3 May 2006 - Case #44
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Misty Jacobs, Medical University of Ohio, Toledo, Ohio, USA.
Case #44
Clinical history:
A 20 year old woman complained of right sided abdominal pain and right shoulder pain for 5 days after delivery of her first child. A CT scan showed a lesion near the dome of the liver. Several biopsies were obtained.
A trichrome stain confirmed the presence of fibrosis within the portal tracts. An iron stain showed no evidence of increased iron stores.
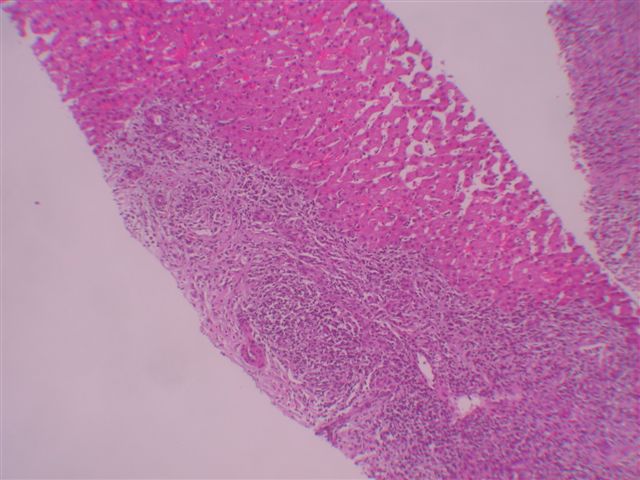
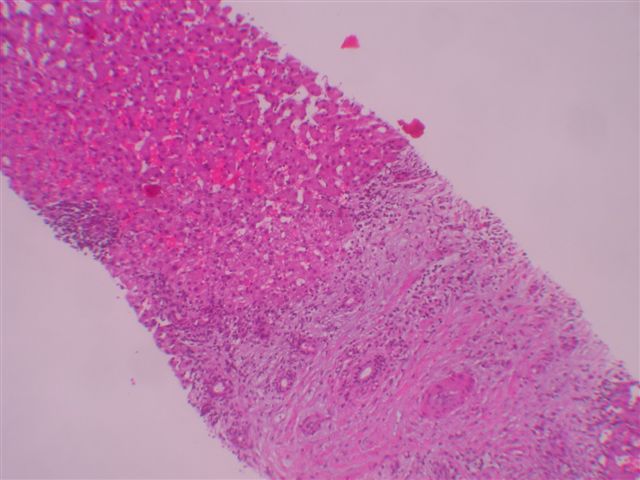
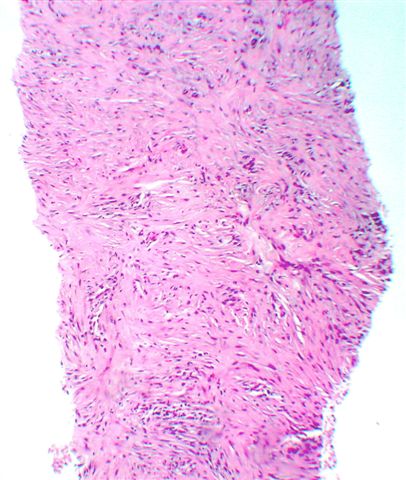
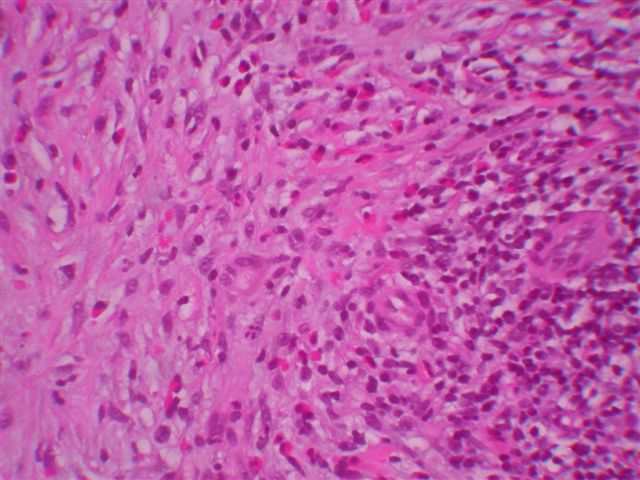
Microscopic images:
What is your diagnosis?
Diagnosis: Inflammatory pseudotumor of the liver
Discussion:
Inflammatory pseudotumor is also called inflammatory myofibroblastic tumor. The diagnosis includes both reactive and neoplastic conditions. Although common in the lung, it is rare in the liver. The mean patient age is 37 years but all ages are affected. 75% of patients are male.
Presenting symptoms include fever and upper abdominal pain. Tumors involving the hepatic hilum may cause portal hypertension and biliary obstruction, rarely requiring liver transplantation (Pediatr Transplant 2004;8:517). Other associated conditions are occlusive phlebitis and chronic cholangitis (Hum Pathol 1994;25:86). Uncommon associations are with Crohn's disease and posthematopoietic stem cell transplantation (J Clin Gastroenterol 2004;38:818, Bone Marrow Transplant 2004;33:103). Surgery is curative, although the tumors occasionally regress spontaneously.
Grossly, the tumors are usually well circumscribed and 70% are solitary. Tumors may extend into the inferior vena cava or retroperitoneal soft tissue. They have a variegated cut surface, often with hemorrhage and necrosis.
