21 June 2012 - Case #246
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Shahrzad Ehdaivand, Women & Infants Hospital & Warren Alpert Medical School of Brown University, for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Advertisement
Case #246
Clinical history:
A 53 year old woman had a hysterectomy for vaginal bleeding.
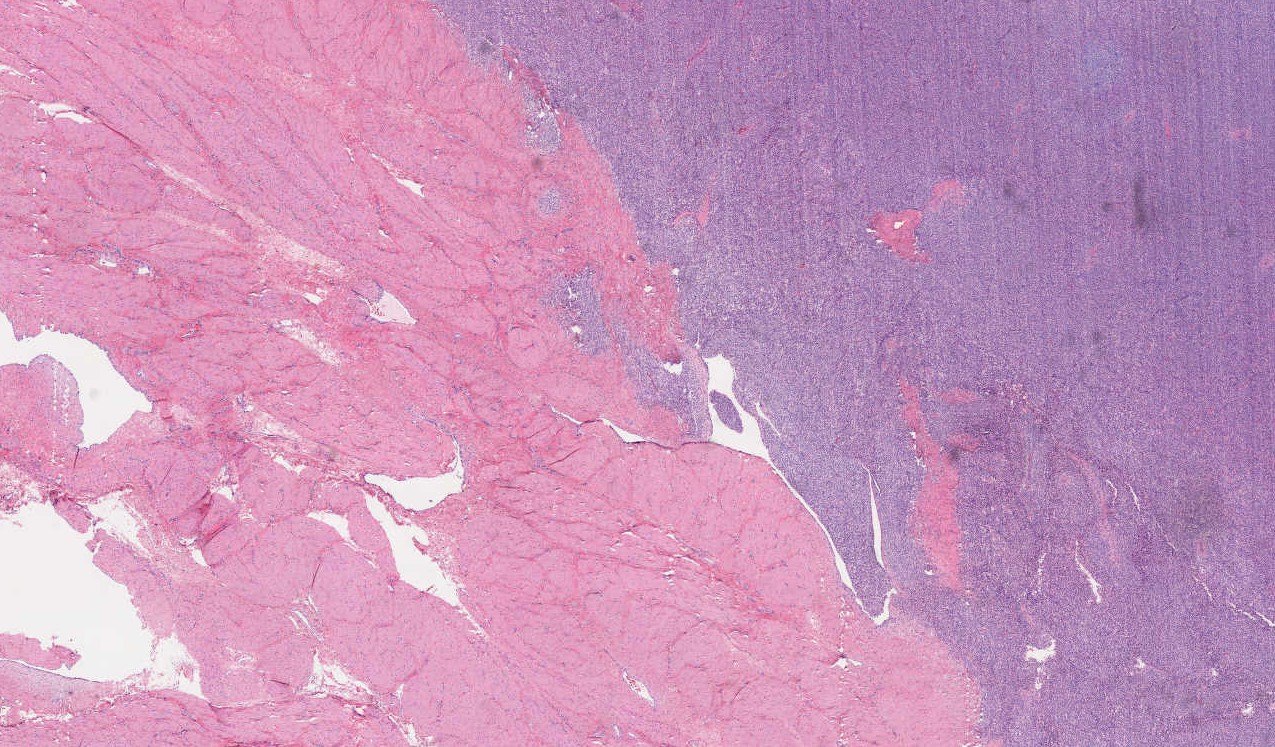
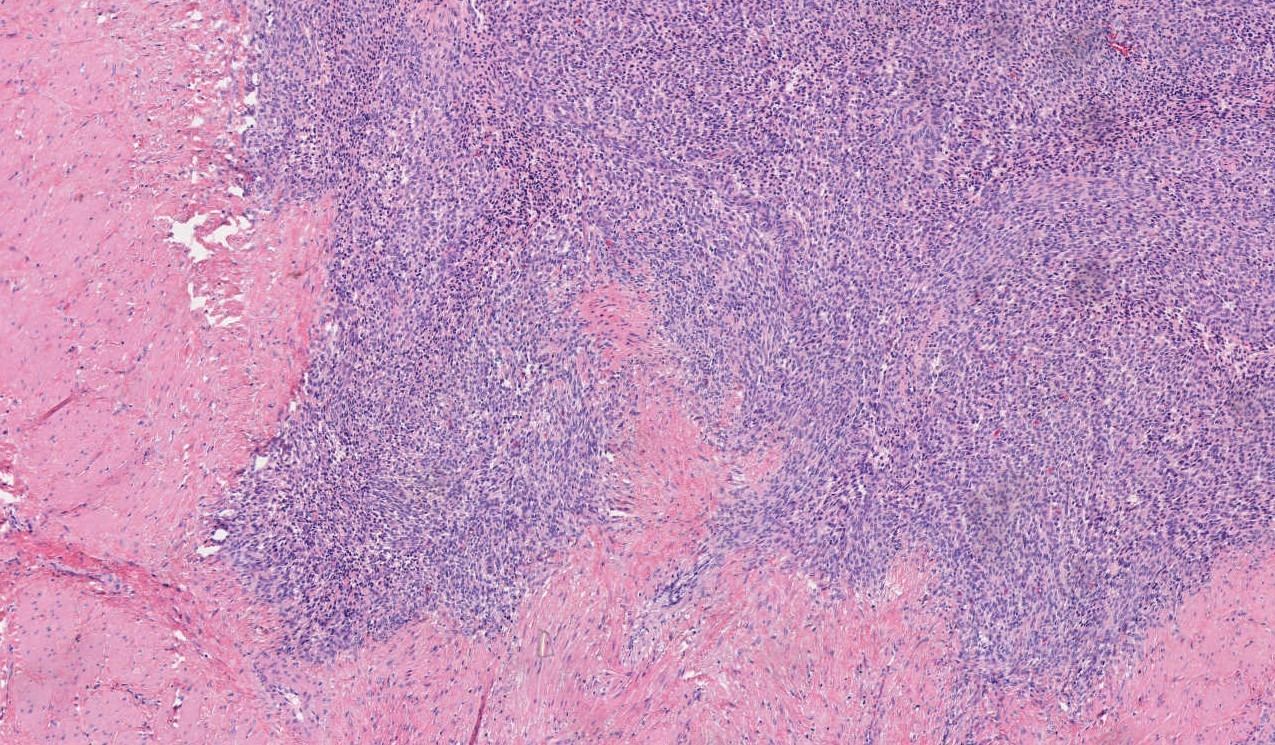
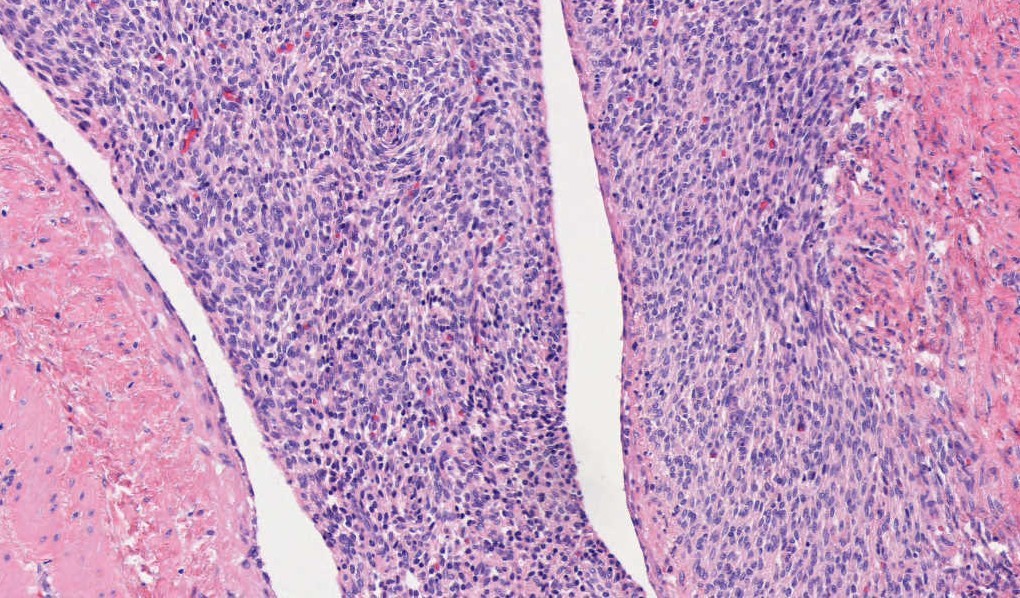
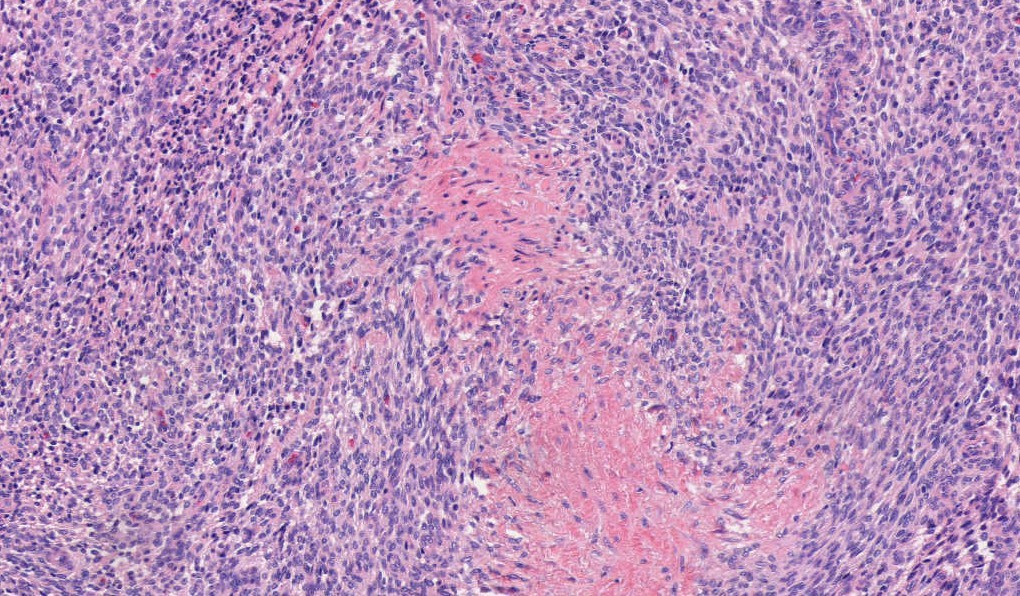
