25 March 2010 – Case of the Week #174
This email is only sent to subscribers. To subscribe or unsubscribe to this or our other email lists, click here.
All cases are archived on our website. To view them sorted by number, diagnosis or category, visit our Home Page and click on the Case of the Week button on the left hand side.
Thanks to Dr. Jaya Mahajan, North Shore-Long Island Jewish Health System, New York (USA) for contributing this case. To contribute a Case of the Week, follow the guidelines on our Case of the Week page.
Website news:
(1) Thanks for stopping by our booth at USCAP. We appreciate your support and feedback, and are working on implementing your suggestions.
(2) We are looking for pathologists to review topics in our Stains or CD Markers chapters, a chapter or a section of a chapter. We pay reviewers for chapters and sections, and list the name of the reviewer on each topic page and on our Author / Reviewer page. If you are interested, email us your areas of interest and CV.
(3) We are currently updating the Bladder and Breast-nonmalignant chapters.
Case of the Week #174
Clinical History
A 45 year old Guyanese woman presented to the Emergency Department with an increasingly severe headache, progressive dizziness, weakness and difficulty walking over the previous week. Her headache was occipital and throbbing, was not associated with visual changes and was not relieved by Tylenol. She had no significant medical history and no history of sick contacts, recent travel, insect bites, nausea or vomiting. Her social history was negative for tobacco, alcohol or intravenous drug use.
CNS imaging revealed an enhancing left cerebellar mass with surrounding edema and leptomeningeal spread. The differential diagnosis was broad and included primary CNS neoplasm, metastatic disease, a demyelinating process or an infectious etiology. Empiric treatment with antibiotics and steroids failed to improve the patient's symptoms.
The patient underwent an emergency cerebellar biopsy.
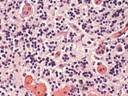
Micro images:
What is your diagnosis?
Diagnosis:
CNS Toxoplasmosis
Discussion:
Significant laboratory results (received after the biopsy) included a positive HIV test and a CD4 count of 28.
In patients with AIDS, toxoplasmosis typically produces brain abscesses with a characteristic central avascular area, surrounded by necrosis and inflammatory cells that may also contain free and intracellular tachyzoites. Cysts may be present outside of the region of inflammation, and contain numerous bradyzoites visible with H&E. PAS, GMS and imunohistochemistry are also useful.
Toxoplasma gondii is an obligate intracellular parasite generally hosted by cats or other warm-blooded animals, which is transmitted to humans by contact with kitty litter or eating undercooked meat (life cycle-CDC). The infection may also be passed from mother to fetus during pregnancy.
The parasites may form cysts in the eye, skeletal muscle, myocardium and brain. Infected individuals may initially present with flu-like symptoms, but are usually asymptomatic. Immunocompromised individuals, such as those with HIV or AIDS, may be the most severely affected. Acute toxoplasmosis in these patients may present with muscle soreness, swollen lymph nodes and skin lesions. PCR of cerebrospinal fluid may be useful in diagnosing Toxoplasmosis infection in HIV/AIDS patients (J Med Microbiol 1996;45:472, Braz J Infect Dis 2009;13:18, Cerebrospinal Fluid Res 2009;6:2). Serology is not useful for diagnosis, because up to 70% of the population is seropositive.
Treatment consists of acute and chronic antimicrobial therapy (AETC National Resource Center), as well as treatment of the underlying HIV, if present.
Of note, infection has been linked to behavioral changes and may have a causal relationship with schizophrenia (Parasitol Res 2009;105:893, Neuroimmunomodulation 2009;16:122).
Additional references: eMedicine, PathologyOutlines.com-lymph nodes
Nat Pernick, M.D., President,
and Kara Hamilton, M.S., Associate Medical Editor
PathologyOutlines.com, Inc.
30100 Telegraph Road, Suite 408
Bingham Farms, Michigan (USA) 48025
Telephone: 248/646-0325
Email: NatPernick@Hotmail.com
Alternate email: NatPernick@gmail.com