Table of Contents
Definition / general | Essential features | Clinical features | Diagnosis | Case reports | Cytology description | Cytology images | Management | Sample cytology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Suzuki A, Bychkov A. Suspicious for malignancy. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/thyroidsuspicious.html. Accessed April 19th, 2024.
Definition / general
- Bethesda category V suspicious for malignancy (SM) is used when some cytologic features are strongly suspected of malignancy but are not sufficient for a conclusive diagnosis (Thyroid 2017;27:1341)
- Higher suspicion of malignancy than atypia of undetermined significance / follicular lesion of undetermined significance (AUS / FLUS) but lower suspicion than malignant
- Molecular testing with mutation panels may be useful, particularly for potential noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) cases
- Purpose of separating suspicious for malignancy from malignant is to preserve the very high positive predictive value of the malignant category without compromising the overall sensitivity of fine needle cytology aspiration
Essential features
- Used when cytology is strongly suspected of malignancy but is not sufficient for a conclusive diagnosis
- Frequency < 5%, resection rate 70%, risk of malignancy 80% (NIFTP = malignant), 45 - 60% (NIFTP ≠ malignant)
- Most common histological diagnosis is papillary thyroid carcinoma (PTC) (Acta Cytol 2014;58:15)
Clinical features
- Frequency: 3% (Acta Cytol 2012;56:333, Cancer Cytopathol 2020;128:238)
- Resection rate: 70% (Cancer Cytopathol 2020;128:238)
- Risk of malignancy: 80% (NIFTP = malignant), 45 - 60% (NIFTP ≠ malignant) (Cancer Cytopathol 2020;128:238, Ali: The Bethesda System for Reporting Thyroid Cytopathology - Definitions, Criteria and Explanatory Notes, 2nd Edition, 2018)
- Suspicious for malignancy interpretation allows for more conservative management options (e.g. lobectomy)
Diagnosis
- Aspirates where malignancy is suspected but cannot be determined due to:
- Suboptimal sampling
- Poor cellular preservation
- Unusual variant of neoplasm
- Overlapping cytological features with other thyroid lesions
- Excluded from this category:
- Specimens suspicious for a follicular or Hürthle cell neoplasm (see FN / SFN and FNHCT / SFNHCT)
- Unequivocally malignant aspirates (see Malignant)
- Specimens with a minor degree of atypia, primarily cytologic or architectural (see AUS / FLUS)
- Frozen section has limited utility for suspicious for malignancy nodules (Thyroid 2002;12:619)
Case reports
- 55 year old man with colon cancer metastasis within a NIFTP which was cytologically suspected of PTC (Head Neck Pathol 2019 Oct 17 [Epub ahead of print])
- 58 year old woman with mammary analogue secretory carcinoma of the thyroid which was cytologically suspected of PTC (Int J Surg Pathol 2018;26:459)
- 63 year old man with follicular variant of papillary thyroid carcinoma presenting as a toxic nodule which was cytologically suspected of follicular variant of PTC (Clin Nucl Med 2010;35:770)
