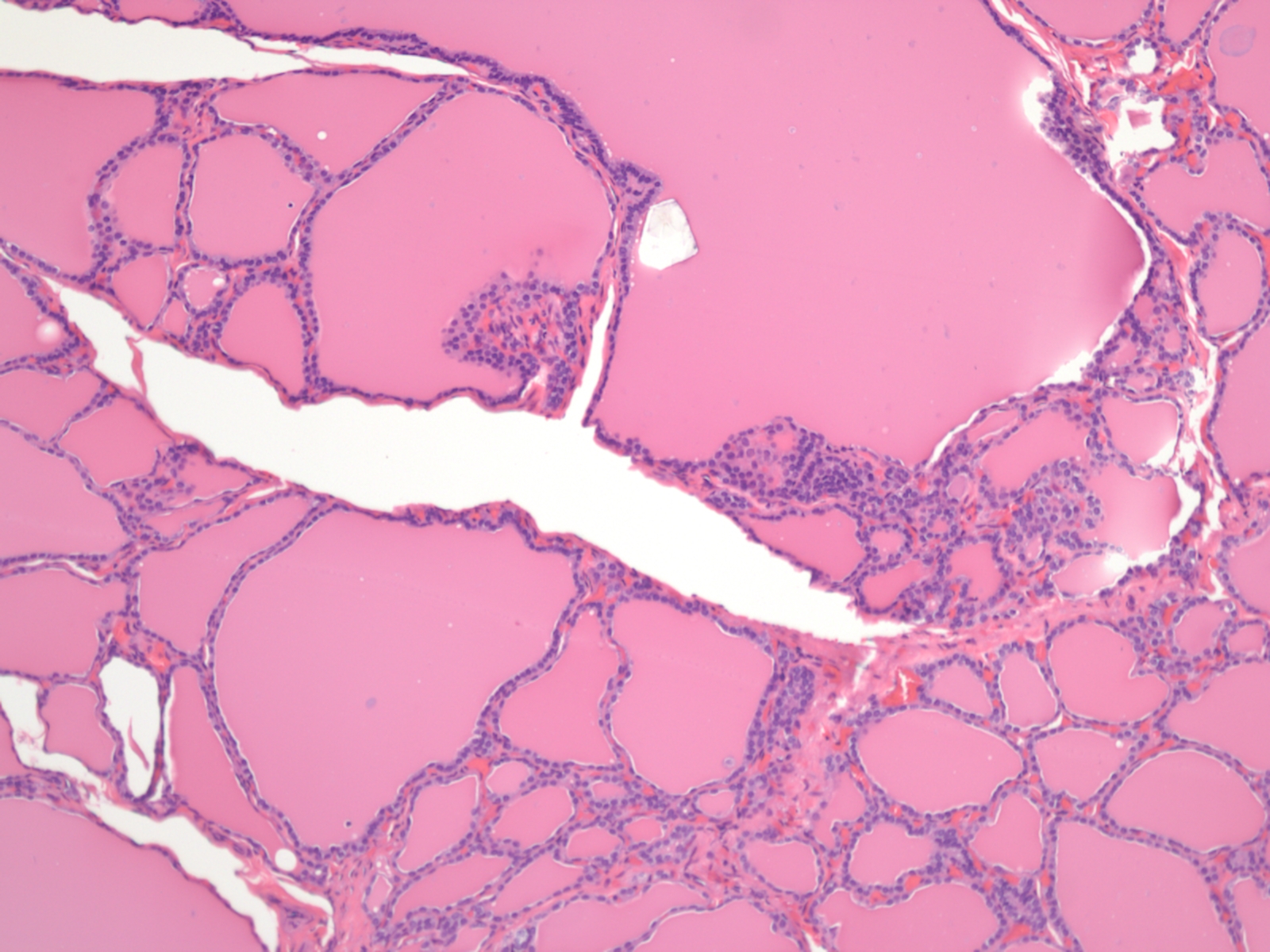
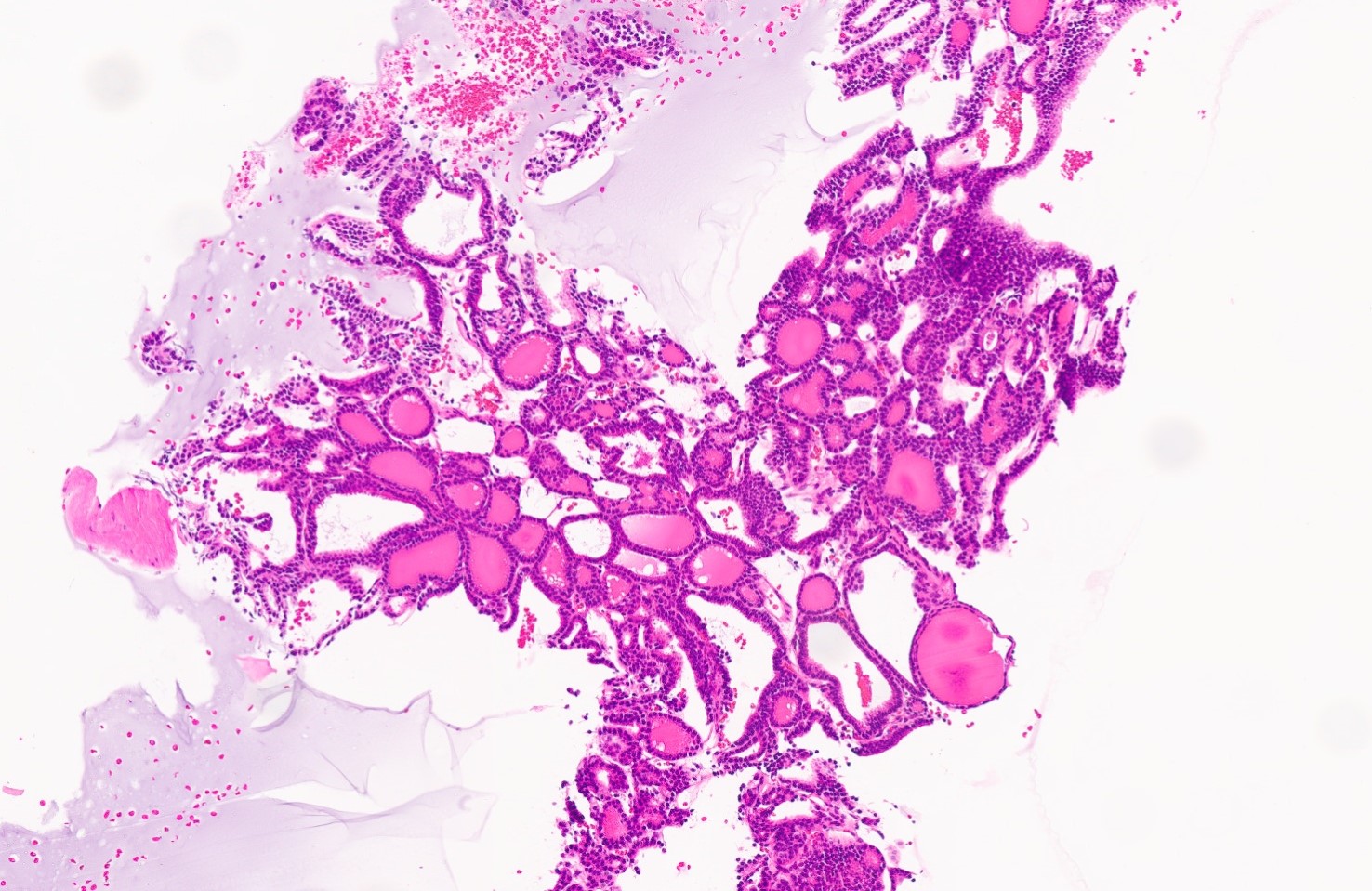
Microscopic (histologic) description
- Variable sized dilated follicles with flattened to hyperplastic epithelium
- Nodules may be present but without thick capsule
- Nodules with variable histological patterns: from colloid and microfollicular to hypercellular / microfollicular
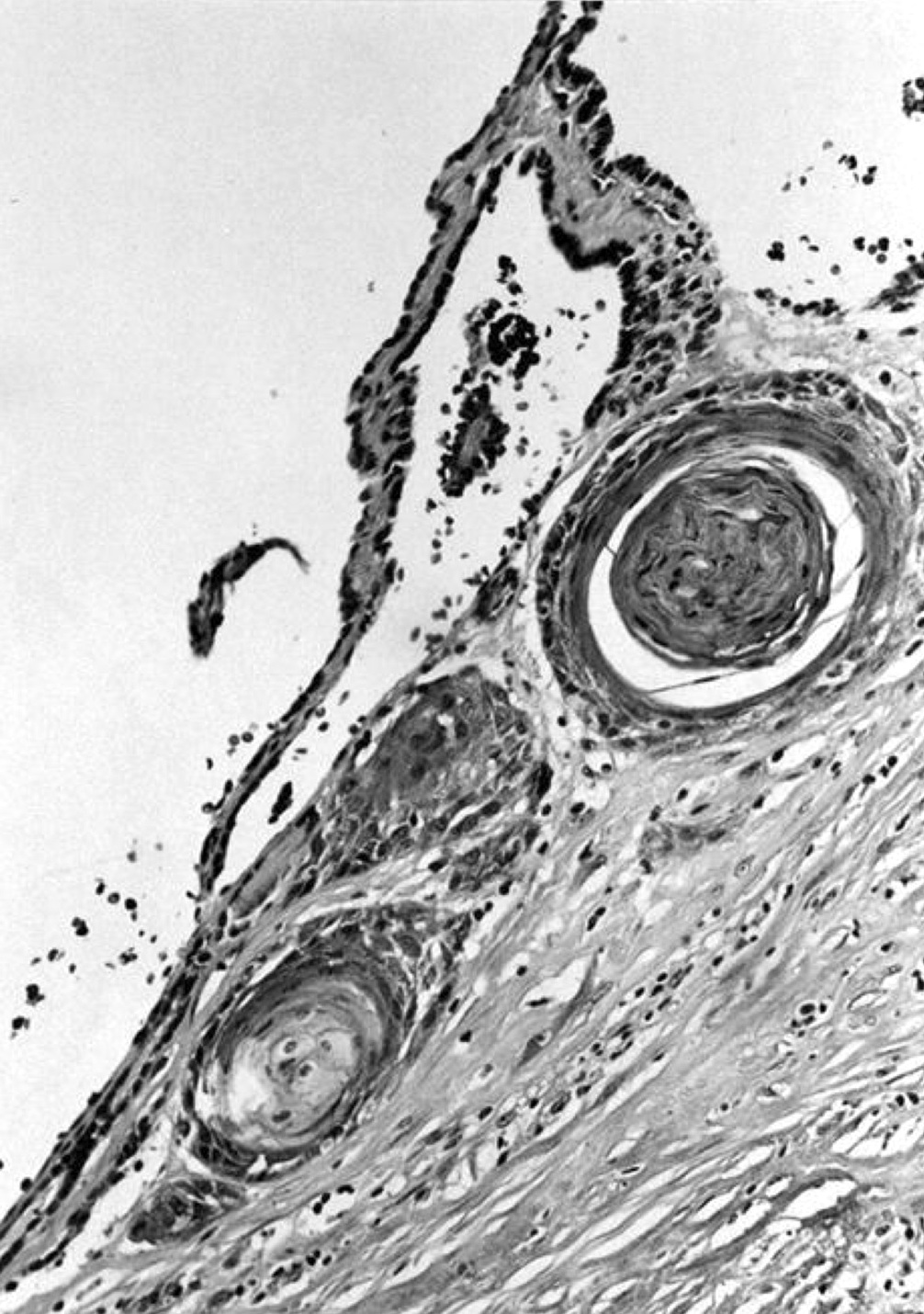
- Secondary changes may be seen, including foci of fresh or old hemorrhage, rupture of follicles with granulomatous response, fibrosis, calcification and even osseous metaplasia
- Some of the cystically dilated follicles may show papillary projections (Sanderson polsters) that may mimic papillary carcinoma; however, they lack the nuclear features of papillary carcinoma
- Cytologic atypia (in the form of highly atypical nuclei) if exposed to radioactive substances
- Non nodular thyroid is reduced and compressed
- Incidental papillary thyroid microcarcinoma may coexist
- References: Neuro Endocrinol Lett 2015;36:48, Eur Endocrinol 2020;16:131
Microscopic (histologic) images
Contributed by Swati Satturwar, M.D., Andrey Bychkov, M.D., Ph.D. and Rajeshwari K. Muthusamy, M.D.
