Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Prognostic factors | Case reports | Treatment | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Gandhi JS. Nephrogenic metaplasia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladdernephroadenoma.html. Accessed April 19th, 2024.
Definition / general
- Nonneoplastic localized or diffuse, papillary, tubular or cystic metaplastic changes of the urothelium in response to chronic infection, calculi, injury or prolonged catheterization
- Characterized by a single layer of cuboidal or hobnail epithelial cells with clear or eosinophilic cytoplasm and small, discrete nuclei without prominent nucleoli
- First described by Davis in 1949; Friedman and Kuhlenbeck coined the term nephrogenic adenoma in 1950 (Northwest Med 1949;48:182, J Urol 1950;64:657)
Essential features
- Nonneoplastic reactive metaplastic lesion with tubular, glandular, papillary or cystic architecture and surrounded (at least focally) by thick basement membrane
- Most cases confined to lamina propria
- May mimic urothelial carcinoma, clear cell or prostatic adenocarcinoma
Terminology
- Also called nephrogenic adenoma, mesonephroid metaplasia, adenomatous metaplasia
ICD coding
- ICD-10: N32.9 - bladder disorder, unspecified
Epidemiology
- M:F = 2 - 3:1
- Age range: 4 - 81 years
- Common in adults; approximately 10% may be observed in children (Arch Pathol Lab Med 2010;134:1455, Diagn Pathol 2015;10:104)
Sites
- Most commonly seen in the bladder neck and trigone (80%) but may occur in the urethra (12%) and ureter (8%) (Arch Pathol Lab Med 2010;134:1455)
- More common at bladder neck, trigone and adjacent urethra
