1 February 2006 - Case #36
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Adrian A. Suarez, National Childrens Hospital, San Jose, Costa Rica.
Case #36
Clinical history:
The patient was a 7 year old girl with a 3 month history of a mass in the right side of her chest. On physical examination the lesion was mildly tender and measured about 3 cm. A CT scan showed a large tumor involving soft tissues and extending from the subcutaneous fat into the anterior mediastinum (image). As is usual in our institution, a fine needle aspiration biopsy was performed.
Fine needle aspiration biopsy:
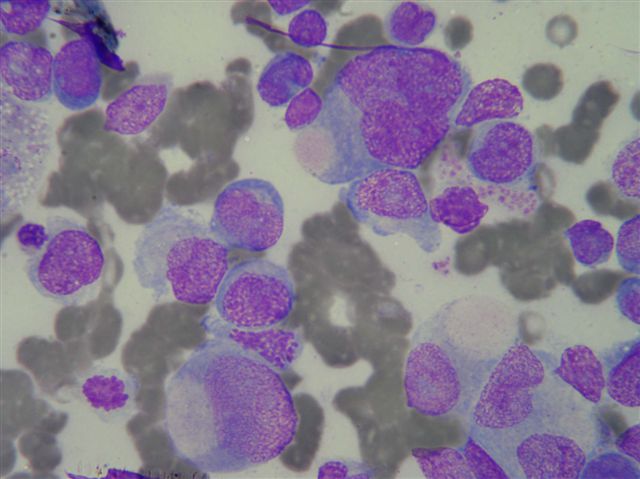
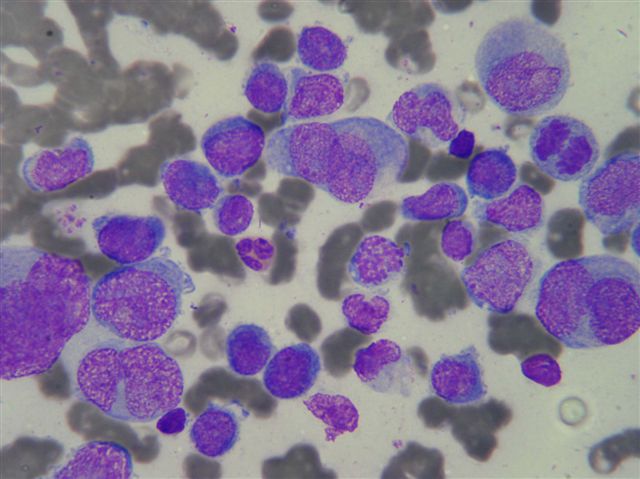
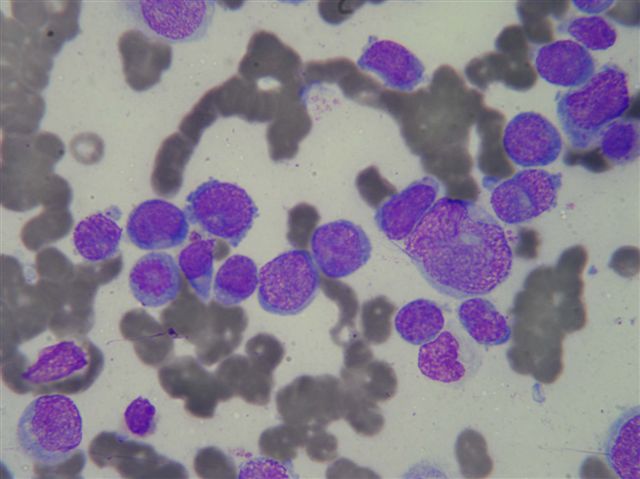
Air dried smears, stained with May-Grünwald-Giemsa, were highly cellular. Cells were noncohesive and ranged from small to very large (FNA image #1, image #2, image #3). Nuclei were pleomorphic, including many multilobulated or convoluted forms and some were doughnut or wreath shaped. The cells had variable amounts of blue cytoplasm and many of the larger ones showed eccentric clear pink areas. There were frequent mitotic figures. Lymphoglandular bodies were scarce.
