16 October 2009 - Case #160
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Daniel Ostler, Baylor College of Medicine, Texas (USA).


This 20-hour workshop is designed to address the activities and issues faced by the surgical pathologist.
The 24th Annual Surgical Pathology Workshop consists of short lectures and case-oriented discussions. Microscopes will be available. Participants will be asked to examine microscopic images and formulate a diagnosis and patient management strategy. The faculty pathologist will then discuss the diagnosis, differential diagnosis, patient management, and other pertinent features. Cases will be selected to represent common and/or difficult diagnostic problems.
This workshop will be held at The Canyons in Park City, Utah. Bring the family and have an incredible winter getaway!
Advertisement
Case #160
Clinical history:
A 52 year old woman presented with chronic, diffuse, lichenified eruptions on her leg. A biopsy was obtained.
Microscopic images:
What is your diagnosis?
Diagnosis: Scabies
Discussion:
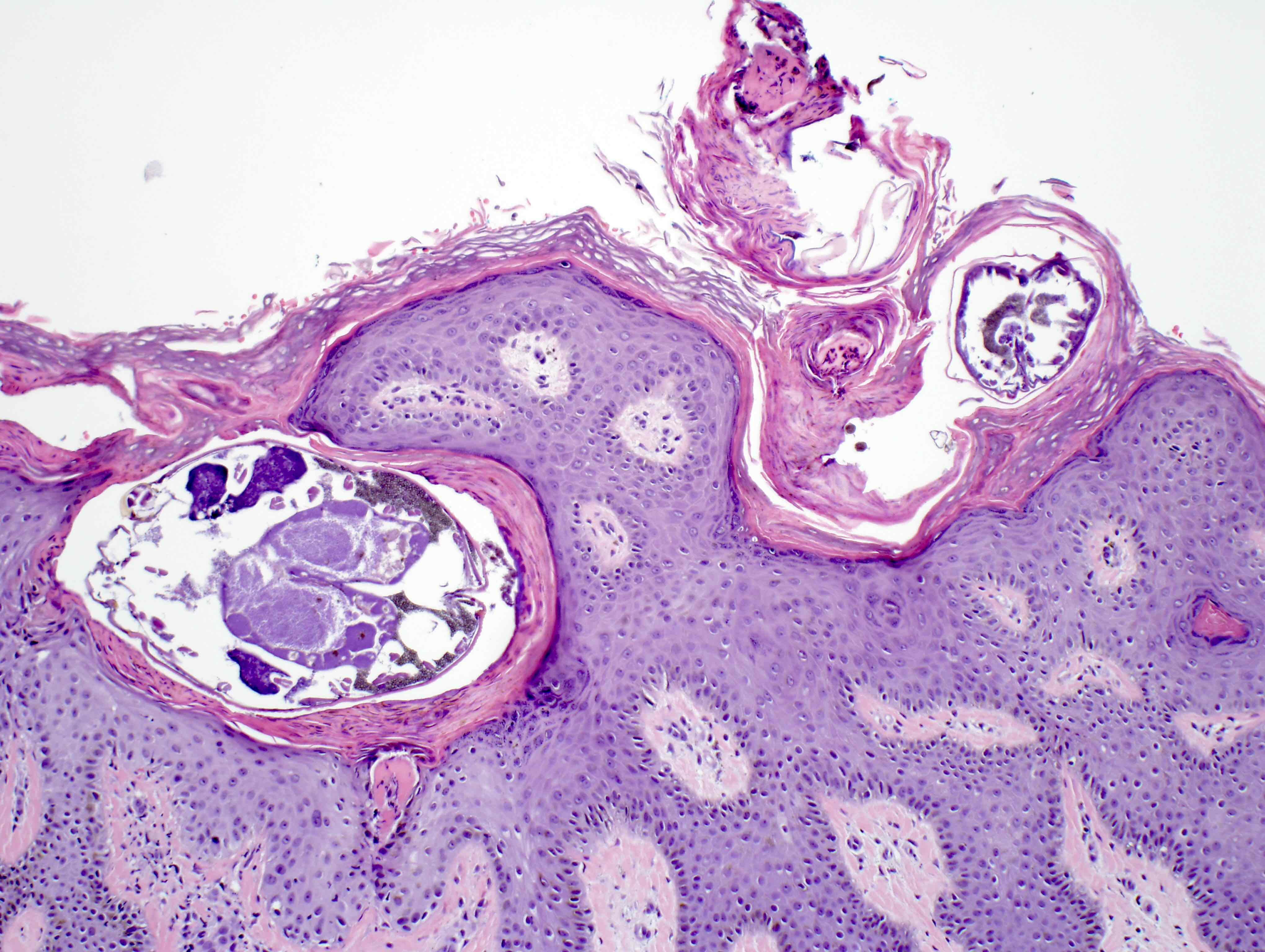
Histology revealed mites in the epidermis (figures 1 and 2). Figure 3 shows a mite and scybala (hardened masses of feces).
