18 January 2006 - Case #34
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Juan Jose Segura Fonseca, Departamento de Patologia, Hospital San Juan de Dios, San Jose, Costa Rica.
Case #34
Clinical history:
A 24 year old White man presented to the outpatient clinic complaining of a slow growing, painless soft tissue mass over the right inguinal area for 8 months. The skin over the mass was tense, and over the past 2 months, a small ulcerated area discharged yellow-white chalky fluid and sometimes small, white, solid granules (Figure 1). A fine needle aspiration was performed and white chalky material was aspirated. A pelvic Xray showed small calcified nodules and a large, dense periarticular calcified mass in the soft tissue around the hip joint (Figure 2). The soft tissue mass was partially resected.
Gross description:
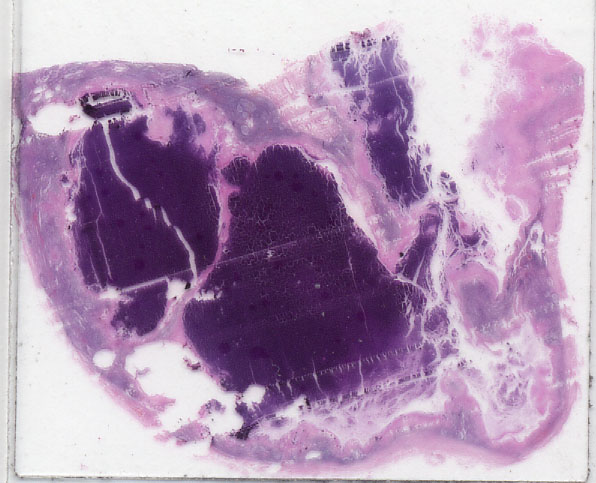
The tissue grossly was composed of white, granular, calcified chalky material surrounded by a fibrous tissue capsule (Figure 3).
Clinical, radiology and gross images:
Microscopic images:
What is your diagnosis?
Diagnosis: Tumoral calcinosis
Discussion:
Tumoral calcinosis was described by Giard in 1888, Duret in 1889 and named by Inclan in 1943 (OMIM: Tumoral Calcinosis, Hyperphosphatemic, Familial, 1; HFTC1 [Accessed 8 December 2023]). Its main feature is large, subcutaneous calcified masses in teenagers and young adults that are usually asymptomatic and slow growing. The masses are always near a large joint, commonly the hip, shoulder or posterior elbow. A few cases have been reported near the hands and feet but the knee joint is always spared. Intraosseous deposits are rare.
Occasionally, there is ulceration of the overlying skin with discharge of chalky material. The deposits contain amorphous calcium phosphate and calcium carbonate with associated hydroxyapatite crystals (Clin Imaging 2003;27:184). The differential diagnosis includes dystrophic calcification, which is associated with necrosis.
Tumor calcinosis has its onset during the first and second decades of life and is rare after age 50 years. It is more common in Black people, and males and females are equally affected. It is usually inherited as an autosomal dominant trait with variable clinical expression. Mutations have been recently described in familial cases (J Clin Endocrinol Metab 2005;90:2424, J Clin Endocrinol Metab 2005;90:5523, Hum Genet 2005;118:261). Typically there is a mild elevation of serum phosphate and vitamin D and normal serum calcium, alkaline phosphatase and uric acid levels (J Clin Endocrinol Metab 1985;60:1093).
