Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mallikarjunappa SS, Hutchings D. CMV appendicitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/appendixCMVappendicitis.html. Accessed April 20th, 2024.
Definition / general
- Tissue invasive cytomegalovirus (CMV) infection of the appendix
- Rare entity; almost exclusively affects immunocompromised individuals
Essential features
- Presents as acute appendicitis in immunocompromised individuals
- Caused by tissue invasive CMV infection
- Treatment includes surgery and antiviral therapy
Terminology
- Cytomegalovirus (CMV) appendicitis
Epidemiology
- Rare entity
- Almost exclusively affects immunocompromised individuals, including those with human immunodeficiency virus (HIV) infection, solid organ transplant or hematopoietic stem cell transplant (J Clin Virol 2015;66:48, Arch Surg 1993;128:467, Transpl Infect Dis 2017;19:e12747)
- Extremely uncommon in immunocompetent individuals (J Clin Virol 2016;78:9)
Sites
- Appendix
Pathophysiology
- Primary CMV infection in the immunocompetent individual is typically either asymptomatic or manifested as mononucleosis-like syndrome
- After primary infection, CMV remains latent in the host and can reactivate
- In immunocompromised individuals, either primary infection or reactivation of CMV can manifest as wide range of pathologies, including gastrointestinal disease and rarely acute appendicitis (J Clin Virol 2016;78:9)
Etiology
- Tissue invasive CMV infection of the appendix
- Immunocompromised patients, including those with history of HIV infection, solid organ transplant or hematopoietic stem cell transplant
Clinical features
- Typical symptoms of acute appendicitis
- Colicky, periumbilical abdominal pain, eventually localizing to the right lower quadrant
- Nausea or vomiting
- Fever
- Immunocompromised patients may present with more prolonged prehospital course with several weeks of fever, diarrhea and abdominal pain (Arch Surg 1993;128:467)
- Perforation is common (Infect Dis Clin North Am 2010;24:995)
Diagnosis
- Clinical history including HIV infection and organ transplantation
- Radiologic evidence of acute appendicitis
