9 September 2005 - Case #19
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Professor D. Y. Cohen, Department of Pathology, Herzliyah Medical Center, Israel.

Case #19
Clinical history:
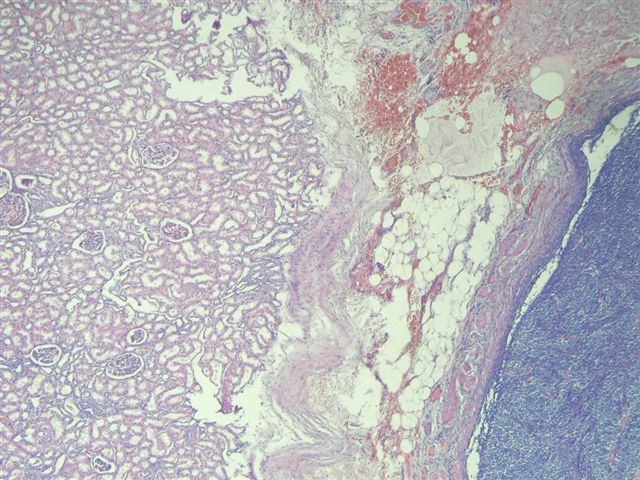
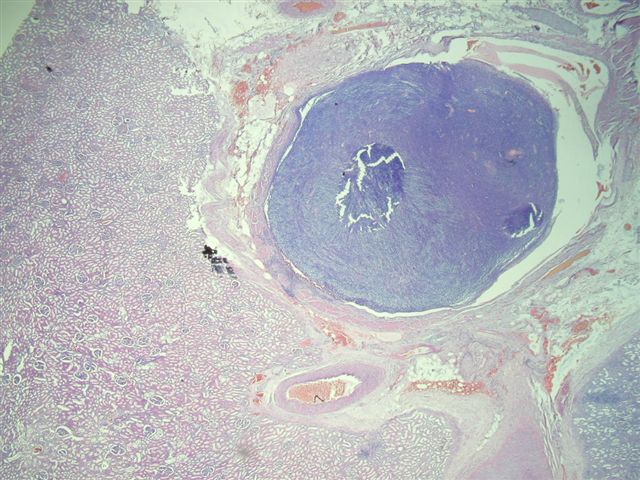
A 40 year old woman had a radical nephrectomy for a large renal mass. The kidney weighed 488 grams after removal of perinephric adipose tissue. The upper portion of the kidney contained a 10 x 9 x 9 cm mass of gray-white solid tissue with central cystic and mucoid degeneration. No golden yellow or hemorrhagic areas were noted. Focally, the tumor formed nodules abutting onto the renal pelvis, 0.5 cm from the renal hilum. The adrenal gland was grossly normal.
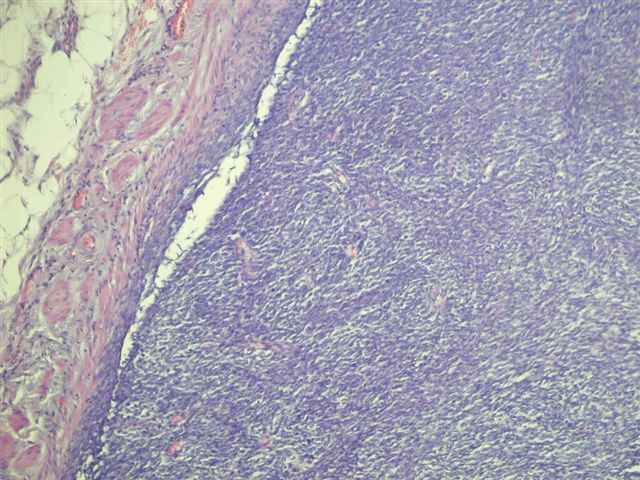
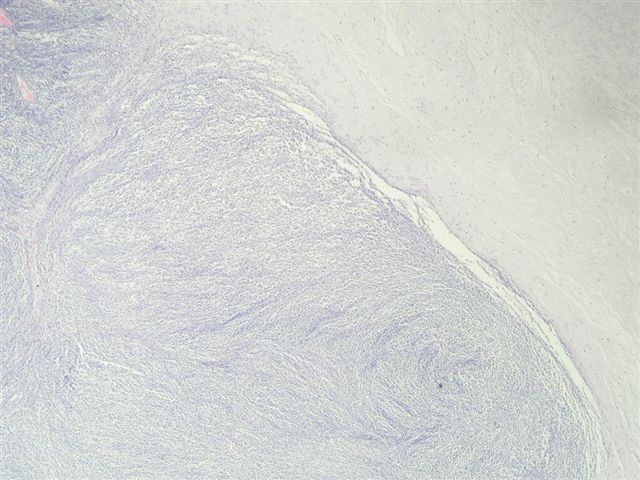
Additional sections showed mitotically active cells but no neoplastic glandular tissue. No bone or cartilagenous foci were present. The tumor extended into the renal pelvis and within large venous channels. It was adherent to but did not infiltrate into the renal capsule.
