17 July 2019 - Case of the Month #481
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Yubo "Mike" Wu, Beth Israel Deaconess Medical Center, Boston, Massachusetts (USA) for contributing this case and Dr. Raul S. Gonzalez Beth Israel Deaconess Medical Center, Boston, Massachusetts (USA), for writing the discussion.
Case of the Month #481
Clinical history:
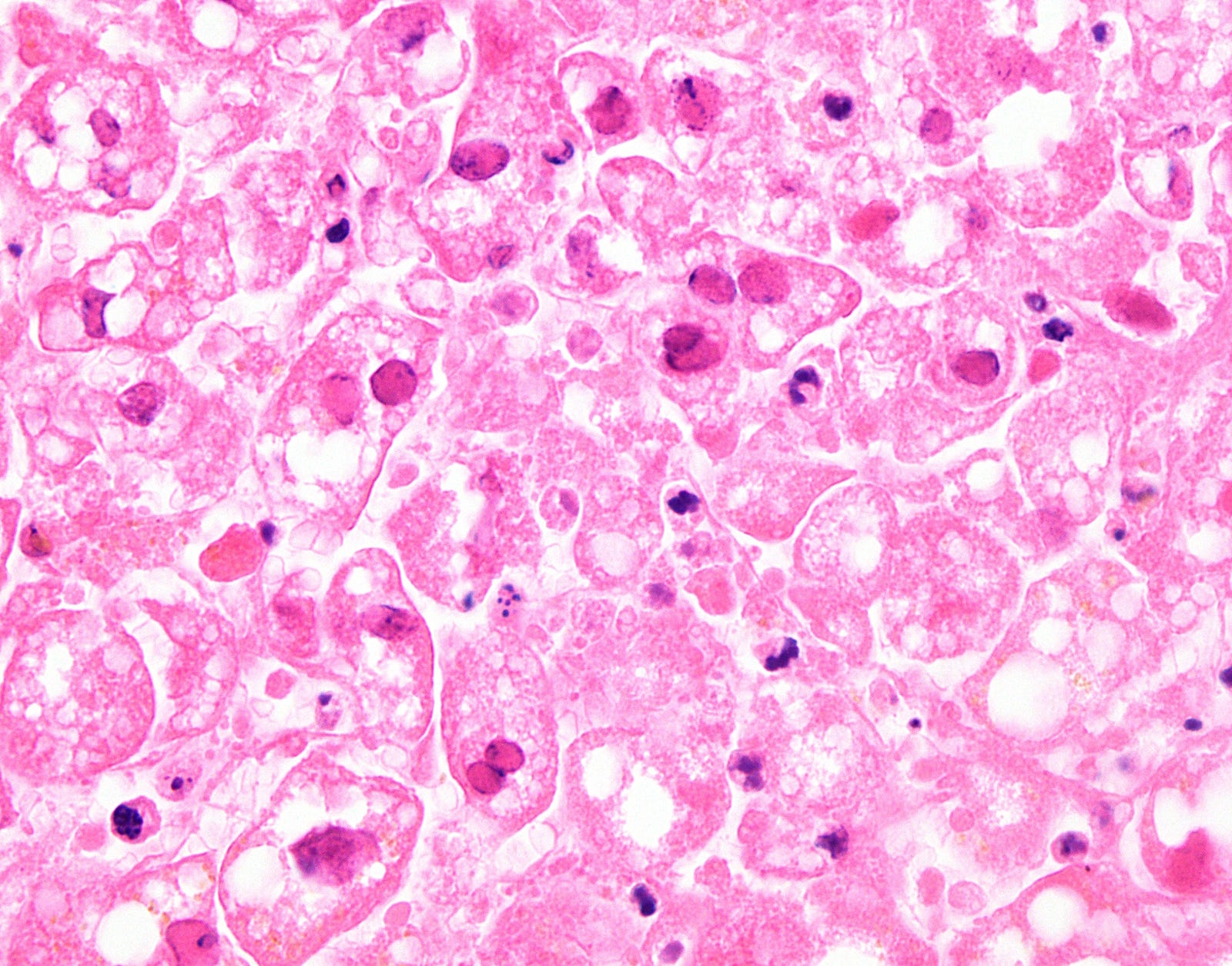
A 44 year old woman presented with nausea and vomiting. She had a history of breast cancer, diagnosed in 2010 and treated with bilateral mastectomy and tamoxifen. She died after later developing diarrhea, uncoordinated gait, intermittent fever and pancytopenia. An autopsy was performed, with liver photomicrographs shown below.
