Table of Contents
Definition / general | Essential features | Terminology | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Positive stains | Negative stains | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Goyette ERJ, Bentz JL. Endometrial metaplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/uterusmetaplasia.html. Accessed April 20th, 2024.
Definition / general
- Nonneoplastic cytomorphologic transformation of the epithelial lining of the uterine cavity from its usual endometrial phenotype to other subtypes of Müllerian epithelial differentiation
- While rare, endometrial stromal transformation to other mesenchymal elements can also occur
Essential features
- Epithelial metaplasia is replacement of the normal endometrium by a differentiated epithelium
- Endometrial metaplasia can be associated with hyperestrogenism, inflammation, repeated irritation or endometrial polyps
- Be sure to rule out a neoplastic process (endometrial hyperplasia or carcinoma)
- Epithelial metaplasias include squamous, mucinous, tubal, eosinophilic, papillary, secretory and hobnail
- Stromal metaplasias (while uncommon) include osseous, cartilaginous, myomatous, adipose and synovial-like
Terminology
- Epithelial cellular change
- Endometrial cytoplasmic change
Epidemiology
- Wide age range; most common in perimenopausal to postmenopausal women
Sites
- Endometrium, including endometrial polyps
Etiology
- Hyperestrogenism
- Exogenous hormone use / unopposed estrogens
- Polycystic ovarian syndrome (PCOS)
- Other causes of persistent anovulation
- Ovarian tumors secreting hormones
- Endometrial hyperplasia or carcinoma
- Prolonged irritation
- Mechanical
- Intrauterine device
- Previous hysteroscopy and manipulation
- Curettage
- Polypectomy
- Infectious / inflammatory
- Chronic endometritis
- Pyometria
- Physiologic
- Breakdown
- Mechanical
- No obvious cause in a small percentage of cases
- Reference: Virchows Arch 2018;472:907
Clinical features
- Some epithelial metaplasias (e.g. squamous or mucinous) tend to coexist with endometrial hyperplasia or carcinoma; this is not true for other epithelial metaplastic changes, such as tubal metaplasia or for the stromal metaplasias (Histopathology 2008;53:325)
Diagnosis
- Microscopic examination of endometrial biopsy / curettage or hysterectomy
Radiology description
- Ultrasound
- Generally no significant findings
- If osseous stromal metaplasia → strongly echogenic endometrial plate with posterior shadowing (Clin Imaging 2018;52:260)
Prognostic factors
- If isolated metaplasia → no clinical significance; no follow up necessary
- If associated with hyperplasia or frank malignancy → dependent upon associated condition (see endometrial hyperplasia and endometrial endometrioid carcinoma)