- 63 year old woman with hyalinizing trabecular tumor which was cytologically suspected of hyalinizing trabecular tumor (J Pathol Transl Med 2018;52:252)
- 71 year old man with mixed medullary and follicular cell carcinoma of the thyroid which was cytologically suspected of thyroid carcinoma (Med Sci Monit 2008;14:CS31)
Cytology description
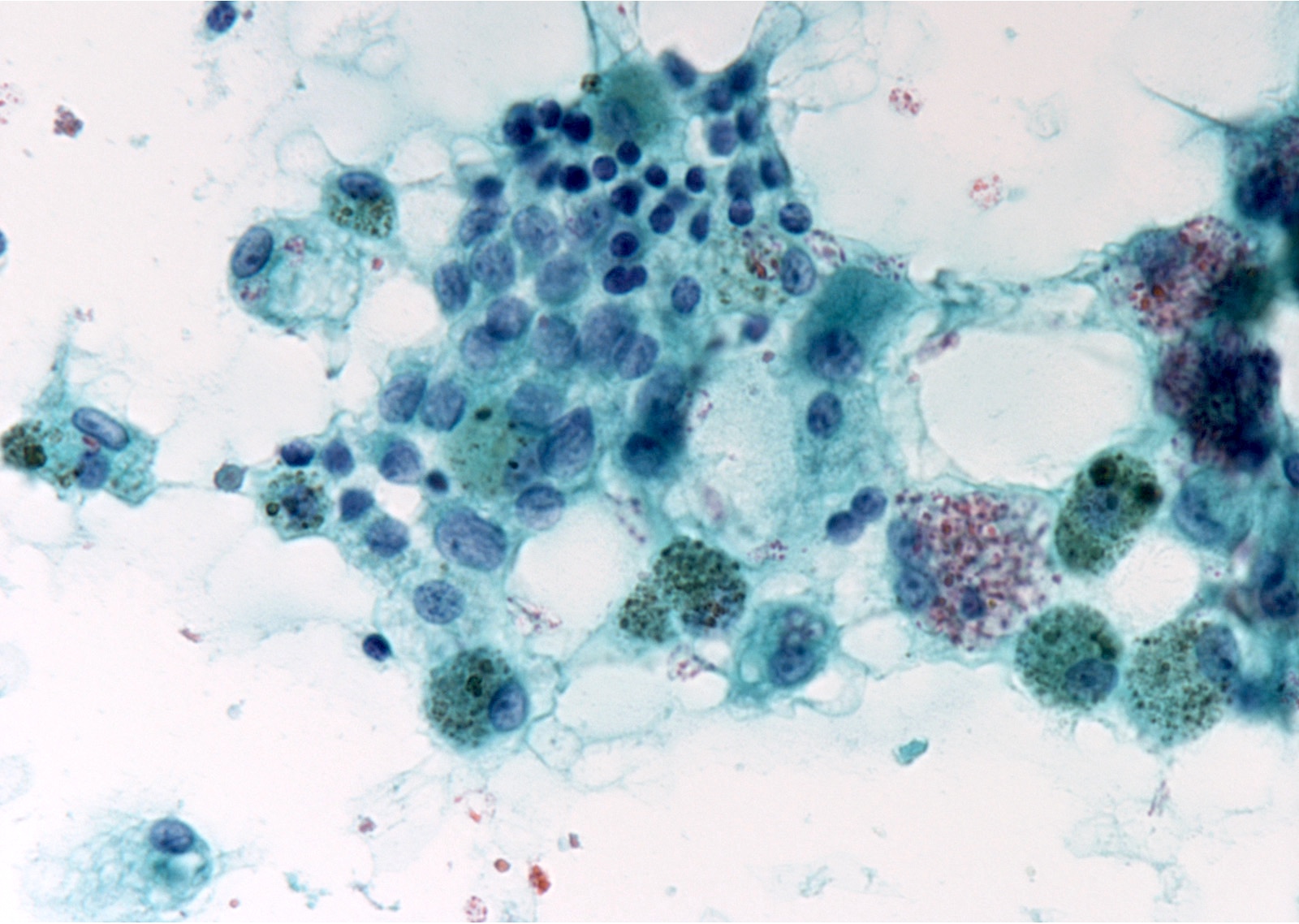
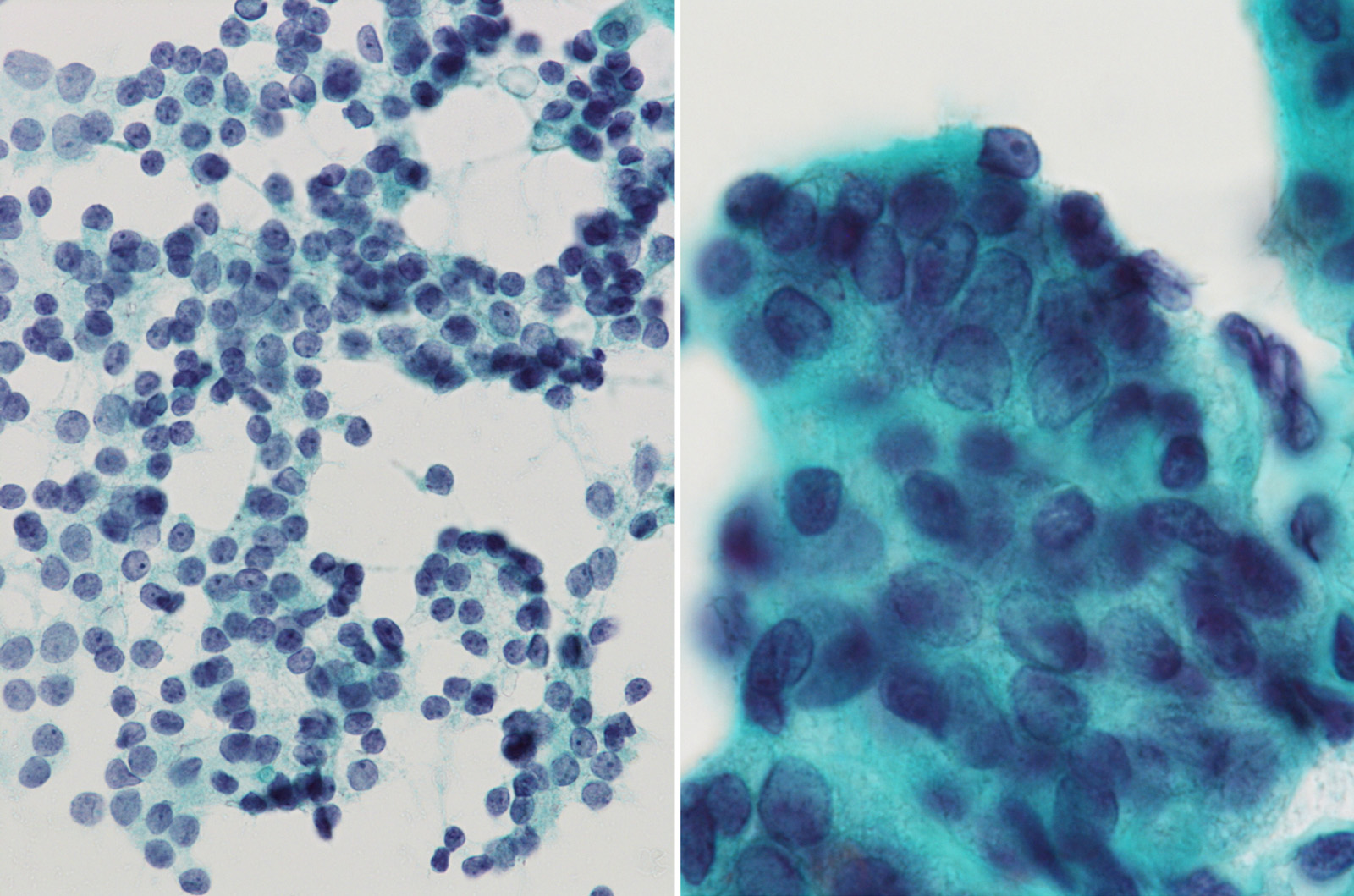
- Suspicious for papillary thyroid carcinoma
- Pattern A (patchy nuclear changes): moderate to high cellularity, nuclei showing enlargement, pallor, grooves, irregularity or molding but absence of nuclear pseudoinclusions, psammoma bodies and papillary architecture
- Pattern B (incomplete nuclear changes): nuclei showing enlargement with mild pallor and grooves, absence of nuclear irregularity, nuclear molding, nuclear pseudoinclusions, psammoma bodies and papillary architecture
- Pattern C (sparsely cellular specimen): poor cellularity, presence of many findings suggesting papillary thyroid carcinoma
- Pattern D (cystic degeneration): cystic degeneration based on foamy histiocytes, scattered clusters of follicular cells with the nuclei showing enlargement, pallor, grooves, absence of nuclear pseudoinclusions, psammoma bodies and papillary architecture, large, atypical, histiocytoid cells with enlarged nuclei and without abundant vacuolated cytoplasm (Ali: The Bethesda System for Reporting Thyroid Cytopathology - Definitions, Criteria and Explanatory Notes, 2nd Edition, 2018)