Immunocytochemistry description:
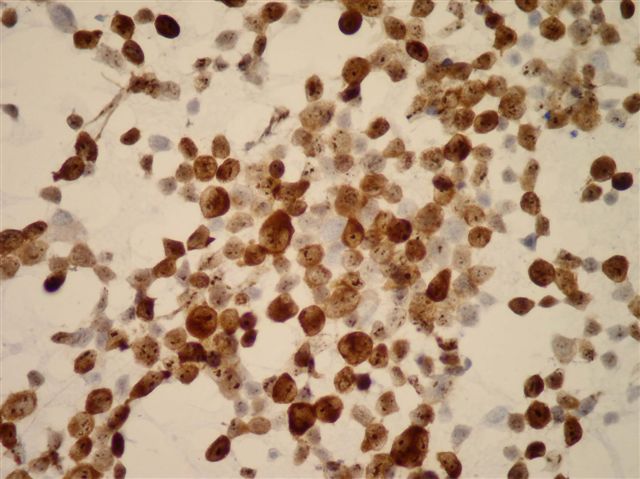
Immunocytochemistry, performed on alcohol fixed material, demonstrated strong nuclear and cytoplasmic reactivity for ALK1 (image), membrane reactivity for CD45 and weak cytoplasmic reactivity for CD30.
Flow cytometry description:
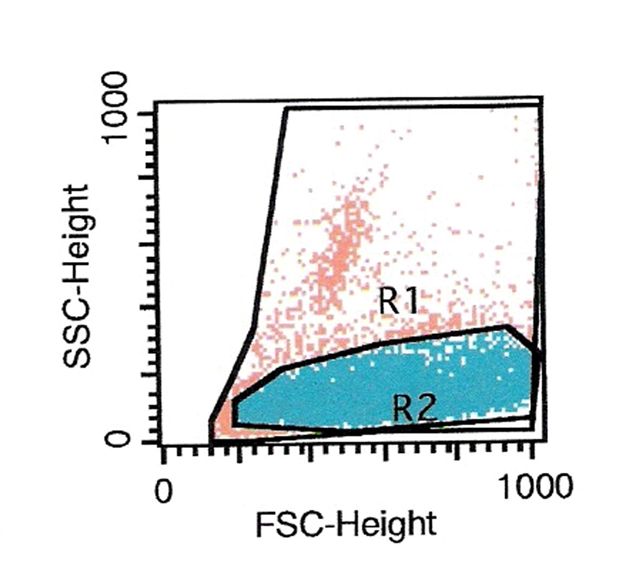
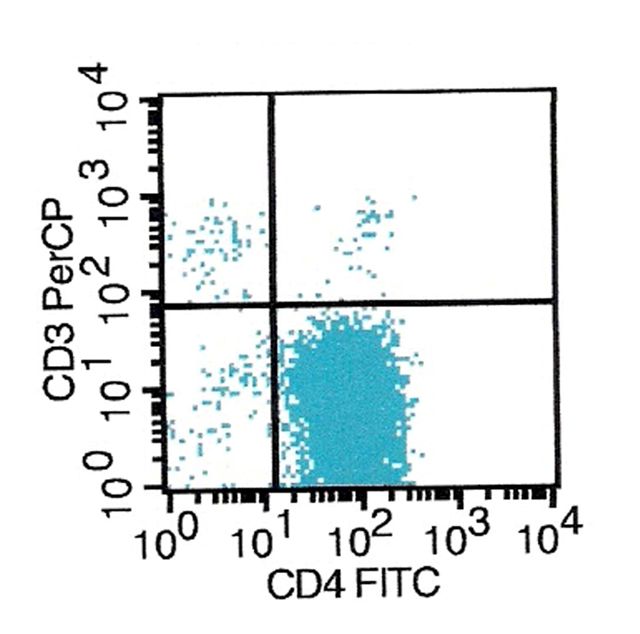
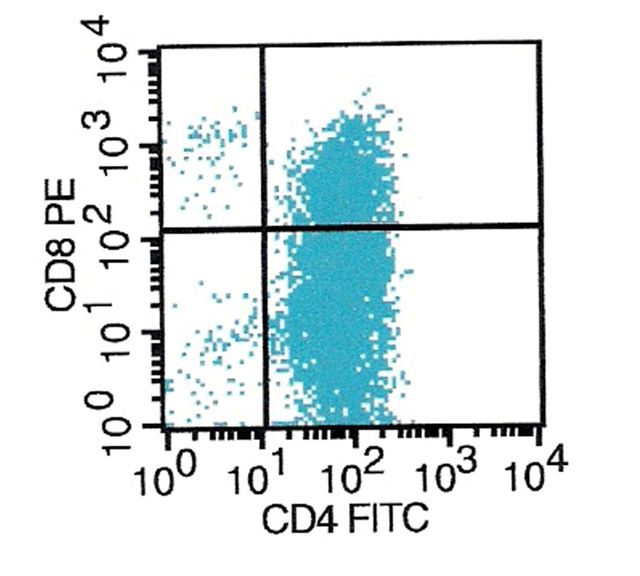
Flow cytometric analysis, performed in a saline cell suspension, showed a neoplastic lymphoid population with partial CD4 and CD8 coexpression (flow cytometry - forward scatter versus side scatter, CD4 versus CD3, CD4 versus CD8). No expression of CD3 was detected.