Case reports
- 31 year old woman with osseous metaplasia (Radiol Bras 2016;49:62)
- 38 year old woman with cartilaginous metaplasia (J Midlife Health 2013;4:195)
- 38 year old woman with tubal metaplasia (Int J Clin Exp Pathol 2015;8:7610)
- 63 and 74 year old women with intestinal metaplasia (Int J Gynecol Pathol 2011;30:492)
- 67 year old woman with ichthyosis uteri (Indian J Pathol Microbiol 2020;63:637)
Frozen section description
- Metaplasia might be mistaken for a hyperplasia on frozen section if the clinicians send a uterus to evaluate for carcinoma; awareness of this pitfall is important to avoid diagnosing an endometrial neoplasm on frozen section
Microscopic (histologic) description
- Squamous metaplasia:
- Subtypes:
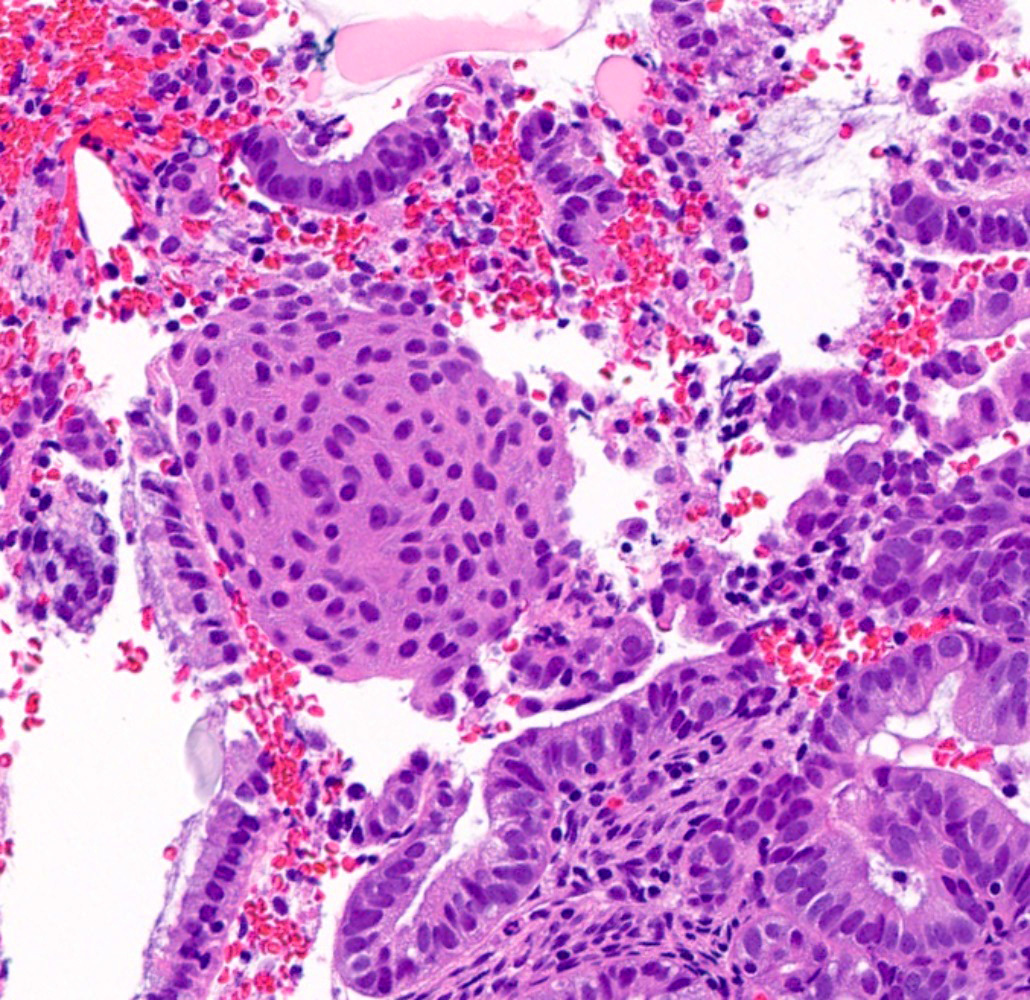
- Morular (Gynecol Endocrinol 2020;36:460):
- Rounded to polygonal nests of immature squamous cells that fill the glandular lumen
- Rarely demonstrates keratinization, mitoses and central necrosis
- Generally cytologically bland but can obscure examination of the glandular architecture
- Morular borders are not well defined
- Characteristic intercellular bridges are not identified
- More commonly associated with endometrioid adenocarcinoma
- Squamous metaplasia:
- Intercellular bridges
- With or without histiocystic or giant cell reaction to the keratin
- Ichthyosis uteri (Eur J Gynaecol Oncol 2011;32:699)