AFIP images
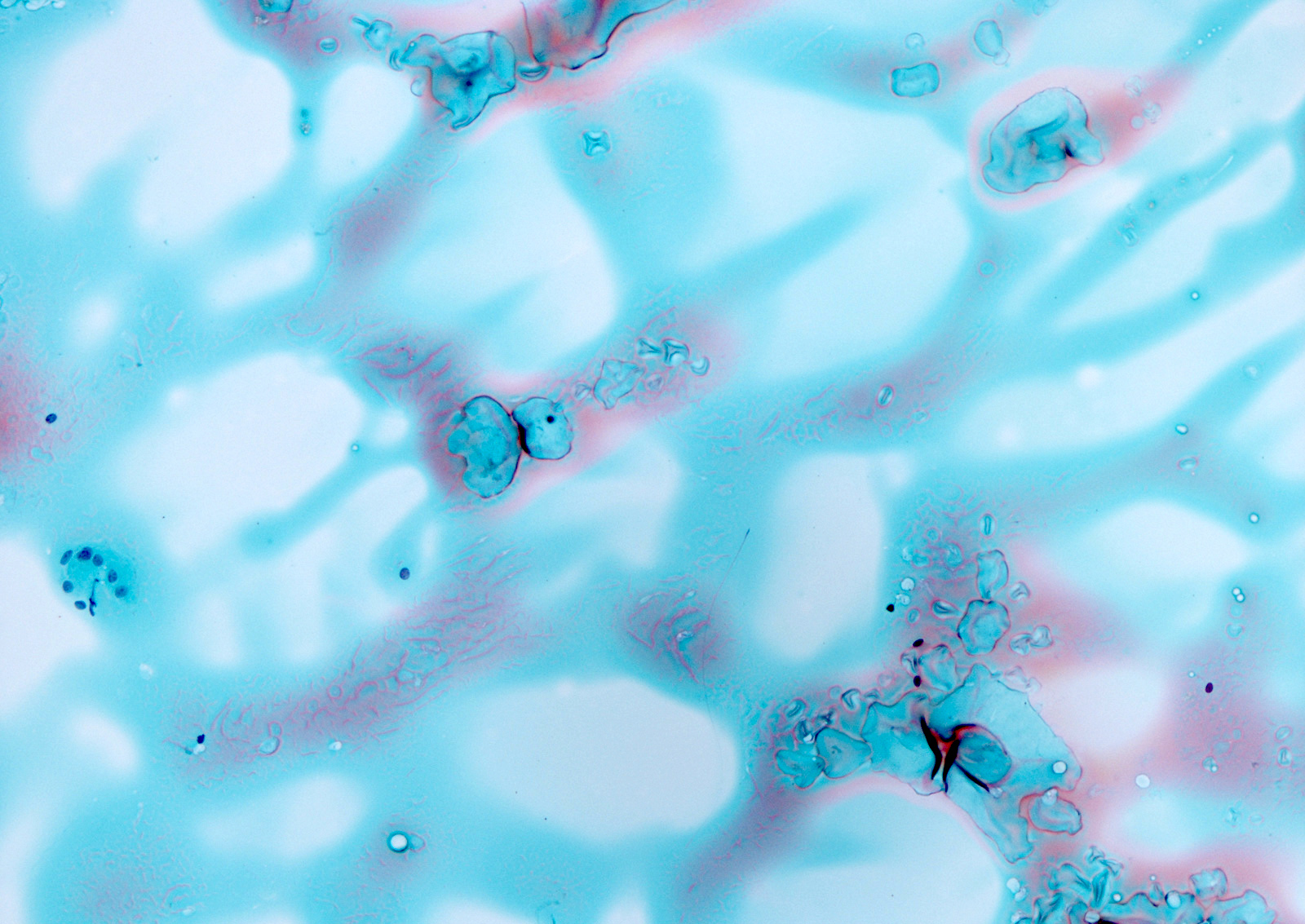
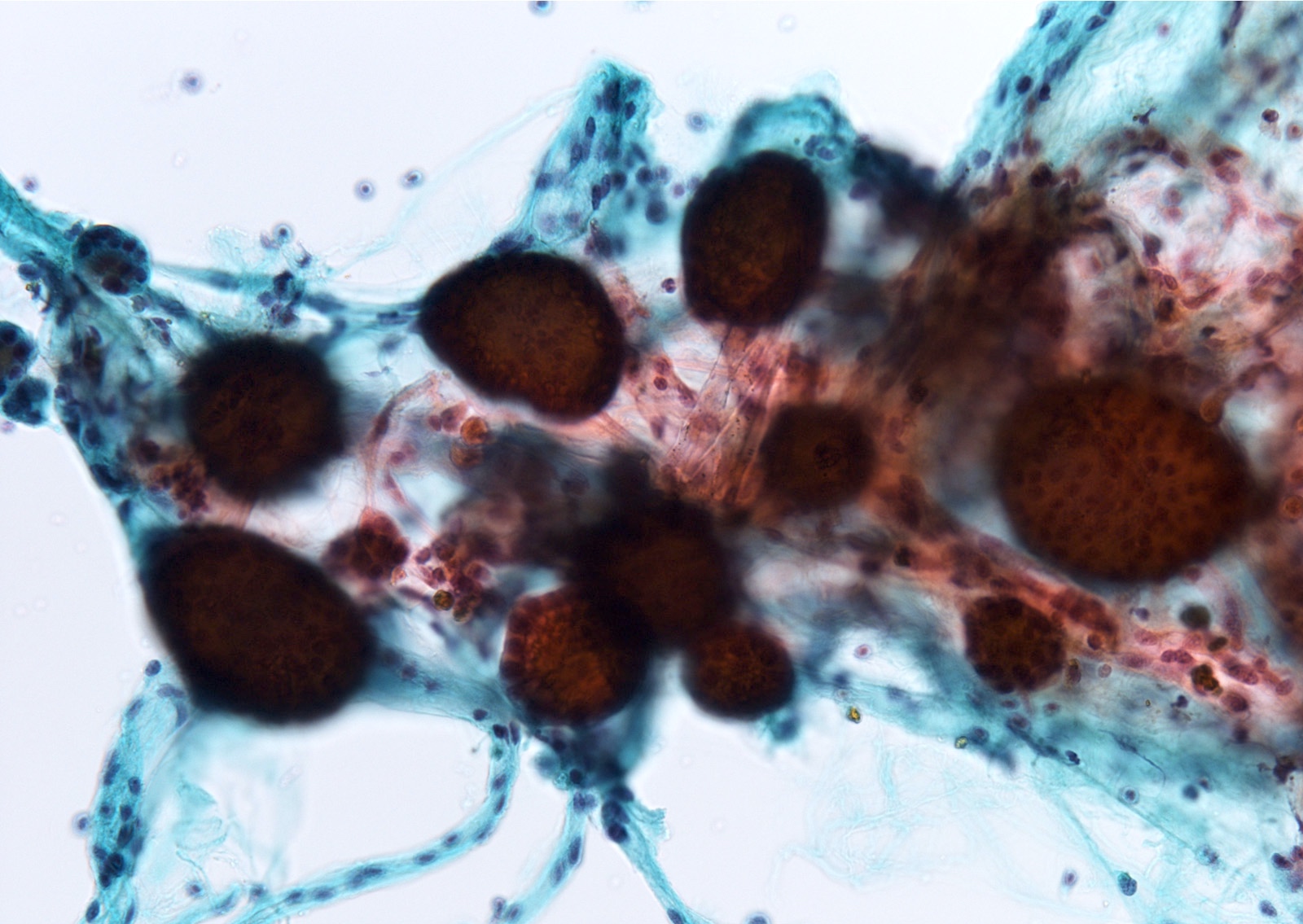
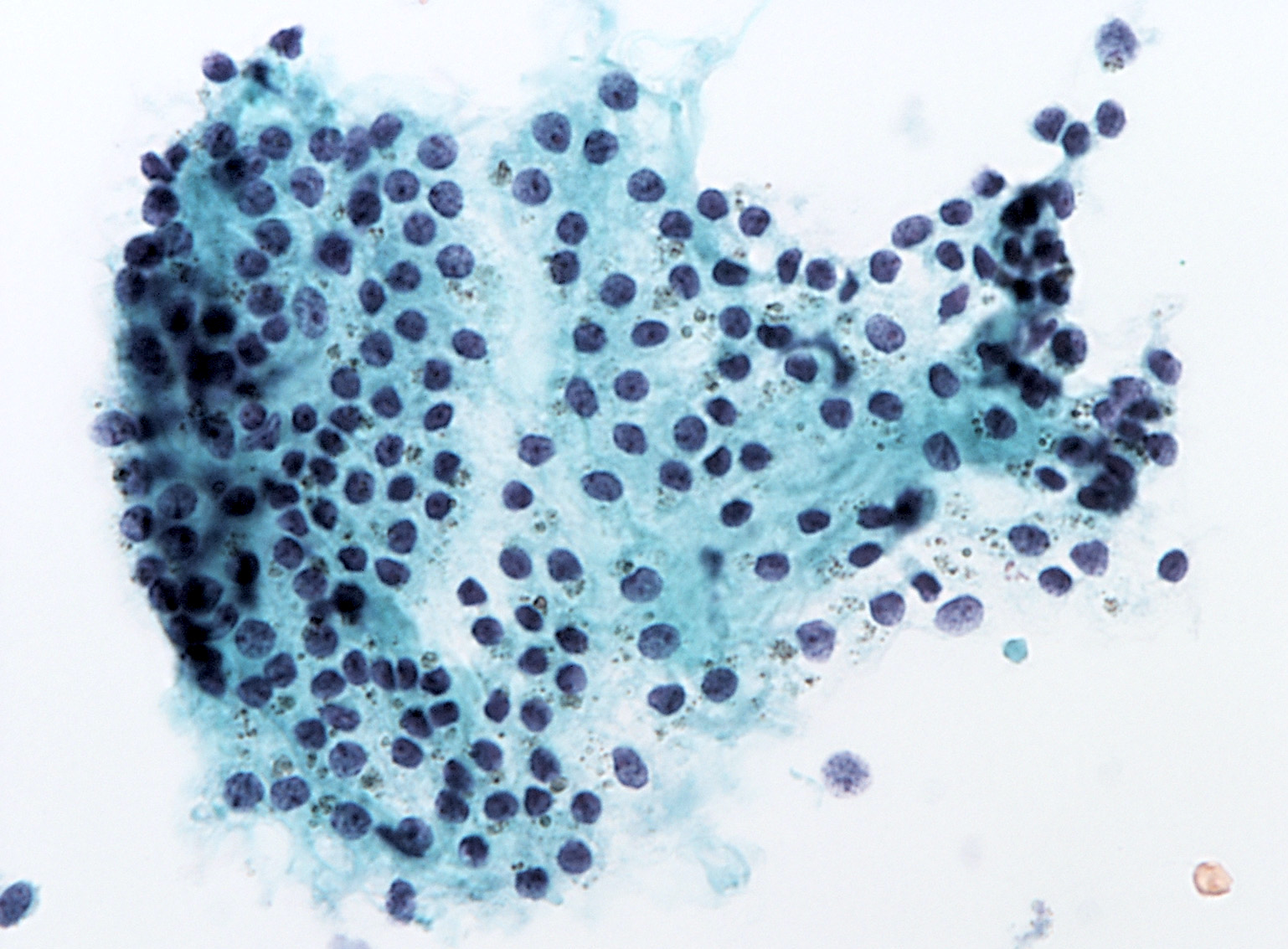
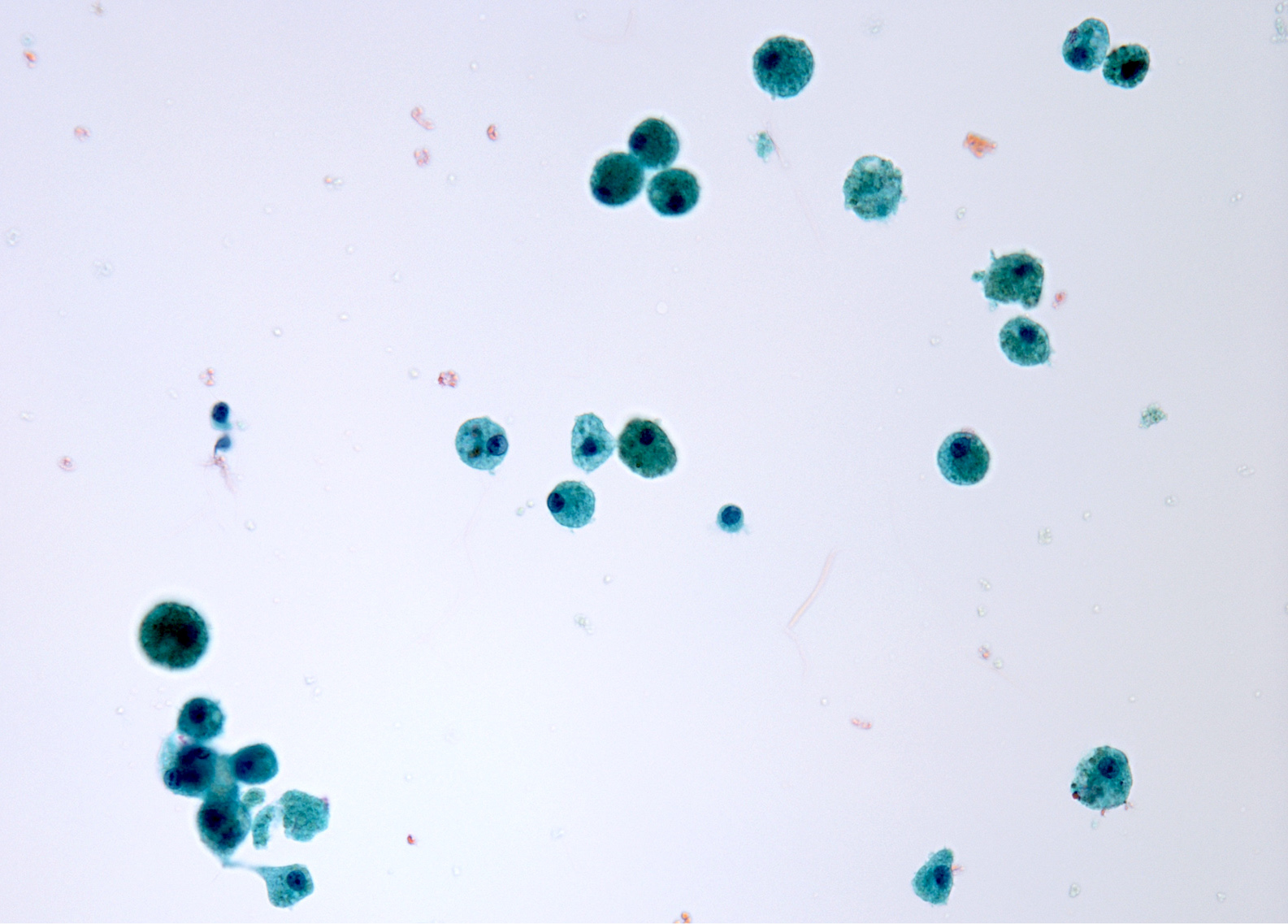
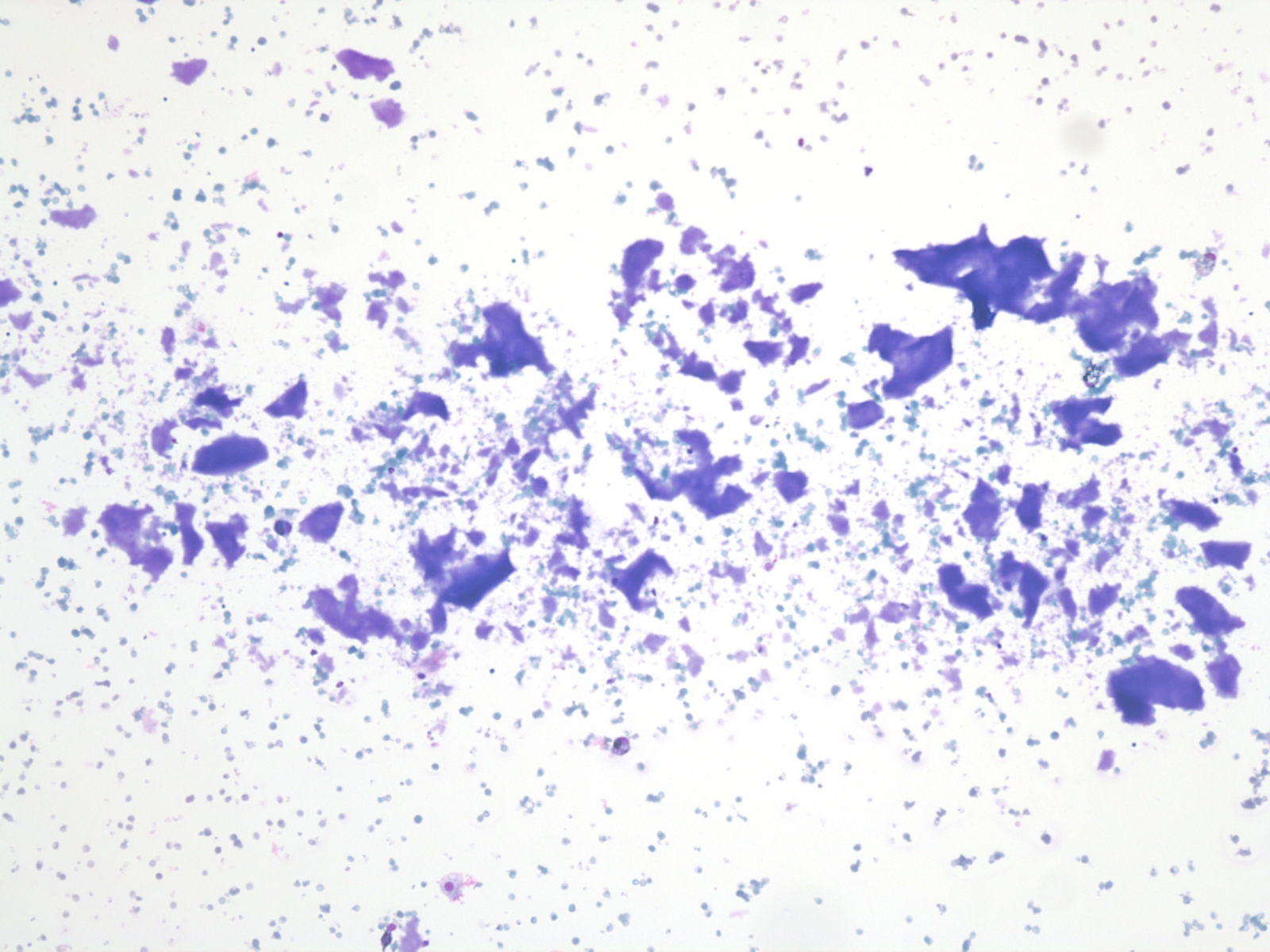
Cytology description
- Sparse to moderately cellular smears with abundant thin or thick colloid, flat sheets with evenly spaced follicular cells, pigment laden macrophages and oncocytic cells
- Rare microfollicles
- No cytologic features of papillary thyroid carcinoma (nuclear pseudoinclusion, nuclear elongation, nuclear overlap, finely dispersed chromatin)
- Mainly classified as category II (Benign) of The Bethesda System for Reporting Thyroid Cytopathology (Thyroid 2017;27:1341)
- Nodules with abundant cystic fluid can be classified as category I (Nondiagnostic / Cyst fluid only)
