1 July 2005 - Case #12
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Ins Raoelfils, Centre Jean Perrin, Clermont-Ferrand, France for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Case #12
Clinical history:
A 22 year old woman had a large right ovarian mass, which was excised.
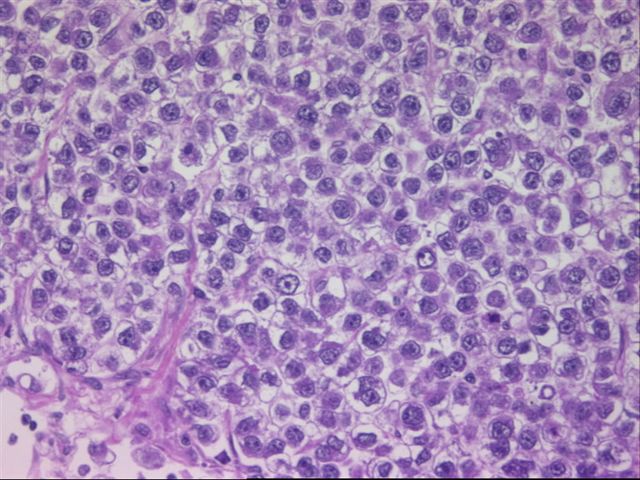
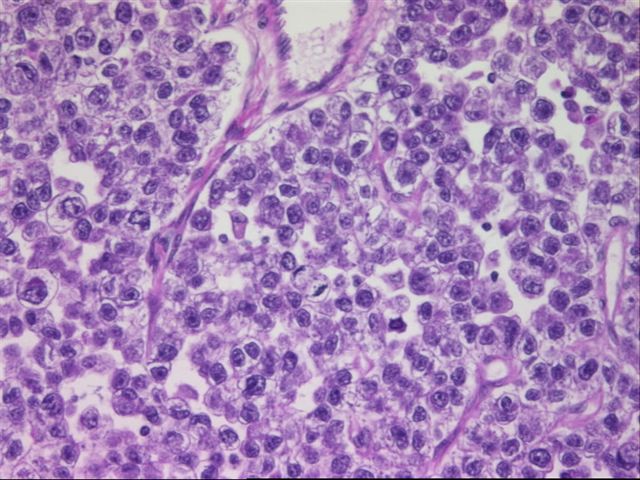
Micro images:
What is your diagnosis?
Diagnosis: Dysgerminoma of the ovary
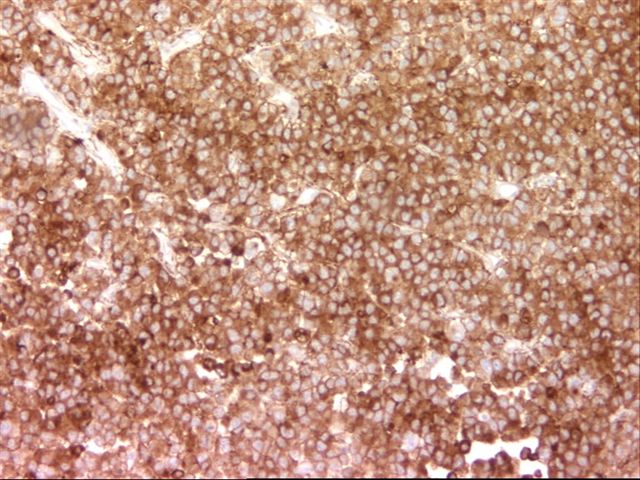
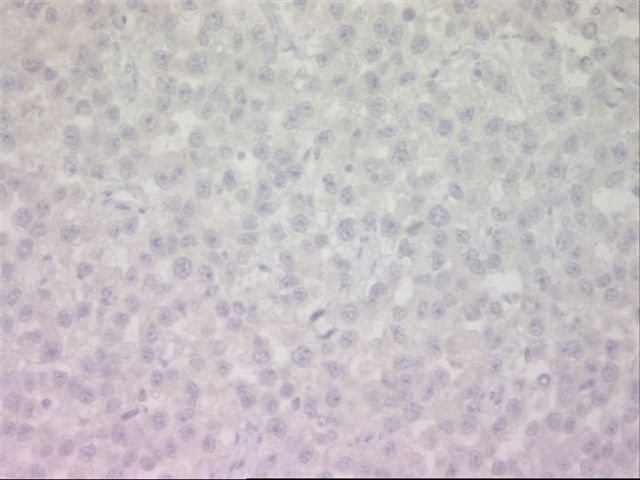
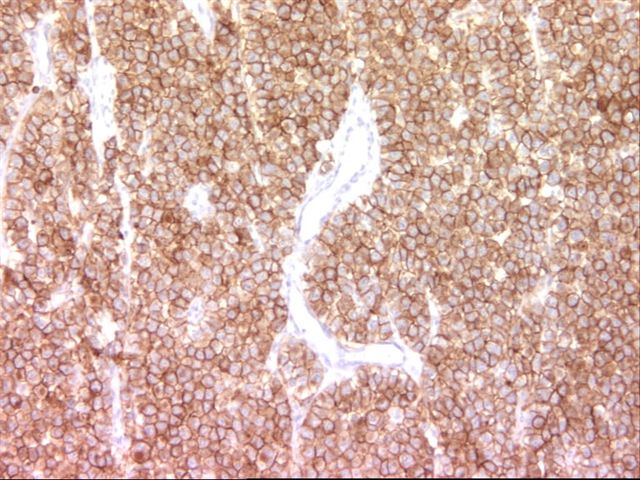
Immunohistochemistry images:
Immunohistochemistry:
The immunohistochemistry was interpreted as PLAP positive, AFP negative, KIT positive.
Discussion:
Dysgerminoma of the ovary is an uncommon tumor, representing < 1% of ovarian malignancies. They usually affect young patients, with 80% under age 30 years. 15% have bilateral tumors. ~5% are associated with gonadal dysgenesis, androgen insensitivity or pseudohermaphroditism. Some cases appear to represent progression from gonadoblastomas (Virchows Arch 2005;447:603). Patients with dysgerminomas typically present with low stage and have a 95% survival. Metastases can occur to the opposite ovary, retroperitoneal lymph nodes or the peritoneal cavity but often don't affect survival. Dysgerminomas are typically treated with surgery and chemotherapy and not radiotherapy, which may impair fertility in these usually young patients (NIH: Ovarian Germ Cell Tumors Treatment [Accessed 12 October 2023]). Dysgerminomas may rarely transform to a yolk sac tumor and may be mixed with other germ cell tumors, such as choriocarcinoma, yolk sac tumor or embryonal carcinoma, which worsens the prognosis (Mod Pathol 1995;8:881). Thus, it is important to adequately section these tumors and search for different looking areas of the tumor.