- Extensive replacement of surface endometrium with mature, keratinizing, squamous epithelium as a result of chronic inflammation or cervical obstruction
- Rarely becomes invasive squamous cell carcinoma (Eur J Gynaecol Oncol 2012;33:552)
- Morular (Gynecol Endocrinol 2020;36:460):
- Subtypes:
- Mucinous metaplasia (Gynecol Oncol 2015;136:389, Diagn Pathol 2017;12:39):
- Cuboidal to columnar cells, most commonly resembling endocervical epithelium
- Rarely, resembling gastric and intestinal type metaplasia
- Generally cytologically bland
- Subtypes (Mod Pathol 1999;12:1137):
- Type A: single cell layer lining the epithelial surface, with or without glandular involvement
- Type B: focal / patchy papillary / micropapillary changes
- Type C: extensive papillary, cribriform or microacinar architecture
- Mucinous metaplasia may be found in the ovaries or cervix of patients with endometrial mucinous metaplasia
- Cuboidal to columnar cells, most commonly resembling endocervical epithelium
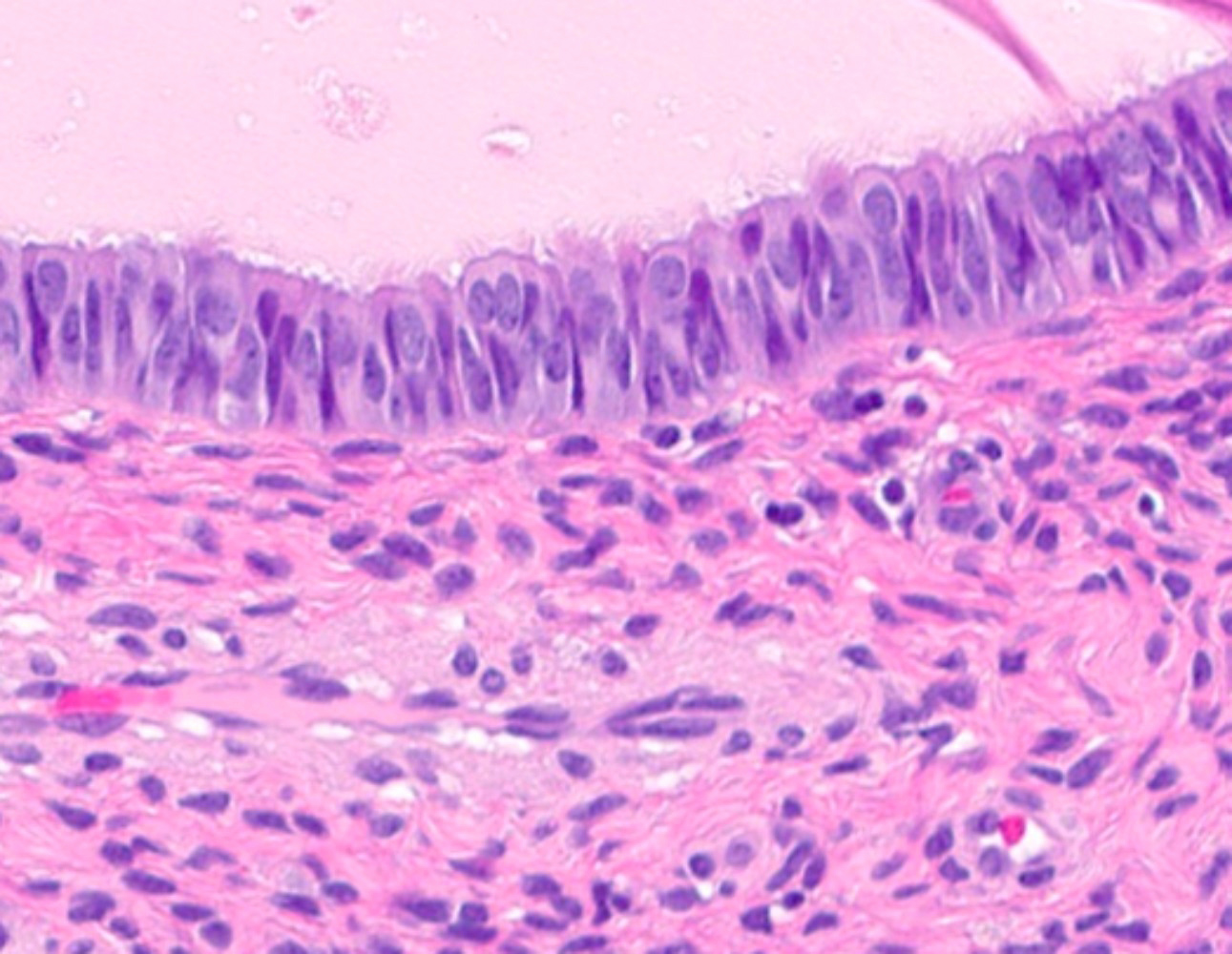
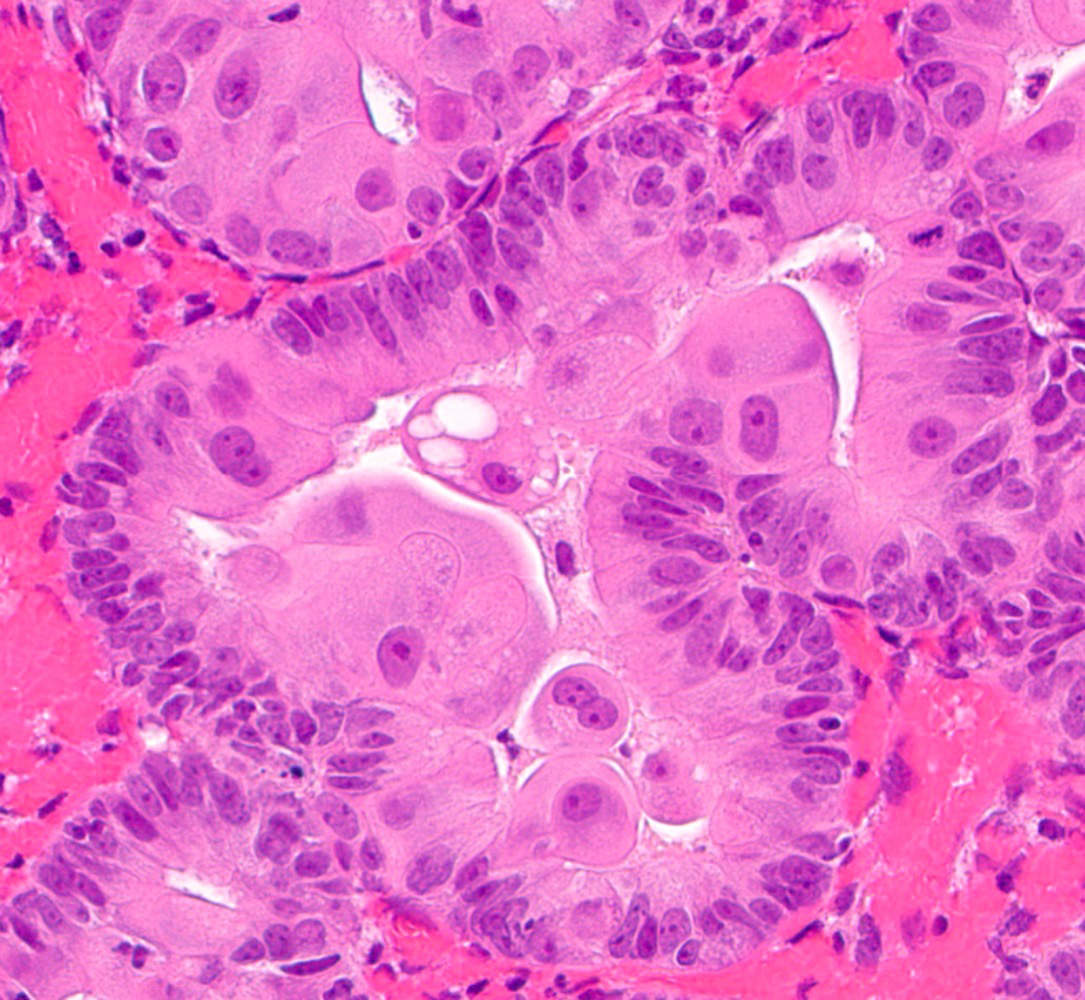
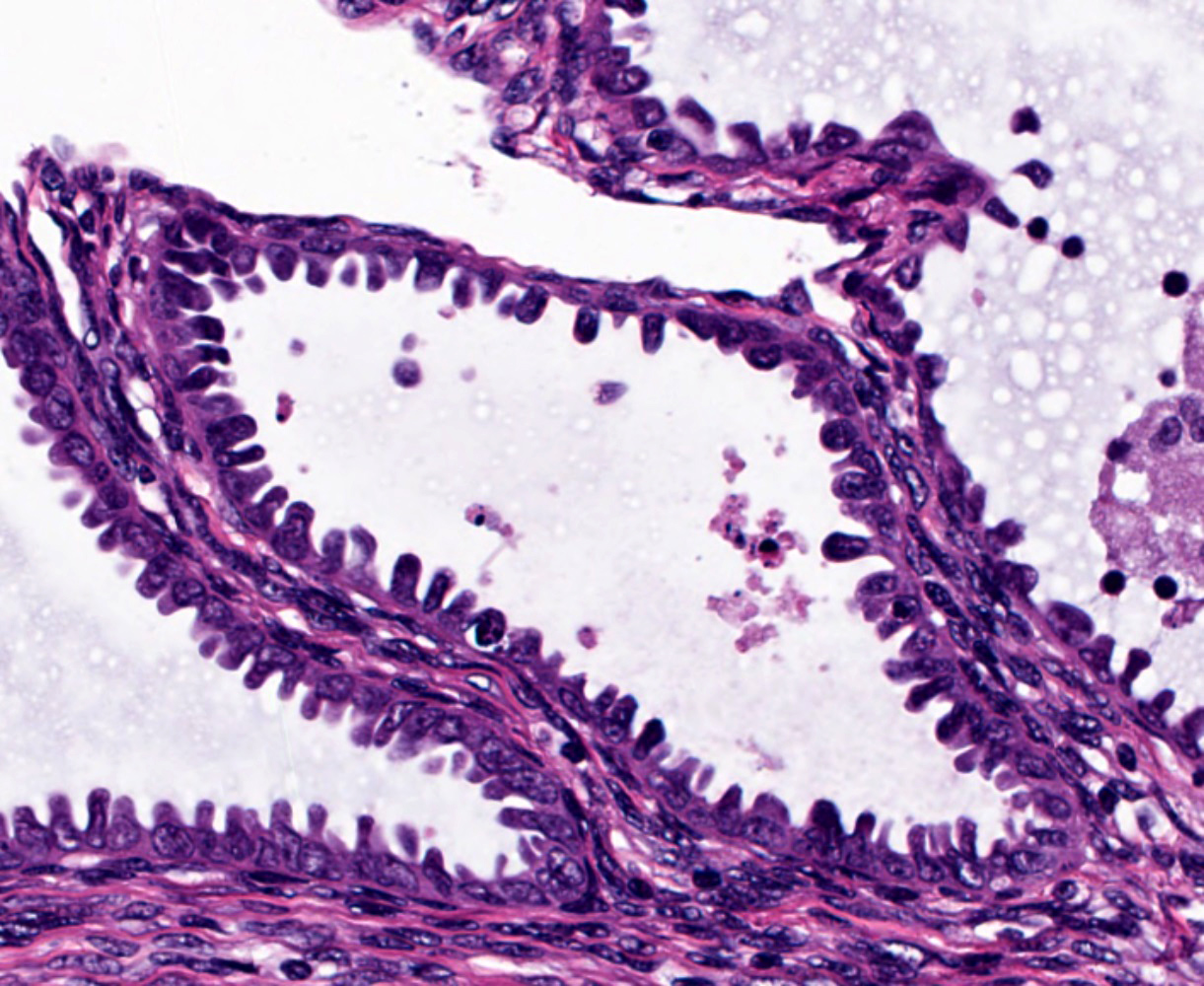
- Tubal metaplasia (Mod Pathol 2011;24:1254):
- Resembling fallopian tube epithelium; pseudostratified with ciliated eosinophilic cells and clear round cells
- Eosinophilic metaplasia:
- Cuboidal to columnar cells with prominent eosinophilic cytoplasm, ranging from granular to dense
- Round nuclei with or without degenerative atypia
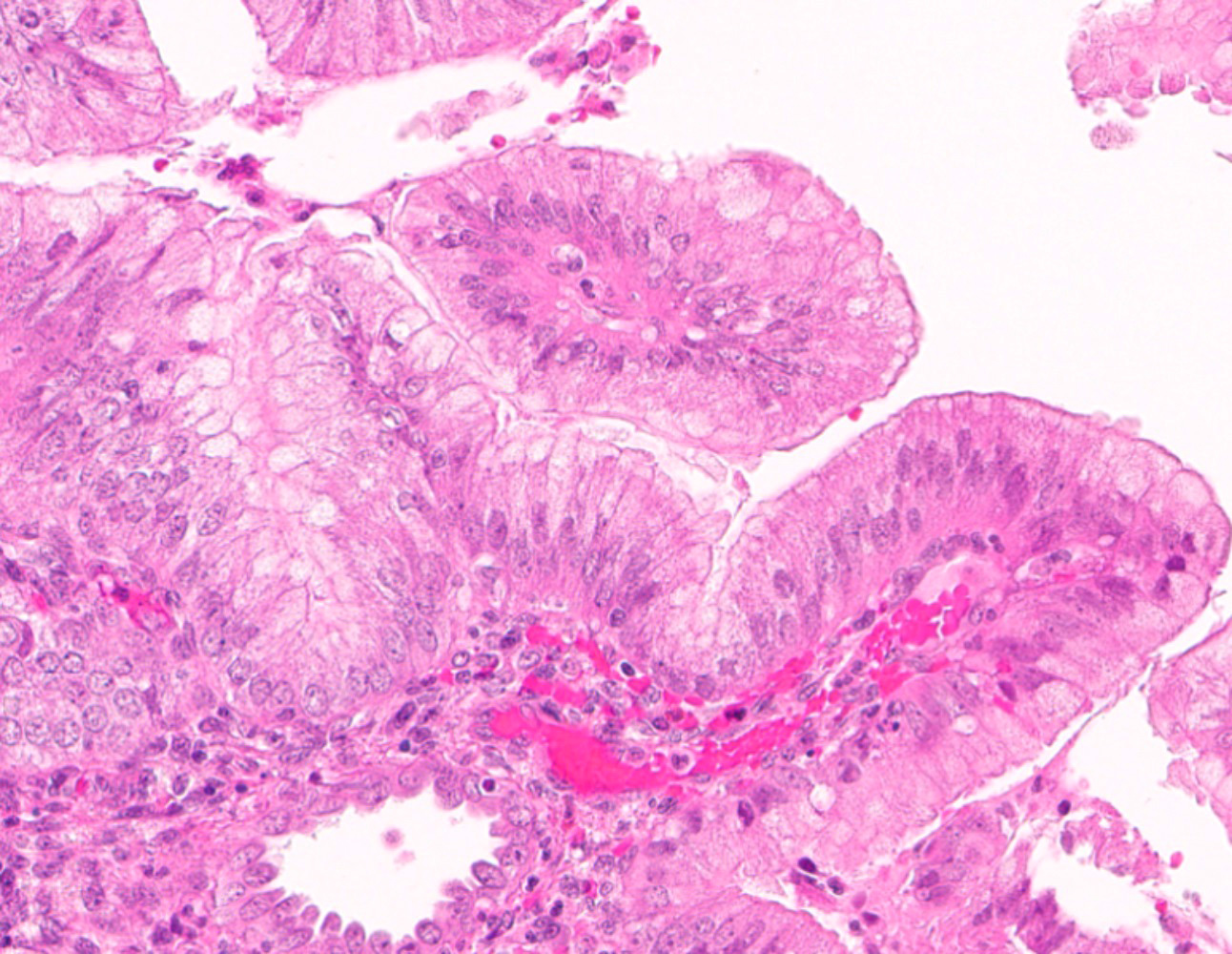
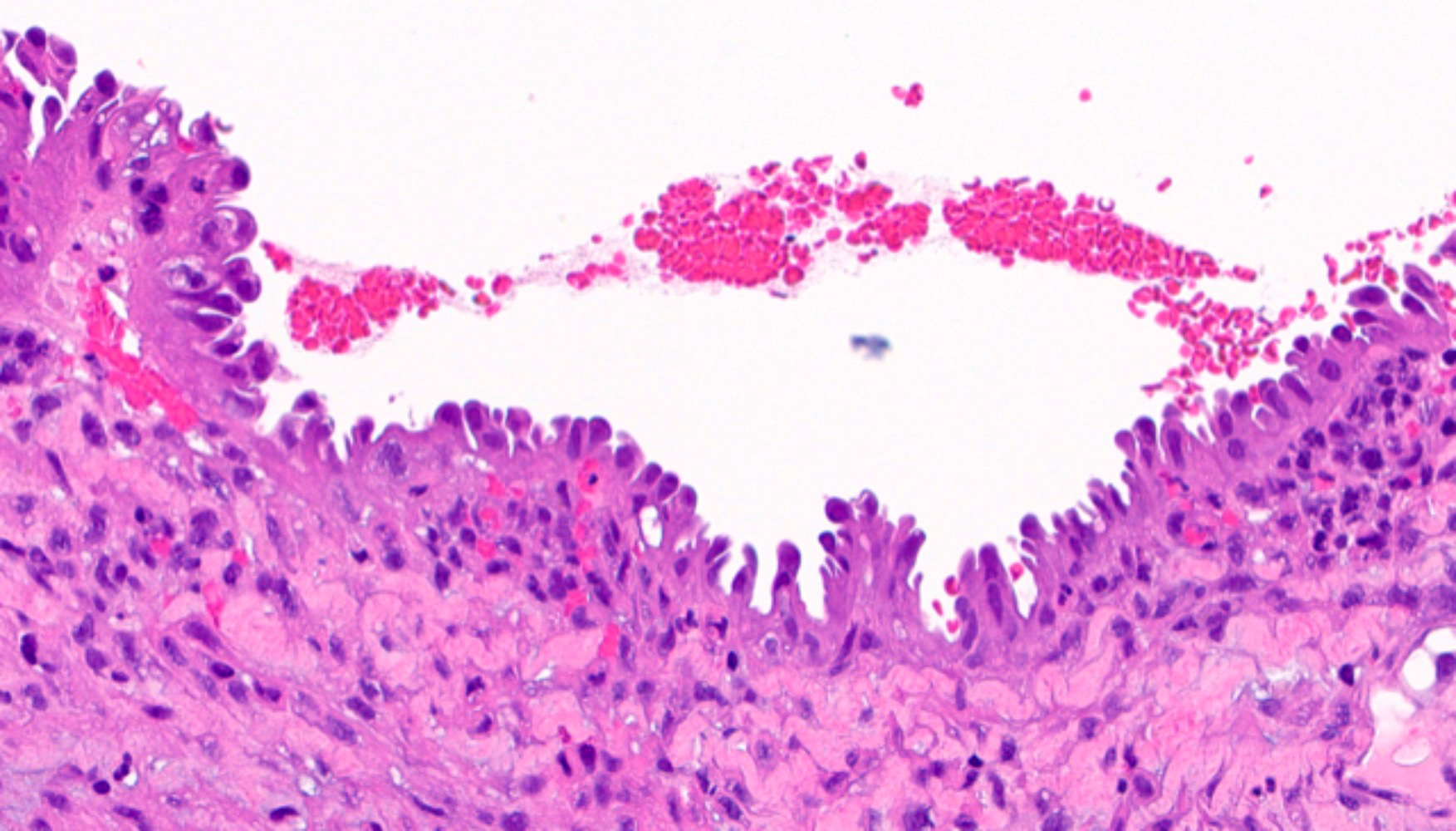
- Papillary metaplasia (Am J Surg Pathol 2013;37:167):
- Subtypes:
- Papillary syncytial: pseudostratified eosinophilic cells with indistinct cell borders and loss of nuclear polarity (Int J Gynecol Pathol 2012;31:206)
- Sometimes termed as pseudopapillary due to the absence of fibrovascular cores
- Generally located on the surface
- Associated with stromal breakdown
- Papillary proliferations: true papillae with fibrovascular cores (Am J Surg Pathol 2001;25:1347)
- Simple / localized: short, nonbranching
- Complex / diffuse: numerous branching with papillae and micropapillae
- Analogous to endometrial intraepithelial neoplasia / atypical hyperplasia
- Papillary syncytial: pseudostratified eosinophilic cells with indistinct cell borders and loss of nuclear polarity (Int J Gynecol Pathol 2012;31:206)
- Subtypes:
- Secretory metaplasia:
- Resembling early to late secretory endometrium, with subnuclear to supranuclear vacuolization
- Hobnail metaplasia:
- Glandular, often eosinophilic cells with apically located nuclei that protrude into the lumen
- Can have cytoplasmic vacuolization
- Generally cytologically bland
- Glandular, often eosinophilic cells with apically located nuclei that protrude into the lumen