- Histopathologic diagnosis
- Laboratory testing, including serum quantitative PCR assays, serology, antigen testing and viral culture (J Clin Virol 2015;66:48)
Laboratory
- Quantitative PCR assays
- Serology, CMV IgM or IgG
- pp65 antigenemia assay
- Viral culture
- References: J Clin Virol 2015;66:48, Infect Dis Clin North Am 2010;24:995
Radiology description
- CT scan of abdomen shows features of acute appendicitis, including
- Enlarged appendiceal diameter
- Wall thickening
- Periappendiceal fat stranding
- Appendiceal wall enhancement
- Appendicolith (Acta Radiol 2003;44:574, J Cardiol Cases 2023;28:113, J Clin Virol 2015;66:48)
Prognostic factors
- Excellent prognosis with surgery and antiviral treatment
- Perforation is common and may complicate course (Infect Dis Clin North Am 2010;24:995)
Case reports
- 22 year old woman with a history of orthotopic heart transplantation presented with 3 days of worsening shortness of breath, lightheadedness, abdominal pain, dysuria and fever found to have CT findings consistent with acute appendicitis (J Cardiol Cases 2023;28:113)
- 36 year old man with history of B cell acute lymphoblastic leukemia status postchemotherapy and stem cell transplantation complicated by gastrointestinal graft versus host disease (GVHD) developed acute perforated appendicitis (Transpl Infect Dis 2017;19:e12747)
- 38 year old woman, recently diagnosed with HIV, presented with right lower quadrant pain, anorexia, nausea and fever 2 weeks after initiating antiretroviral therapy found to have CT findings consistent with acute appendicitis (BMC Infect Dis 2014;14:313)
- 63 year old man with history of renal transplant presented with right iliac fossa pain, fluctuating, dull, not colicky and 1 month of progressive fatigue and no fever, found to have acute appendicitis on CT scan (Transpl Infect Dis 2013;15:96)
Treatment
- Surgery and antiviral therapy (usually ganciclovir)
Gross description
- Variable appearance depending on severity
- Changes may be present diffusely or affect only a portion of appendix
- Gross findings may not correlate with the degree of microscopic inflammation
- Early changes include dull appearance of serosa and dilatation of serosal vessels
