15 May 2008 - Case #119
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Nazar M. T. Jawhar, University of Science and Technology Hospital, Sana'a, Yemen.
Case #119
Clinical history:
A 17 year old girl presented with ataxia and an intraventricular mass within the lateral ventricle was identified by imaging. A biopsy was performed.
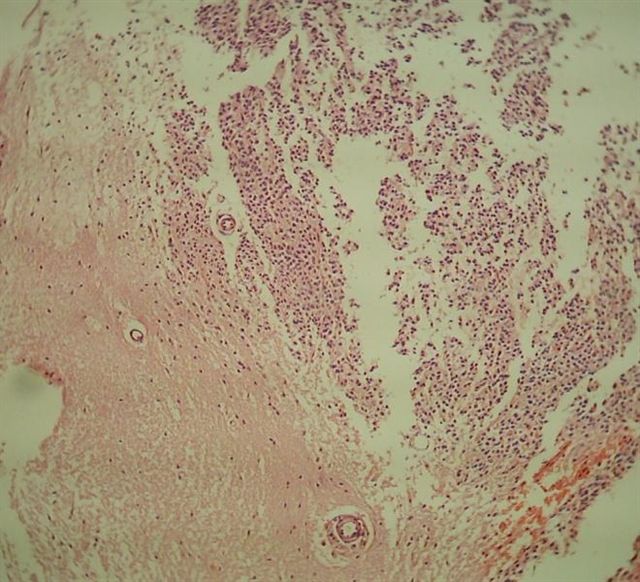
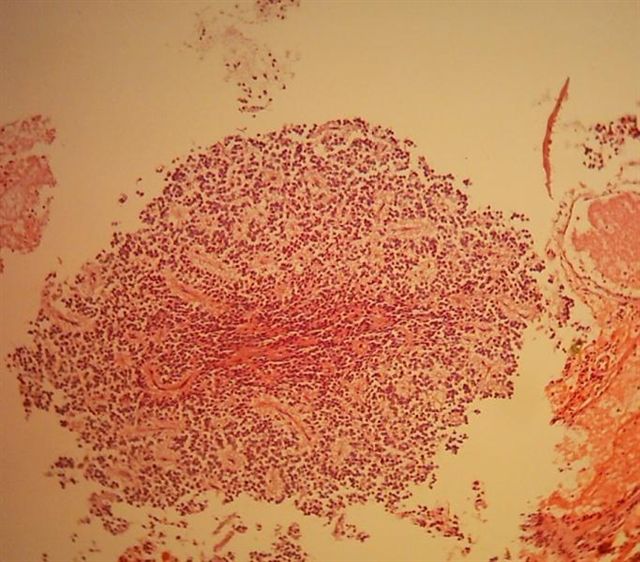
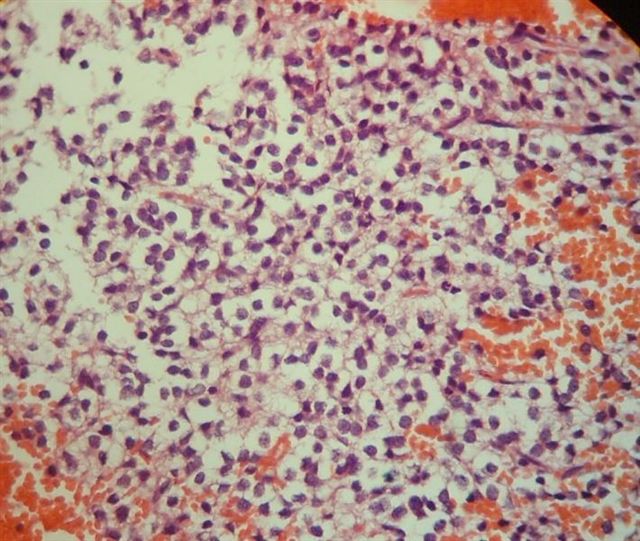
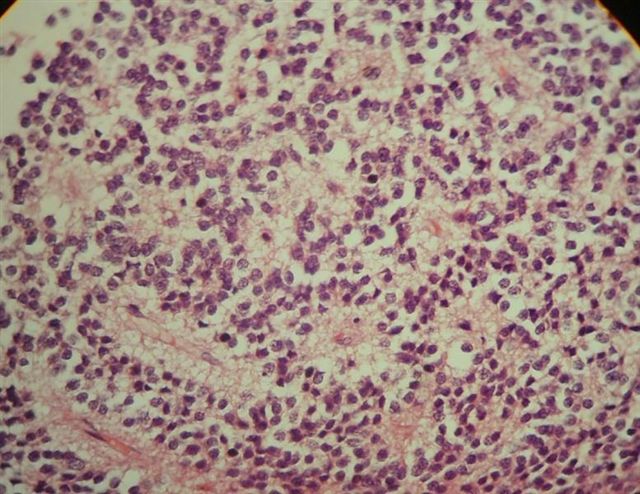
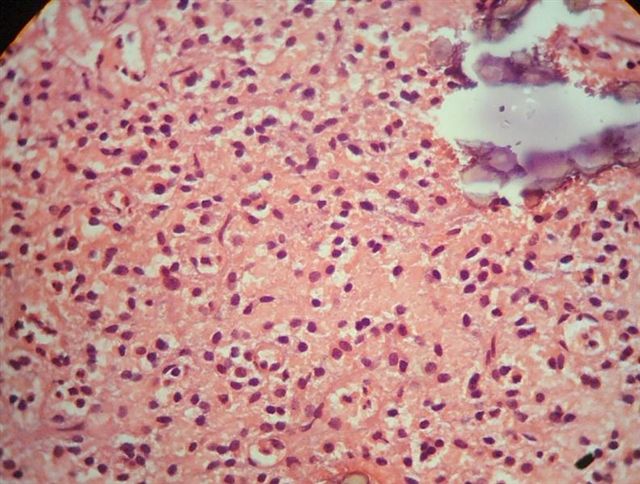
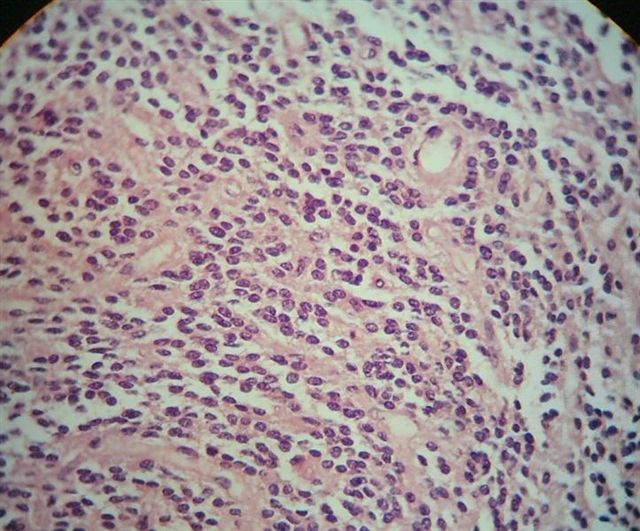
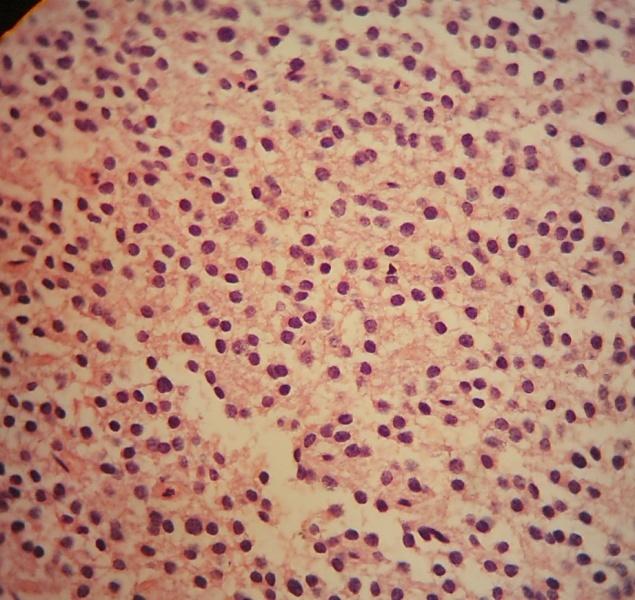
Microscopic images:
What is your diagnosis?