Histopathology images:
What is your diagnosis?
Diagnosis: Herpetic hepatitis
Test question (answer at the end):
Herpes simplex hepatitis causes necrosis of hepatocytes in what pattern?
A. Nonzonal necrosis
B. Zone 1 necrosis
C. Zone 2 necrosis
D. Zone 3 necrosis
Stains:
Discussion:
Herpes simplex virus is an uncommon cause of liver failure in adults (Liver Transpl 2008;14:1498). Immunocompromised patients are most susceptible but immunocompetent patients can be affected as well (Am J Clin Pathol 1986;85:694), with risk factors including malignancy and pregnancy (Hum Pathol 1992;23:183). The clinical presentation in adults is typically that of shock; diagnosis may not be established until autopsy. Neonates can also acquire herpes congenitally (as it is one of the TORCH infections), with roughly a quarter of them at risk for developing fulminant hepatitis.
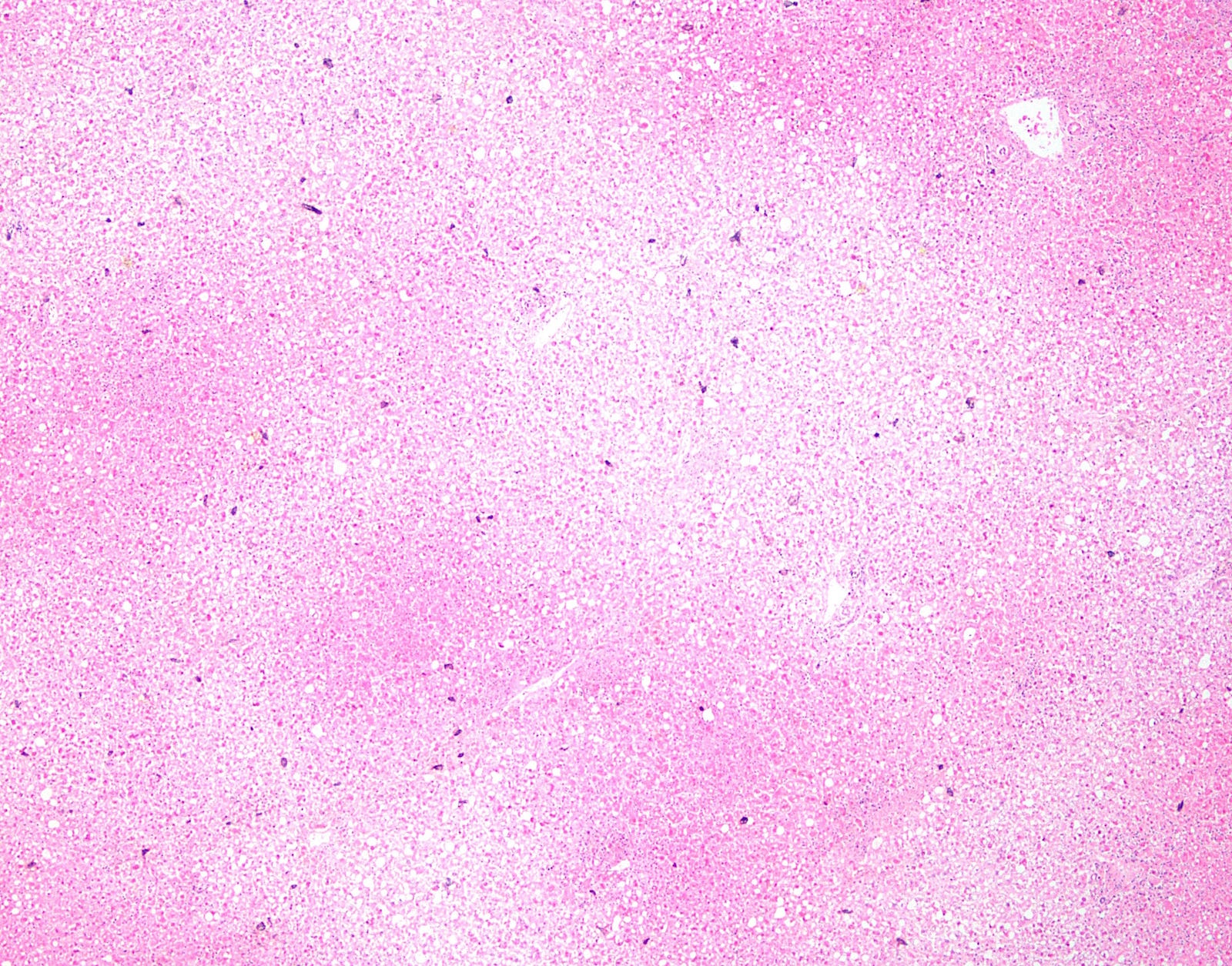
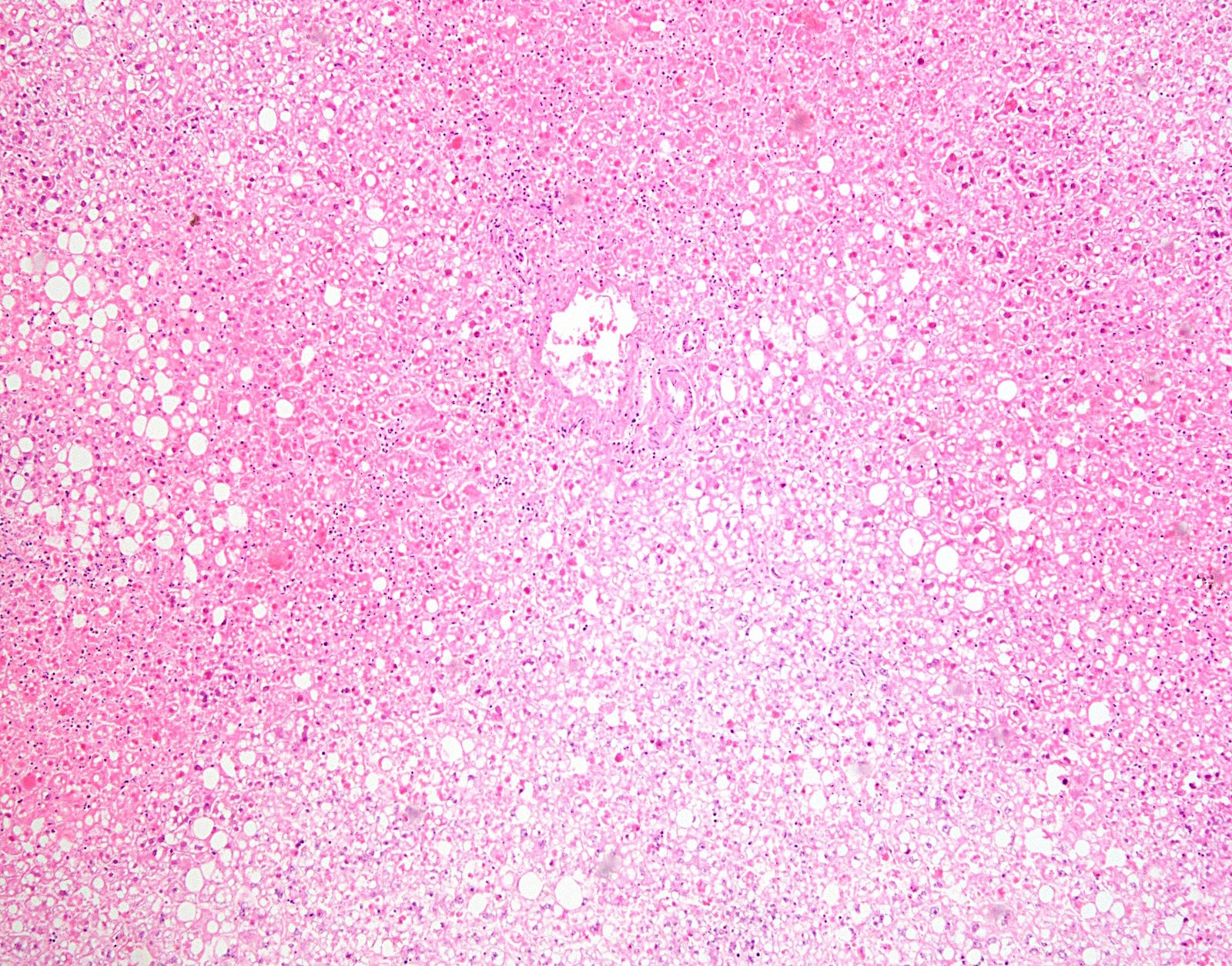
