Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Skala SL. Endometritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusendometritis.html. Accessed April 25th, 2024.
Definition / general
- Inflammatory process involving the endometrium
Essential features
- Endometrial stromal plasma cells required for the diagnosis of chronic endometritis
- Chronic endometritis is implicated in infertility and recurrent pregnancy loss
- Acute endometritis typically represents ascending infection from lower genital tract
- Xanthogranulomatous endometritis usually associated with cervical stenosis
ICD coding
Epidemiology
- Typically premenopausal women
Sites
- Endometrium
Pathophysiology
- Unknown
Etiology
- Chronic endometritis
- Unclear etiology
- Causative organisms include Streptococcus species, Escherichia coli, Enterococcus, Staphylococcus species and Mycoplasma / Ureaplasma species (Fertil Steril 2008;89:677)
- Acute endometritis
- Ascending infection from lower genital tract
- Causative organisms include Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, Mycoplasma species (Sex Transm Infect 2020;96:436)
- Group A streptococcal infection rarely causes postpartum endometritis (Postgrad Med 2020;132:526)
- May be secondary to retained products of conception
- Actinomyces-like organisms are a rare cause of acute and chronic endometritis with prolonged intrauterine device use (Int J Gynecol Pathol 2019;38:138)
- Ascending infection from lower genital tract
- Xanthogranulomatous endometritis
- Pyometra, cervical stenosis (Clin Case Rep 2021;9:e04299, J Midlife Health 2019;10:206)
- Granulomatous endometritis
- Tuberculosis (Am J Obstet Gynecol 2020;223:737.e1)
- Sarcoidosis (Int J Surg Pathol 2017;25:246)
- Coccidioidomycosis (Arch Pathol Lab Med 1986;110:232)
- Postendometrial ablation (Br J Obstet Gynaecol 1992;99:928)
- Cytomegalovirus (Am J Surg Pathol 1992;16:716)
Clinical features
- Chronic endometritis
- Often asymptomatic (Int J Gynecol Pathol 2010;29:44, Am J Reprod Immunol 2011;66:410)
- Abnormal uterine bleeding, pelvic discomfort (Int J Gynecol Pathol 2010;29:44, Am J Reprod Immunol 2011;66:410)
- Associated with moderate to severe intrauterine adhesions (Fertil Steril 2019;111:1002)
- May be associated with unexplained infertility, unexplained recurrent miscarriages and repeated implantation failure after in vitro fertilization embryo transfer (Mod Pathol 2010;23:1136, Fertil Steril 2011;95:1156, Fertil Steril 2010;93:437)