Etiology
- Commonly appears to be metaplastic and associated with secondary urothelial injury, such as past surgery (60%), calculi (14%) or trauma including chronic catheterization (9%) and urinary tract infection (Hum Pathol 1981;12:907)
- ~8% associated with prior renal transplant recipients, supporting seeding / exfoliation of renal tubular cells in the urinary tract (N Engl J Med 2002;347:653, J Urol 1988;139:45)
- Less commonly associated with intravesical therapy for urothelial carcinomas (bacillus Calmette-Guérin (BCG), thiotepa, etc.), NSAID use, diverticulum, exstrophy, interstitial cystitis, malakoplakia
Clinical features
- Usually asymptomatic and incidental microscopic finding (Br J Urol 1997;80:539)
- Rare cases may present with obstructive features, bladder irritation or hematuria (Pediatr Surg Int 2008;24:605, Br J Urol 1997;80:539)
- Cystoscopy may have a friable and velvety appearance or a papillary / polypoid appearance mimicking a urothelial neoplasm (Urol Case Rep 2020;33:101382, J Pediatr Urol 2006;2:323)
Diagnosis
- Made on histopathological evaluation
Prognostic factors
- Nonneoplastic lesion with a propensity for recurrences
- Occasional cases with worrisome features may require resampling / frequent surveillances
- Rare case reports progressing to clear cell adenocarcinoma (Hum Pathol 2006;37:117, Curr Urol 2012;6:106)
Case reports
- 33 year old man with long term follow up following kidney transplantation (Case Rep Transplant 2020;2020:8831966)
- 67 year old man following laser therapy of benign prostatic hyperplasia (Urol Case Rep 2020;33:101382)