Microscopically, the tumors consist of a mixture of inflammatory cells, particularly polyclonal plasma cells, lymphocytes, eosinophils and macrophages. Neutrophils may also be present. There are also variable amounts of plump spindled cells resembling myofibroblasts and mature fibroblasts. The stroma is often whorled, resembling leiomyoma or fibrotic resembling sclerosing hemangioma. Mitotic activity is rare.
The spindled cells are immunoreactive for vimentin, smooth muscle actin and muscle specific actin in 80% of cases. There is variable immunoreactivity for desmin and pankeratin stains. These tumors are negative for S100, CD21 and CD35. A small percentage are ALK+, which is associated with a favorable prognosis at all sites combined (Am J Surg Pathol 2001;25:761).
The differential diagnosis is large. First, if the excision is subtotal, the diagnosis must be considered tentative, as other neoplasms may have a similar inflammatory component. Second, dendritic cell tumors must be excluded. They usually occur in women, often have systemic symptoms and are immunoreactive for follicular dendritic cell markers CD21 and CD35. The inflammatory tumor-like variant is usually associated with Epstein-Barr virus infection (Am J Surg Pathol 2001;25:721). Third, infectious disorders, such as TB, syphilis or bacterial abscess may cause an inflammatory infiltrate and antibiotics or NSAIDS may cause tumor regression (Acta Gastroenterol Belg 2005;68:382, Scand J Gastroenterol 2005;40:875, J Clin Pathol 2003;56:868). Fourth, inflammatory disorders such as sarcoidosis, malakoplakia, abscess and cholangiohepatitis should be considered. Finally, tumors to consider include sclerosing hemangioma, leiomyoma, solitary fibrous tumor, sarcomatoid carcinoma, nerve sheath tumors, Hodgkin lymphoma and MFH. Postoperative spindle cell nodule is similar morphologically but has a different clinical history.
A recent study suggests that cases associated with sclerosing cholangitis may represent an IgG4 related biliary disease that is part of the spectrum of sclerosing pancreatitis and is responsive to steroids (Am J Surg Pathol 2004;28:1193).
References: Am J Surg Pathol 1993;17:231
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Misty Jacobs, Medical University of Ohio, Toledo, Ohio, USA.
Case #44
Clinical history:
A 20 year old woman complained of right sided abdominal pain and right shoulder pain for 5 days after delivery of her first child. A CT scan showed a lesion near the dome of the liver. Several biopsies were obtained.
A trichrome stain confirmed the presence of fibrosis within the portal tracts. An iron stain showed no evidence of increased iron stores.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Inflammatory pseudotumor of the liver
Discussion:
Inflammatory pseudotumor is also called inflammatory myofibroblastic tumor. The diagnosis includes both reactive and neoplastic conditions. Although common in the lung, it is rare in the liver. The mean patient age is 37 years but all ages are affected. 75% of patients are male.
Presenting symptoms include fever and upper abdominal pain. Tumors involving the hepatic hilum may cause portal hypertension and biliary obstruction, rarely requiring liver transplantation (Pediatr Transplant 2004;8:517). Other associated conditions are occlusive phlebitis and chronic cholangitis (Hum Pathol 1994;25:86). Uncommon associations are with Crohn's disease and posthematopoietic stem cell transplantation (J Clin Gastroenterol 2004;38:818, Bone Marrow Transplant 2004;33:103). Surgery is curative, although the tumors occasionally regress spontaneously.
Grossly, the tumors are usually well circumscribed and 70% are solitary. Tumors may extend into the inferior vena cava or retroperitoneal soft tissue. They have a variegated cut surface, often with hemorrhage and necrosis.
Microscopically, the tumors consist of a mixture of inflammatory cells, particularly polyclonal plasma cells, lymphocytes, eosinophils and macrophages. Neutrophils may also be present. There are also variable amounts of plump spindled cells resembling myofibroblasts and mature fibroblasts. The stroma is often whorled, resembling leiomyoma or fibrotic resembling sclerosing hemangioma. Mitotic activity is rare.
The spindled cells are immunoreactive for vimentin, smooth muscle actin and muscle specific actin in 80% of cases. There is variable immunoreactivity for desmin and pankeratin stains. These tumors are negative for S100, CD21 and CD35. A small percentage are ALK+, which is associated with a favorable prognosis at all sites combined (Am J Surg Pathol 2001;25:761).
The differential diagnosis is large. First, if the excision is subtotal, the diagnosis must be considered tentative, as other neoplasms may have a similar inflammatory component. Second, dendritic cell tumors must be excluded. They usually occur in women, often have systemic symptoms and are immunoreactive for follicular dendritic cell markers CD21 and CD35. The inflammatory tumor-like variant is usually associated with Epstein-Barr virus infection (Am J Surg Pathol 2001;25:721). Third, infectious disorders, such as TB, syphilis or bacterial abscess may cause an inflammatory infiltrate and antibiotics or NSAIDS may cause tumor regression (Acta Gastroenterol Belg 2005;68:382, Scand J Gastroenterol 2005;40:875, J Clin Pathol 2003;56:868). Fourth, inflammatory disorders such as sarcoidosis, malakoplakia, abscess and cholangiohepatitis should be considered. Finally, tumors to consider include sclerosing hemangioma, leiomyoma, solitary fibrous tumor, sarcomatoid carcinoma, nerve sheath tumors, Hodgkin lymphoma and MFH. Postoperative spindle cell nodule is similar morphologically but has a different clinical history.
A recent study suggests that cases associated with sclerosing cholangitis may represent an IgG4 related biliary disease that is part of the spectrum of sclerosing pancreatitis and is responsive to steroids (Am J Surg Pathol 2004;28:1193).
References: Am J Surg Pathol 1993;17:231