7 June 2006 - Case #48
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Raghava Munivenkatappa, University of Maryland, USA.
Case #48
Clinical history:
A 50 year old African American woman with a past medical history of hypertension, asthma, steroid use and hepatitis C underwent right radical nephrectomy for a renal mass. The right kidney measured 12.1 cm superior to inferior, 4.9 cm medial to lateral and 2.8 cm anterior to posterior. The attached urethra measured 7.3 cm in length x 0.4 cm in average diameter and was slightly dilated. A well capsulated mass was present at upper pole, protruding into the hilar region. The cut surface was tan-yellow, homogeneous and slightly greasy. The mass was 6.7 x 5.9 x 5.5 cm. The mass replaced most of the renal parenchyma of the upper pole and protruded into the hilar region. No hemorrhage or necrosis was identified. The uninvolved kidney parenchyma was tan-pink to brown with a distinct corticomedullary junction.
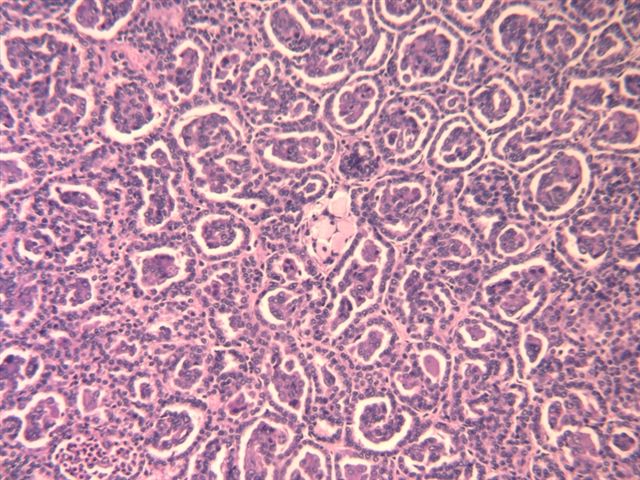
Microscopic image:
What is your diagnosis?
Diagnosis: Papillary carcinoma, solid variant
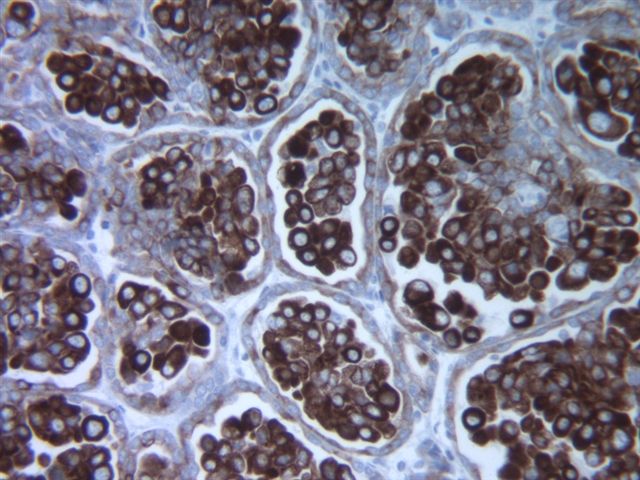
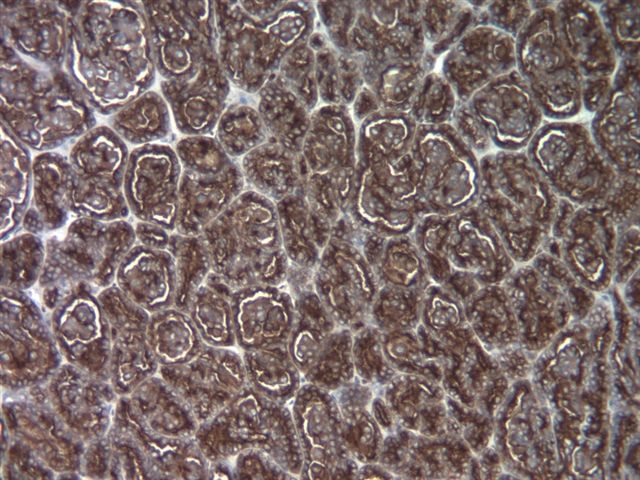
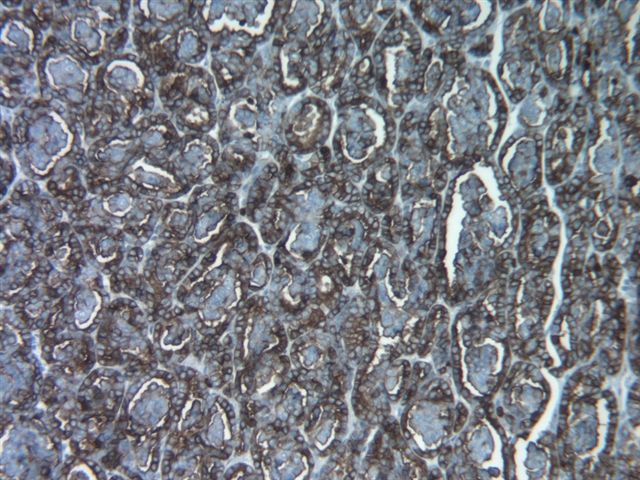
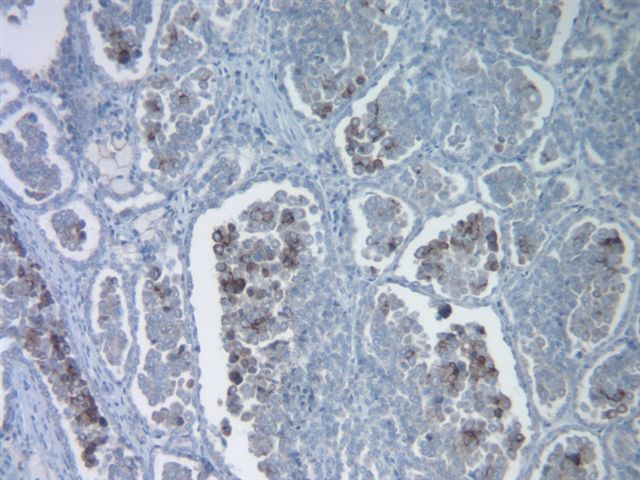
Stain images:
Discussion:
Papillary carcinoma is a common subtype of renal cell carcinoma, representing 10 - 20% of adult tumors. It is also called chromophil carcinoma and some cases were previously called granular type. Accurate classification is important because these tumors tend to present at an early stage and to have a better prognosis than other types. These tumors are often multifocal, are immunoreactive for CK7 and usually have trisomy 7 or 17. Classically, they are defined as having at least 50% true papillae.