- Stromal metaplasias:
- Subtypes:
- Osseous
- Cartilaginous
- Myomatous
- Adipose
- Synovial-like (Int J Gynecol Pathol 2015;34:570)
- Subtypes:
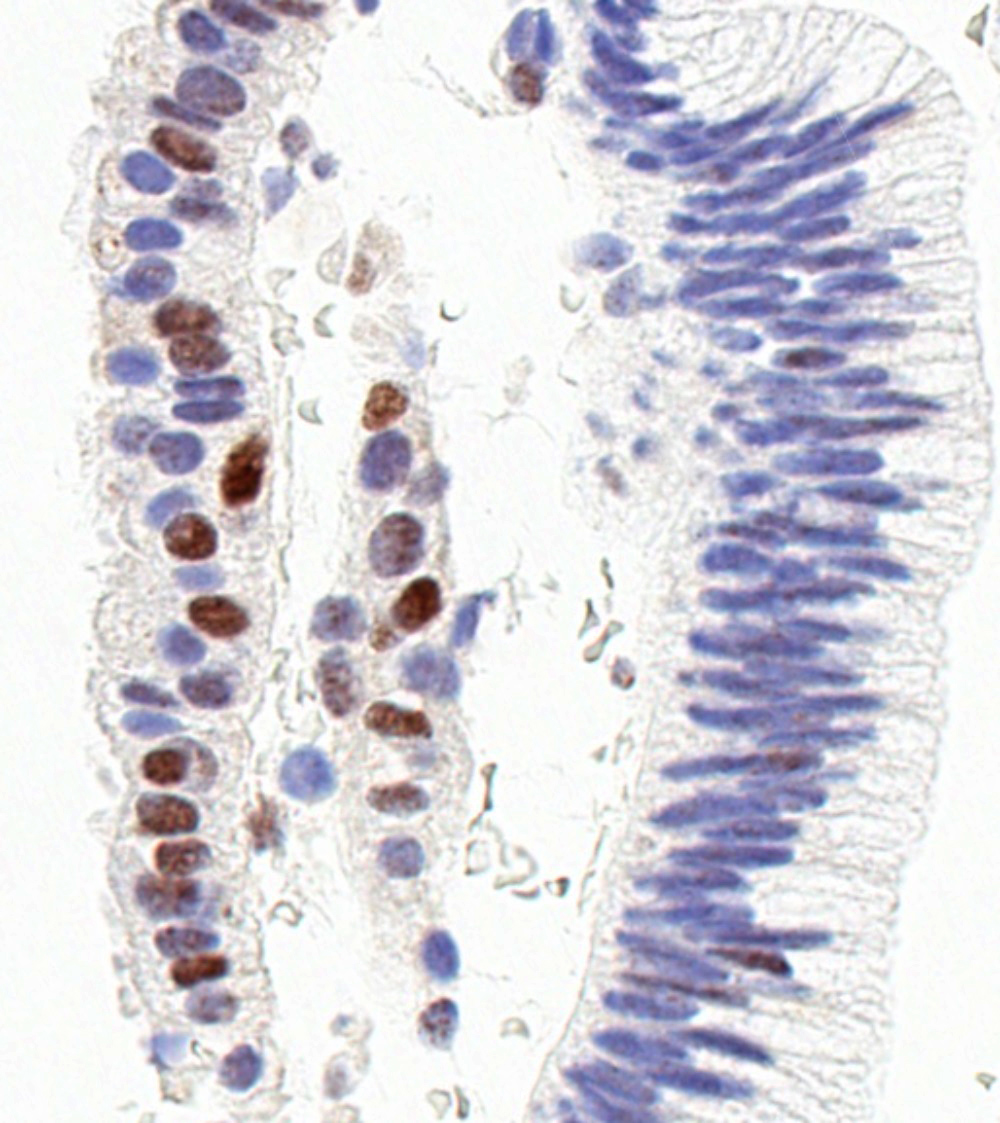
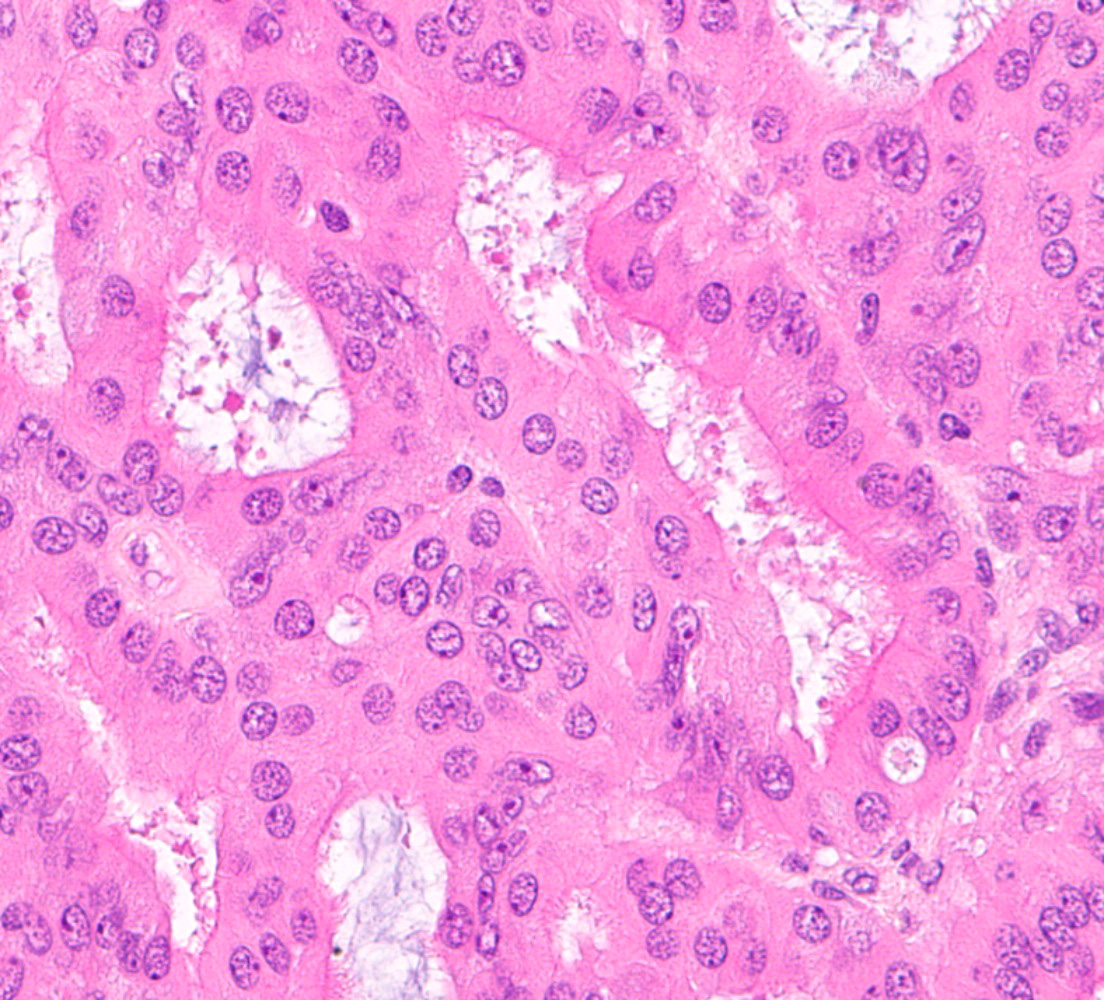
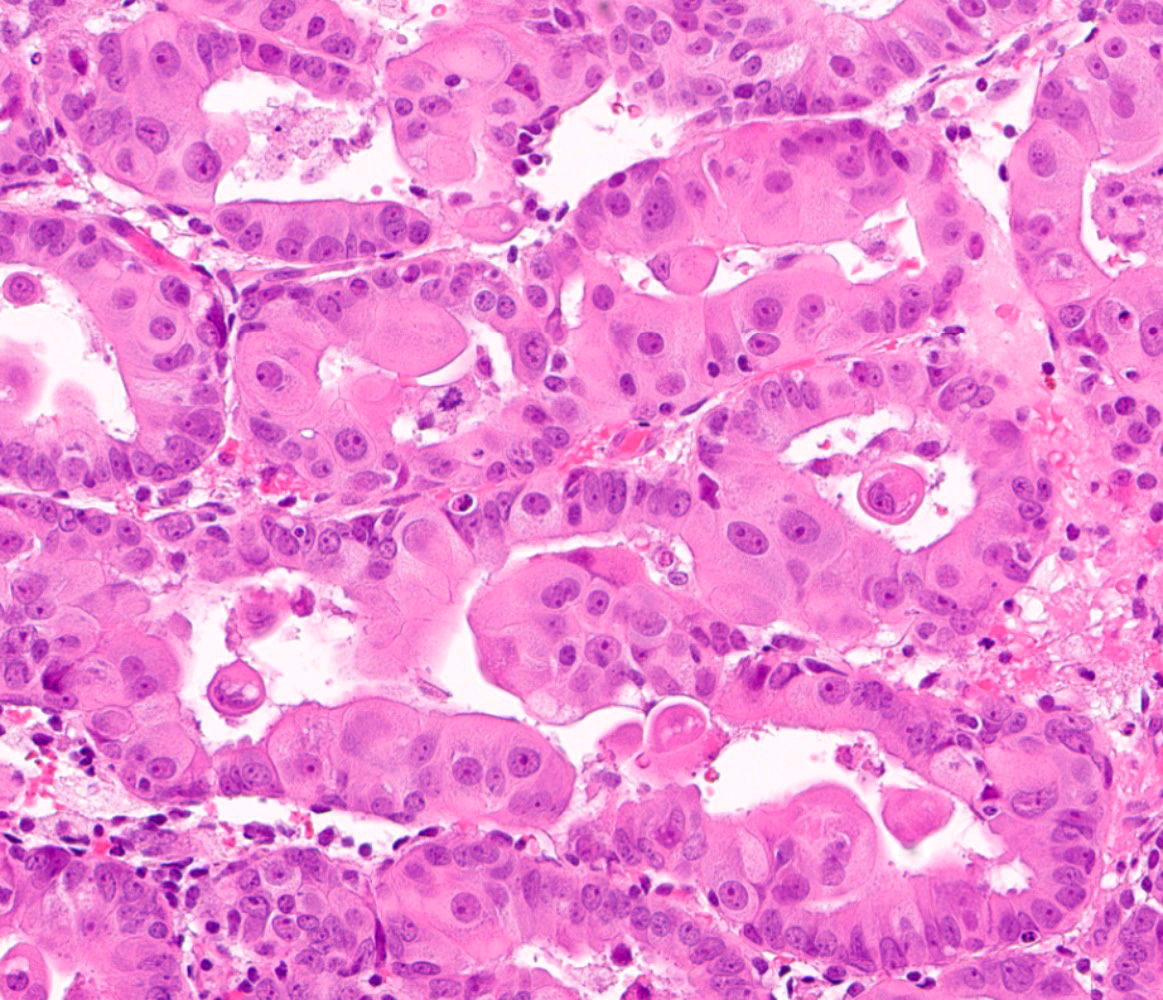
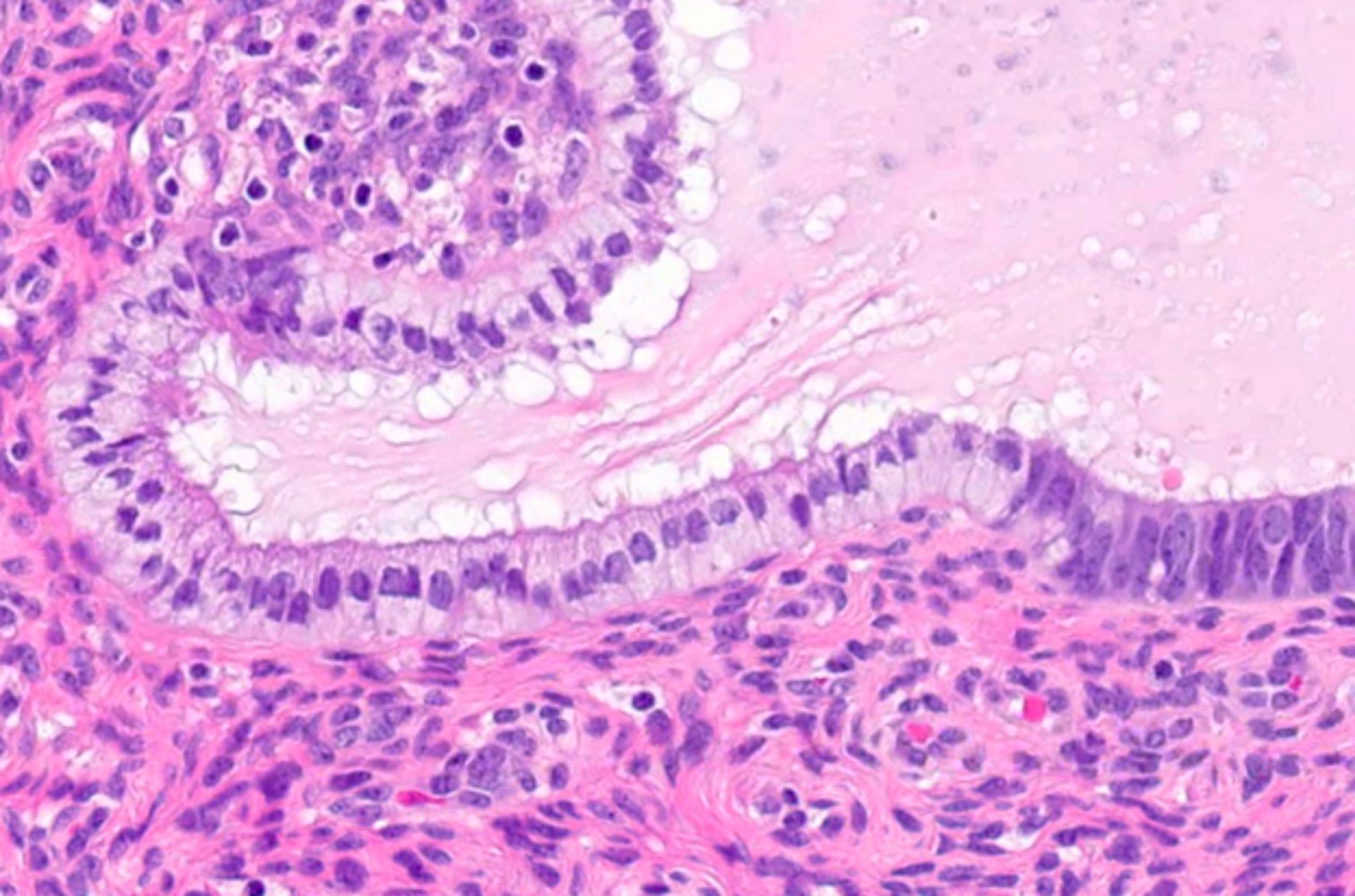
Microscopic (histologic) images
Contributed by Jessica L. Bentz, M.D.
Positive stains
- Morular metaplasia:
- CD10, CDX2, SATB2, beta catenin (nuclear and cytoplasmic)
- Mucinous metaplasia (Mod Pathol 2012;25:1496):
- Hobnail metaplasia:
- Papillary syncytial metaplasia (Int J Gynecol Pathol 2012;31:206):
Negative stains
- Morular metaplasia:
- Mucinous metaplasia (Mod Pathol 2012;25:1496):
- Simple: p16, PTEN, beta catenin
- Complex (papillary): PAX2, PR, PTEN, beta catenin
- Low Ki67 proliferative index
- Hobnail metaplasia:
- Secretory changes:
- Low Ki67 proliferative index
- Papillary syncytial metaplasia (Int J Gynecol Pathol 2012;31:206):
Videos
Benign and premalignant lesions of the endometrium - Dr. Parra-Herran, from pathCast
Sample pathology report
- Endometrium, biopsy:
- Complex atypical hyperplasia (endometrial intraepithelial neoplasia) with metaplastic changes (see comment)
- Comment: There are foci with cytologic atypia that exceed the allowable spectrum of atypical changes seen in endometrial metaplasia. Therefore, the findings are most consistent with atypical endometrial hyperplasia.
