Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Parakh R, Tretiakova M. Urachal adenocarcinoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderadenourachal.html. Accessed August 26th, 2025.
Definition / general
- Adenocarcinoma arising from the epithelium lined tubular structure known as urachus, an embryological derivative of the urogenital sinus and allantois that connects the bladder to the umbilicus
- Diagnosis of urachal adenocarcinoma is usually established after excluding other mimics
Essential features
- Criteria for urachal origin of adenocarcinoma
- Centered in the anterior wall or dome of bladder
- Predominant invasion of muscularis or deeper tissues with sharp demarcation between tumor and surface bladder urothelium
- Surface urothelium is free of carcinoma in situ or glandular metaplasia or cystitis glandularis
- Presence of urachal remnants is helpful but not always identifiable
- No primary adenocarcinoma elsewhere confirmed clinically
Terminology
- Some authors prefer terminology of median umbilical ligament for completely regressed involuted urachus (fibrous cord-like structure) and reserve urachus for the patent urachus (tube-like structure lined by urothelium)
ICD coding
- ICD-10: C67.7 - malignant neoplasm of urachus
Epidemiology
- Rare, < 1 case per 1 million of population
- 10 - 30% of bladder adenocarcinomas, 0.2 - 0.3% of all bladder cancers (J Urol 2012;188:1102, Rare Tumors 2016;8:6257)
- Age: fifth to sixth decade (younger than nonurachal adenocarcinomas; median age 52 - 56 versus 69 years) (Cancer 2006;107:721, Urol Oncol 2016;34:388)