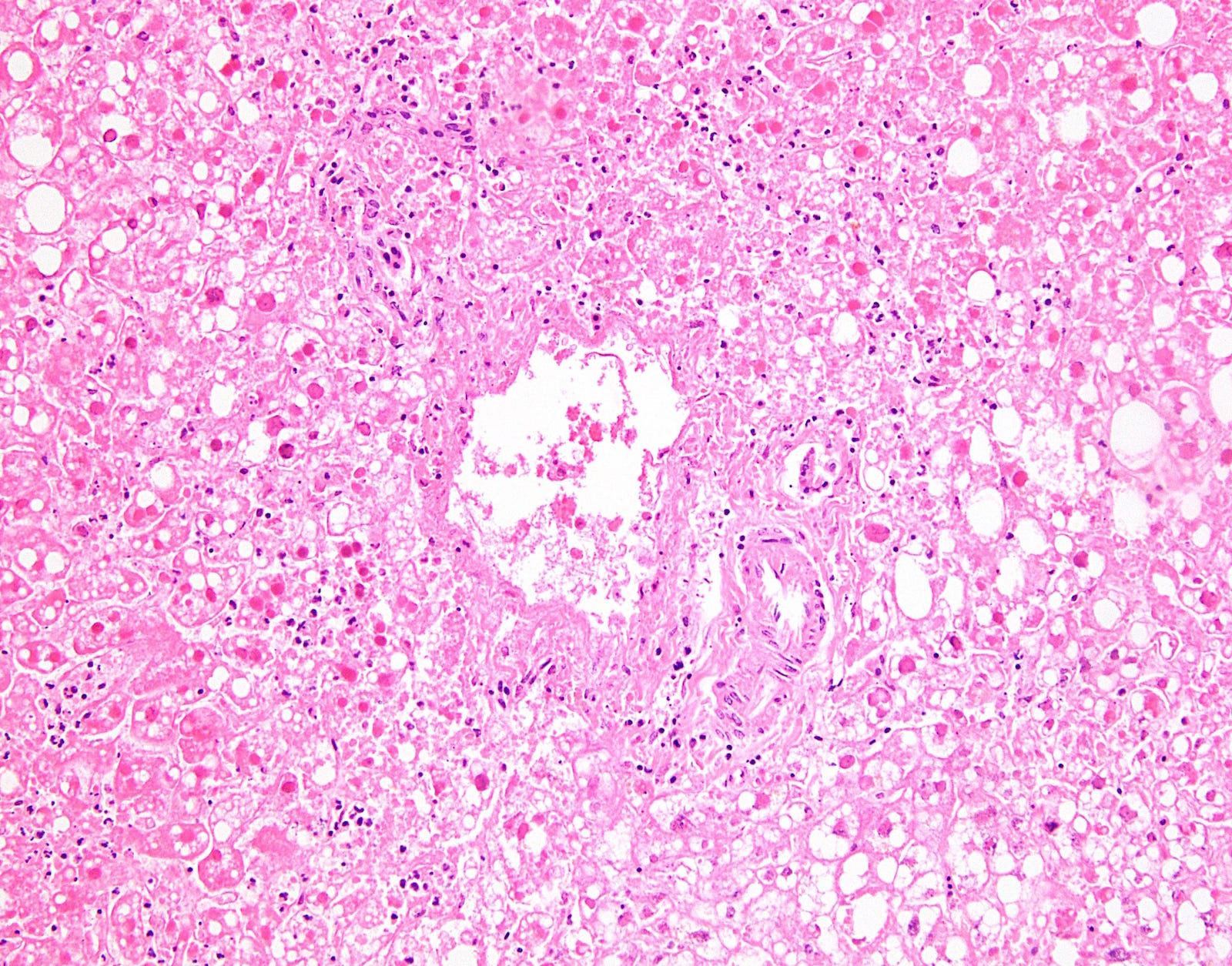
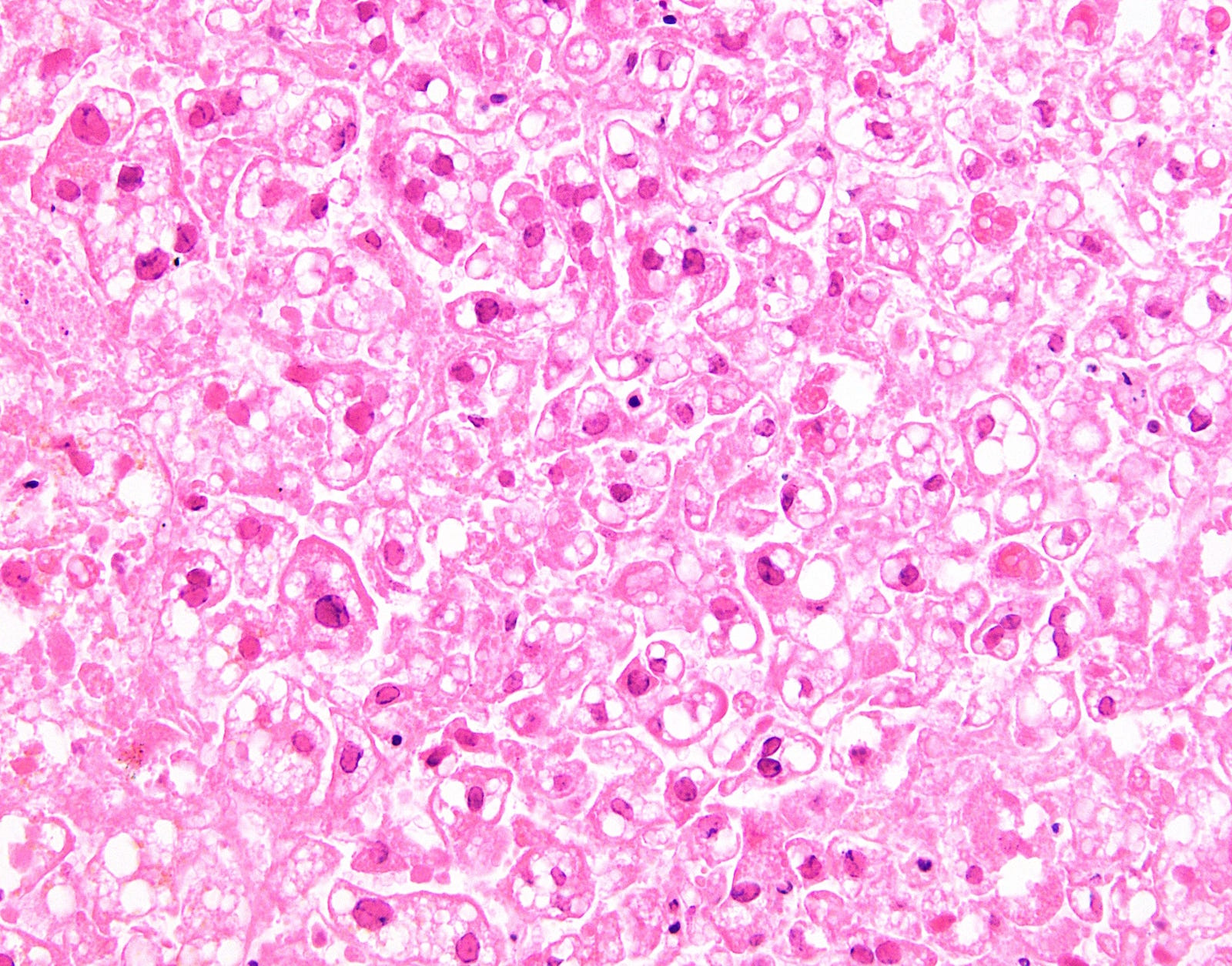
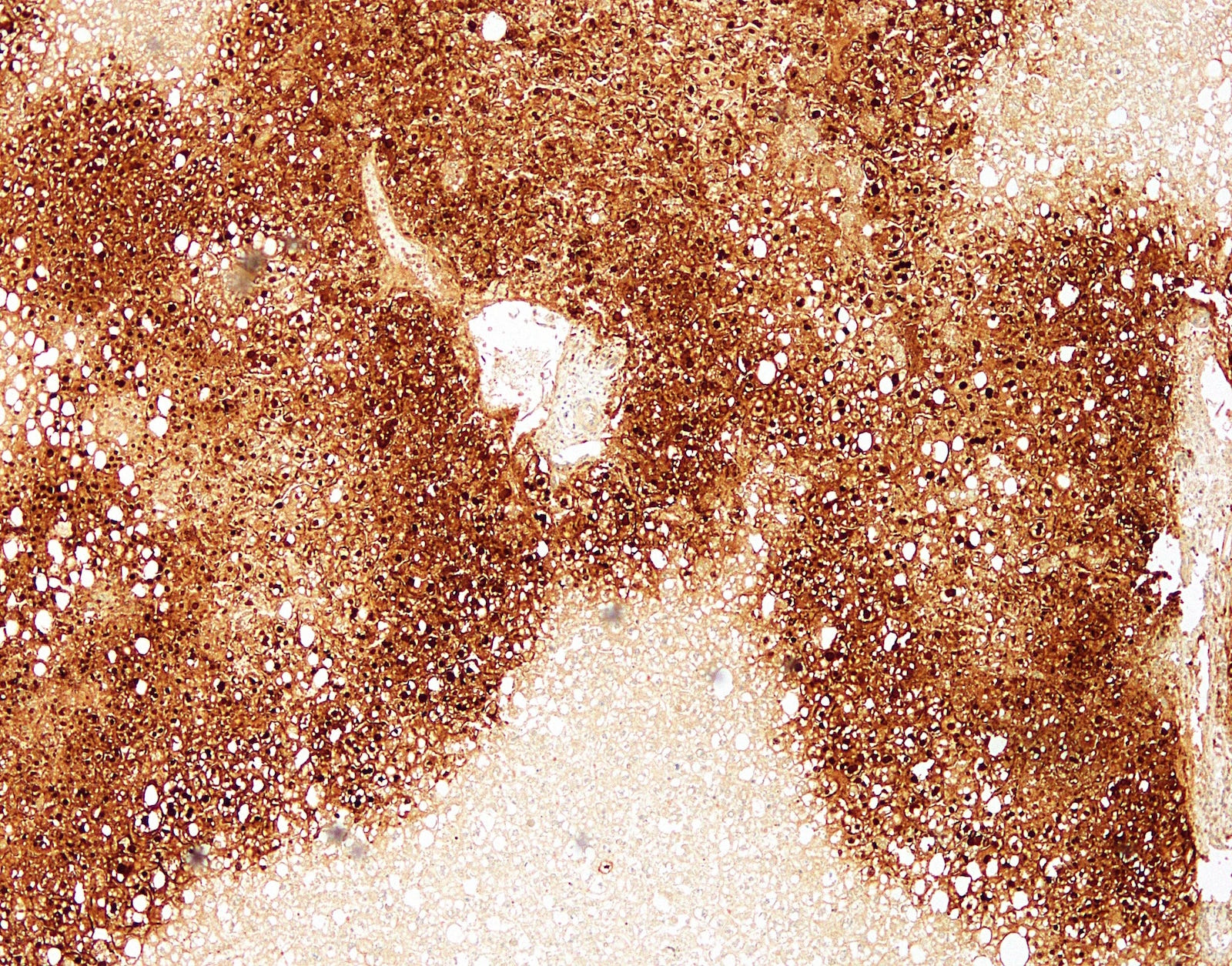
At low power, herpes causes geographic (nonzonal) hemorrhagic necrosis of the hepatic parenchyma, with viable and nonviable areas distributed in a patchy, seemingly random fashion, sometimes with a clean separating border. On higher power, the classic nuclear features of herpes infection (margination, multinucleation, molding) are seen in hepatocytes, although multinucleation is not always observed in the liver. Immunohistochemistry for HSV1 is positive, confirming the diagnosis.