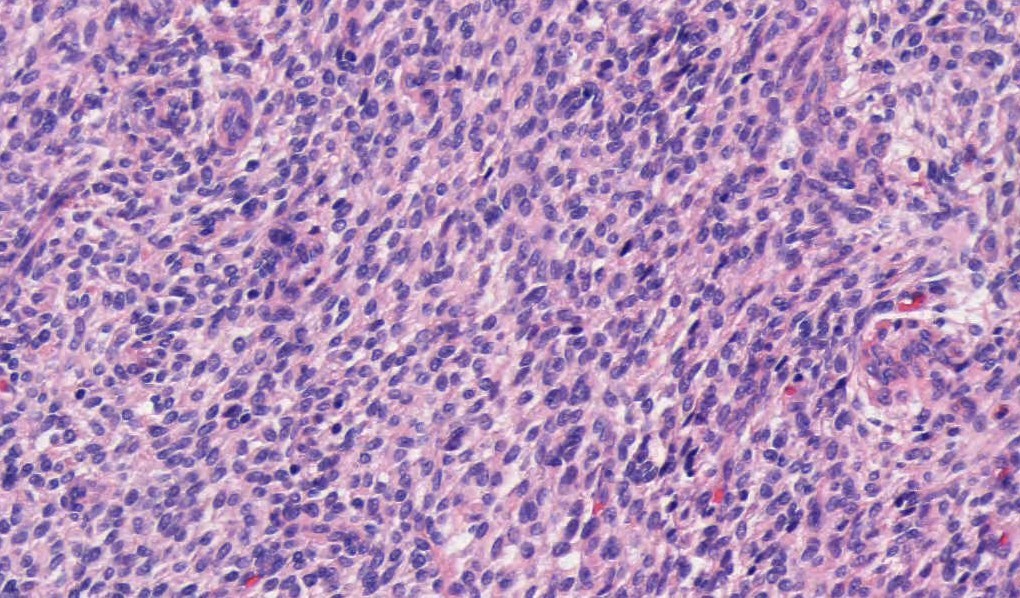
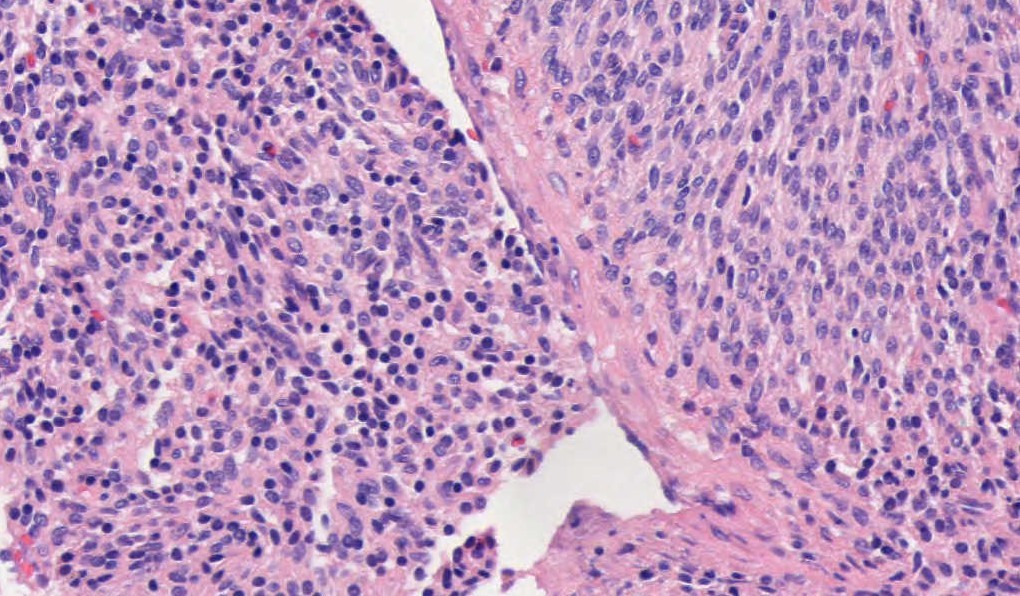
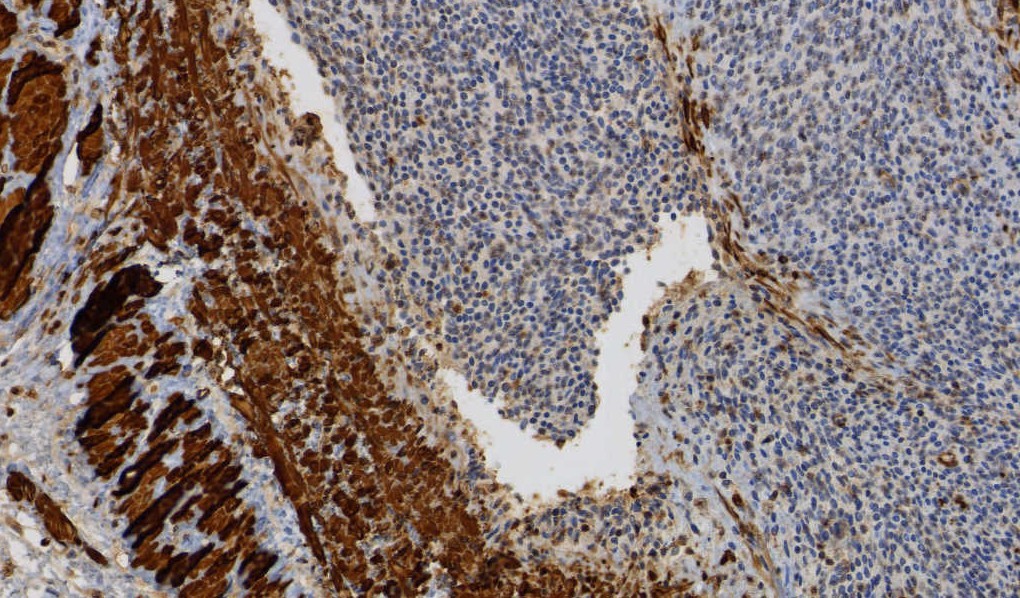
Microscopic images:
What is your diagnosis?