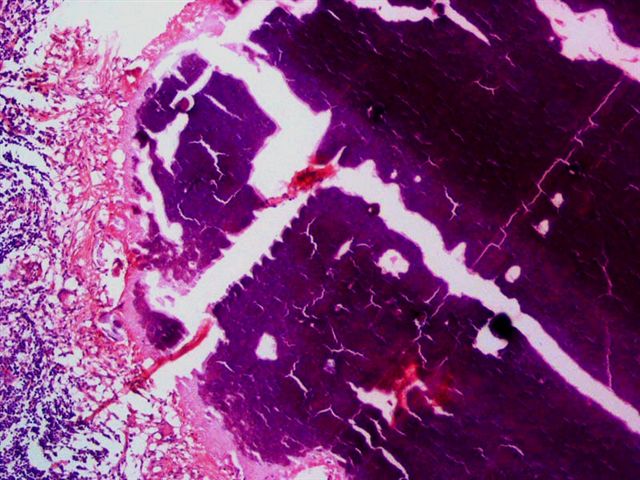
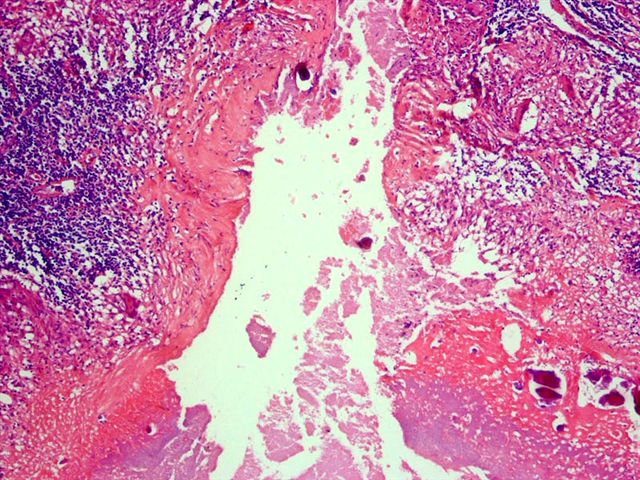
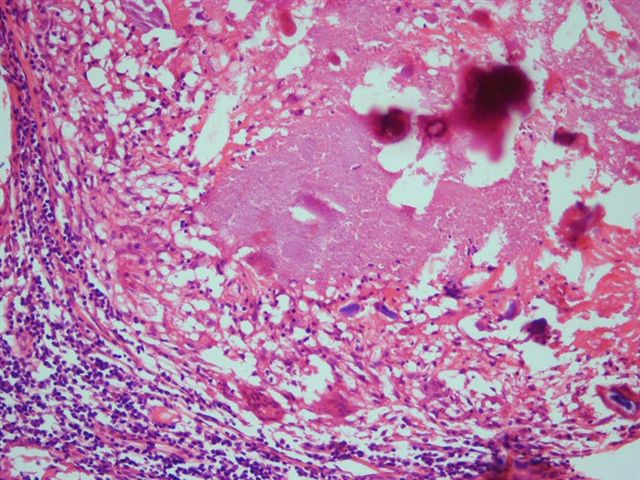
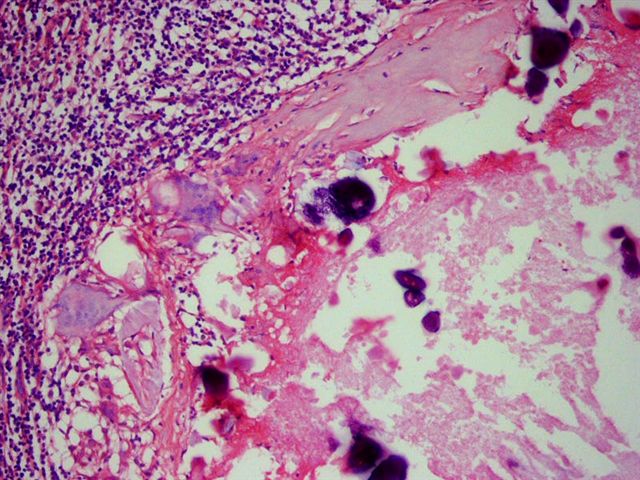
Microscopically, an active cellular phase is characterized by a central mass of amorphous or granular calcified material surrounded by hyalinized fibrous tissue separating several cavities. The fibrous tissue is bordered by a granulomatous and chronic inflammatory infiltrate. There may be prominent small psammoma-like bodies or calcospherites (Histopathology 1997;31:18).
Treatment is complete surgical excision, due to a high recurrence rate. Fine needle aspiration may be helpful in diagnosis (Diagn Cytopathol 1995;13:339).