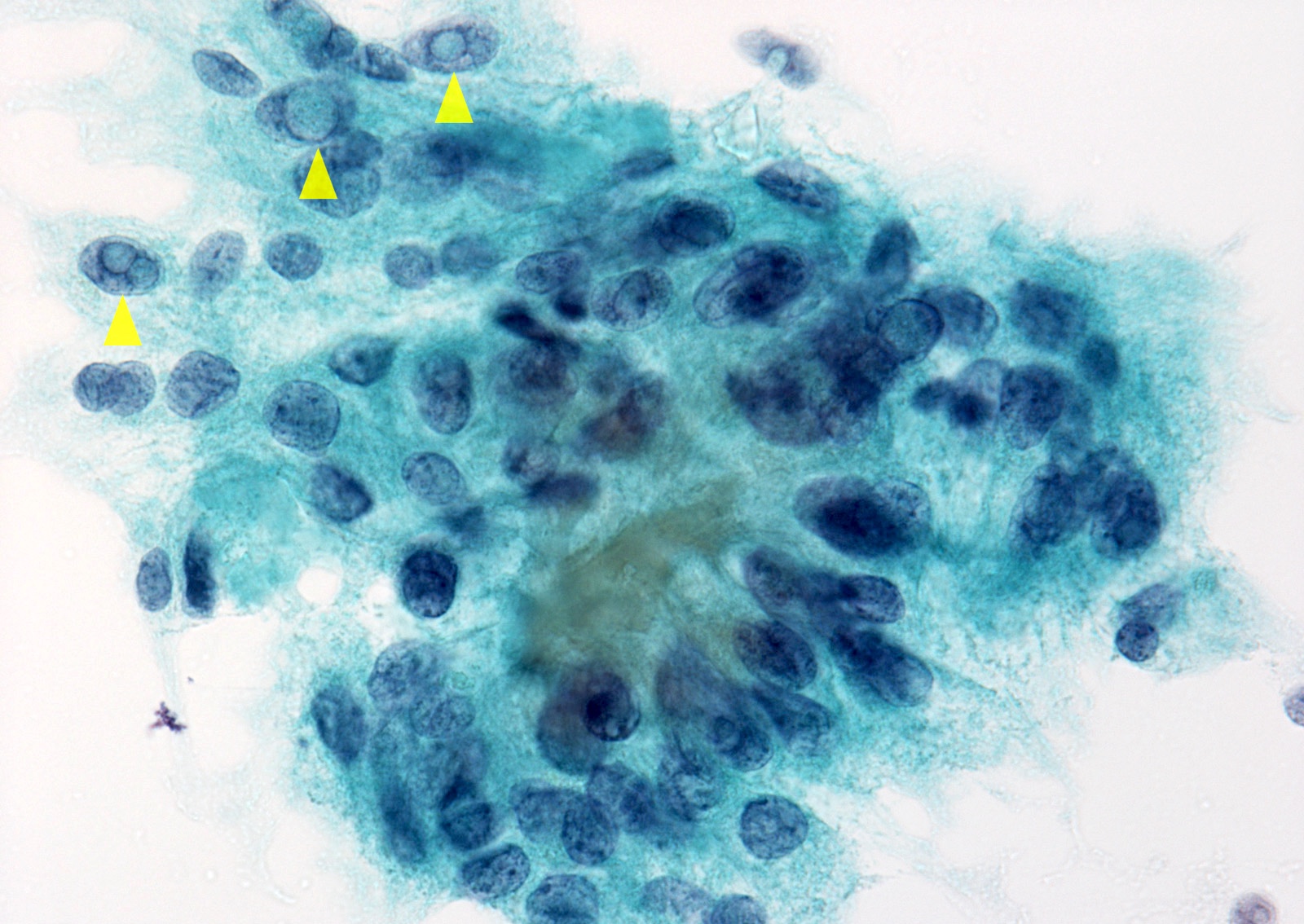
- Suspicious for medullary thyroid carcinoma
- Sparse or moderate cellularity
- Monomorphic population of isolated small or medium sized cells with a high nuclear cytoplasmic ratio
- Nuclei are eccentrically located, with smudged chromatin
- Small fragments of amorphous material
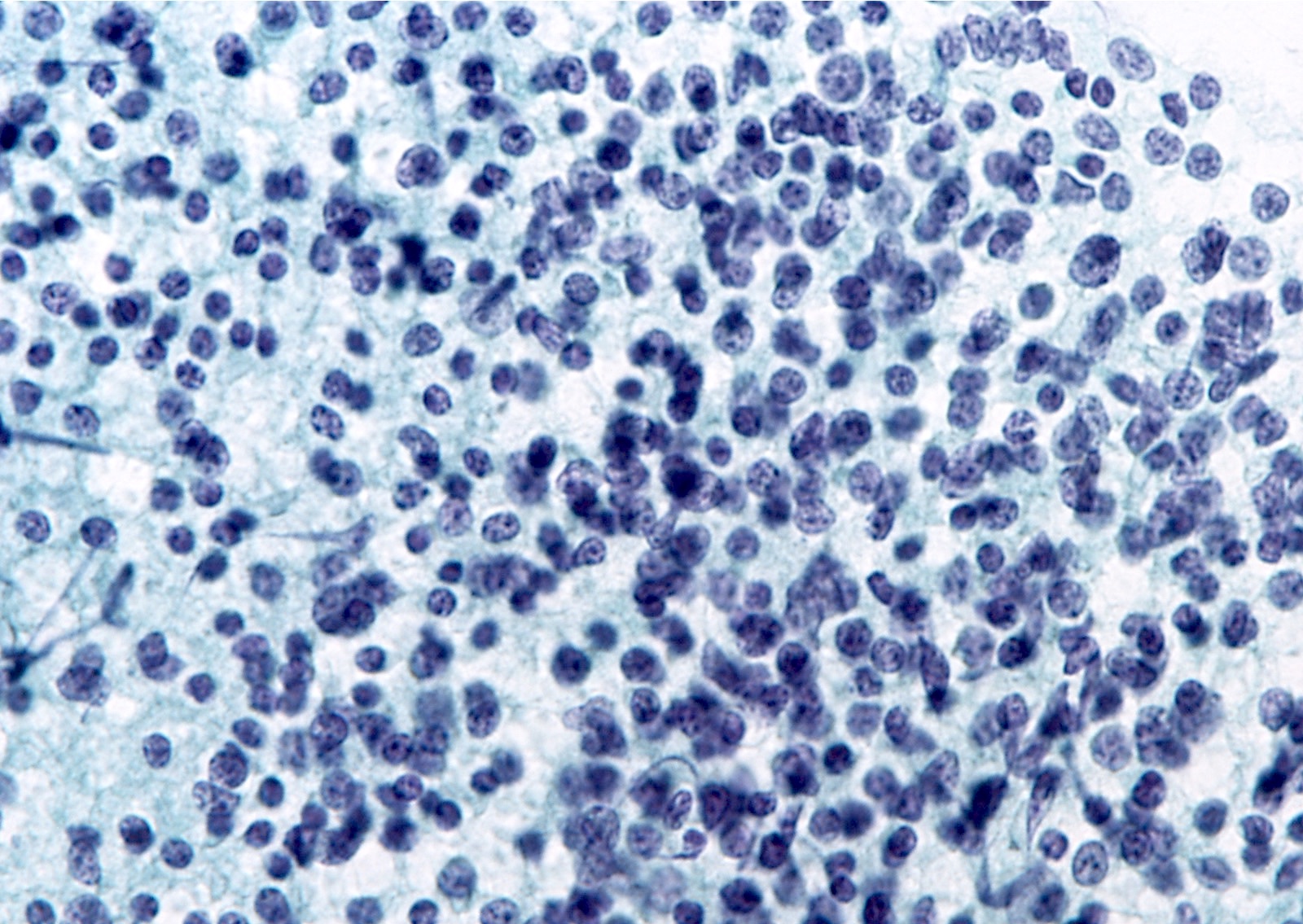
- Suspicious for lymphoma
- Numerous monomorphic small to intermediate sized lymphoid cells
- Sparsely cellular and contains atypical lymphoid cells
- Suspicious for malignancy, not otherwise specified
- Other primary thyroid malignancies like anaplastic carcinoma and poorly differentiated carcinoma
- Suboptimal cellularity or preservation can lead to uncertainty and result in a suspicious for malignancy interpretation
Cytology images
Management
- Usually surgical management similar to that of malignant nodules (Thyroid 2016;26:1)
- In suspicious for papillary thyroid carcinoma cases with low risk features (≤ 1 cm, without extrathyroidal extension and clinical metastasis), active surveillance is an option (Thyroid 2018;28:23)
- Molecular testing with high positive predictive value (BRAF mutation or mutation panel) active surveillance is an option (Thyroid 2016;26:1)
- For suspicious for medullary thyroid carcinoma
- Measuring serum calcitonin level or calcitonin immunostaining are recommended (Endocr J 2017;64:1099)
- For suspicious for lymphoma