Diagnosis: Endometrial stromal sarcoma
Discussion:
Endometrial stromal tumors may be benign (stromal nodule) or malignant (low grade and high grade endometrial stromal sarcomas). Endometrial stromal nodules and low grade endometrial stromal sarcomas have a haphazard (not fascicular) arrangement of uniform small cells resembling endometrial stroma (i.e., blunt, spindled to oval cells with scant cytoplasm and small, uniform nuclei). Each cell is individually enveloped by reticulin fibers. The stromal cells surround small / thin vessels that resemble spiral arterioles; thick vessels can be seen at the periphery of the tumor.
Low grade endometrial stromal sarcomas are defined by the presence of infiltration into the surrounding wall, which typically has a finger-like or tongue-like appearance (given the bulbous and convex size of the infiltrative nodularities); lymphovascular invasion is often seen and is a feature exclusive of low grade endometrial stromal sarcoma (endometrial stromal nodules should not have LVI). There is usually little cytological atypia or pleomorphism, and mitoses are scanty. Recurrent translocations are detected in > 80% of cases, most commonly the JAZF1::SUZ12 fusion (Am J Surg Pathol 2007;31:1277, Histopathology 2015;67:1).
High grade endometrial stromal sarcomas are a relatively recent diagnostic category, defined by the presence of recurrent aberrations such as YWHAE::NUTM2 fusion and BCOR alterations (Am J Surg Pathol 2012;36:641). YWHAE::NUTM2 rearranged sarcomas are characterized by a round cell component in which tumor nuclei are larger than in low grade sarcomas; a low grade spindle cell component is seen in 50% of cases. BCOR altered sarcomas tend to be predominantly fibromyxoid and feature monotonous to moderately atypical spindle cells (Mod Pathol 2018;31:674). Both forms of high grade endometrial stromal sarcoma are clinically aggressive.
In contrast, undifferentiated uterine sarcomas are frankly malignant and lack specific differentiation and any features of normal endometrial stroma. They often have destructive and irregular myometrial invasion, hemorrhage and necrosis, as well as marked nuclear pleomorphism and high mitotic activity.
The differential diagnosis of low grade endometrial stromal sarcoma includes:
In low grade endometrial stromal sarcoma, even after hysterectomy, there is often slow clinical progression with repeated local recurrences in up to 50%. Death due to disease occurs in 15%, often due to lung metastases, which may occur 30 years later.
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Shahrzad Ehdaivand, Women & Infants Hospital & Warren Alpert Medical School of Brown University, for contributing this case. This case was reviewed in May 2020 by Dr. Jennifer Bennett, University of Chicago and Dr. Carlos Parra-Herran, University of Toronto.
Best Practices for Anatomic Pathology Quality
Pathology Leadership: Free 45 minute webinar
Wednesday June 27th at 12:00pm Eastern
Register (link invalid)
Sponsored by: AccuPathology - Pathology Quality Management Software
● Integrate with your LIS to automate tasks, identifying potential QA to be performed
● Identify pre-analytic and post-analytic variables that contribute to diagnostic errors
● Automate mandated OPPE, FPPE processes with quantitative data
● Dashboards and pro-forma reports for improved operations, CAP and The Joint Commission audits
Spend less time, getting better information to make REAL changes while always being compliant.
Website (link invalid)
Phone: (267) 564-5015
Website news:
(1) In our popular Stains chapter, we have updated these topics: AMACR, EMA / MUC1, IgH, PD-1, PU.1. We have also updated CD133 from the CD Markers chapter.
(2) The Ovary-nontumor chapter has now been updated, based on reviews by Mohiedean Ghofrani, M.D. and Shahidul Islam, M.D. The Colon tumor chapter has also been updated, based on reviews by Jela Bandovic, M.D., Shilpa Jain, M.D. and Charanjeet Singh, M.D.