Radiology images:
Cytology images:
Flow cytometry images:
What is your diagnosis?
Diagnosis: Anaplastic large cell lymphoma
Immunocytochemistry image:
Discussion:
Anaplastic large cell lymphoma (ALCL) causes 10 - 15% of childhood non-Hodgkin lymphomas versus 3% in adults. T cell origin and T cell lineage can usually be proven by molecular studies, even if no T cell antigen expression is present by immunohistochemistry. Nodal involvement is common.
In lymph nodes, there is infiltration of interfollicular T cell zones and nodal sinuses. Tumor cells are anaplastic and large, and may resemble Reed-Sternberg cells, with abundant cytoplasm and either horseshoe, wreath-like or multiple nuclei. Tumor cells also have multiple nucleoli and a perinuclear eosinophilic region. There is brisk mitotic activity, and frequent vascular wall invasion, particularly in extranodal cases.
Fine needle aspiration cytology smears show dissociated cells with abundant, lightly basophilic, vacuolated cytoplasm; oval, round or lobulated nuclei; and binucleate, trinucleate and multinucleate cells with a wreath-like arrangement of nuclei and prominent nucleoli (Acta Cytol 1997;41:1253, Acta Cytol 1996;40:779, Diagn Cytopathol 1996;14:155).
Immunohistochemistry is necessary to confirm the diagnosis of anaplastic large cell lymphoma. Tumor cells have characteristic surface membrane and cytoplasmic paranuclear dot-like staining for CD30. They are also often immunoreactive for CD2, CD4 and CD25, with variable staining for CD43 and EMA and occasional staining for B cell markers.
Anaplastic large cell lymphoma is associated with t(2;5)(p23;q35), with a translocation of the anaplastic lymphoma kinase gene (producing the ALK or ALK1 protein) on chromosome #2 and the nucleophosmin gene on chromosome #5 (FISH for NPM::ALK fusion product; translocation diagram). The ALK rearrangement can be detected by fluorescence in situ hybridization (FISH) or by ALK immunohistochemical staining. In a recent study of children, FISH identified a translocation in 83% of cases and ALK immunostaining was present in 97% of cases (Br J Haematol 2005;131:624).
The differential diagnosis includes various carcinomas (usually keratin positive), Hodgkin lymphoma (has few neoplastic cells, usually CD15+, PAX5 / BSAP+, ALK-, EMA-), anaplastic variant of diffuse large cell lymphoma (PAX5 / BSAP+, usually CD20+, CD79a+), lymphomatoid granulomatosis (angiocentric, with a background of reactive lymphocytes and histiocytes, EBV+) and nonneoplastic disorders with atypical CD30+ cells.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Adrian A. Suarez, National Childrens Hospital, San Jose, Costa Rica.
Website news:
(1) Be sure to visit our Books page when deciding what books to buy. We list over 900 pathology related books by topic (dermatopathology, hematopathology, etc.) and by author, and also list all the WHO and AFIP books separately. Purchases made through Amazon.com from these pages support our free website, without costing you anything.
Visit and follow our Blog to see recent updates to the website.
