16 December 2021 - Case of the Month #510
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Lisa Han and Ricardo Lastra, University of Chicago Medical Center, Chicago, Illinois, USA, for contributing this case and the discussion and to Dr. Gulisa Turashvili, Mount Sinai Hospital, Toronto, Ontario, Canada, for reviewing the discussion.

Case of the Month #510
Clinical history:
A 69 year old woman with a history of bilateral hydronephrosis presented with weight loss and vaginal spotting and underwent vaginal biopsy.
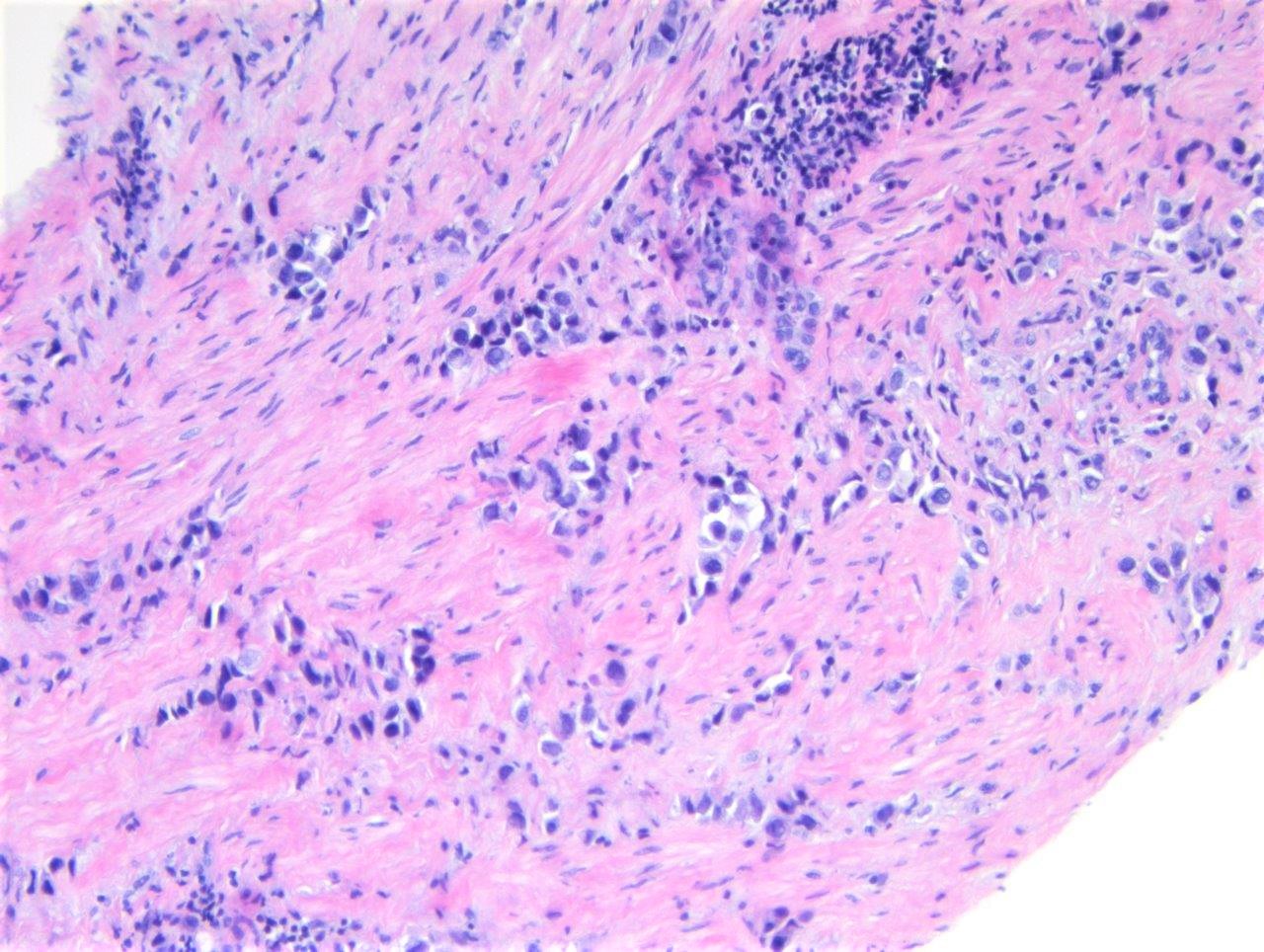
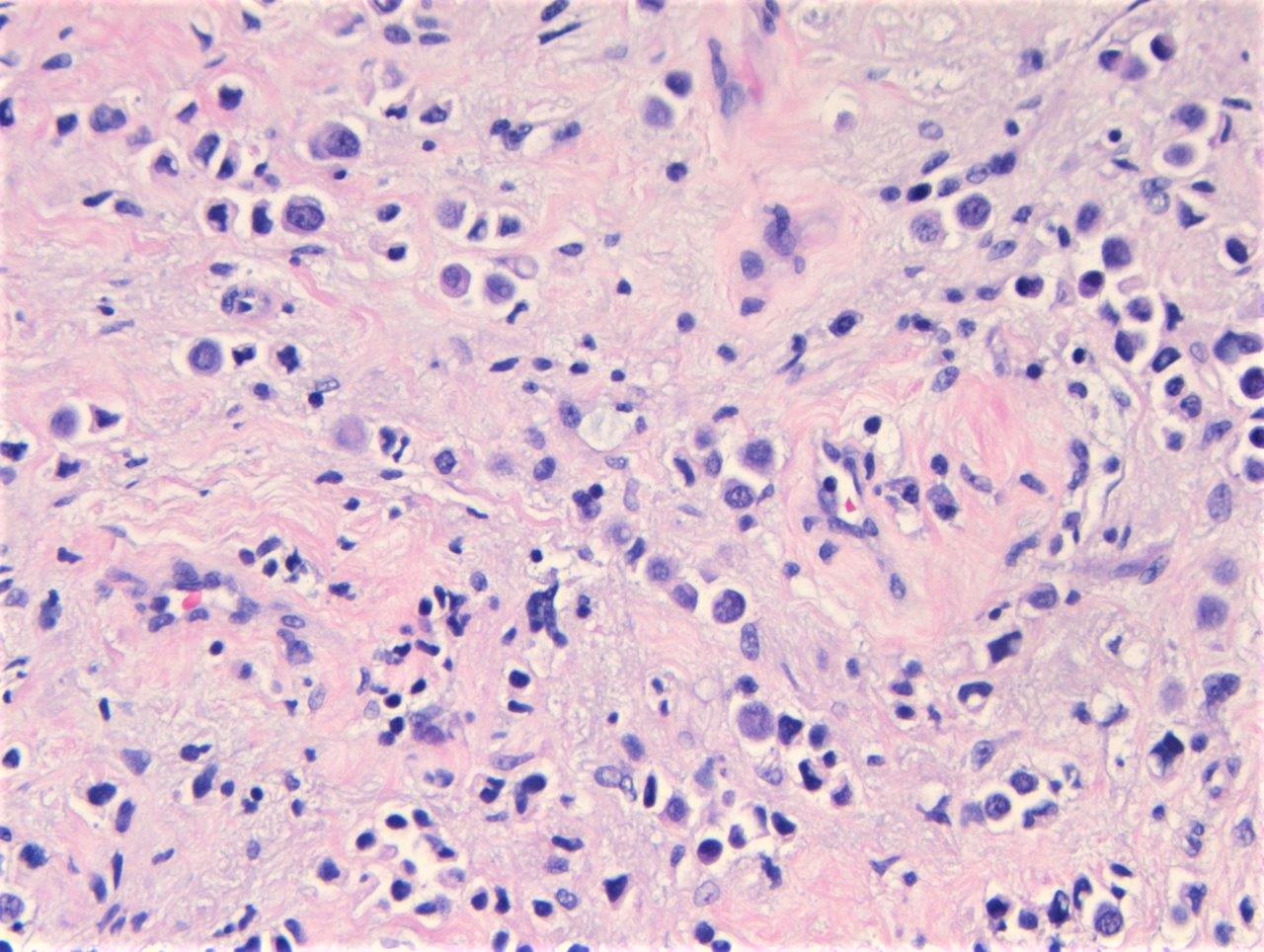
Histopathology images:
What is your diagnosis?