The differential diagnosis includes other causes of hepatic necrosis and other causes of viral cytopathic effect:
• Hypoperfusion (e.g., due to hypovolemic shock) can cause zone 3 necrosis (diagram)
• Most medications that cause hepatic necrosis (e.g., acetaminophen causes zone 3 necrosis; unusual substances may primarily induce necrosis in other zones)
• Viral hemorrhagic fever (e.g., yellow fever) can cause zone 2 necrosis, possibly also with zone 3 necrosis
• Disseminated intravascular coagulation and eclampsia may cause zone 1 necrosis
• Cytomegalovirus can cause prominent "owl’s-eye" inclusions in hepatocytes, endothelial cells and biliary epithelium. They are easier to detect in immunocompromised patients. Fulminant hepatic failure is not the typical presentation but can occur.
• Adenovirus is the closest histologic mimicker of hepatic hepatitis. It also causes random zones of necrosis and viral cytopathic effect. The involved hepatocytes have a basophilic, smudgy nucleus without any multinucleation. Immunohistochemistry for adenovirus can distinguish adenovirus from herpes.
• Measles in the liver may cause multinucleation without margination or molding. Additionally, eosinophilic cytoplasmic inclusions may be detected. Necrosis would be spotty.
Test question answer:
A. Nonzonal necrosis
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Dr. Yubo "Mike" Wu, Beth Israel Deaconess Medical Center, Boston, Massachusetts (USA) for contributing this case and Dr. Raul S. Gonzalez Beth Israel Deaconess Medical Center, Boston, Massachusetts (USA), for writing the discussion.
Case of the Month #481
Clinical history:
A 44 year old woman presented with nausea and vomiting. She had a history of breast cancer, diagnosed in 2010 and treated with bilateral mastectomy and tamoxifen. She died after later developing diarrhea, uncoordinated gait, intermittent fever and pancytopenia. An autopsy was performed, with liver photomicrographs shown below.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Herpetic hepatitis
Test question (answer at the end):
Herpes simplex hepatitis causes necrosis of hepatocytes in what pattern?
A. Nonzonal necrosis
B. Zone 1 necrosis
C. Zone 2 necrosis
D. Zone 3 necrosis
Stains:
Discussion:
Herpes simplex virus is an uncommon cause of liver failure in adults (Liver Transpl 2008;14:1498). Immunocompromised patients are most susceptible but immunocompetent patients can be affected as well (Am J Clin Pathol 1986;85:694), with risk factors including malignancy and pregnancy (Hum Pathol 1992;23:183). The clinical presentation in adults is typically that of shock; diagnosis may not be established until autopsy. Neonates can also acquire herpes congenitally (as it is one of the TORCH infections), with roughly a quarter of them at risk for developing fulminant hepatitis.
At low power, herpes causes geographic (nonzonal) hemorrhagic necrosis of the hepatic parenchyma, with viable and nonviable areas distributed in a patchy, seemingly random fashion, sometimes with a clean separating border. On higher power, the classic nuclear features of herpes infection (margination, multinucleation, molding) are seen in hepatocytes, although multinucleation is not always observed in the liver. Immunohistochemistry for HSV1 is positive, confirming the diagnosis.
The differential diagnosis includes other causes of hepatic necrosis and other causes of viral cytopathic effect:
• Hypoperfusion (e.g., due to hypovolemic shock) can cause zone 3 necrosis (diagram)
• Most medications that cause hepatic necrosis (e.g., acetaminophen causes zone 3 necrosis; unusual substances may primarily induce necrosis in other zones)
• Viral hemorrhagic fever (e.g., yellow fever) can cause zone 2 necrosis, possibly also with zone 3 necrosis
• Disseminated intravascular coagulation and eclampsia may cause zone 1 necrosis
• Cytomegalovirus can cause prominent "owl’s-eye" inclusions in hepatocytes, endothelial cells and biliary epithelium. They are easier to detect in immunocompromised patients. Fulminant hepatic failure is not the typical presentation but can occur.
• Adenovirus is the closest histologic mimicker of hepatic hepatitis. It also causes random zones of necrosis and viral cytopathic effect. The involved hepatocytes have a basophilic, smudgy nucleus without any multinucleation. Immunohistochemistry for adenovirus can distinguish adenovirus from herpes.
• Measles in the liver may cause multinucleation without margination or molding. Additionally, eosinophilic cytoplasmic inclusions may be detected. Necrosis would be spotty.
Test question answer:
A. Nonzonal necrosis