- Repeat fine needle aspiration to obtain cells for flow cytometry (Endocr J 2017;64:859, Endocr J 2019;66:1083)
Sample cytology report
- Dx / category: suspicious for malignancy
- Suspicious for papillary thyroid carcinoma
- A few follicular cells showing nuclear enlargement, pale and powdery chromatin and nuclear grooves are present
- Dx / category: suspicious for malignancy
- Suspicious for medullary thyroid carcinoma
- Correlation with serum calcitonin level or immunostaining might be helpful for definitive diagnosis if clinically indicated
- Dx / category: suspicious for malignancy
- Suspicious for lymphoma
- Re-aspiration for flow cytometry might be helpful to better characterize the lymphocyte population if clinically indicated
Differential diagnosis
- Noninvasive follicular thyroid neoplasm with papillary-like nuclear features:
- Microfollicular architecture with minimal nuclear features of papillary thyroid carcinoma, absence of nuclear pseudoinclusions, papillae or psammoma bodies
- Impossible to distinguish from invasive follicular variant of papillary thyroid carcinoma by fine needle aspiration alone
- Hyalinizing trabecular tumor:
- Trabecular growth pattern of the cells with nuclear grooves and abundant nuclear pseudoinclusions, intratrabecular hyaline material
- MIB1 membranous positivity is useful to distinguish from papillary thyroid carcinoma (Am J Surg Pathol 2000;24:575)
- Chronic thyroiditis (versus papillary thyroid carcinoma):
- Nuclear changes of follicular cells with focal enlargement, grooves, prominent nucleoli and chromatin clearing in the lymphocytic background