Dysgerminomas are grossly solid and nodular tumors of variable size. They are gray-pink, resembling cerebral cortex and commonly have hemorrhage and necrosis. Microscopically, they are composed of tumor cells separated by fibrous stroma with T lymphocytes. The tumor cells are large with well defined cell borders. The cytoplasm contains glycogen and the nuclei are central, vesicular and contain one or more prominent nucleoli. Granulomas may be present.
The differential diagnosis includes yolk sac tumor, undifferentiated carcinoma, clear cell adenocarcinoma (usually in postmenopausal women, PLAP negative), lymphoma, melanoma, granulosa cell tumor and metastatic breast carcinoma. Careful review of the histology of multiple sections, special stains and clinical history are helpful in distinguishing these other tumors. Dysgerminomas are immunoreactive for PLAP, KIT and vimentin. They may be focally positive for hCG in giant cells and focally positive for cytokeratin. They are negative for AFP. Recent reports indicate that OCT4, a transcription factor involved in the regulation of pluripotency during embryonic development, is sensitive and relatively specific for dysgerminomas (Am J Surg Pathol 2004;28:1341).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Ins Raoelfils, Centre Jean Perrin, Clermont-Ferrand, France for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Website news:
(1) This week's case is sponsored by Invitrogen. The Zymed EGFr antibody clone 31G7 is the most widely referenced clone and the industry standard for EGFr detection in formalin fixed, paraffin embedded (FFPE) tissue samples. Zymed's 31G7 antibody is extremely specific for EGFr and does not react with the highly homologous c-erbB-2 (HER2) protein. Invitrogen now offers the Zymed 31G7 antibody clone as part of a convenient, standardized immunohistochemical kit for the detection of EGFr protein expression in normal and neoplastic tissue. Invitrogen's Zymed EGFr Kit is compatible with manual or automated immunostainers and offers the greatest flexibility with FFPE tissue samples. For more information, visit www.invitrogen.com/antibodies. Note: sponsors do NOT have access in any manner to email addresses or other personal information in the possession of PathologyOutlines.com.