Reference: Am J Surg Pathol 1993;17:788
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Juan Jose Segura Fonseca, Departamento de Patologia, Hospital San Juan de Dios, San Jose, Costa Rica.
Website news:
(1) This week's case is sponsored by Nature Publishing Group (NPG). The United States and Canadian Academy of Pathology (USCAP) and Nature Publishing Group publish 2 major scientific pathology journals as part of their educational mission - Modern Pathology and Laboratory Investigation - which are among the top journals in the field. Both journals publish innovate studies of etiology and pathogenesis along with cutting edge diagnostic, screening and pragmatic studies and technological breakthroughs.
Need a job? Visit www.nature.com/naturecareers - the career service for Laboratory Investigation and Modern Pathology.
Visit and follow our Blog to see recent updates to the website.
(1) This week's case is sponsored by Nature Publishing Group (NPG). The United States and Canadian Academy of Pathology (USCAP) and Nature Publishing Group publish 2 major scientific pathology journals as part of their educational mission - Modern Pathology and Laboratory Investigation - which are among the top journals in the field. Both journals publish innovate studies of etiology and pathogenesis along with cutting edge diagnostic, screening and pragmatic studies and technological breakthroughs.
Need a job? Visit www.nature.com/naturecareers - the career service for Laboratory Investigation and Modern Pathology.
Visit and follow our Blog to see recent updates to the website.
Case #34
Clinical history:
A 24 year old White man presented to the outpatient clinic complaining of a slow growing, painless soft tissue mass over the right inguinal area for 8 months. The skin over the mass was tense, and over the past 2 months, a small ulcerated area discharged yellow-white chalky fluid and sometimes small, white, solid granules (Figure 1). A fine needle aspiration was performed and white chalky material was aspirated. A pelvic Xray showed small calcified nodules and a large, dense periarticular calcified mass in the soft tissue around the hip joint (Figure 2). The soft tissue mass was partially resected.
Gross description:
The tissue grossly was composed of white, granular, calcified chalky material surrounded by a fibrous tissue capsule (Figure 3).
Clinical, radiology and gross images:
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Tumoral calcinosis
Discussion:
Tumoral calcinosis was described by Giard in 1888, Duret in 1889 and named by Inclan in 1943 (OMIM: Tumoral Calcinosis, Hyperphosphatemic, Familial, 1; HFTC1 [Accessed 8 December 2023]). Its main feature is large, subcutaneous calcified masses in teenagers and young adults that are usually asymptomatic and slow growing. The masses are always near a large joint, commonly the hip, shoulder or posterior elbow. A few cases have been reported near the hands and feet but the knee joint is always spared. Intraosseous deposits are rare.
Occasionally, there is ulceration of the overlying skin with discharge of chalky material. The deposits contain amorphous calcium phosphate and calcium carbonate with associated hydroxyapatite crystals (Clin Imaging 2003;27:184). The differential diagnosis includes dystrophic calcification, which is associated with necrosis.
Tumor calcinosis has its onset during the first and second decades of life and is rare after age 50 years. It is more common in Black people, and males and females are equally affected. It is usually inherited as an autosomal dominant trait with variable clinical expression. Mutations have been recently described in familial cases (J Clin Endocrinol Metab 2005;90:2424, J Clin Endocrinol Metab 2005;90:5523, Hum Genet 2005;118:261). Typically there is a mild elevation of serum phosphate and vitamin D and normal serum calcium, alkaline phosphatase and uric acid levels (J Clin Endocrinol Metab 1985;60:1093).
Microscopically, an active cellular phase is characterized by a central mass of amorphous or granular calcified material surrounded by hyalinized fibrous tissue separating several cavities. The fibrous tissue is bordered by a granulomatous and chronic inflammatory infiltrate. There may be prominent small psammoma-like bodies or calcospherites (Histopathology 1997;31:18).
Treatment is complete surgical excision, due to a high recurrence rate. Fine needle aspiration may be helpful in diagnosis (Diagn Cytopathol 1995;13:339).
Reference: Am J Surg Pathol 1993;17:788