Diagnosis: Urothelial carcinoma, plasmacytoid variant
Test question (answer at the end):
Which panel of immunohistochemical stains would be most helpful to distinguish plasmacytoid urothelial carcinoma from its mimickers at other primary sites?
A. CD138, CK20, CK7, ER, PR
B. CD138, CK20, CDX2, GCDFP-15
C. p63, GATA3, E-cadherin
D. GATA3, mammaglobin, ER, uroplakin II
Discussion:
Plasmacytoid urothelial carcinoma (PUC) is a rare variant of invasive urothelial carcinoma characterized by discohesive infiltrating cells with plasmacytoid morphology. PUC is typically diagnosed at a more advanced clinical stage than conventional urothelial carcinoma, likely owing to its widely infiltrative growth, permeating the bladder in a linitis plastica-like manner rather than as an exophytic mass (Urology 2017;102:143). In one study of 510 patients, lymph node metastasis was identified in 72% at presentation (Urology 2014;83:1112).
The morphology of the malignant cells of PUC range from discohesive round to ovoid cells with moderate eosinophilic cytoplasm and eccentric nuclei to signet ring cells with intracytoplasmic mucin (Hum Pathol 2009;40:1023, Am J Surg Pathol 2017;41:1570). They may infiltrate as single cells or grow in sheets. Mitoses may be abundant. A surface urothelial in situ component, when present, may be very helpful in establishing the diagnosis.
The differential diagnosis includes metastatic breast lobular carcinoma and gastrointestinal signet ring cell carcinoma. The wide morphologic overlap necessitates use of a panel of immunohistochemical stains to aid diagnosis. The immunohistochemical profile of PUC is similar to that of conventional urothelial carcinoma, with expression of GATA3, p63, S100P, high molecular weight keratin, CK7, CK20 and uroplakin II (Am J Surg Pathol 2017;41:1570, Arch Pathol Lab Med 2019;143:1562). GATA3 is expressed in approximately 80% of PUC cases, while p63 stains 45%, which is less than observed in conventional urothelial carcinoma. PUC mostly coexpress CK7 (92%) and CK20 (72%). In one study comparing immunohistochemistry of PUC to lobular breast carcinoma, a panel of mammaglobin, ER and uroplakin II was recommended because mammaglobin and ER were not expressed in any cases of PUC (Am J Surg Pathol 2017;41:1570). Unfortunately, PUC was found to express GCDFP-15 (24%), PR (13%), CDX2 (18%) and p-CEA (49%). To rule out gastrointestinal primary, the use of GATA3 and uroplakin II may be more helpful, as neither stains are expressed in those tumors.
Test question answer:
D. A panel including GATA3, mammaglobin, ER and uroplakin II would be helpful. GATA3, more so than p63, is positive in plasmacytoid urothelial carcinoma (PUC) and while it does not differentiate between breast and urothelial origin, is helpful in ruling out gastrointestinal metastases. Mammaglobin and ER are consistently negative in PUC, which helps differentiate PUC from breast metastasis, particularly lobular carcinoma, which is more often ER positive. UroplakinII is helpful as it is negative in nonurothelial mimickers. CD138 has been reported to be positive in PUC although it is nonspecific with expression reported in squamous cell carcinoma, normal urothelium and other epithelial and lymphoid malignancies (Int J Surg Pathol 2016;24:614). E-cadherin expression is typically abnormal in both PUC and breast lobular carcinoma, which includes complete absence of staining or aberrant cytoplasmic staining. Of note, E-cadherin staining was normal in 27% of PUC cases in a recent study (Hum Pathol 2020;102:54).
All cases are archived on our website. To view them sorted by case number, diagnosis or category, visit our main Case of the Month page. To subscribe or unsubscribe to Case of the Month or our other email lists, click here.