Scabies, the first human disease recognized as caused by a specific pathogen, is caused by the mite Sarcoptes scabiei, which burrows into the skin and causes intense itching (eMedicine: Scabies [Accessed 25 April 2024]). It is highly contagious and difficult to diagnose early; symptoms may not occur for up to 6 weeks after infection (Clin Microbiol Rev 2007;20:268). Diagnosis requires examining the skin for burrows, then confirming the presence of mites, ova or scybala by microscopy (Dermatol Ther 2009;22:279).
Scabies is spread by prolonged (15 to 20 minutes) skin to skin contact with an infected individual, often as a sexually transmitted disease or between members of a household. Overcrowding in hospitals or nursing homes may also encourage its spread. Although animals can get scabies, they do not spread human scabies. Bedding or clothing of infected individuals should be machine washed and dried with hot water or sealed in a plastic bag for at least 3 days (CDC: Parasites - Scabies [Accessed 25 April 2024]).
Excessive scratching may lead to sores, bacterial infections and even glomerulonephritis (Postgrad Med J 2004;80:382). Patients with immunocompromise are at risk for developing crusted scabies, also called Norwegian scabies, characterized by scaly rashes, a thickening of the skin, and an overwhelming number of mites (J Am Podiatr Med Assoc 2004;94:583).
Clinically, scabies can mimic eczema, mycosis fungoides, syphilis and bullous pemphigoid (Dermatol Online J 2006;12:19). Scratch marks often obscure signs of burrows. Microscopic examination is required for definitive diagnosis.
Treatment consists of topical permethrin (drug of choice), topical lindane or oral ivermectin (Am J Clin Dermatol 2002;3:9). Topical treatments must coat the body to be effective. Household members and close personal contacts should be treated at the same time.
References: Wikipedia: Scabies [Accessed 25 April 2024]
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Daniel Ostler, Baylor College of Medicine, Texas (USA).


This 20-hour workshop is designed to address the activities and issues faced by the surgical pathologist.
The 24th Annual Surgical Pathology Workshop consists of short lectures and case-oriented discussions. Microscopes will be available. Participants will be asked to examine microscopic images and formulate a diagnosis and patient management strategy. The faculty pathologist will then discuss the diagnosis, differential diagnosis, patient management, and other pertinent features. Cases will be selected to represent common and/or difficult diagnostic problems.
This workshop will be held at The Canyons in Park City, Utah. Bring the family and have an incredible winter getaway!
Website news:
(1) We have updated the Breast-malignant chapter. Each topic now has clear, concise formatting and thumbnail images.
Visit and follow our Blog to see recent updates to the website.
(1) We have updated the Breast-malignant chapter. Each topic now has clear, concise formatting and thumbnail images.
Visit and follow our Blog to see recent updates to the website.
Case #160
Clinical history:
A 52 year old woman presented with chronic, diffuse, lichenified eruptions on her leg. A biopsy was obtained.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Scabies
Discussion:
Histology revealed mites in the epidermis (figures 1 and 2). Figure 3 shows a mite and scybala (hardened masses of feces).
Scabies, the first human disease recognized as caused by a specific pathogen, is caused by the mite Sarcoptes scabiei, which burrows into the skin and causes intense itching (eMedicine: Scabies [Accessed 25 April 2024]). It is highly contagious and difficult to diagnose early; symptoms may not occur for up to 6 weeks after infection (Clin Microbiol Rev 2007;20:268). Diagnosis requires examining the skin for burrows, then confirming the presence of mites, ova or scybala by microscopy (Dermatol Ther 2009;22:279).
Scabies is spread by prolonged (15 to 20 minutes) skin to skin contact with an infected individual, often as a sexually transmitted disease or between members of a household. Overcrowding in hospitals or nursing homes may also encourage its spread. Although animals can get scabies, they do not spread human scabies. Bedding or clothing of infected individuals should be machine washed and dried with hot water or sealed in a plastic bag for at least 3 days (CDC: Parasites - Scabies [Accessed 25 April 2024]).
Excessive scratching may lead to sores, bacterial infections and even glomerulonephritis (Postgrad Med J 2004;80:382). Patients with immunocompromise are at risk for developing crusted scabies, also called Norwegian scabies, characterized by scaly rashes, a thickening of the skin, and an overwhelming number of mites (J Am Podiatr Med Assoc 2004;94:583).
Clinically, scabies can mimic eczema, mycosis fungoides, syphilis and bullous pemphigoid (Dermatol Online J 2006;12:19). Scratch marks often obscure signs of burrows. Microscopic examination is required for definitive diagnosis.
Treatment consists of topical permethrin (drug of choice), topical lindane or oral ivermectin (Am J Clin Dermatol 2002;3:9). Topical treatments must coat the body to be effective. Household members and close personal contacts should be treated at the same time.
References: Wikipedia: Scabies [Accessed 25 April 2024]