Immunohistochemistry description:
The tumor was immunoreactive for vimentin, CD99 (O - 13) and Ki67 (15 - 20% of cells). The tumor was negative for lymphocyte markers CD45, CD20 and CD3; keratins CK7, CK20 and pankeratin MNF118; neuroendocrine markers NSE, chromogranin A and synaptophysin. It was also negative for desmin, smooth muscle actin, CD10 and KIT / CD117. Cytogenetics or molecular studies were not available.
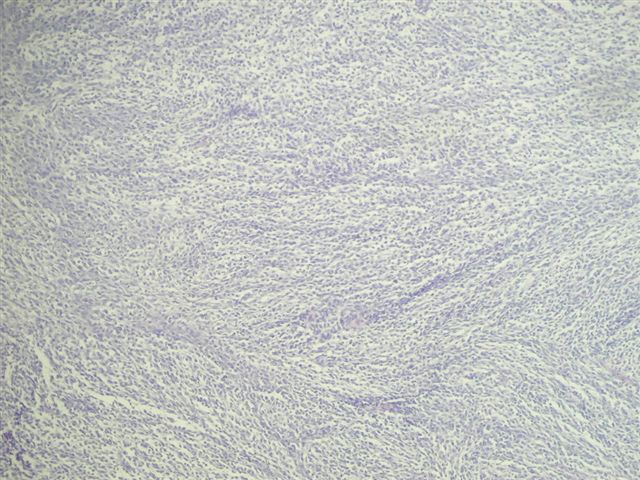
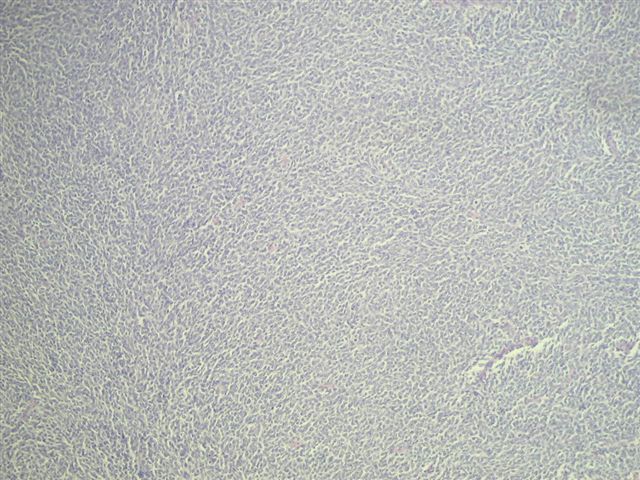
Microscopic images:
What is your diagnosis?