- Edematous appendiceal wall with dilated lumen and hyperemia
- Fibrinopurulent serosal exudate
- Gangrenous appendicitis may appear as purple, green or black discoloration
- Perforation may be present
- Cut surface may show reddish discoloration, congestion or intraluminal or intramural abscess (Semin Diagn Pathol 2004;21:86)
Gross images
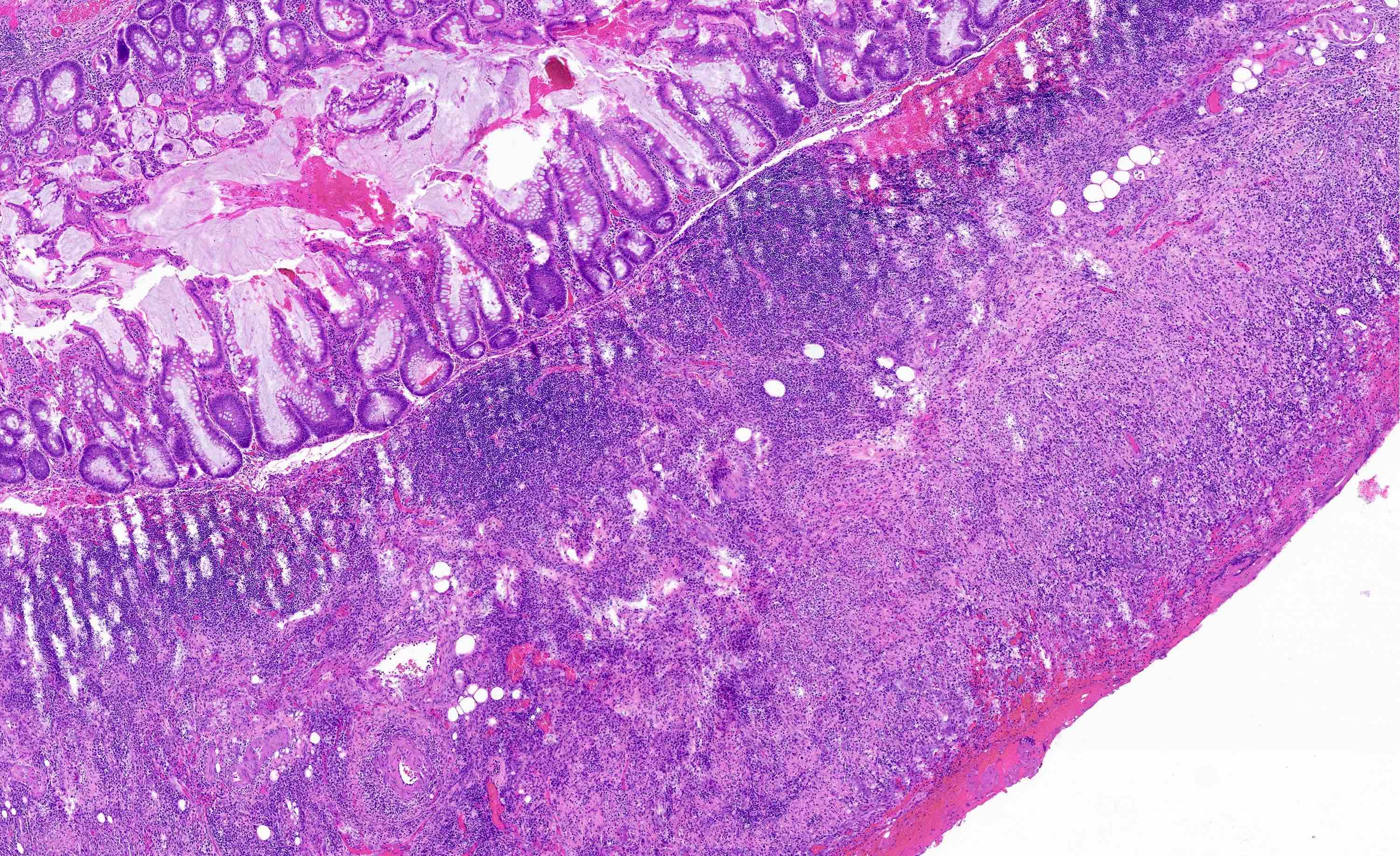
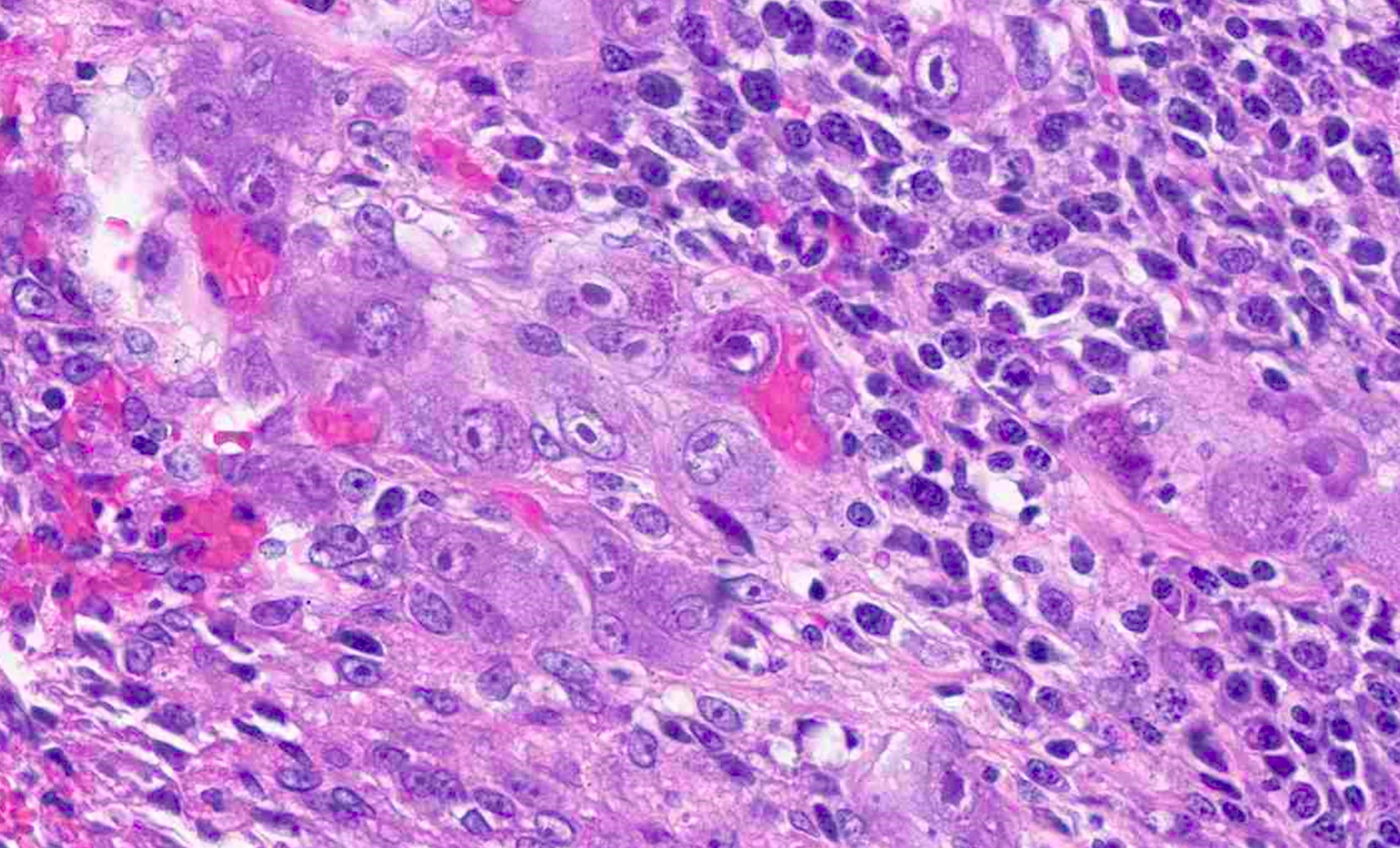
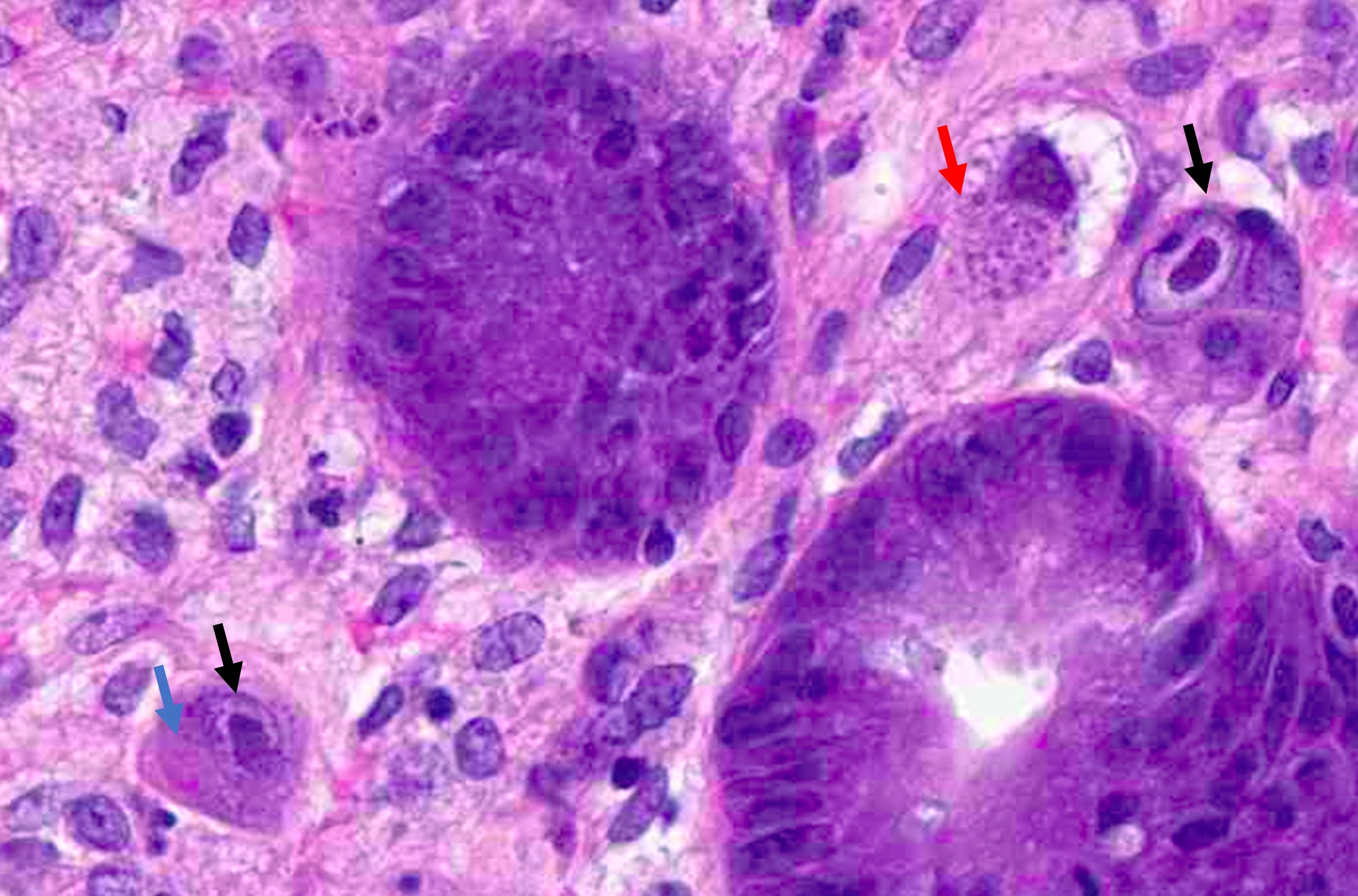
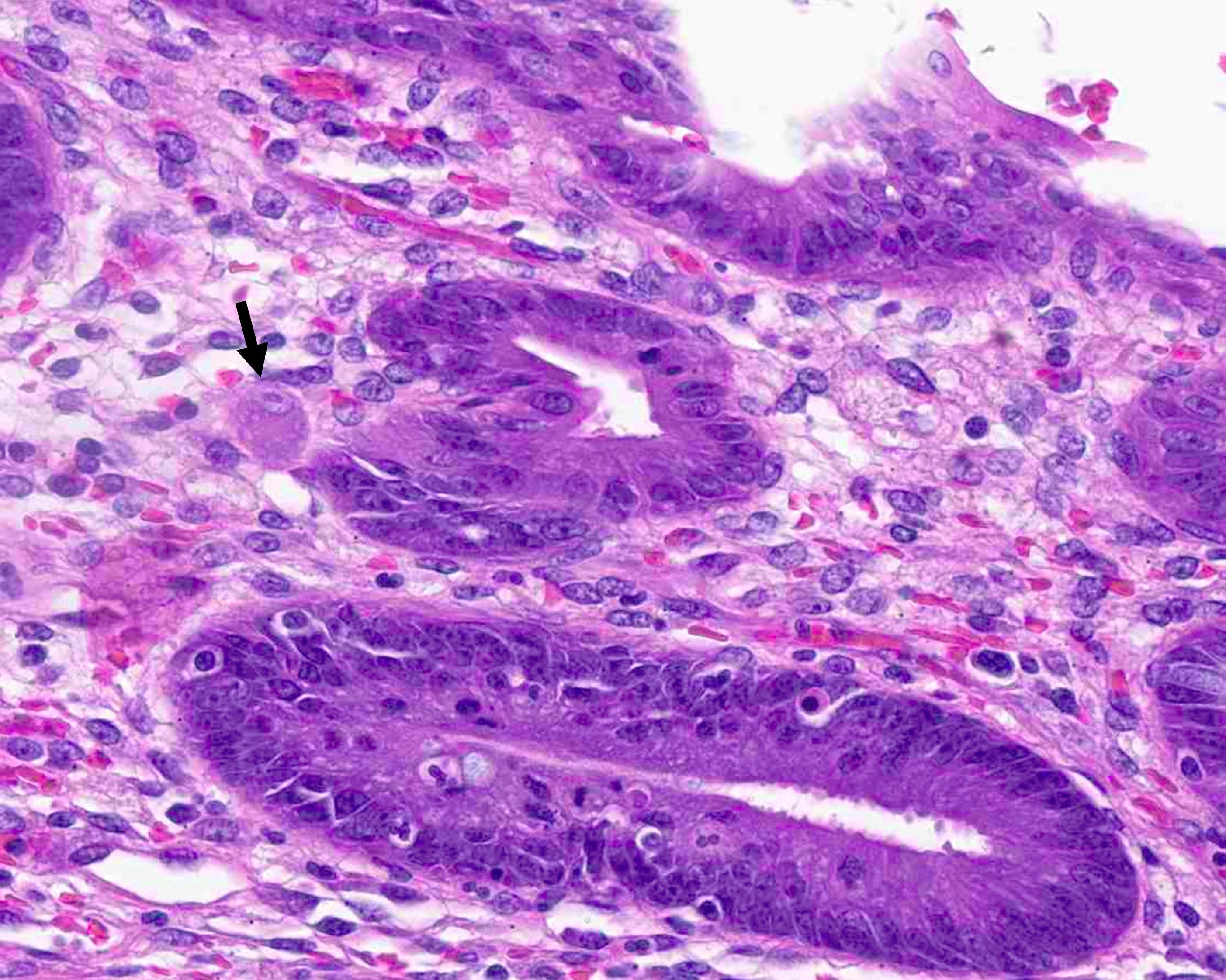
Microscopic (histologic) description
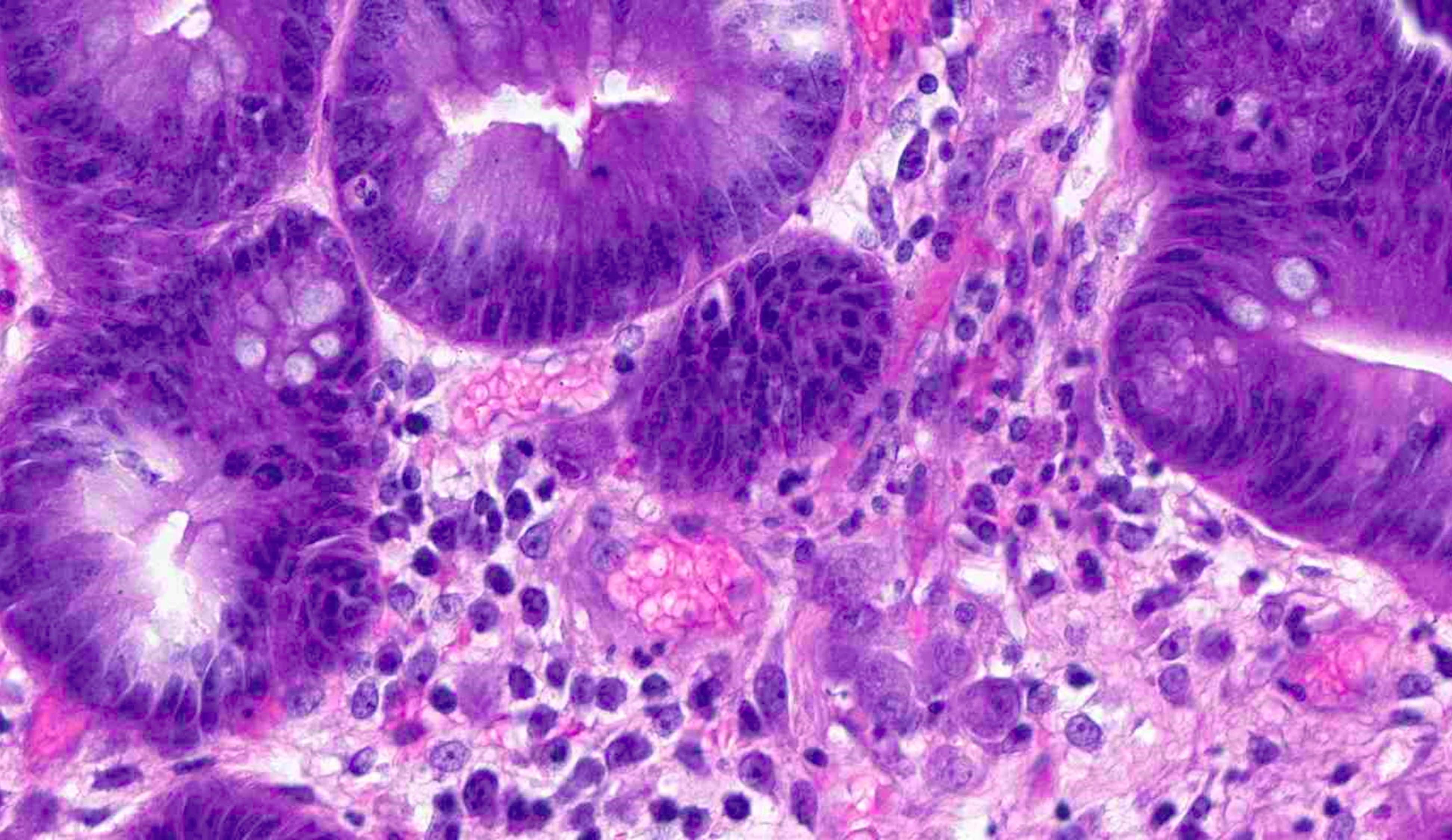
- Variably ulcerated appendiceal mucosa with a transmural mixed inflammatory infiltrate, including abundant neutrophils, histiocytes, plasma cells and lymphocytes
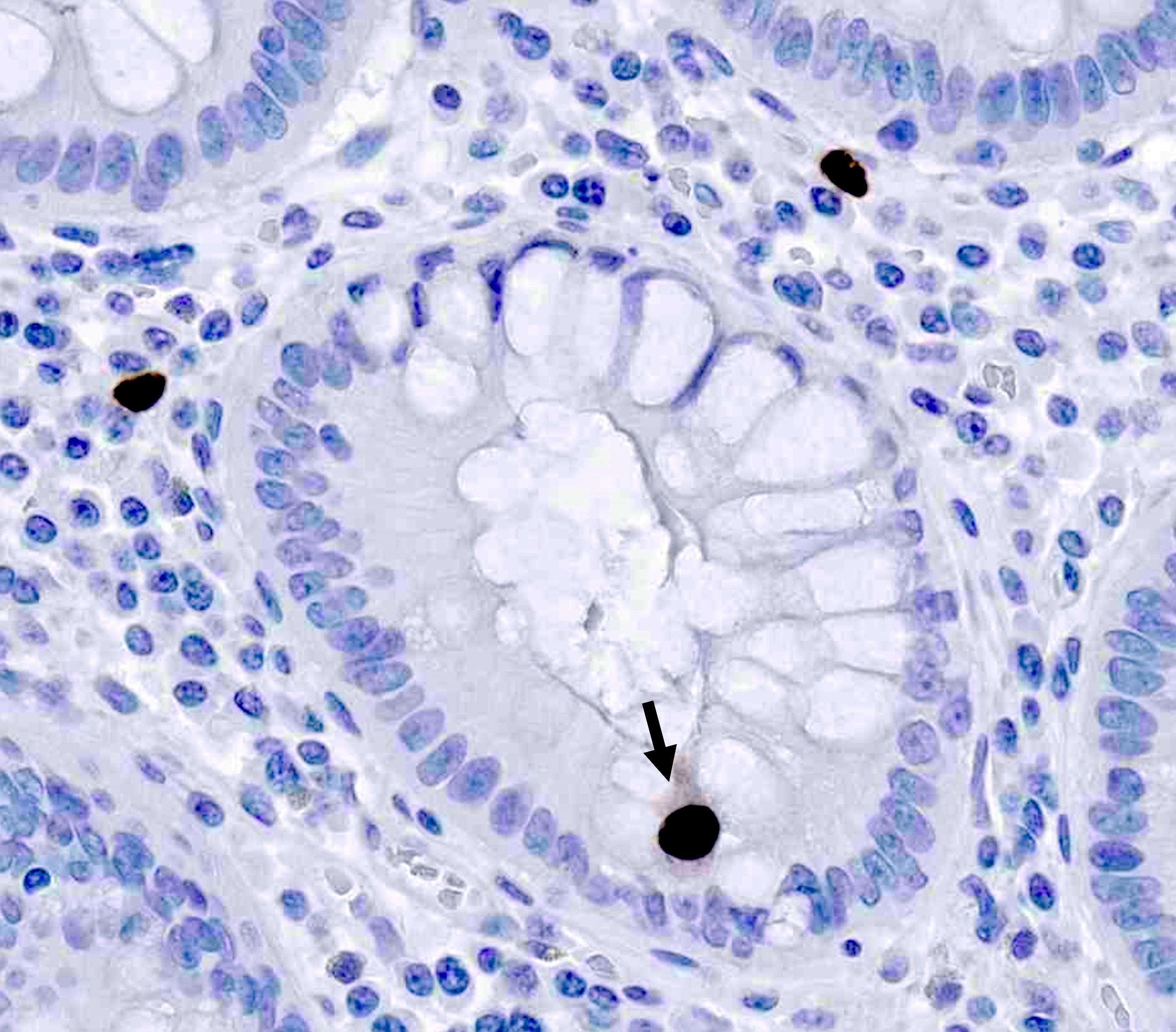
- Infected cells appear cytomegalic (enlarged 2 - 4 fold)
- Owl eye inclusions: targetoid, basophilic intranuclear inclusions (Cowdry bodies) surrounded by a clear halo
- Intracytoplasmic inclusions
- Reddish granules in cytoplasm