- Somewhat controversial
- Acute endometritis
- Fever, pelvic pain, vaginal discharge
Diagnosis
- Microscopic examination is the gold standard
- Hysteroscopic scoring systems have been proposed (J Minim Invasive Gynecol 2020;27:1127)
- Features: endometrial hyperemia (focal or diffuse), hemorrhagic spots, dilated endometrial vessels, micropolyps, endometrial polyp
Prognostic factors
- Women with cured chronic endometritis may have higher ongoing pregnancy rate / live birth rate, clinical pregnancy rate and implantation rate (Fertil Steril 2018;110:103)
- Untreated acute endometritis has a fatality rate ~17% (StatPearls: Endometritis [Accessed 3 August 2021])
- Acute endometritis is not associated with infertility (Am J Obstet Gynecol 2003;188:141)
Case reports
- 61 year old woman with pyometra and enlarged uterus (J Midlife Health 2019;10:206)
- 70 year old woman with intrauterine device in place for 42 years (Acta Medica (Hradec Kralove) 2019;62:35)
- 74 year old woman with endometrial fluid collection and clinical concern for endometrial cancer (Radiol Case Rep 2018;14:121)
Treatment
- Chronic endometritis
- Antibiotic therapy (often empiric treatment with doxycycline [first line] or metronidazole / ciprofloxacin [second line]) (Am J Reprod Immunol 2017;78:e12719)
- Acute endometritis
- Oral antibiotics for mild disease (doxycycline / metronidazole, levofloxacin / metronidazole or amoxicillin / clavulanate) (StatPearls: Endometritis [Accessed 3 August 2021])
- IV antiobiotics (such as gentamicin or clindamycin) if more severe (StatPearls: Endometritis [Accessed 3 August 2021])
Microscopic (histologic) description
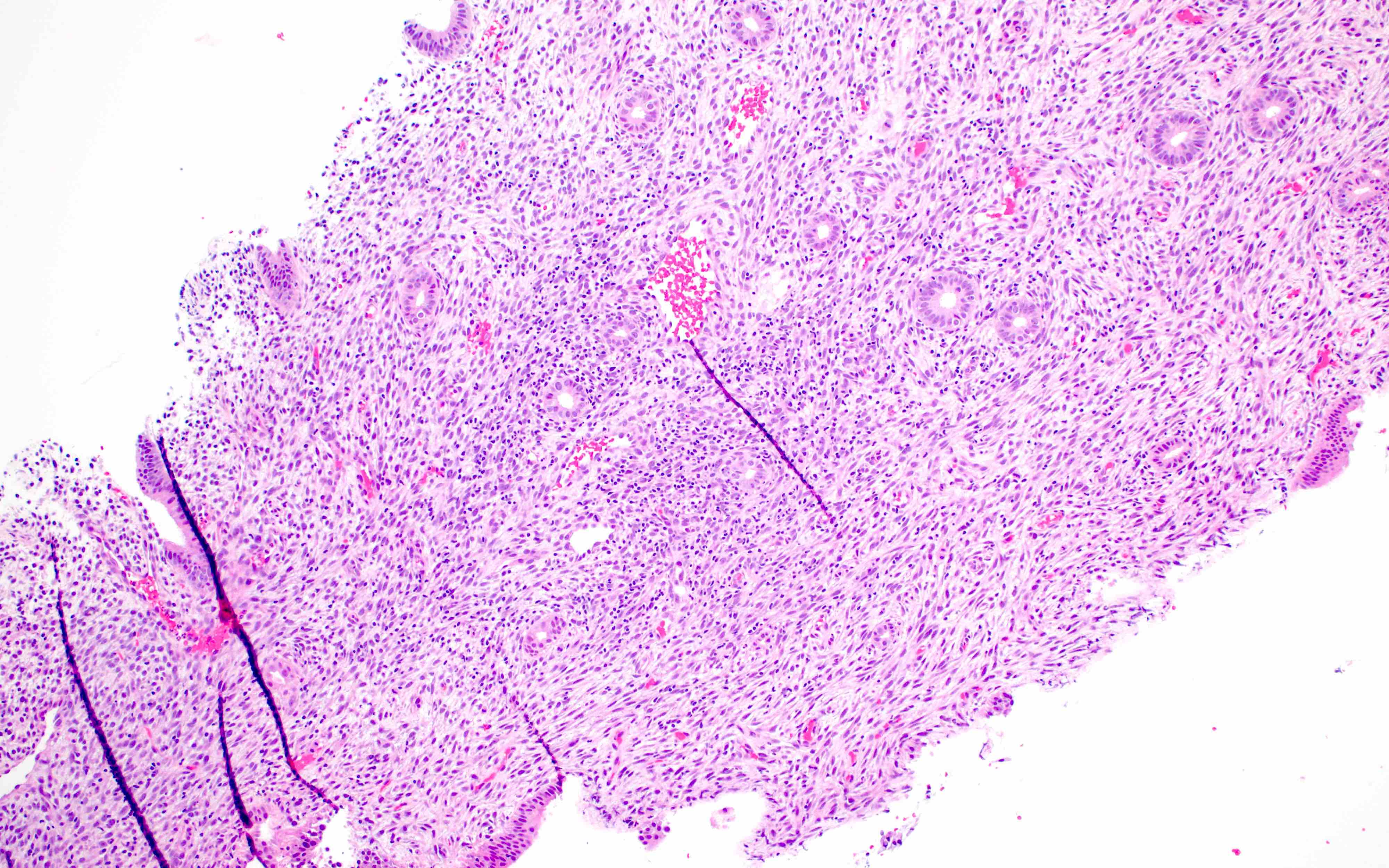
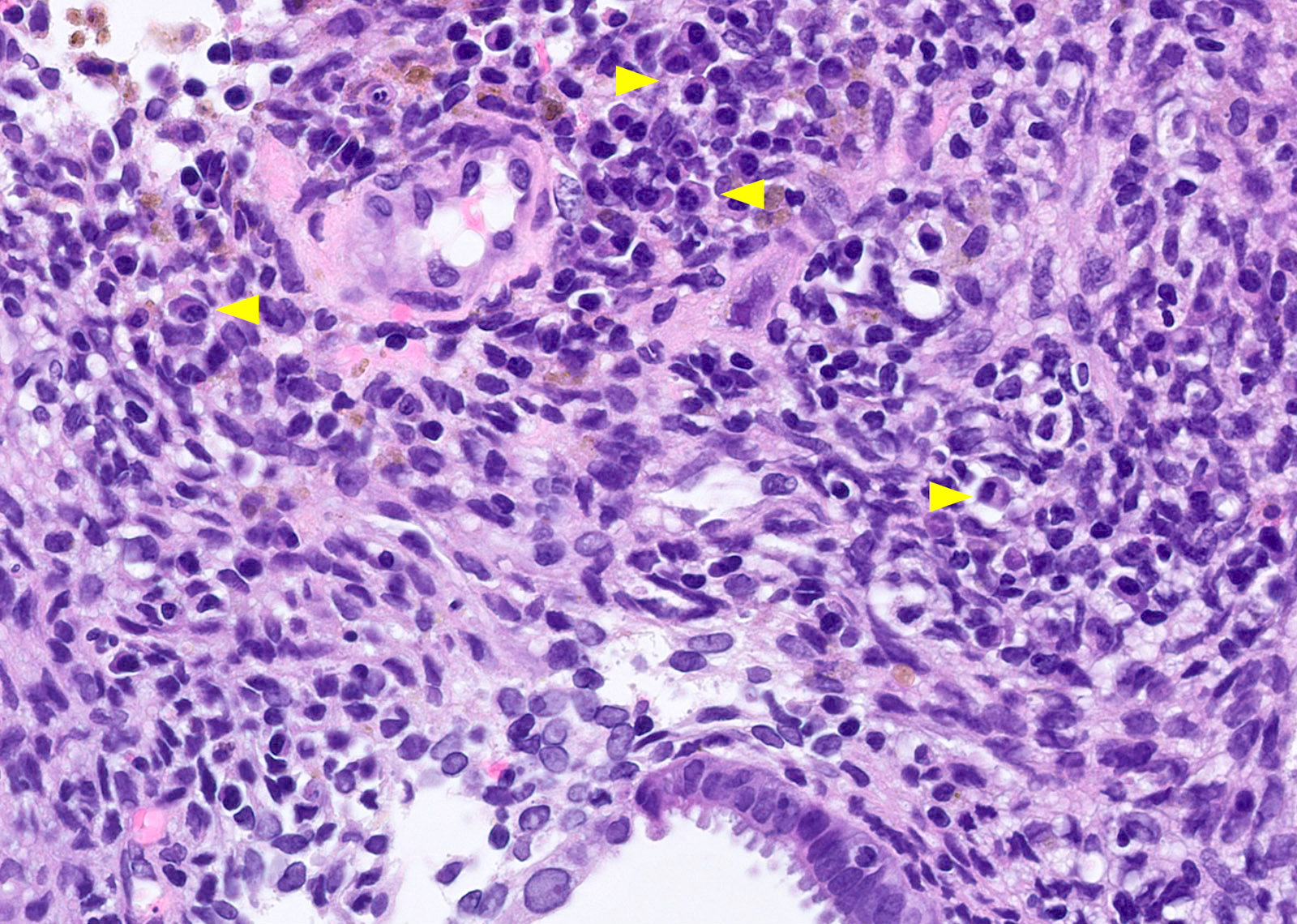
- Chronic endometritis
- Plasma cells (required) with or without lymphoid follicles
- Presence of eosinophils associated with plasma cells (Hum Pathol 2010;41:33)
- Currently no specific guidelines about required number of plasma cells or whether detection of rare plasma cells by IHC alone is sufficient (Int J Gynecol Pathol 2020 Dec 14 [Epub ahead of print])
- Plasma cells can be seen in disordered proliferative or breakdown endometrium in the absence of infection (Hum Pathol 2007;38:581)
- Spindled stromal cells
- Endometrial dating is unreliable due to frequent out of phase morphology (Am J Reprod Immunol 2011;66:410)
- Higher prevalence in proliferative phase (Reprod Biomed Online 2018;36:78)