- M:F = 2:1 (Dis Markers 2018;2018:7308168)
Sites
- Usually dome of bladder, occasionally anterior wall of bladder (intramural mass)
Pathophysiology
- The urachus lies in the space of Retzius, a space anterior to the peritoneum between the layers of umbilicovesical fascia (see Urachus)
- Involution usually happens before birth (by the fourth month of fetal life) and the urachus becomes a fibrous cord known as the median umbilical ligament
- In adults, it is usually 5 cm long and 6 mm broad
- It can be divided into supravesical, intramural and intramucosal segments
- Persistent remnant is a relatively normal condition found in 25 - 35% of bladders at the time of autopsy (J Urol 1982;127:40)
- Persistent remnants of the allantois develop into cysts or epithelial neoplasms; not all neoplasms are glandular (see Urachus) (Urology 1985;26:218)
- Among urachal epithelial neoplasms, 80% are adenocarcinomas with enteric features and are mucinous (J Urol 1986;135:1240, Cancer 1991;67:2165)
Etiology
- Embryologic derivative undergoing neoplastic transformation (J Urol 1984;131:1)
- Risk factors include bladder exstrophy and urachal anomalies
Clinical features
- Hematuria and irritative bladder symptoms with voiding difficulties (hematuria, dysuria, nocturia, frequency, suprapubic pain) (Cancer 2006;107:712, Urol Oncol 2016;34:388)
- Rare mucusuria (associated with villous morphology and connection with bladder lumen) (J Urol 1986;135:1240)
Diagnosis
- Urachal adenocarcinoma is a clinicopathologic diagnosis