- Viral cytopathic changes may be found in endothelial, epithelial, histiocytic or stromal cells (Infect Dis Clin North Am 2010;24:995)
Microscopic (histologic) images
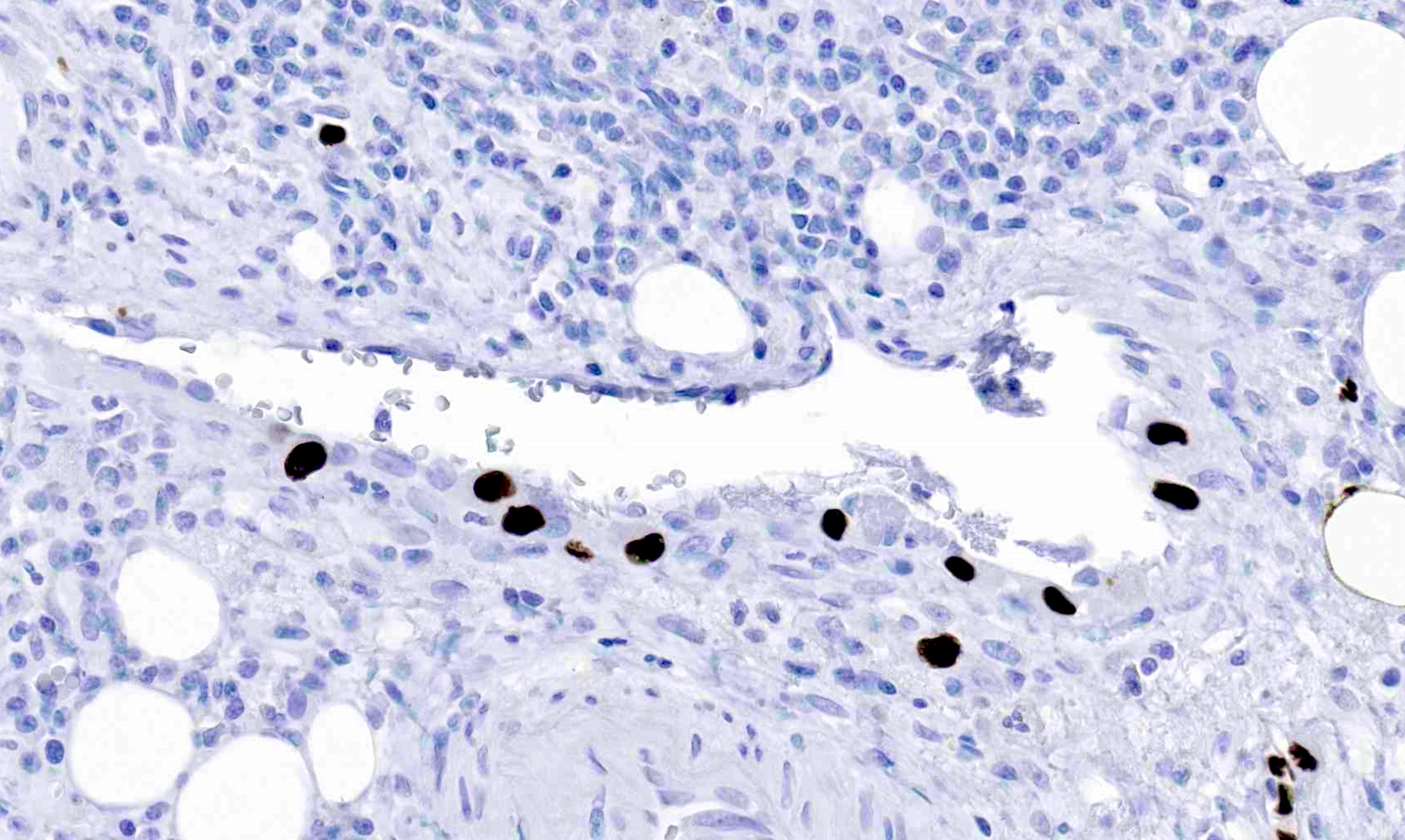
Positive stains
- Cytomegalovirus (CMV) immunohistochemistry
Negative stains
- Adenovirus immunohistochemistry
Sample pathology report
- Appendix, appendectomy:
- Acute appendicitis with numerous CMV infected cells (confirmed by positive CMV immunostain), consistent with CMV appendicitis
Differential diagnosis
- Adenovirus appendicitis:
- Viral inclusions are only intranuclear and show smudgy, crescent shaped appearance (smudge cells)
- Positive adenovirus immunostain
- Negative CMV immunostain
- Appendicitis related to other infectious etiology:
- Identification of other microorganisms; e.g., Entamoeba histolytica (flask shaped mucosal ulcers with foamy appearing amoebae containing ingested erythrocytes)
- Negative CMV immunostain
- Nonspecific acute appendicitis:
- Negative CMV immunostain
Board review style question #1