Cytology images
Positive stains
- Thyroid specific markers: thyroglobulin, TTF1, PAX8
Molecular / cytogenetics description
- Promoter hypermethylation of tumor suppressor gene RASSF1A (Thyroid 2017;27:1341)
- DICER1 mutation
- PTEN mutation
- Thyroid hormonogenesis related protein mutations (dyshormonogenetic goiter)
Videos
Thyroid multinodular goiter
Histopathology thyroid: nodular goiter
Histopathology thyroid: colloid goiter
Sample pathology report
- Thyroid, partial / total thyroidectomy:
- Multinodular hyperplasia
- Thyroid, partial / total thyroidectomy:
- Adenomatoid nodule in a background of diffuse hyperplasia
- Thyroid, partial / total thyroidectomy:
- Hemorrhagic nodule in background of multinodular hyperplasia
- Thyroid, partial / total thyroidectomy:
- Colloid nodule
Differential diagnosis
- Adenoma:
- Usually single, totally surrounded by capsule, dissimilar from remaining parenchyma, compresses adjacent tissue and composed of follicles smaller than normal gland
- Can mimic monoclonal dominant nodule in nodular goiter
- Clonal event, such as RAS mutation or PPARG fusion
- Dyshormonogenetic goiter:
- Increased cellularity is usually diffuse
- Follicular carcinoma:
- Has vascular or capsular invasion, although multinodular goiter may have vascular invasion at periphery of nodule
- Papillary carcinoma:
- Distinct nuclear features seen in papillary carcinoma; lacks the Sanderson polsters found in goiters
- Toxic goiter:
- Clinical hyperthyroidism
Additional references