- Note: structural abnormalities (endometrial polyp, submucosal leiomyoma) can be associated with plasma cells; such cases should not be diagnosed as chronic endometritis
- Plasma cells (required) with or without lymphoid follicles
- Acute endometritis
- Neutrophils infiltrating and destroying endometrial epithelium
- Neutrophils filling gland lumina
- With or without microabscess formation
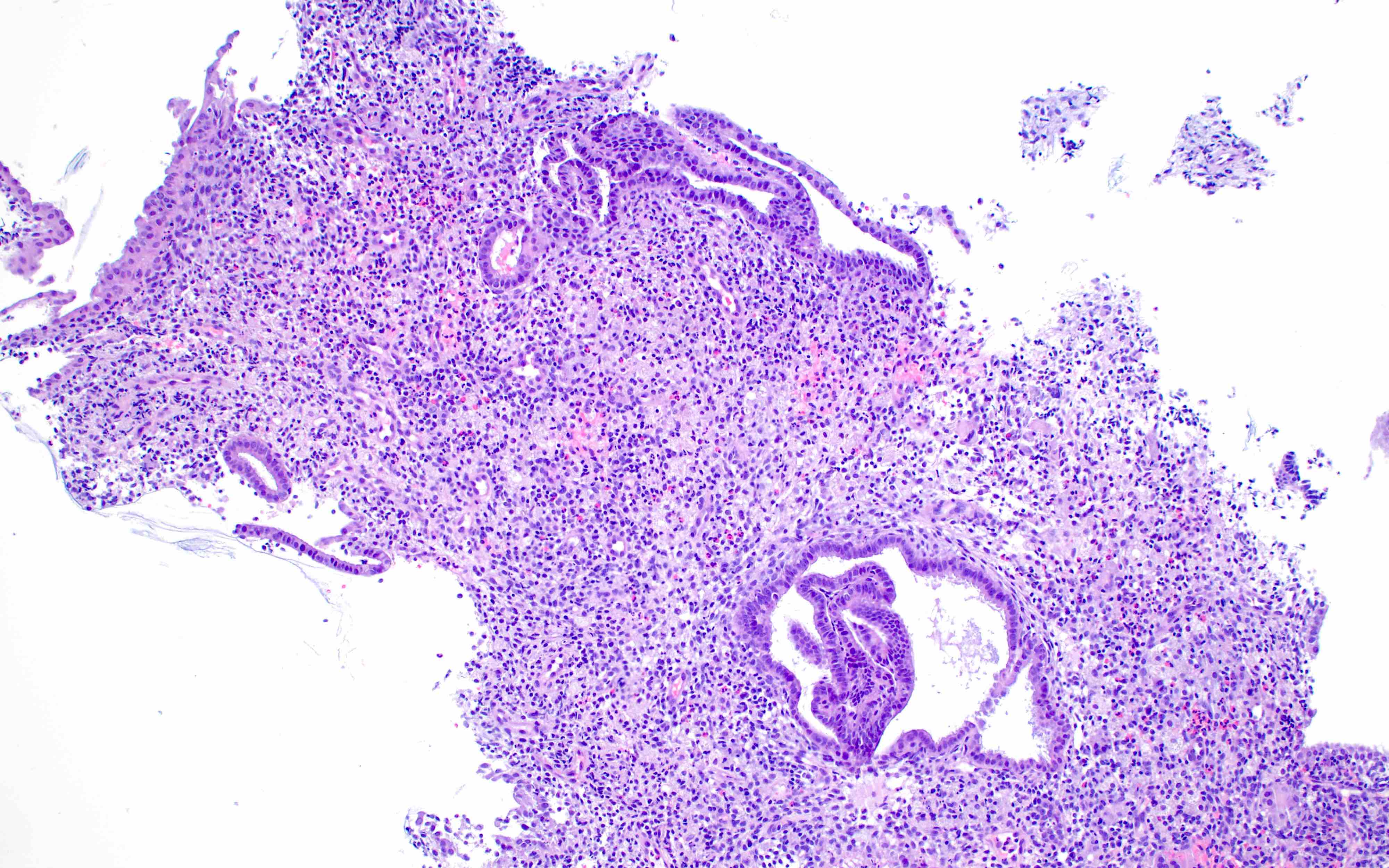
- Granulomatous endometritis
- Clusters of epithelioid histiocytes rimmed by lymphocytes
- Cytopathic effects if viral etiology (herpes simplex virus, cytomegalovirus)
- Tuberculosis: necrotizing granulomas with multinucleated giant cells, usually in superficial functional endometrium (Am J Obstet Gynecol 2020;223:737.e1)
- Sarcoidosis: nonnecrotizing granulomatous inflammation, more commonly in myometrium
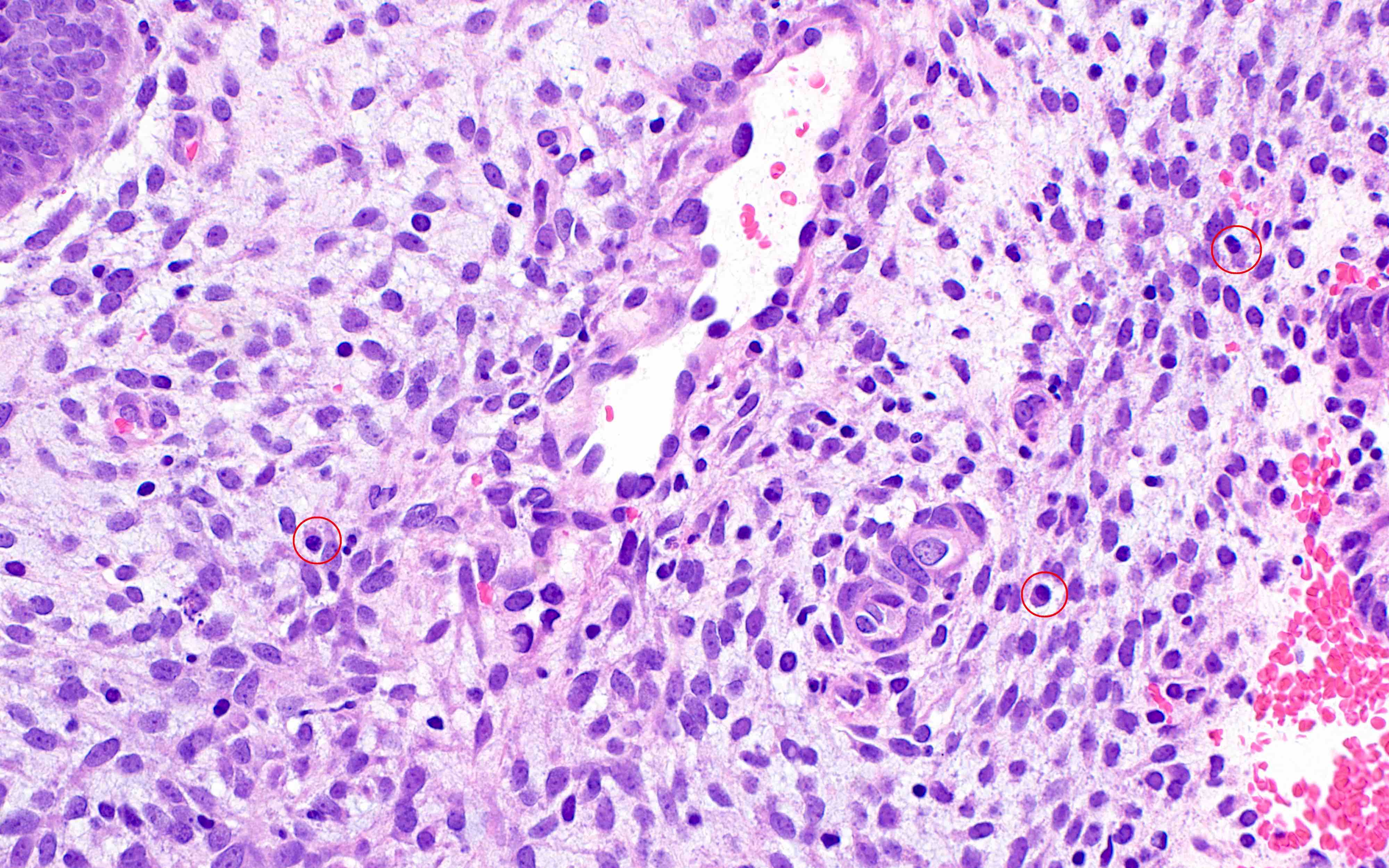
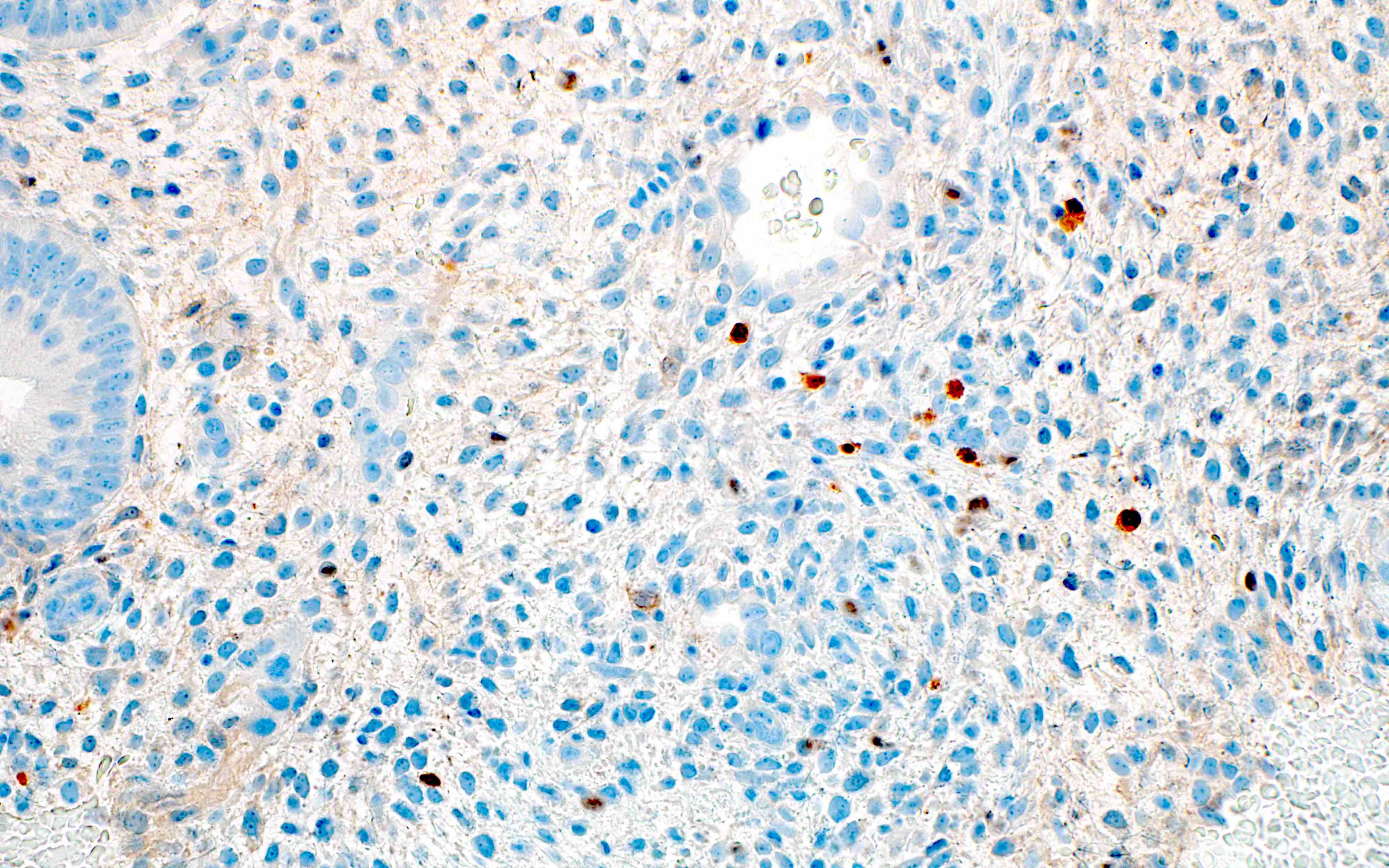
- Xanthogranulomatous endometritis
- Abundant foamy histiocytes, siderophages, neutrophils, plasma cells, lymphocytes
- With or without fibrosis, calcification
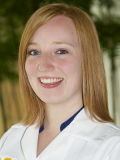
Microscopic (histologic) images
Contributed by Stephanie L. Skala, M.D. and Yuri Tachibana, M.D.