- Clinical confirmation of location of mass and presence of urachal remnant
- Radiologic and colonoscopic exclusion of extension (colorectal, prostatic and gynecologic) or metastasis (hematogenous) from another organ (breast, pancreas, gastric and pulmonary)
- Reference: Urol Oncol 2016;34:388
Radiology description
- Cystoscopy: usually single, solid irregularity / nodularity in the dome / anterior wall
- Ultrasound findings
- Uneven internal echogenicity with involvement of anterior bladder wall / dome
- Solid / cystic mass, with or without calcification
- Computed tomography (CT) findings
- Solid / cystic mass and punctate calcification
- Thickened bladder dome and anterior wall and urachal area
- For staging and assessment of muscle invasion
- Magnetic resonance imaging (MRI): for staging
- References: J Clin Pathol 2006;59:1091, Indian J Med Res 2013;137:398
Radiology images
Prognostic factors
- Since the entire length of the median umbilical ligament may harbor urachal remnants and carcinoma may present in perivesical tissue, staging is different than bladder carcinoma
- Staging of urachal carcinoma has reduction in substages (applied to invasion of the bladder wall) and management differs according to the pathologic stage at the time of surgery (Hum Pathol 1996;27:240)
- First staging proposed by Sheldon (J Urol 1984;131:1, Urol Oncol 2016;34:388)
- I: confined to urachal mucosa (in situ)
- II: urachus invasion confined to urachus itself
- III: local extension
- Bladder (IIIA)
- Abdominal wall (IIIB)
- Peritoneum (IIIC)
- Other viscera (IIID)