Visit and follow our Blog to see recent updates to the website.
(1) This week's case is sponsored by Invitrogen. The Zymed EGFr antibody clone 31G7 is the most widely referenced clone and the industry standard for EGFr detection in formalin fixed, paraffin embedded (FFPE) tissue samples. Zymed's 31G7 antibody is extremely specific for EGFr and does not react with the highly homologous c-erbB-2 (HER2) protein. Invitrogen now offers the Zymed 31G7 antibody clone as part of a convenient, standardized immunohistochemical kit for the detection of EGFr protein expression in normal and neoplastic tissue. Invitrogen's Zymed EGFr Kit is compatible with manual or automated immunostainers and offers the greatest flexibility with FFPE tissue samples. For more information, visit www.invitrogen.com/antibodies. Note: sponsors do NOT have access in any manner to email addresses or other personal information in the possession of PathologyOutlines.com.
Visit and follow our Blog to see recent updates to the website.
Case #12
Clinical history:
A 22 year old woman had a large right ovarian mass, which was excised.
Micro images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Dysgerminoma of the ovary
Immunohistochemistry images:
Immunohistochemistry:
The immunohistochemistry was interpreted as PLAP positive, AFP negative, KIT positive.
Discussion:
Dysgerminoma of the ovary is an uncommon tumor, representing < 1% of ovarian malignancies. They usually affect young patients, with 80% under age 30 years. 15% have bilateral tumors. ~5% are associated with gonadal dysgenesis, androgen insensitivity or pseudohermaphroditism. Some cases appear to represent progression from gonadoblastomas (Virchows Arch 2005;447:603). Patients with dysgerminomas typically present with low stage and have a 95% survival. Metastases can occur to the opposite ovary, retroperitoneal lymph nodes or the peritoneal cavity but often don't affect survival. Dysgerminomas are typically treated with surgery and chemotherapy and not radiotherapy, which may impair fertility in these usually young patients (NIH: Ovarian Germ Cell Tumors Treatment [Accessed 12 October 2023]). Dysgerminomas may rarely transform to a yolk sac tumor and may be mixed with other germ cell tumors, such as choriocarcinoma, yolk sac tumor or embryonal carcinoma, which worsens the prognosis (Mod Pathol 1995;8:881). Thus, it is important to adequately section these tumors and search for different looking areas of the tumor.
Dysgerminomas are grossly solid and nodular tumors of variable size. They are gray-pink, resembling cerebral cortex and commonly have hemorrhage and necrosis. Microscopically, they are composed of tumor cells separated by fibrous stroma with T lymphocytes. The tumor cells are large with well defined cell borders. The cytoplasm contains glycogen and the nuclei are central, vesicular and contain one or more prominent nucleoli. Granulomas may be present.
The differential diagnosis includes yolk sac tumor, undifferentiated carcinoma, clear cell adenocarcinoma (usually in postmenopausal women, PLAP negative), lymphoma, melanoma, granulosa cell tumor and metastatic breast carcinoma. Careful review of the histology of multiple sections, special stains and clinical history are helpful in distinguishing these other tumors. Dysgerminomas are immunoreactive for PLAP, KIT and vimentin. They may be focally positive for hCG in giant cells and focally positive for cytokeratin. They are negative for AFP. Recent reports indicate that OCT4, a transcription factor involved in the regulation of pluripotency during embryonic development, is sensitive and relatively specific for dysgerminomas (Am J Surg Pathol 2004;28:1341).