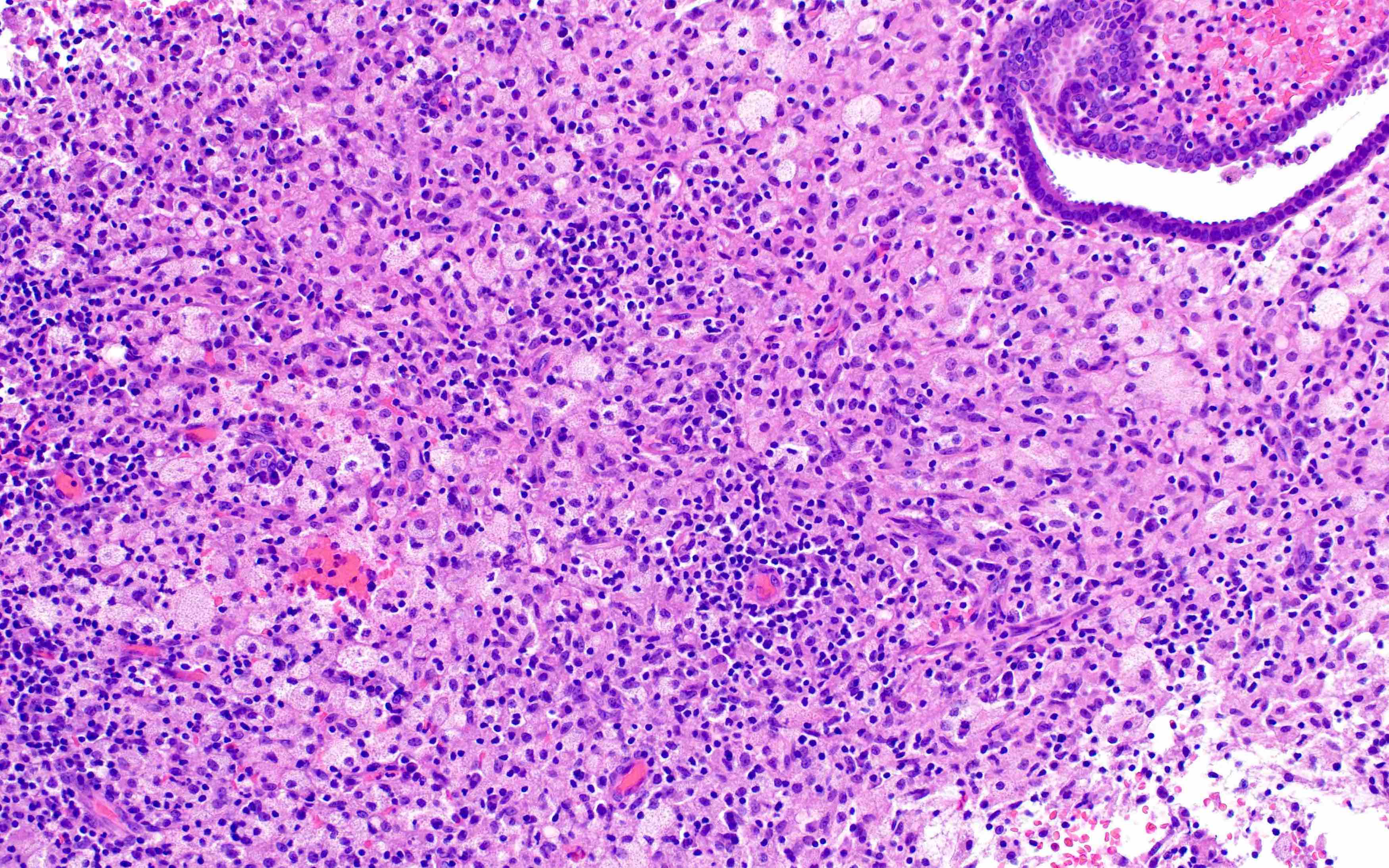
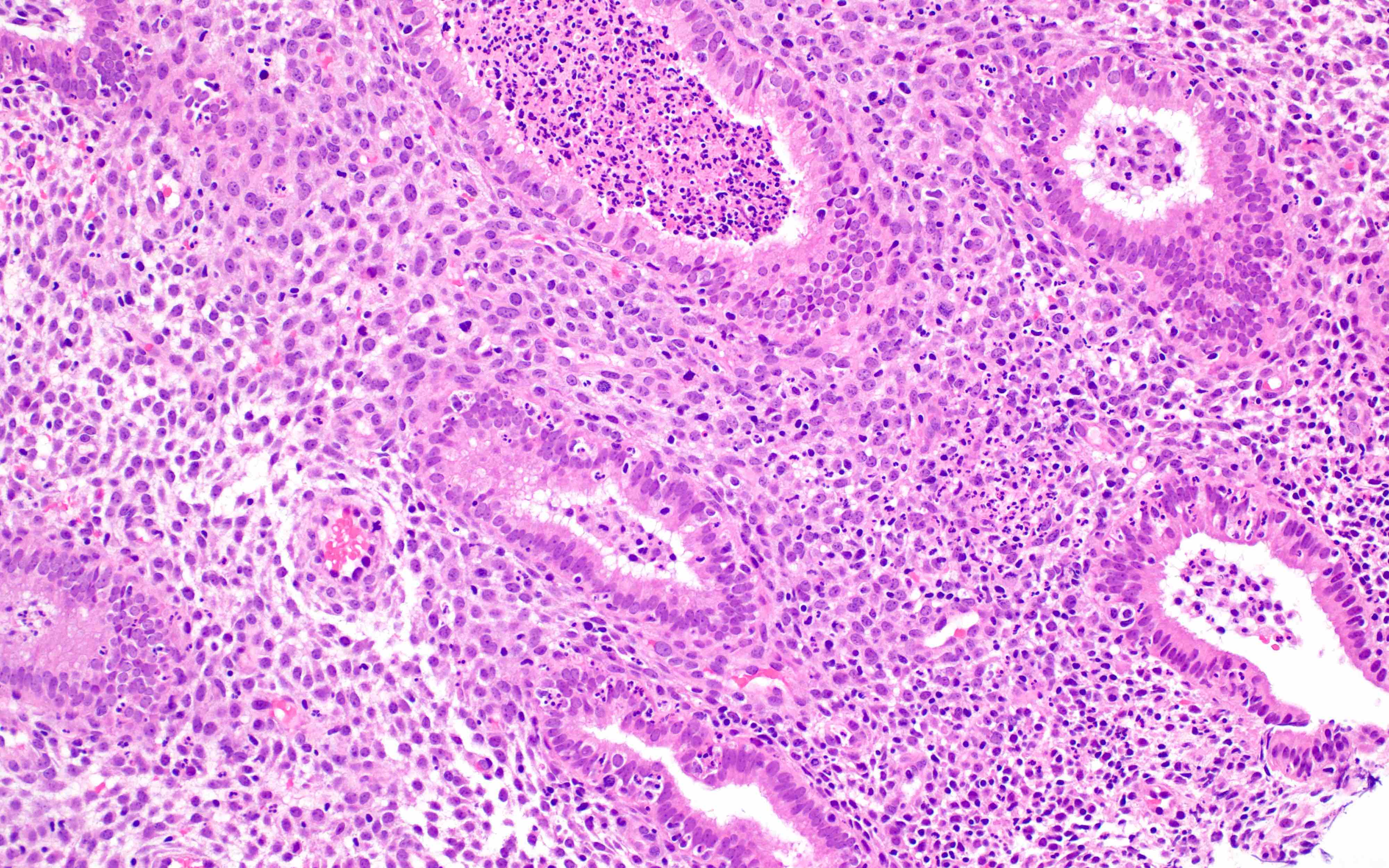
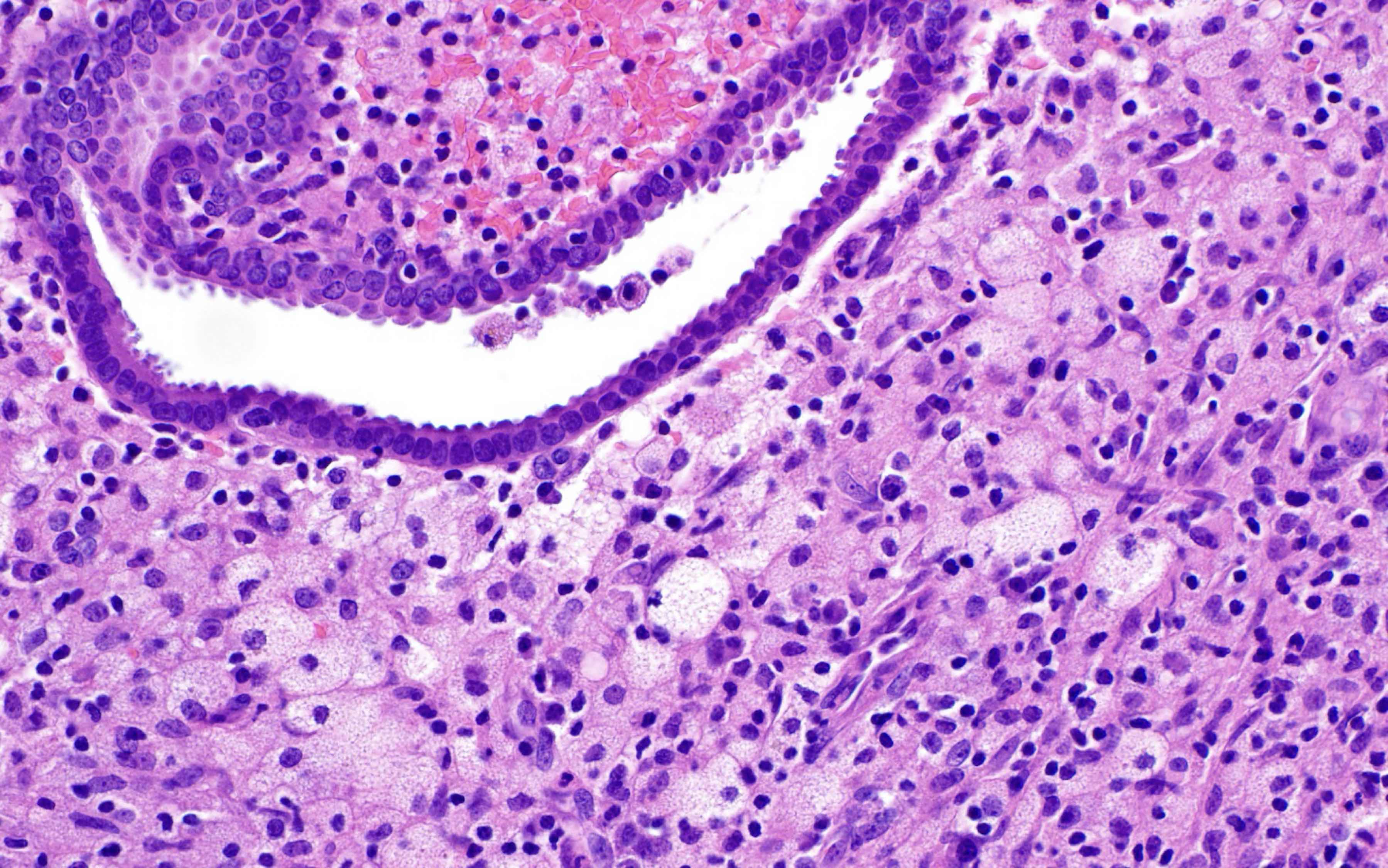
Chronic endometritis
Xanthogranulomatous endometritis
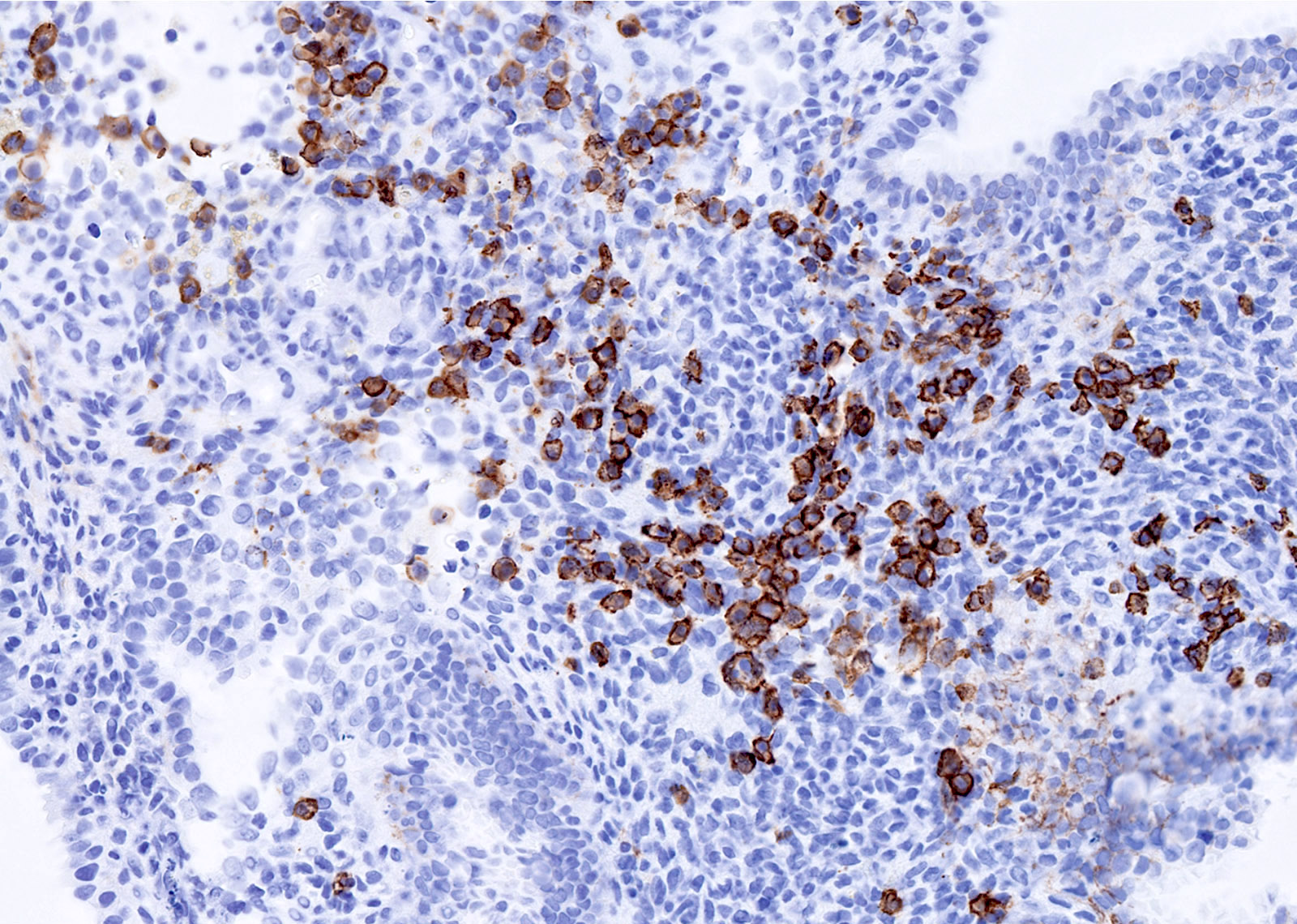
Positive stains
- Chronic endometritis
- CD138 / syndecan in plasma cells (Arch Pathol Lab Med 2004;128:1000)
- MUM1 in plasma cells; higher sensitivity, cleaner background (Int J Surg Pathol 2019;27:372)
Sample pathology report
- Endometrium, biopsy:
- Chronic endometritis
Differential diagnosis
- Predecidualized endometrial stromal cells:
- Lack "clock face" chromatin
- Plasma cell markers negative
- Lymphoma:
- Atypical proliferation of clonal lymphoid cells
Board review style question #1
Board review style answer #1
Board review style question #2
Which of the following conditions is thought to be associated with infertility and recurrent pregnancy loss?
- Acute endometritis
- Chronic endometritis
- Granulomatous endometritis
- Xanthogranulomatous endometritis
Board review style answer #2