Thanks to Drs. Lisa Han and Ricardo Lastra, University of Chicago Medical Center, Chicago, Illinois, USA, for contributing this case and the discussion and to Dr. Gulisa Turashvili, Mount Sinai Hospital, Toronto, Ontario, Canada, for reviewing the discussion.

Case of the Month #510
Clinical history:
A 69 year old woman with a history of bilateral hydronephrosis presented with weight loss and vaginal spotting and underwent vaginal biopsy.
Histopathology images:
What is your diagnosis?
Click here for diagnosis, test question and discussion:
Diagnosis: Urothelial carcinoma, plasmacytoid variant
Test question (answer at the end):
Which panel of immunohistochemical stains would be most helpful to distinguish plasmacytoid urothelial carcinoma from its mimickers at other primary sites?
A. CD138, CK20, CK7, ER, PR
B. CD138, CK20, CDX2, GCDFP-15
C. p63, GATA3, E-cadherin
D. GATA3, mammaglobin, ER, uroplakin II
Discussion:
Plasmacytoid urothelial carcinoma (PUC) is a rare variant of invasive urothelial carcinoma characterized by discohesive infiltrating cells with plasmacytoid morphology. PUC is typically diagnosed at a more advanced clinical stage than conventional urothelial carcinoma, likely owing to its widely infiltrative growth, permeating the bladder in a linitis plastica-like manner rather than as an exophytic mass (Urology 2017;102:143). In one study of 510 patients, lymph node metastasis was identified in 72% at presentation (Urology 2014;83:1112).
The morphology of the malignant cells of PUC range from discohesive round to ovoid cells with moderate eosinophilic cytoplasm and eccentric nuclei to signet ring cells with intracytoplasmic mucin (Hum Pathol 2009;40:1023, Am J Surg Pathol 2017;41:1570). They may infiltrate as single cells or grow in sheets. Mitoses may be abundant. A surface urothelial in situ component, when present, may be very helpful in establishing the diagnosis.
The differential diagnosis includes metastatic breast lobular carcinoma and gastrointestinal signet ring cell carcinoma. The wide morphologic overlap necessitates use of a panel of immunohistochemical stains to aid diagnosis. The immunohistochemical profile of PUC is similar to that of conventional urothelial carcinoma, with expression of GATA3, p63, S100P, high molecular weight keratin, CK7, CK20 and uroplakin II (Am J Surg Pathol 2017;41:1570, Arch Pathol Lab Med 2019;143:1562). GATA3 is expressed in approximately 80% of PUC cases, while p63 stains 45%, which is less than observed in conventional urothelial carcinoma. PUC mostly coexpress CK7 (92%) and CK20 (72%). In one study comparing immunohistochemistry of PUC to lobular breast carcinoma, a panel of mammaglobin, ER and uroplakin II was recommended because mammaglobin and ER were not expressed in any cases of PUC (Am J Surg Pathol 2017;41:1570). Unfortunately, PUC was found to express GCDFP-15 (24%), PR (13%), CDX2 (18%) and p-CEA (49%). To rule out gastrointestinal primary, the use of GATA3 and uroplakin II may be more helpful, as neither stains are expressed in those tumors.
Test question answer:
D. A panel including GATA3, mammaglobin, ER and uroplakin II would be helpful. GATA3, more so than p63, is positive in plasmacytoid urothelial carcinoma (PUC) and while it does not differentiate between breast and urothelial origin, is helpful in ruling out gastrointestinal metastases. Mammaglobin and ER are consistently negative in PUC, which helps differentiate PUC from breast metastasis, particularly lobular carcinoma, which is more often ER positive. UroplakinII is helpful as it is negative in nonurothelial mimickers. CD138 has been reported to be positive in PUC although it is nonspecific with expression reported in squamous cell carcinoma, normal urothelium and other epithelial and lymphoid malignancies (Int J Surg Pathol 2016;24:614). E-cadherin expression is typically abnormal in both PUC and breast lobular carcinoma, which includes complete absence of staining or aberrant cytoplasmic staining. Of note, E-cadherin staining was normal in 27% of PUC cases in a recent study (Hum Pathol 2020;102:54).