- IV
- Metastasis to regional lymph nodes (IVA)
- Distant sites (IVB)
- Local recurrence and metastatic disease are common (J Urol 2007;178:74, Cancer 2006;107:712)
- 5 year cancer specific survival rate is ~50% (median ~45 months, significantly longer than bladder urothelial carcinoma) (Cancer 2006;107:712, Hum Pathol 2015;46:1808, J Urol 2006;175:2042, Dis Markers 2018;2018:7308168)
- In Sheldon classification, > 80% patients presented in stage III (bladder invasion) with 5 year survival rate from 25 - 61% (J Urol 1984;131:1, Urol Oncol 2016;34:388)
- Mayo and Ontario staging systems simplify the Sheldon staging using larger dataset (2006) (Cancer 2006;107:712, J Urol 2006;175:2042)
- In the Mayo system
- Bladder mucosa and muscularis propria invasion are stage II instead of III
- Regional lymph node involvement is stage III instead of IVA
- Distant metastasis is stage IV instead of IVB
- In 2023, a new TNM staging system was proposed based on the 626 cases included in Surveillance, Epidemiology, and End Results (SEER) database as follows (Cancer Med 2023;12:2752)
- Stage I
- pT0, Ta, Tis (confined to urachal mucosa)
- N0, M0
- Stage II
- pT2, pT3a (invasion of bladder muscularis propria or microscopic invasion of perivesical tissue)
- N0, M0
- Stage III
- pT3b, 4a (macroscopic invasion of bladder perivesical tissue or invasion of uterus, vagina, prostate)
- N0, M0
- Stage IV
- pT4b (invasion of pelvic wall, abdominal wall or peritoneum)
- Any nodal involvement or distant metastasis regardless of pT category
- Stage I