Diagnosis: Monophasic synovial sarcoma of the kidney
Discussion:
Synovial sarcomas are typically found in the extremities of young adults, with less than 30 cases reported in the kidney since 1999. In the kidney, the median patient age is 35 years, range of 20 - 59 years, with no gender preference. They are usually large, partially necrotic masses, with grossly noted cysts in 70%. Histologically, they are usually highly cellular and monomorphic, composed of short intersecting fascicles of plump spindle cells. The tumor cells have indistinct cell borders, minimal cytoplasm, ovoid nuclei and inconspicuous nucleoli. They infiltrate around native, nonneoplastic renal tubules that undergo secondary dilatation, which may simulate a biphasic pattern. They often have a hemangiopericytoma-like vascular pattern with staghorn vessels. Cystic spaces are lined by hobnail type cells with eosinophilic cytoplasm and apically oriented nuclei. Renal synovial sarcomas may rarely exhibit rhabdoid features, be biphasic (with epithelial cells) or have small cell or high grade spindle cell features (Am J Surg Pathol 2004;28:634). Immunostains are helpful in excluding other spindle cell tumors. Synovial sarcomas are immunoreactive for vimentin and CD56, with variable staining for CD99, BCL2 and EMA. They are typically negative for keratins, S100, CD34, smooth muscle actin and desmin. Over 90% of cases demonstrate t(X;18)(p11.2;q11.2), which produces the SYT::SSX2 (also SSX1 or rarely SSX4) transcript that is specific for synovial sarcoma (figure 4-karyotype #1, #2 (tumor of arm), Arch Pathol Lab Med 2005;129:238). These tumors appear to have aggressive behavior.
The histologic differential diagnosis includes other spindle cell tumors of the kidney, all of which are negative for t(X;18), although some synovial sarcomas are also negative for this translocation. Of particular concern is the relatively common sarcomatoid renal cell carcinoma. It typically affects older patients, with a mean age of 60 years. Its malignant epithelial component may be focal, so adequate sampling is important. The epithelial component is keratin+ and EMA+ and the sarcomatoid component is often EMA+ and S100+. Another histologic mimic is cellular mesonephric nephroma, although almost all of these patients are newborns (up to age 1 year) and tumor cells have more cytoplasm and are desmin+. The differential also includes two CD34+ tumors: hemangiopericytoma (less cellular pleomorphism and no / rare mitotic activity) and solitary fibrous tumor. Blastemal variants of Wilms tumor are spindled but often have serpentine or nodular patterns and are immunoreactive for WT1, in contrast to synovial sarcomas, which are WT1 negative. Finally, Ewing / PNET may appear similar, although they usually have primitive round cells with variable rosette formation, instead of short fascicles of spindled cells and have a characteristic t(11;22)(q24;q12) translocation.
References: Am J Surg Pathol 2000;24:1087, Am J Surg Pathol 2000;24:1097, Murphy: Tumors of the Kidney, Bladder and Related Urinary Structures, 4th Edition, 2004
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Professor D. Y. Cohen, Department of Pathology, Herzliyah Medical Center, Israel.

Website news:
(1) This week's case is sponsored by Invitrogen. Invitrogen offers Zymed total system solution for pathology reagents and automation. From antibodies, kits and probes for IHC and CISH to immunostainers for automation, you can be confident that Zymed products will always deliver high quality staining results and offer the cutting edge pathology solutions you need. (Note: sponsors do NOT have access to email addresses or other personal information in the possession of PathologyOutlines.com.)
Visit and follow our Blog to see recent updates to the website.
(1) This week's case is sponsored by Invitrogen. Invitrogen offers Zymed total system solution for pathology reagents and automation. From antibodies, kits and probes for IHC and CISH to immunostainers for automation, you can be confident that Zymed products will always deliver high quality staining results and offer the cutting edge pathology solutions you need. (Note: sponsors do NOT have access to email addresses or other personal information in the possession of PathologyOutlines.com.)
Visit and follow our Blog to see recent updates to the website.