The solid variant was first described in detail in 1997 (Am J Surg Pathol 1997;21:1203). It contains sheets of cells, often with distinct micronodules resembling abortive papillae but with no true papillae. Cells have abundant eosinophilic or clear cytoplasm with vesicular nuclei and often prominent nucleoli. Tumor cells are immunoreactive for CK7 and EMA and negative for 34 beta E12 (high molecular weight keratin) and vimentin. As with classic papillary carcinoma, there is often trisomy 7 or 17.
The differential diagnosis includes mucinous tubular and spindle cell carcinoma, a recently described subtype of renal cell carcinoma that also has a compact tubular architecture with focal papillary features and a similar immunohistochemistry profile as the solid variant of papillary carcinoma. However, it has a low grade spindle cell population not found in papillary carcinoma (Am J Surg Pathol 2006;30:13).
The differential diagnosis also includes metanephric adenoma, which may also exhibit trisomy 7 and 17 (Chang Gung Med J 2001;24:582, J Urol 1997;158:370 but see Mod Pathol 2003;16:1060). However, the cells in metanephric adenoma are more primitive with scant cytoplasm, instead of abundant eosinophilic cytoplasm and the chromatin is hyperchromatic and grainy with instinct nucleoli. In addition, metanephric adenoma typically is vimentin positive with only focal CK7 immunoreactivity and is EMA negative.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Raghava Munivenkatappa, University of Maryland, USA.
Case #48
Clinical history:
A 50 year old African American woman with a past medical history of hypertension, asthma, steroid use and hepatitis C underwent right radical nephrectomy for a renal mass. The right kidney measured 12.1 cm superior to inferior, 4.9 cm medial to lateral and 2.8 cm anterior to posterior. The attached urethra measured 7.3 cm in length x 0.4 cm in average diameter and was slightly dilated. A well capsulated mass was present at upper pole, protruding into the hilar region. The cut surface was tan-yellow, homogeneous and slightly greasy. The mass was 6.7 x 5.9 x 5.5 cm. The mass replaced most of the renal parenchyma of the upper pole and protruded into the hilar region. No hemorrhage or necrosis was identified. The uninvolved kidney parenchyma was tan-pink to brown with a distinct corticomedullary junction.
Microscopic image:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Papillary carcinoma, solid variant
Stain images:
Discussion:
Papillary carcinoma is a common subtype of renal cell carcinoma, representing 10 - 20% of adult tumors. It is also called chromophil carcinoma and some cases were previously called granular type. Accurate classification is important because these tumors tend to present at an early stage and to have a better prognosis than other types. These tumors are often multifocal, are immunoreactive for CK7 and usually have trisomy 7 or 17. Classically, they are defined as having at least 50% true papillae.
The solid variant was first described in detail in 1997 (Am J Surg Pathol 1997;21:1203). It contains sheets of cells, often with distinct micronodules resembling abortive papillae but with no true papillae. Cells have abundant eosinophilic or clear cytoplasm with vesicular nuclei and often prominent nucleoli. Tumor cells are immunoreactive for CK7 and EMA and negative for 34 beta E12 (high molecular weight keratin) and vimentin. As with classic papillary carcinoma, there is often trisomy 7 or 17.
The differential diagnosis includes mucinous tubular and spindle cell carcinoma, a recently described subtype of renal cell carcinoma that also has a compact tubular architecture with focal papillary features and a similar immunohistochemistry profile as the solid variant of papillary carcinoma. However, it has a low grade spindle cell population not found in papillary carcinoma (Am J Surg Pathol 2006;30:13).
The differential diagnosis also includes metanephric adenoma, which may also exhibit trisomy 7 and 17 (Chang Gung Med J 2001;24:582, J Urol 1997;158:370 but see Mod Pathol 2003;16:1060). However, the cells in metanephric adenoma are more primitive with scant cytoplasm, instead of abundant eosinophilic cytoplasm and the chromatin is hyperchromatic and grainy with instinct nucleoli. In addition, metanephric adenoma typically is vimentin positive with only focal CK7 immunoreactivity and is EMA negative.