(1) Be sure to visit our Books page when deciding what books to buy. We list over 900 pathology related books by topic (dermatopathology, hematopathology, etc.) and by author, and also list all the WHO and AFIP books separately. Purchases made through Amazon.com from these pages support our free website, without costing you anything.
Visit and follow our Blog to see recent updates to the website.
Case #36
Clinical history:
The patient was a 7 year old girl with a 3 month history of a mass in the right side of her chest. On physical examination the lesion was mildly tender and measured about 3 cm. A CT scan showed a large tumor involving soft tissues and extending from the subcutaneous fat into the anterior mediastinum (image). As is usual in our institution, a fine needle aspiration biopsy was performed.
Fine needle aspiration biopsy:
Air dried smears, stained with May-Grünwald-Giemsa, were highly cellular. Cells were noncohesive and ranged from small to very large (FNA image #1, image #2, image #3). Nuclei were pleomorphic, including many multilobulated or convoluted forms and some were doughnut or wreath shaped. The cells had variable amounts of blue cytoplasm and many of the larger ones showed eccentric clear pink areas. There were frequent mitotic figures. Lymphoglandular bodies were scarce.
Immunocytochemistry description:
Immunocytochemistry, performed on alcohol fixed material, demonstrated strong nuclear and cytoplasmic reactivity for ALK1 (image), membrane reactivity for CD45 and weak cytoplasmic reactivity for CD30.
Flow cytometry description:
Flow cytometric analysis, performed in a saline cell suspension, showed a neoplastic lymphoid population with partial CD4 and CD8 coexpression (flow cytometry - forward scatter versus side scatter, CD4 versus CD3, CD4 versus CD8). No expression of CD3 was detected.
Radiology images:
Cytology images:
Flow cytometry images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Anaplastic large cell lymphoma
Immunocytochemistry image:
Discussion:
Anaplastic large cell lymphoma (ALCL) causes 10 - 15% of childhood non-Hodgkin lymphomas versus 3% in adults. T cell origin and T cell lineage can usually be proven by molecular studies, even if no T cell antigen expression is present by immunohistochemistry. Nodal involvement is common.
In lymph nodes, there is infiltration of interfollicular T cell zones and nodal sinuses. Tumor cells are anaplastic and large, and may resemble Reed-Sternberg cells, with abundant cytoplasm and either horseshoe, wreath-like or multiple nuclei. Tumor cells also have multiple nucleoli and a perinuclear eosinophilic region. There is brisk mitotic activity, and frequent vascular wall invasion, particularly in extranodal cases.
Fine needle aspiration cytology smears show dissociated cells with abundant, lightly basophilic, vacuolated cytoplasm; oval, round or lobulated nuclei; and binucleate, trinucleate and multinucleate cells with a wreath-like arrangement of nuclei and prominent nucleoli (Acta Cytol 1997;41:1253, Acta Cytol 1996;40:779, Diagn Cytopathol 1996;14:155).
Immunohistochemistry is necessary to confirm the diagnosis of anaplastic large cell lymphoma. Tumor cells have characteristic surface membrane and cytoplasmic paranuclear dot-like staining for CD30. They are also often immunoreactive for CD2, CD4 and CD25, with variable staining for CD43 and EMA and occasional staining for B cell markers.
Anaplastic large cell lymphoma is associated with t(2;5)(p23;q35), with a translocation of the anaplastic lymphoma kinase gene (producing the ALK or ALK1 protein) on chromosome #2 and the nucleophosmin gene on chromosome #5 (FISH for NPM::ALK fusion product; translocation diagram). The ALK rearrangement can be detected by fluorescence in situ hybridization (FISH) or by ALK immunohistochemical staining. In a recent study of children, FISH identified a translocation in 83% of cases and ALK immunostaining was present in 97% of cases (Br J Haematol 2005;131:624).
The differential diagnosis includes various carcinomas (usually keratin positive), Hodgkin lymphoma (has few neoplastic cells, usually CD15+, PAX5 / BSAP+, ALK-, EMA-), anaplastic variant of diffuse large cell lymphoma (PAX5 / BSAP+, usually CD20+, CD79a+), lymphomatoid granulomatosis (angiocentric, with a background of reactive lymphocytes and histiocytes, EBV+) and nonneoplastic disorders with atypical CD30+ cells.