Differential diagnosis
- For squamous metaplasia:
- Squamous cell carcinoma:
- Cytologic malignancy with invasion
- Mitoses
- Show immunophenotype typical of squamous differentiation
- Diffuse p16 expression may suggest cervical origin of a squamous carcinoma
- Reactive / reparative
- Atypical polypoid adenomyoma:
- Polypoid lesion with prominent myofibroblastic stroma and endometrial intraepithelial neoplasia
- Squamous cell carcinoma:
- For mucinous metaplasia:
- Benign endocervical proliferations:
- Presence of reserve cells
- Endometrial neoplasia with progestin effect
- Benign endocervical proliferations:
- For tubal metaplasia:
- Atypical endometrial hyperplasia / endometrial intraepithelial neoplasia
- Serous carcinoma:
- For eosinophilic metaplasia:
- For papillary metaplasia:
- Surface repair
- Serous carcinoma:
- For secretory metaplasia:
- Clear cell carcinoma:
- Malignant nuclear features
- Clinically, may describe a mass lesion
- Arias-Stella reaction:
- Pregnancy, trophoblastic disease, progestin therapy
- Decidualization of the stroma
- Low nuclear to cytoplasmic ratio without stromal invasion
- Clear cell carcinoma:
- For hobnail metaplasia:
- Serous carcinoma
- Clear cell carcinoma (Histopathology 2014;64:585):
- Arias-Stella reaction (Int J Gynecol Pathol 2004;23:223):