Diagnosis: Central (differentiated) neurocytoma (WHO grade II)
Discussion:
Central neurocytoma, first described in 1982, is a common tumor of the septum pellucidum in young adults but still represents less than 1% of all CNS tumors (Acta Neuropathol 1982;56:151). It commonly grows into the lateral or third ventricle. It often presents with increased intracranial pressure due to obstructive hydrocephalus and, exceptionally, with sudden death due to hemorrhage (Am J Forensic Med Pathol 1999;20:180). Similar tumors within CNS parenchyma are called extraventricular neurocytoma.
Grossly, it is well demarcated from surrounding tissue and is gray and friable. It may be gritty due to microcalcifications. Microscopically, it has well developed neuronal features, including monotonous bland cells with modest cytoplasm, halos similar to oligodendroglioma and salt and pepper chromatin. Tumor cells are embedded in an eosinophilic fibrillar matrix with rare Homer Wright rosettes and ganglion cells. Necrosis or mitotic figures occur rarely, if at all, and there is no endothelial proliferation.
The tumor cells are immunoreactive for synaptophysin, NeuN (strong) and neuron specific enolase but negative for GFAP, although reactive astrocytes are GFAP+ (Histopathology 2006;48:438). The tumor cells also show low Ki67 (< 2%) immunostaining.
The differential diagnosis includes glioma (no / few halo cells, no / focal neuronal features, strongly GFAP+), oligodendroglioma (negative or focal for neuronal markers) and clear cell ependymoma (negative for neuronal markers, strongly positive for GFAP, vimentin and EMA).
These tumors have a good prognosis after complete surgical excision or gamma knife radiosurgery, although up to 33% recur or progress (Cancer 2007;110:2276, Int J Radiat Oncol Biol Phys 2007;67:1145). Recurrence is associated with incomplete excision or the presence of necrosis, mitotic activity / increased proliferation rates or microvascular proliferation (Cancer 2000;89:1111, Clin Neurol Neurosurg 2008;110:129).
Additional reference: Louis: WHO Classification of Tumours of the Central Nervous System, 4th Edition, 2007
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
This case was contributed by Dr. Nazar M. T. Jawhar, University of Science and Technology Hospital, Sana'a, Yemen.
Case #119
Clinical history:
A 17 year old girl presented with ataxia and an intraventricular mass within the lateral ventricle was identified by imaging. A biopsy was performed.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Central (differentiated) neurocytoma (WHO grade II)
Discussion:
Central neurocytoma, first described in 1982, is a common tumor of the septum pellucidum in young adults but still represents less than 1% of all CNS tumors (Acta Neuropathol 1982;56:151). It commonly grows into the lateral or third ventricle. It often presents with increased intracranial pressure due to obstructive hydrocephalus and, exceptionally, with sudden death due to hemorrhage (Am J Forensic Med Pathol 1999;20:180). Similar tumors within CNS parenchyma are called extraventricular neurocytoma.
Grossly, it is well demarcated from surrounding tissue and is gray and friable. It may be gritty due to microcalcifications. Microscopically, it has well developed neuronal features, including monotonous bland cells with modest cytoplasm, halos similar to oligodendroglioma and salt and pepper chromatin. Tumor cells are embedded in an eosinophilic fibrillar matrix with rare Homer Wright rosettes and ganglion cells. Necrosis or mitotic figures occur rarely, if at all, and there is no endothelial proliferation.
The tumor cells are immunoreactive for synaptophysin, NeuN (strong) and neuron specific enolase but negative for GFAP, although reactive astrocytes are GFAP+ (Histopathology 2006;48:438). The tumor cells also show low Ki67 (< 2%) immunostaining.
The differential diagnosis includes glioma (no / few halo cells, no / focal neuronal features, strongly GFAP+), oligodendroglioma (negative or focal for neuronal markers) and clear cell ependymoma (negative for neuronal markers, strongly positive for GFAP, vimentin and EMA).
These tumors have a good prognosis after complete surgical excision or gamma knife radiosurgery, although up to 33% recur or progress (Cancer 2007;110:2276, Int J Radiat Oncol Biol Phys 2007;67:1145). Recurrence is associated with incomplete excision or the presence of necrosis, mitotic activity / increased proliferation rates or microvascular proliferation (Cancer 2000;89:1111, Clin Neurol Neurosurg 2008;110:129).
Additional reference: Louis: WHO Classification of Tumours of the Central Nervous System, 4th Edition, 2007