Case #19
Clinical history:
A 40 year old woman had a radical nephrectomy for a large renal mass. The kidney weighed 488 grams after removal of perinephric adipose tissue. The upper portion of the kidney contained a 10 x 9 x 9 cm mass of gray-white solid tissue with central cystic and mucoid degeneration. No golden yellow or hemorrhagic areas were noted. Focally, the tumor formed nodules abutting onto the renal pelvis, 0.5 cm from the renal hilum. The adrenal gland was grossly normal.
Additional sections showed mitotically active cells but no neoplastic glandular tissue. No bone or cartilagenous foci were present. The tumor extended into the renal pelvis and within large venous channels. It was adherent to but did not infiltrate into the renal capsule.
Immunohistochemistry description:
The tumor was immunoreactive for vimentin, CD99 (O - 13) and Ki67 (15 - 20% of cells). The tumor was negative for lymphocyte markers CD45, CD20 and CD3; keratins CK7, CK20 and pankeratin MNF118; neuroendocrine markers NSE, chromogranin A and synaptophysin. It was also negative for desmin, smooth muscle actin, CD10 and KIT / CD117. Cytogenetics or molecular studies were not available.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Monophasic synovial sarcoma of the kidney
Discussion:
Synovial sarcomas are typically found in the extremities of young adults, with less than 30 cases reported in the kidney since 1999. In the kidney, the median patient age is 35 years, range of 20 - 59 years, with no gender preference. They are usually large, partially necrotic masses, with grossly noted cysts in 70%. Histologically, they are usually highly cellular and monomorphic, composed of short intersecting fascicles of plump spindle cells. The tumor cells have indistinct cell borders, minimal cytoplasm, ovoid nuclei and inconspicuous nucleoli. They infiltrate around native, nonneoplastic renal tubules that undergo secondary dilatation, which may simulate a biphasic pattern. They often have a hemangiopericytoma-like vascular pattern with staghorn vessels. Cystic spaces are lined by hobnail type cells with eosinophilic cytoplasm and apically oriented nuclei. Renal synovial sarcomas may rarely exhibit rhabdoid features, be biphasic (with epithelial cells) or have small cell or high grade spindle cell features (Am J Surg Pathol 2004;28:634). Immunostains are helpful in excluding other spindle cell tumors. Synovial sarcomas are immunoreactive for vimentin and CD56, with variable staining for CD99, BCL2 and EMA. They are typically negative for keratins, S100, CD34, smooth muscle actin and desmin. Over 90% of cases demonstrate t(X;18)(p11.2;q11.2), which produces the SYT::SSX2 (also SSX1 or rarely SSX4) transcript that is specific for synovial sarcoma (figure 4-karyotype #1, #2 (tumor of arm), Arch Pathol Lab Med 2005;129:238). These tumors appear to have aggressive behavior.
The histologic differential diagnosis includes other spindle cell tumors of the kidney, all of which are negative for t(X;18), although some synovial sarcomas are also negative for this translocation. Of particular concern is the relatively common sarcomatoid renal cell carcinoma. It typically affects older patients, with a mean age of 60 years. Its malignant epithelial component may be focal, so adequate sampling is important. The epithelial component is keratin+ and EMA+ and the sarcomatoid component is often EMA+ and S100+. Another histologic mimic is cellular mesonephric nephroma, although almost all of these patients are newborns (up to age 1 year) and tumor cells have more cytoplasm and are desmin+. The differential also includes two CD34+ tumors: hemangiopericytoma (less cellular pleomorphism and no / rare mitotic activity) and solitary fibrous tumor. Blastemal variants of Wilms tumor are spindled but often have serpentine or nodular patterns and are immunoreactive for WT1, in contrast to synovial sarcomas, which are WT1 negative. Finally, Ewing / PNET may appear similar, although they usually have primitive round cells with variable rosette formation, instead of short fascicles of spindled cells and have a characteristic t(11;22)(q24;q12) translocation.
References: Am J Surg Pathol 2000;24:1087, Am J Surg Pathol 2000;24:1097, Murphy: Tumors of the Kidney, Bladder and Related Urinary Structures, 4th Edition, 2004