- Staging systems have prognostic utility but lack validation because of the overall smaller sample size due to disease rarity (Cancer Med 2023;12:2752, Hum Pathol 2015;46:1808)
Case reports
- 30 year old woman with vertebral metastasis (Arch Pathol Lab Med 2004;128:1043)
- 49 year old man with primary urachal signet ring cell carcinoma (Front Oncol 2022;12:1034245)
- 54 year old man with in situ adenocarcinoma of the urachus arising in a giant urachal cyst and associated pseudomyxoma peritonei (J Clin Pathol 2003;56:152)
- 55 year old man with enteric type tumor (Can J Urol 2009;16:4753)
- 70 year old patient with malignant transformation of urachal cyst (J Cancer Res Ther 2022;18:291)
Treatment
- Umbilectomy with partial cystectomy, possibly laparoscopic (Clinics (Sao Paulo) 2008;63:731)
- Since the entire length of median umbilical ligament may harbor urachal remnants, which may develop carcinoma synchronously or metachronously, the surgery of choice includes en bloc resection of the entire length of the ligament with umbilectomy with negative margins
- Adjuvant treatment given depending on the stage includes chemoradiation
Clinical images
Gross description
- Firm, white-gray mass with epicenter in the anterior wall or dome of bladder with urachal tract
- Usually lacks intraluminal mass or surface mucosal changes
- Could be cystic with abundant mucin production (Am J Surg Pathol 2014;38:1033)
- Ulceration with previous biopsy site or if endophytic growth (Am J Surg Pathol 2012;36:432)
- Median size is 6 - 7 cm (Dis Markers 2018;2018:7308168)