Board review style question #1
Which of the histological features is seen in nodular goiter?
- Nodules with distinct thick capsule
- Papillary projections of the epithelium with nuclear features of papillary thyroid carcinoma
- Variably sized follicles with flattened hyperplastic epithelium, cysts, hemorrhage, granulomatous response, fibrosis, calcification or osseous metaplasia
- Vascular invasion
Board review style answer #1
C. Variably sized follicles with flattened hyperplastic epithelium, cysts, hemorrhage, granulomatous response, fibrosis, calcification or osseous metaplasia. Nodules may or may not be present in nodular goiter but generally lack a thick capsule. Prominent features are variably sized dilated follicles with flattened hyperplastic epithelium. Secondary changes include foci of fresh or old hemorrhage, rupture of follicles with granulomatous response, fibrosis, calcification and even osseous metaplasia. Some of the cystically dilated follicles may show papillary projections (Sanderson polsters). Cytologic atypia in the form of highly atypical nuclei occurs in patients exposed to radioactive substances.
Comment Here
Reference: Multinodular goiter
Comment Here
Reference: Multinodular goiter
Board review style question #2
Board review style answer #2
B. Category II (benign). These images represent a colloid nodule / benign thyroid nodule. They are typically managed by clinical and sonographic followup.
Comment Here
Reference: Multinodular goiter
Comment Here
Reference: Multinodular goiter