- An abundance of lymphocytes and plasma cells does not exclude the possibility of a coexisting papillary thyroid carcinoma (Acta Cytol 2012;56:352)
- Chronic thyroiditis (versus MALT lymphoma):
- Numerous lymphocytes, few follicular cells
- Difficult to distinguish from MALT lymphoma without immunophenotyping by flow cytometry
- Benign cyst:
- Elongated cells with pale chromatin, nuclear grooves and relatively large nucleoli
- Spindle shaped morphology of the cell and nucleus, reminiscent of reparative epithelium in cervical Pap smears
Board review style question #1
Board review style answer #1
C. Follicular variant of papillary thyroid carcinoma follicular cells appear as microfollicular pattern. A few follicular cells showing nuclear enlargement, pale and powdery chromatin and nuclear grooves are present.
Comment Here
Reference: Suspicious for malignancy
Comment Here
Reference: Suspicious for malignancy
Board review style question #2
- What is the most common histological equivalent of suspicious for malignancy aspirate of thyroid?
- Anaplastic thyroid carcinoma
- Follicular carcinoma
- Medullary thyroid carcinoma
- Papillary thyroid carcinoma
- Poorly differentiated thyroid carcinoma
Board review style answer #2
D. Papillary thyroid carcinoma. More than 85% of suspicious for malignancy cases are papillary thyroid carcinoma.
Comment Here
Reference: Suspicious for malignancy
Comment Here
Reference: Suspicious for malignancy