A 31 year old man presenting with right lower quadrant pain, fever and radiologic evidence of acute appendicitis undergoes appendectomy, which reveals the findings above. What is the most likely clinical risk factor?
- History of recent antibiotic use
- HIV infection
- Inflammatory bowel disease
- Trauma
- Travel outside the U.S.
Board review style answer #1
B. HIV infection. Immunocompromised states like HIV infection or history of solid organ transplantation are risk factors for CMV infection.
Answer D is incorrect because trauma is not a risk factor for CMV infection.
Answer A is incorrect because recent antibiotic use is not a risk factor for CMV infection, though may predispose other infections, such as C. difficile.
Answer C is incorrect because the patient's clinical presentation is not typical of inflammatory bowel disease (IBD), though patients with IBD may be at increased risk for CMV infection, particularly after steroid therapy.
Answer E is incorrect because travel outside the U.S. may predispose to certain infections (e.g., parasitic) but it is not a risk factor for CMV infection.
Comment Here
Reference: CMV appendicitis
Comment Here
Reference: CMV appendicitis
Board review style question #2
Which histologic feature is characteristic of CMV appendicitis?
- Intranuclear and intracytoplasmic inclusions
- Luminal amoebae with foamy cytoplasm and ingested erythrocytes
- Multinucleate Warthin-Finkeldey giant cells
- Rod shaped bacteria in the appendiceal lumen
- Smudgy, crescent shaped intranuclear inclusions (smudge cells)
Board review style answer #2
A. Intranuclear and intracytoplasmic inclusions. The presence of basophilic intranuclear inclusions (owl eye inclusions) and intracytoplasmic inclusions are characteristic of CMV infected cells.
Answer D is incorrect because rod shaped bacteria in the appendiceal lumen are nonspecific and may not be pathogenic.
Answer E is incorrect because these features are typical of adenovirus infection.
Answer B is incorrect because these features are typical of Entamoeba histolytica infection.
Answer C is incorrect because these features are typical of measles (rubeola virus) infection.
Comment Here
Reference: CMV appendicitis
Comment Here
Reference: CMV appendicitis