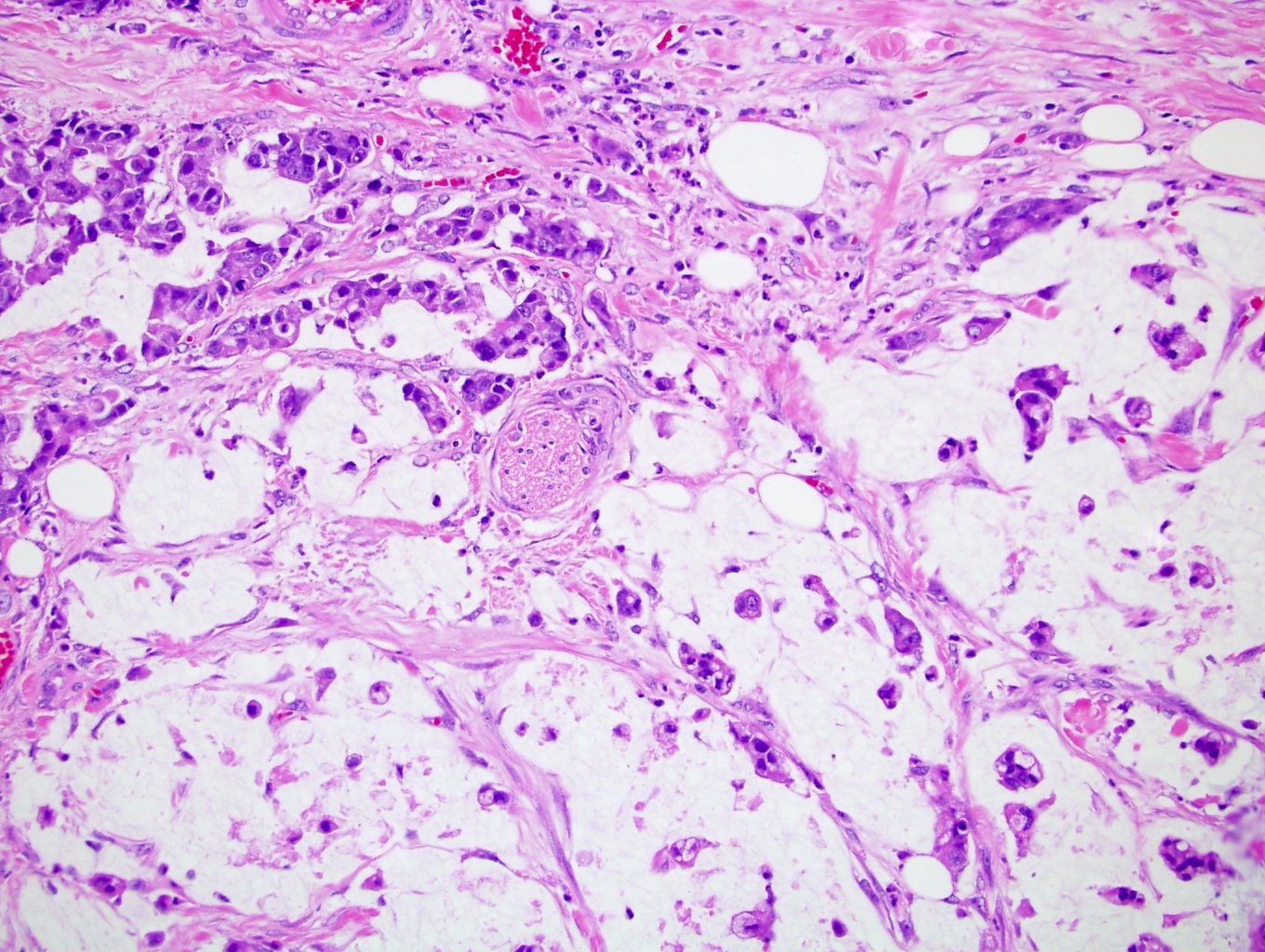
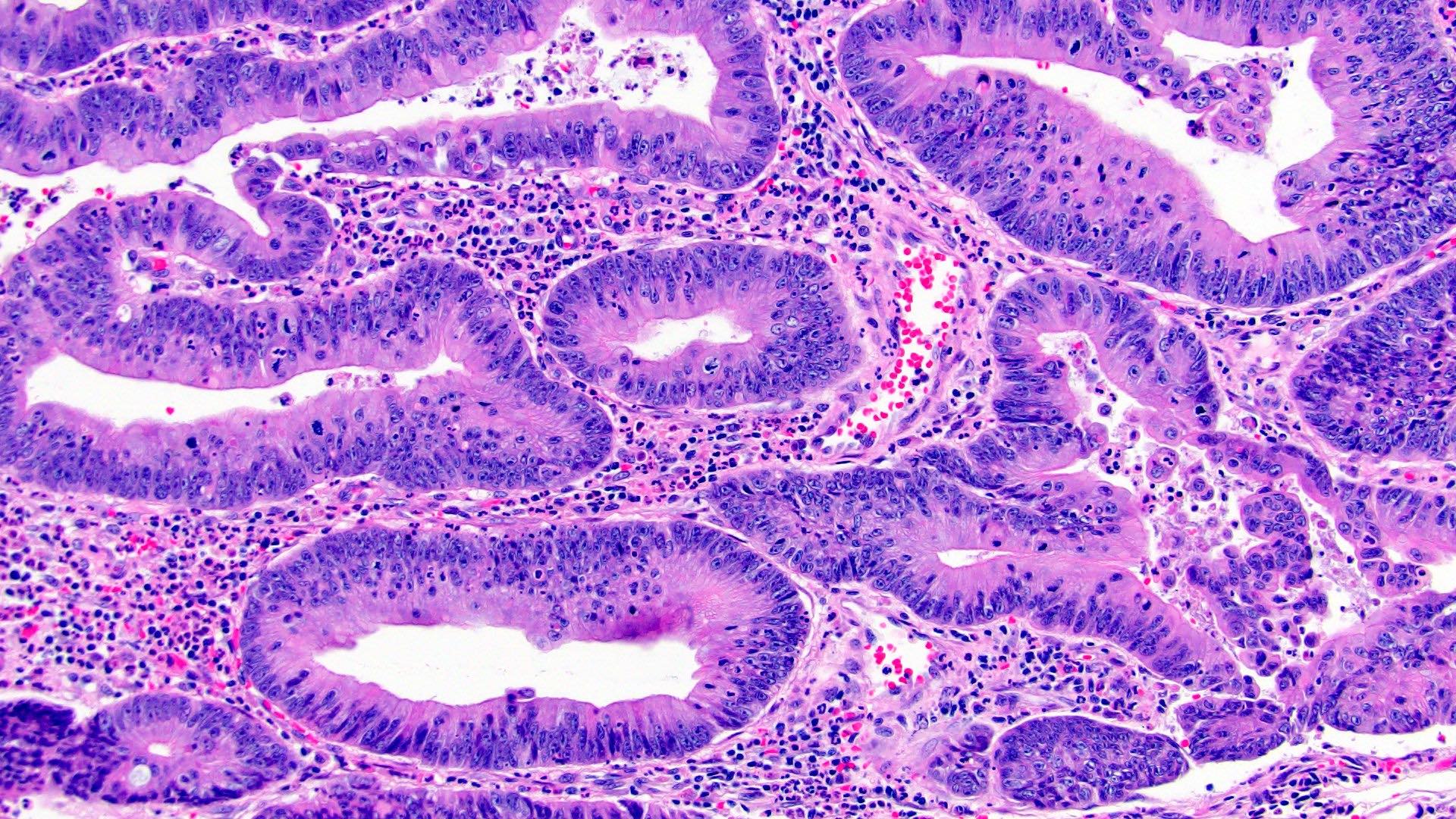
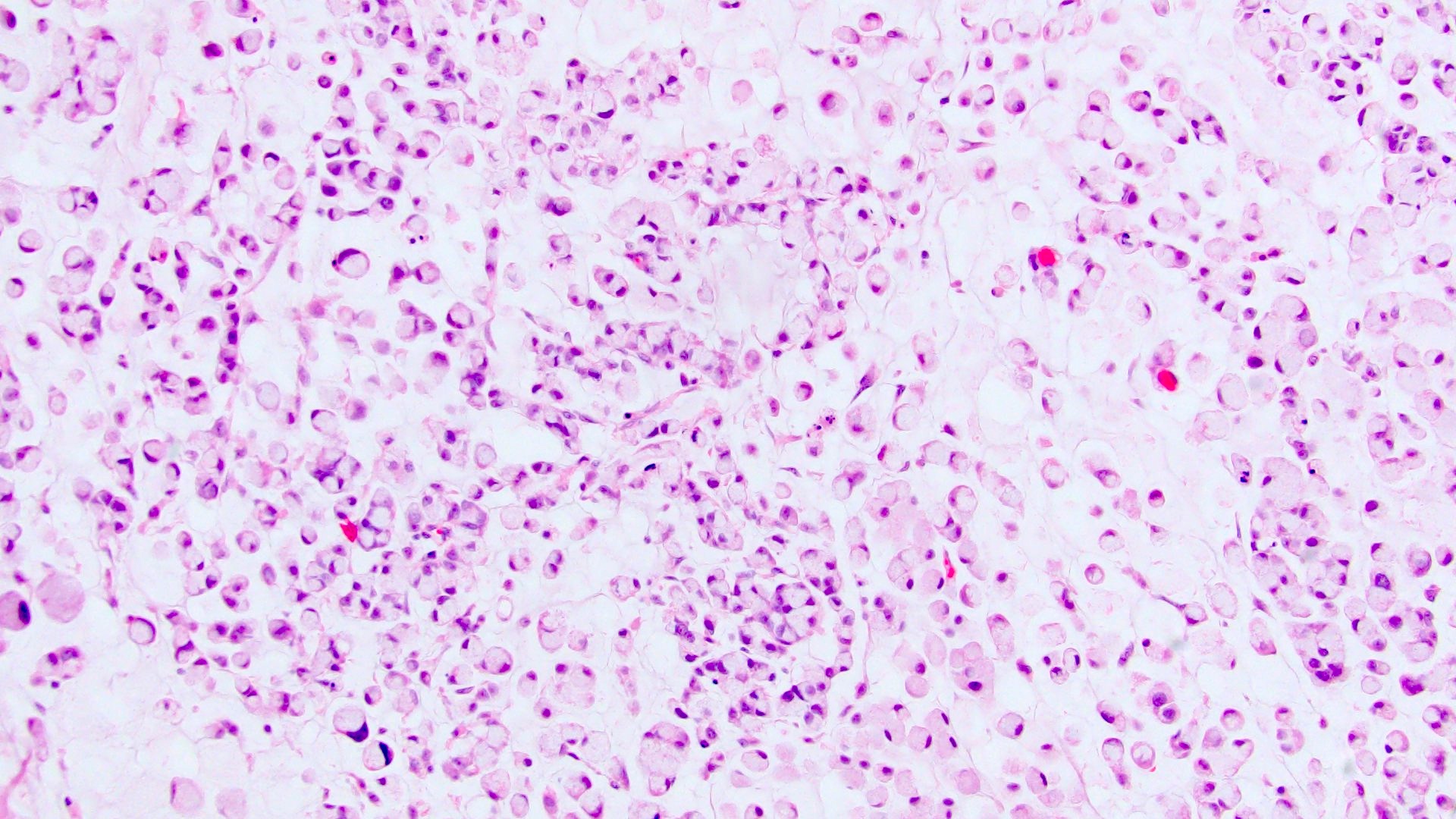
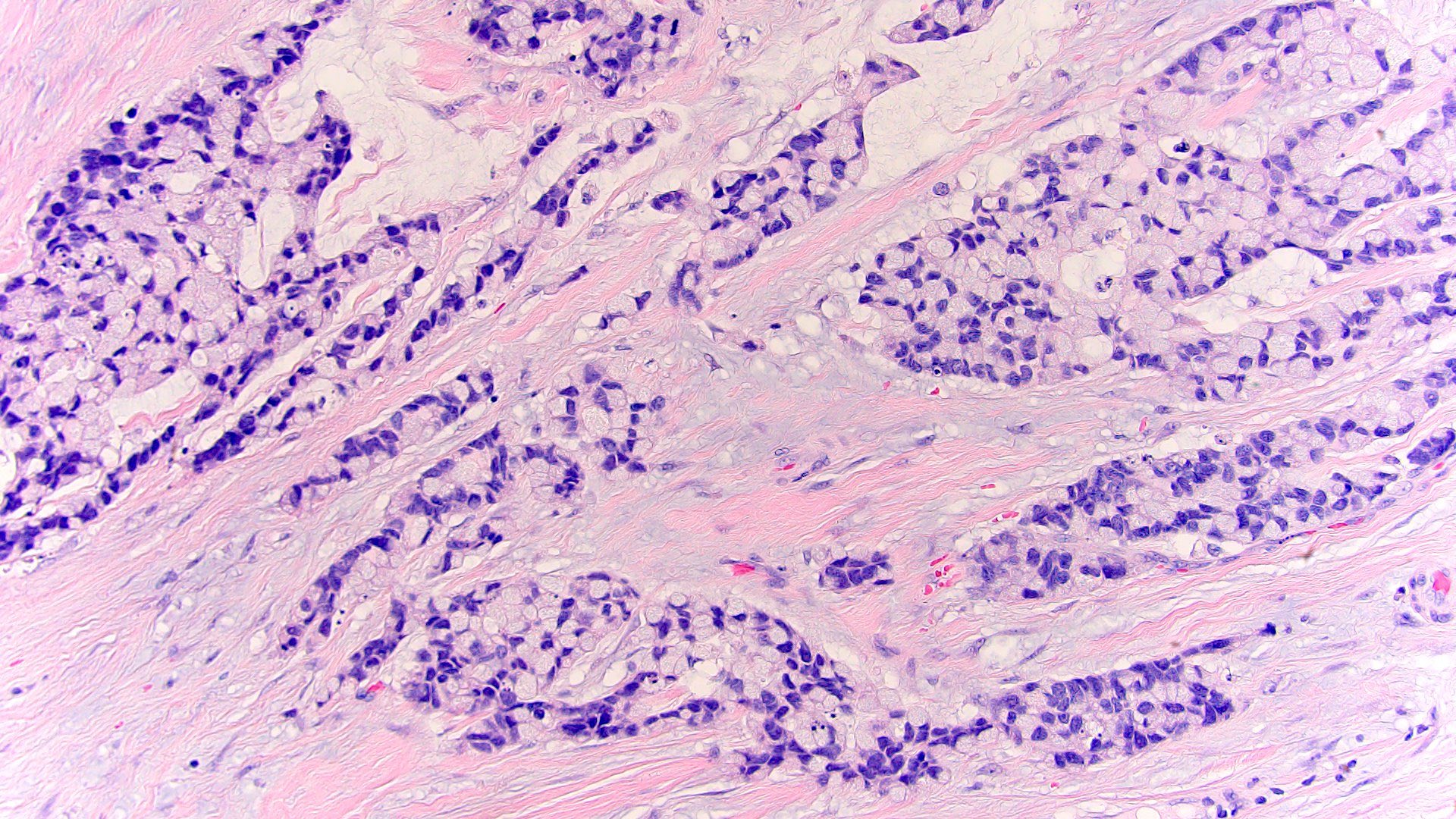
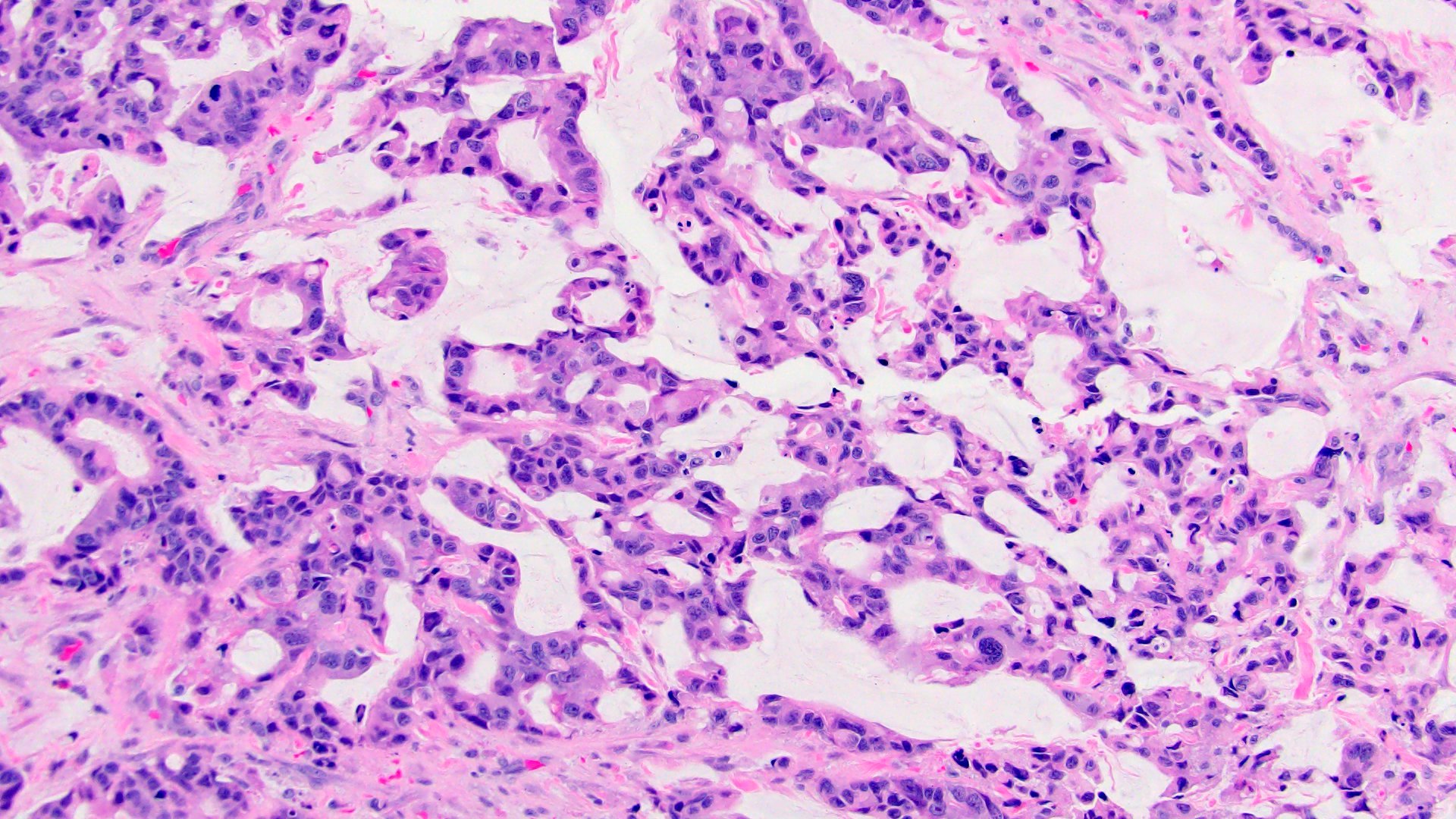
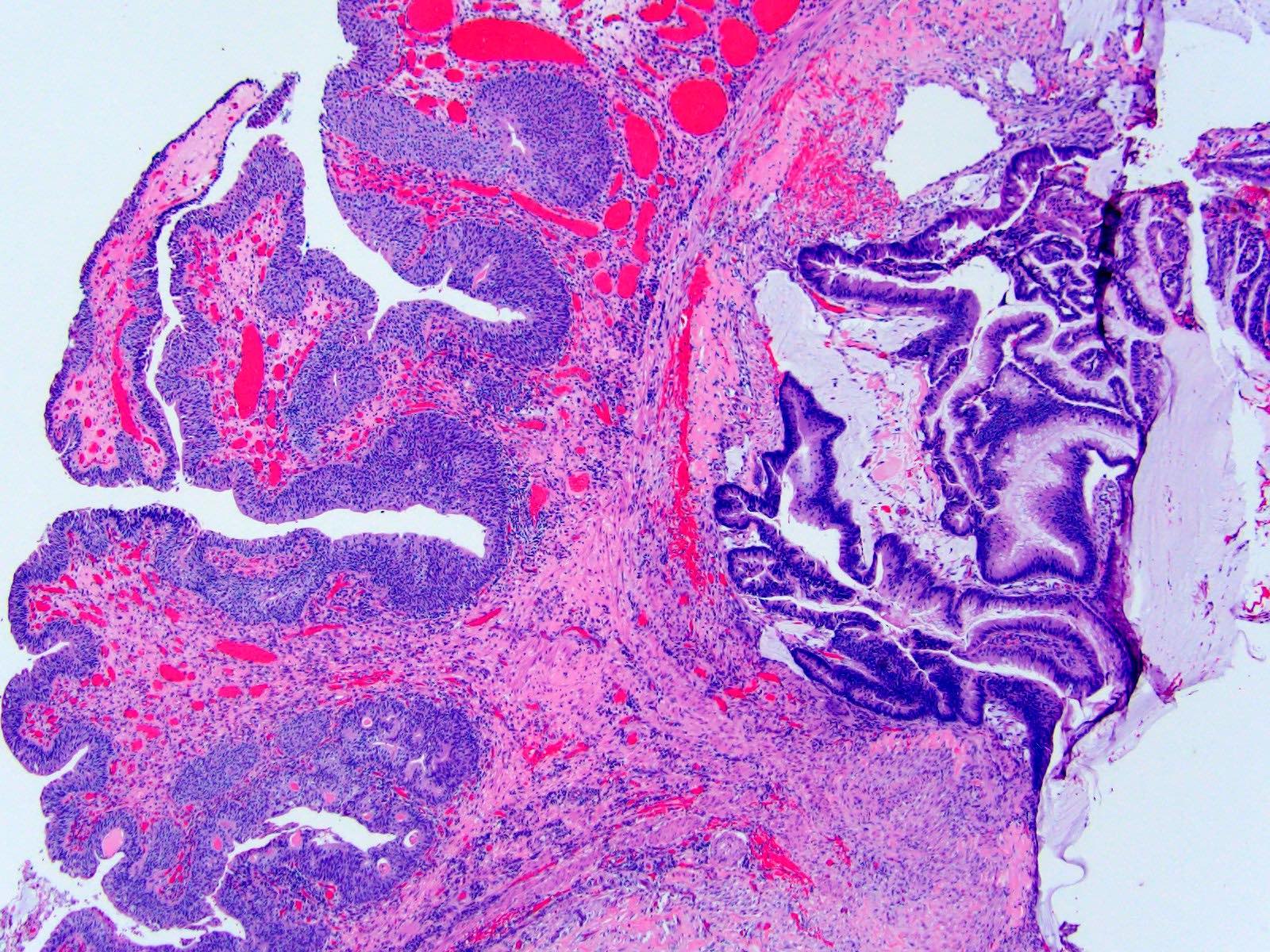
Microscopic (histologic) description
- Arises from intramural portion of urachus, grows into bladder wall, lacks mucosal involvement, is sharply demarcated from normal epithelium and lacks intestinal metaplasia
- Most tumors are well differentiated adenocarcinomas with histologic variations of mucinous / colloid (57%), enteric (15%), signet ring (6%), mixed morphology (8%) or nonspecific / NOS (14%) (Dis Markers 2018;2018:7308168)
- Mucinous neoplasms are predominant
- Mucinous cystic tumors form a spectrum from cystadenoma to mucinous cystic tumors of low malignant potential to microinvasive and frankly invasive cystadenocarcinomas similar to other organs (i.e., appendix, ovary) (Am J Surg Pathol 2014;38:1033)
- Residual benign urachal remnants can be intermingled with carcinoma and harbor preinvasive lesions
- Enteric subtype is morphologically identical to colorectal primary carcinomas
- Signet ring subtype is characterized by infiltrative stromal growth of signet ring cells
- < 5% of cases present with other malignant epithelial neoplastic morphology such as usual urothelial, squamous cell carcinoma and neuroendocrine (Adv Anat Pathol 2016;23:71)
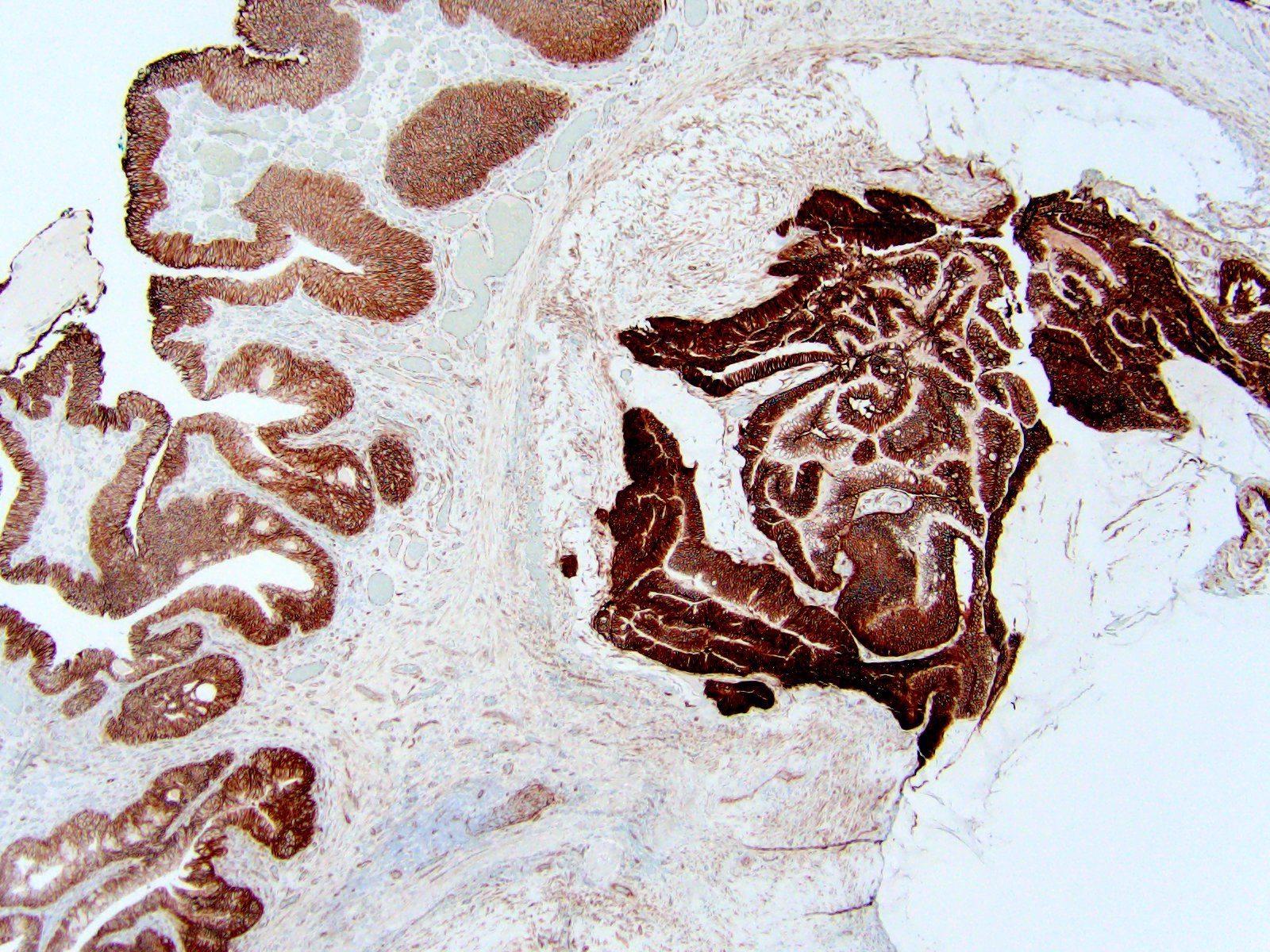
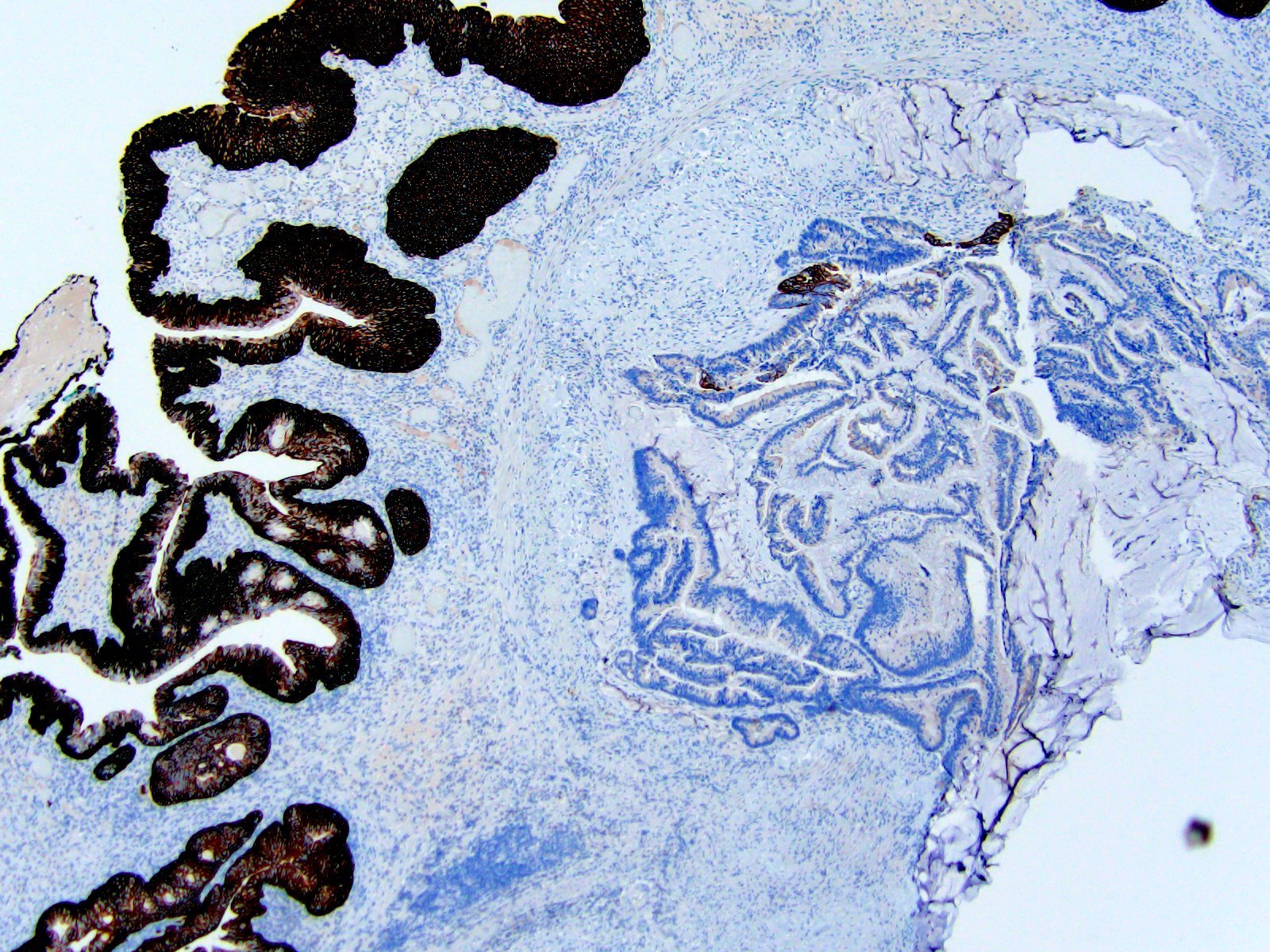
Microscopic (histologic) images
Contributed by Maria Tretiakova, M.D., Ph.D.