- Nucleomegaly with exaggerated hyperplastic appearance and centronuclear vacuolization with hormone effect
- Pregnancy, trophoblastic disease, progestin therapy
- Decidualization of the stroma
- Low nuclear to cytoplasmic ratio without stromal invasion
- For stromal metaplasias:
- Retained fetal parts
- Heterologous elements in carcinosarcoma or adenosarcoma
- If adipose stromal metaplasia → consider uterine perforation
Additional references
Board review style question #1
A 53 year old woman presents to the gynecologist with chief complaint of vaginal bleeding. An endometrial biopsy is performed and shows fragments of ciliated inactive endometrial tissue with foci of cytologic atypia. Immunohistochemical studies show a wild type pattern of p53 expression, patchy expression of p16 and low Ki67 proliferative index. What is the most likely diagnosis?
- Atypical endometrial hyperplasia
- Endometrioid adenocarcinoma
- Hobnail metaplasia
- Serous endometrial intraepithelial carcinoma (SEIC)
- Tubal metaplasia
Board review style answer #1
Board review style question #2
What subtype of carcinoma is most commonly associated with squamous metaplasia?
- Endometrioid adenocarcinoma
- Invasive squamous cell carcinoma of the cervix
- Ovarian high grade serous carcinoma
- Uterine carcinosarcoma
- Uterine serous carcinoma
Board review style answer #2