(3) Our Feature Page for the month highlights Diagnostic testing / reagents, and includes Advanced Cell Diagnostics, Inc. (ACD), bioTheranostics, Covance, Epitomics, Horizon Diagnostics, Leica Microsystems and Ventana Medical.
Visit and follow our Blog to see recent updates to the website.
(1) In our popular Stains chapter, we have updated these topics: AMACR, EMA / MUC1, IgH, PD-1, PU.1. We have also updated CD133 from the CD Markers chapter.
(2) The Ovary-nontumor chapter has now been updated, based on reviews by Mohiedean Ghofrani, M.D. and Shahidul Islam, M.D. The Colon tumor chapter has also been updated, based on reviews by Jela Bandovic, M.D., Shilpa Jain, M.D. and Charanjeet Singh, M.D.
(3) Our Feature Page for the month highlights Diagnostic testing / reagents, and includes Advanced Cell Diagnostics, Inc. (ACD), bioTheranostics, Covance, Epitomics, Horizon Diagnostics, Leica Microsystems and Ventana Medical.
Visit and follow our Blog to see recent updates to the website.
Case #246
Clinical history:
A 53 year old woman had a hysterectomy for vaginal bleeding.
Microscopic images:
What is your diagnosis?
Click here for diagnosis and discussion:
Diagnosis: Endometrial stromal sarcoma
Discussion:
Endometrial stromal tumors may be benign (stromal nodule) or malignant (low grade and high grade endometrial stromal sarcomas). Endometrial stromal nodules and low grade endometrial stromal sarcomas have a haphazard (not fascicular) arrangement of uniform small cells resembling endometrial stroma (i.e., blunt, spindled to oval cells with scant cytoplasm and small, uniform nuclei). Each cell is individually enveloped by reticulin fibers. The stromal cells surround small / thin vessels that resemble spiral arterioles; thick vessels can be seen at the periphery of the tumor.
Low grade endometrial stromal sarcomas are defined by the presence of infiltration into the surrounding wall, which typically has a finger-like or tongue-like appearance (given the bulbous and convex size of the infiltrative nodularities); lymphovascular invasion is often seen and is a feature exclusive of low grade endometrial stromal sarcoma (endometrial stromal nodules should not have LVI). There is usually little cytological atypia or pleomorphism, and mitoses are scanty. Recurrent translocations are detected in > 80% of cases, most commonly the JAZF1::SUZ12 fusion (Am J Surg Pathol 2007;31:1277, Histopathology 2015;67:1).
High grade endometrial stromal sarcomas are a relatively recent diagnostic category, defined by the presence of recurrent aberrations such as YWHAE::NUTM2 fusion and BCOR alterations (Am J Surg Pathol 2012;36:641). YWHAE::NUTM2 rearranged sarcomas are characterized by a round cell component in which tumor nuclei are larger than in low grade sarcomas; a low grade spindle cell component is seen in 50% of cases. BCOR altered sarcomas tend to be predominantly fibromyxoid and feature monotonous to moderately atypical spindle cells (Mod Pathol 2018;31:674). Both forms of high grade endometrial stromal sarcoma are clinically aggressive.
In contrast, undifferentiated uterine sarcomas are frankly malignant and lack specific differentiation and any features of normal endometrial stroma. They often have destructive and irregular myometrial invasion, hemorrhage and necrosis, as well as marked nuclear pleomorphism and high mitotic activity.
The differential diagnosis of low grade endometrial stromal sarcoma includes:
- Endometrial stromal nodule: no / minimal infiltration, no angiolymphatic invasion
- Adenomyosis with sparse glands: this is usually an incidental finding in post menopausal women with typical areas of adenomyosis usually present; the foci of endometrial type stroma are small and do not have an expansile convex outline
- Cellular leiomyoma: no infiltration, no angiolymphatic invasion, fascicular growth with thick walled vessels throughout the tumor; strong expression of smooth muscle markers
In low grade endometrial stromal sarcoma, even after hysterectomy, there is often slow clinical progression with repeated local recurrences in up to 50%. Death due to disease occurs in 15%, often due to lung metastases, which may occur 30 years later.