Cytology description
- Cytomorphology differs according to type of adenocarcinoma (e.g., mucinous versus signet ring)
- Cluster of cells with eccentric irregular nuclei; prominent nucleoli and vacuolated cytoplasm
- Background may show mucin (Cancer 1998;84:335, J Clin Diagn Res 2016;10:ED10)
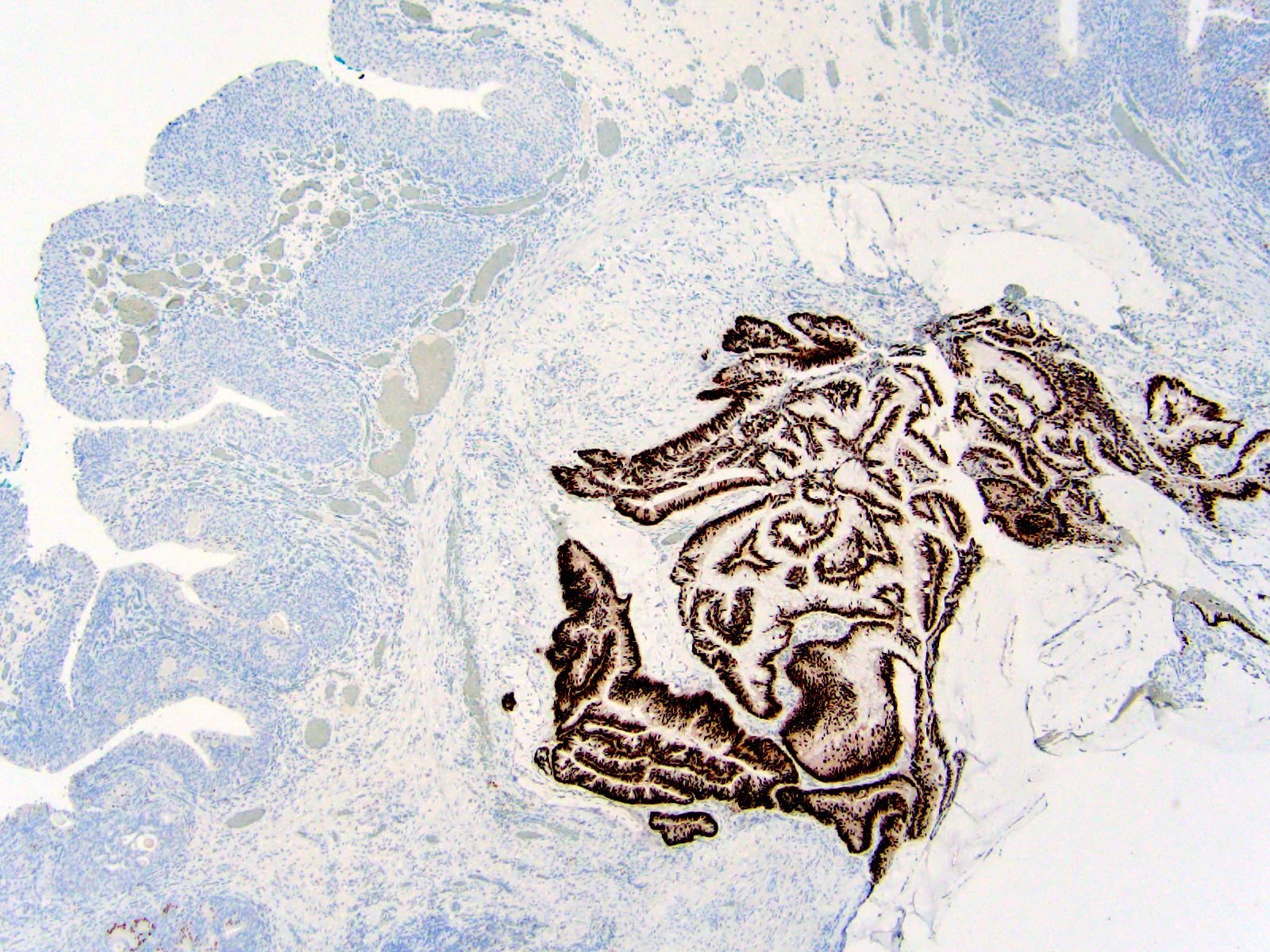
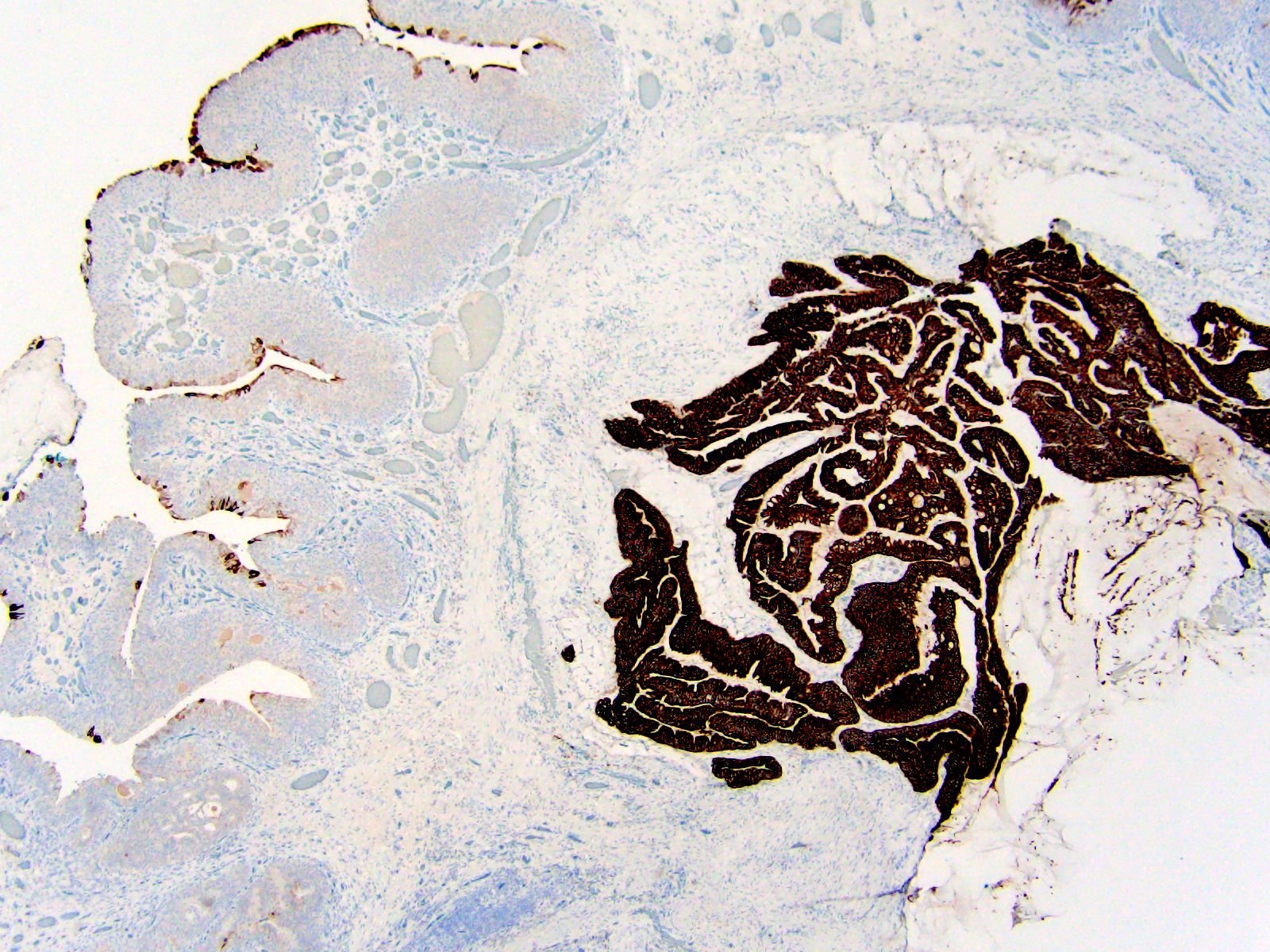
Positive stains
- CK20, CDX2, CK7, high molecular weight keratin, CD15, CEA (Am J Surg Pathol 2011;35:787, Dis Markers 2018;2018:7308168)
- CK7 is more frequent (~50%) than in colonic primary
- High molecular weight keratin is the most useful marker to differentiate from negative colonic primary
Negative stains
- Nuclear beta catenin is the most useful marker to distinguish from colonic primary which is positive (Am J Surg Pathol 2011;35:787, Dis Markers 2018;2018:7308168, Pathol Oncol Res 2020;26:2773)
- AMACR (p504) may be useful to distinguish from primary bladder adenocarcinoma and colonic primary that are both positive (Dis Markers 2018;2018:7308168)
- GATA3 may be useful to distinguish from primary bladder carcinoma with glandular differentiation
Electron microscopy description
- Ultrastructurally, by transmission and scanning electron microscopy, the tissue resembles gut mucosa (J Urol 1986;135:1240)
Molecular / cytogenetics description
- Bladder and urachal adenocarcinoma genomic profiles resemble colorectal adenocarcinoma with frequent TP53, KRAS, BRAF, NRAS and PIK3CA alterations (JCO Precis Oncol 2022;6:e2100392, Oncotarget 2016;7:39293)
- Although mutation profiles of bladder and urachal adenocarcinoma overlap, their differences may aid in separating these 2 entities (Int J Surg Pathol 2020;28:51)
- Mutations of GNAS, SMAD4 and BRAF are found in urachal but not bladder adenocarcinomas
- The most common recurrent somatic mutations of urachal carcinomas involve 6 genes: APC, COL5A1, KIF26B, LRP1B, SMAD4 and TP53 (J Med Genet 2017;54:572)
- MicroRNA expression profiling does not show distinct pattern of the main morphologic subtypes (Hum Pathol 2013;44:1605)
- Extent of chromosomal amplification is highly associated with the patient's cancer stage; 35% of focal DNA amplifications were in fibroblast growth factor receptor family genes (J Med Genet 2017;54:572)
Videos
Mini tutorial of urachal tumors
Urachal adenocarcinoma diagnosis and treatment
Sample pathology report
- Dome of bladder, biopsy:
- Adenocarcinoma, NOS (see comment)
- Comment: Given the presence of surface ulceration, an in situ component cannot be evaluated. A possibility of adenocarcinoma of urachal origin is favored at this site although adenocarcinoma of bladder origin is also a consideration. Negative beta catenin nuclear positivity and clinical information confirms that there is no metastasis or direct extension from another organ.
Differential diagnosis
- Local extension of colonic or other adenocarcinoma:
- Clinical history, radiological and endoscopic investigation are important
- Diffuse nuclear immunoreactivity for beta catenin suggests nonurachal colorectal carcinoma; diffuse positivity for 34 beta E12 supports urachal carcinoma (Am J Surg Pathol 2009;33:659, Adv Anat Pathol 2016;23:71)
- Metastatic adenocarcinoma:
- Clinical history is important
- Nonurachal primary adenocarcinoma of bladder:
- Usually posterior wall or trigone
- Intraluminal mass, carcinoma in situ or extensive glandular metaplasia of adjacent urothelium
- Invasive urothelial carcinoma with glandular differentiation:
- Usual urothelial carcinoma with urothelial carcinoma in situ is noted in the vicinity
- Positive urothelial markers (e.g., uroplakin II, S100P, p63 and GATA3)
- Villous adenoma:
- Noninvasive
Additional references
Practice question #1
The photomicrograph depicts urachal adenocarcinoma. Which of the following is the most important criterion for the diagnosis of urachal adenocarcinoma?
- Beta catenin nuclear positivity on immunohistochemistry
- Intraluminal mass in posterior wall
- Intramural mass in dome or anterior wall
- Presence of carcinoma in situ in mucosal lining
Practice answer #1
C. Intramural mass in dome or anterior wall. Considering the embryologic aspect, the most important criterion for urachal origin is the presence of an intramural mass in the dome or anterior bladder wall. Answers B and D are incorrect because lack of intraluminal mass and absence of carcinoma in situ favor urachal origin over primary bladder origin. Answer A is incorrect because nuclear beta catenin is often positive in colonic adenocarcinoma, which may extend or metastasize in rare cases and excludes urachal origin.
Comment Here
Reference: Urachal adenocarcinoma
Comment Here
Reference: Urachal adenocarcinoma
Practice question #2
What is the importance of diagnosing primary urachal origin in a malignant glandular neoplasm of the bladder and perivesical area?
- Familial predisposition
- It arises from embryologic remnant
- Rarity of disease representing scientific curiosity
- Staging and management are different than bladder primary
Practice answer #2
D. Staging and management are different than that of primary adenocarcinoma of the bladder. The urachus is a fibrous cord extending from the bladder wall to the umbilicus; along the free surface of the bladder urachus, carcinoma is frequently amenable to partial cystectomy if it presents as a solitary mass. The entire tract of median umbilical ligament must be excised. Staging of urachal carcinoma differs from those that arise from the bladder surface. Most urachal carcinomas (80%) present at advanced stages but are still associated with a better survival rate than bladder urothelial carcinomas (Hum Pathol 2015;46:1808). Answer A is incorrect because no familial predisposition has been described.
Comment Here
Reference: Urachal adenocarcinoma
Comment Here
Reference: Urachal adenocarcinoma