- 79 year old man presenting with a fibromyxoid nephrogenic metaplasia of the ureter (J Endourol Case Rep 2018;4:97)
Treatment
- Transurethral resection of the lesion and fulguration of tumor base in symptomatic cases
- Individual case reports treated by intravesical sodium hyaluronate (Urol Ann 2020;12:187, J Pediatr Urol 2007;3:156)
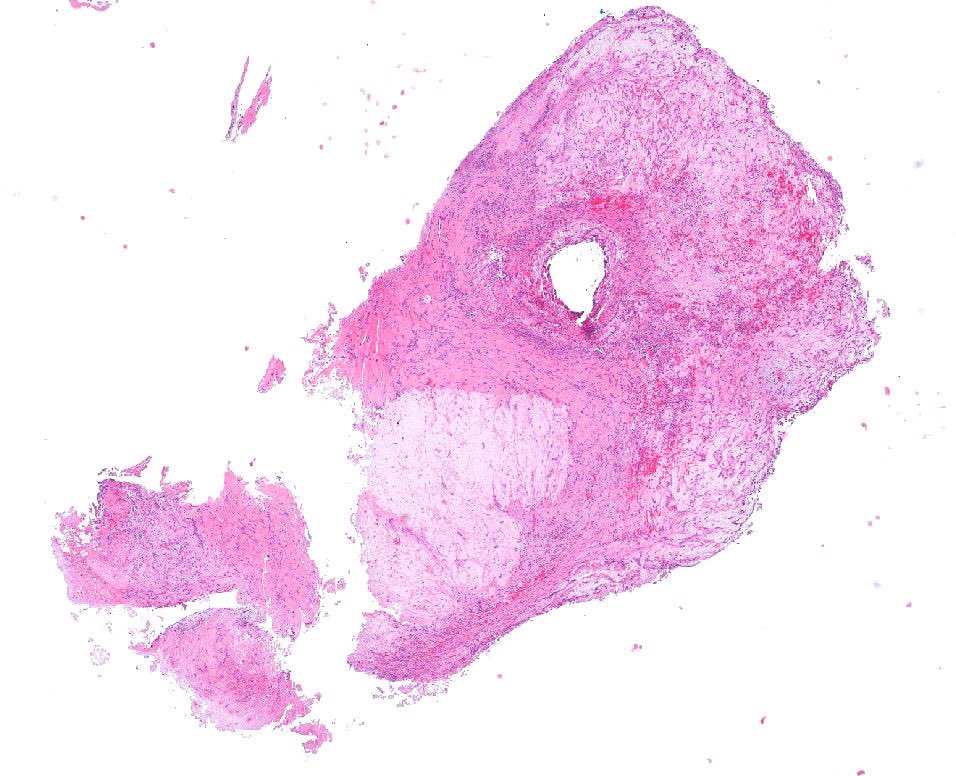
Gross description
- May be papillary (56%), polypoid (10%), fungating or sessile (10%) lesions (Arch Pathol Lab Med 2010;134:1455)
- Most (62%) are small lesions (1 cm), although rarely may be as large as 7 cm
- Multiple (~18 - 20%) and large, especially in the setting of end stage renal disease (Adv Anat Pathol 2006;13:247)
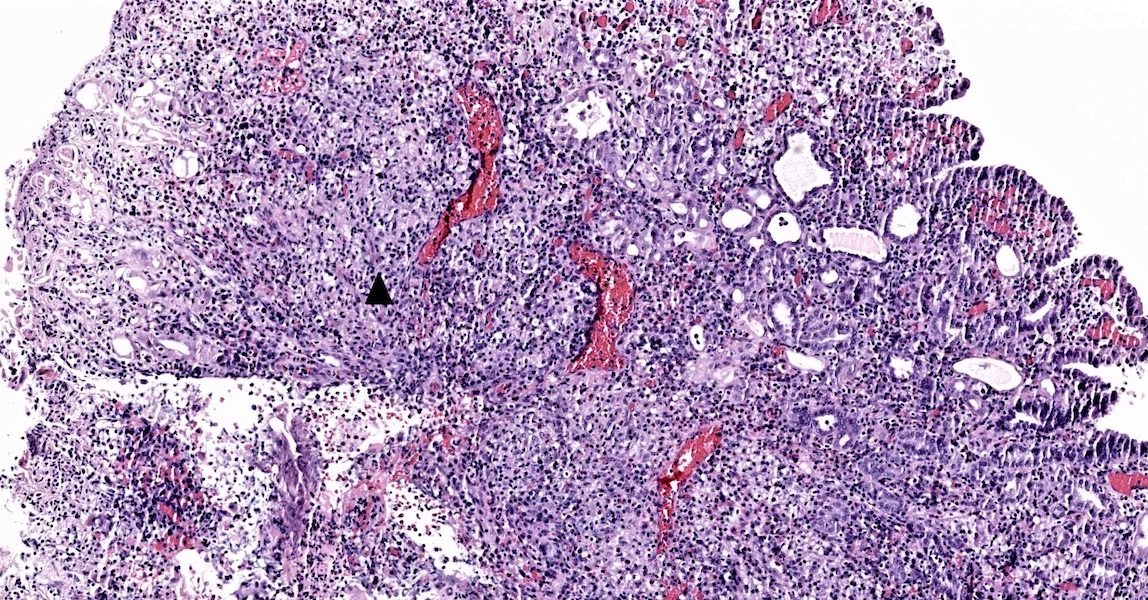
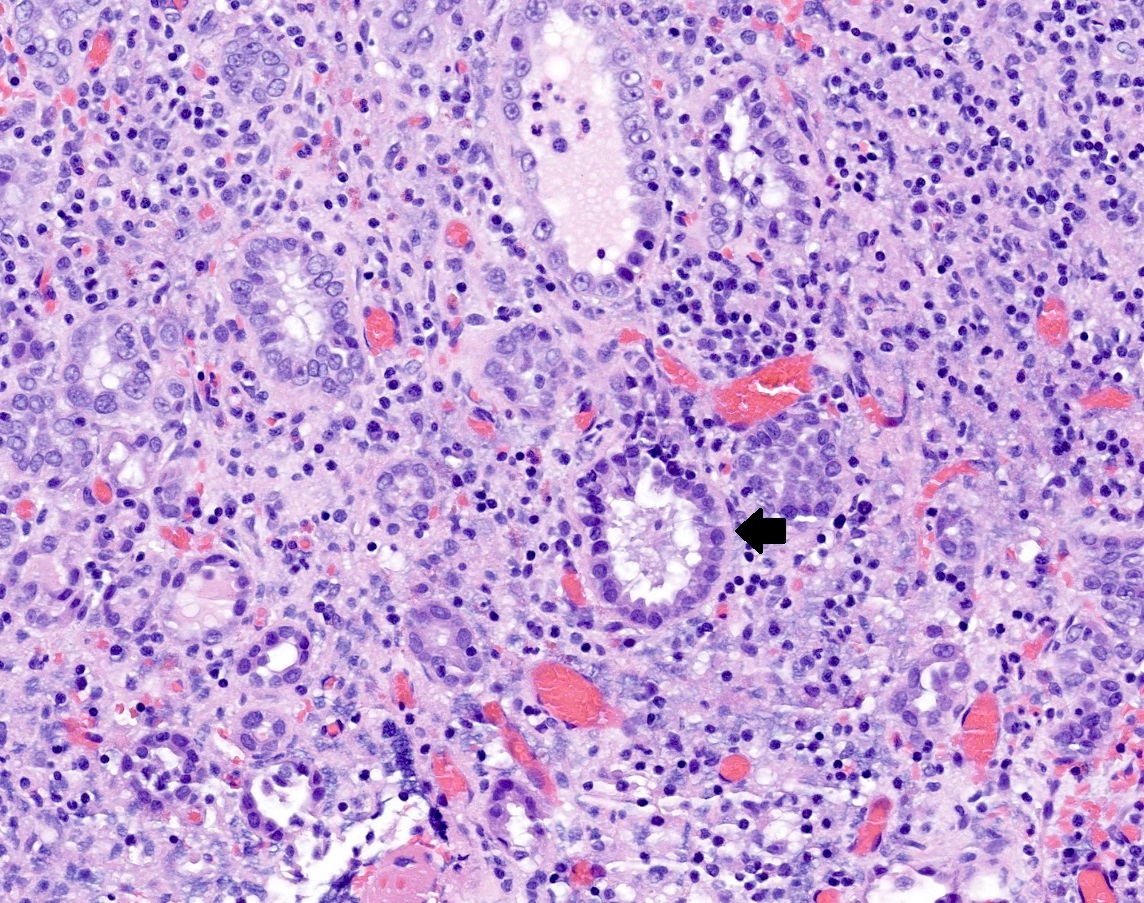
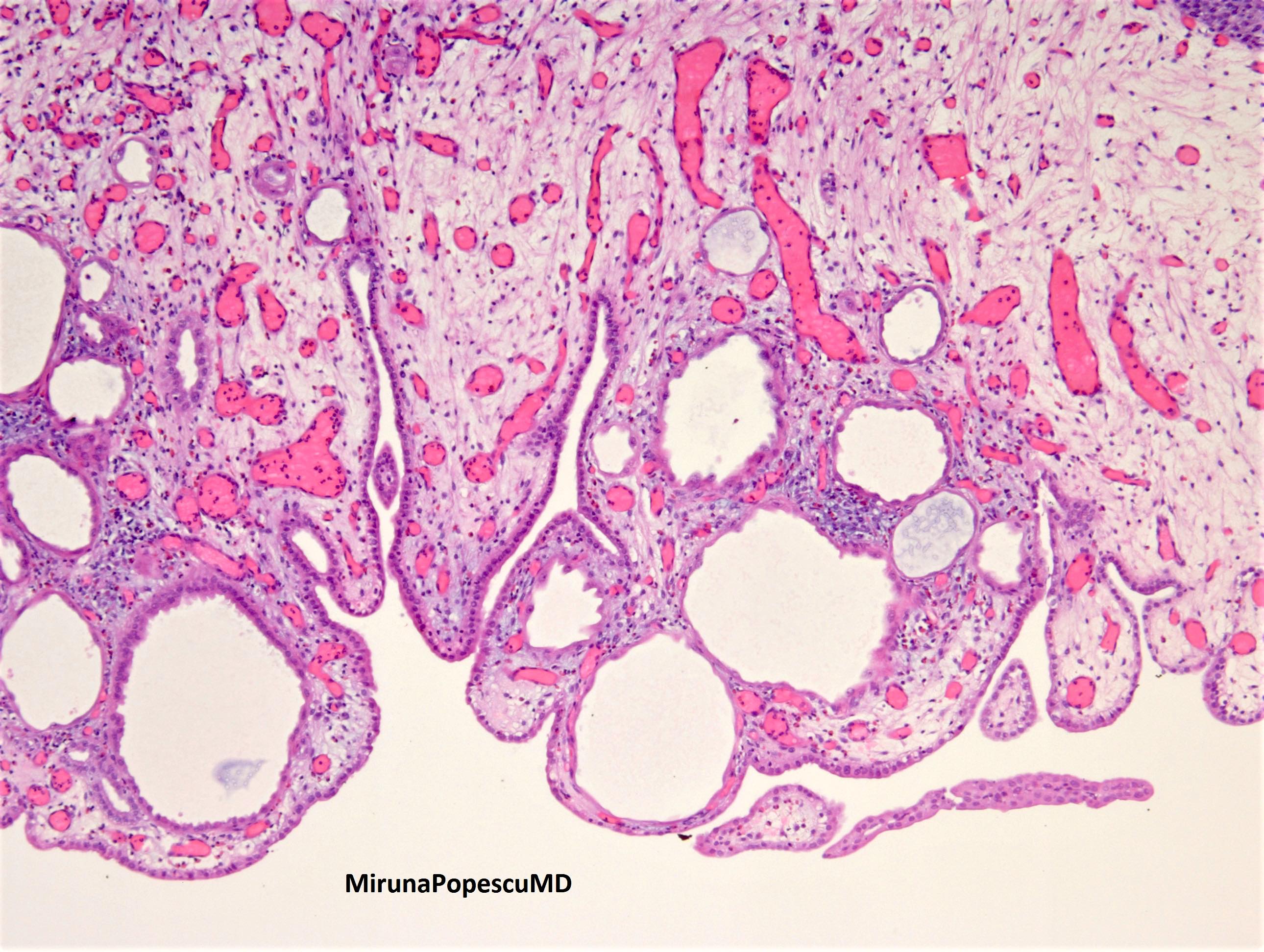
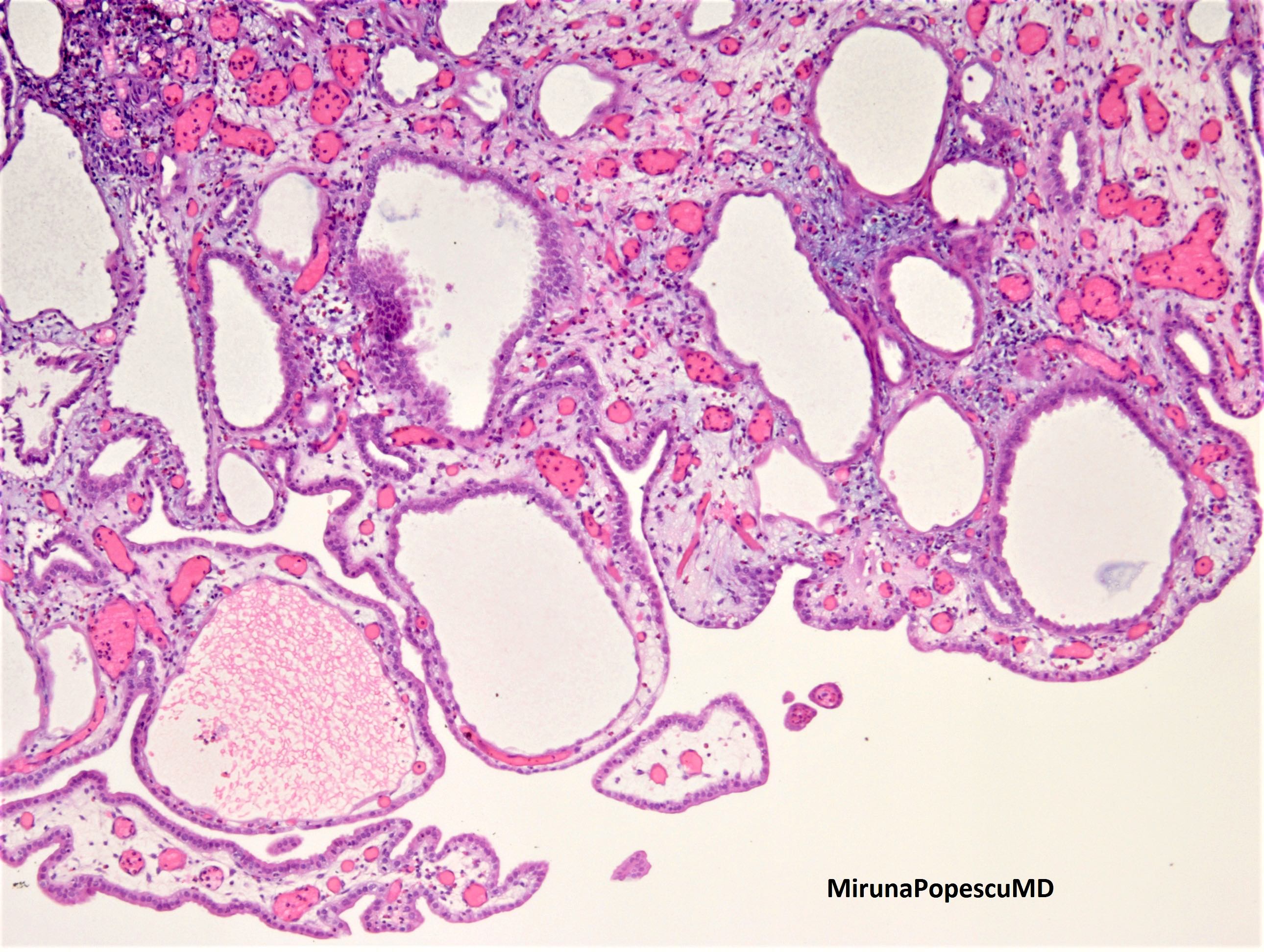
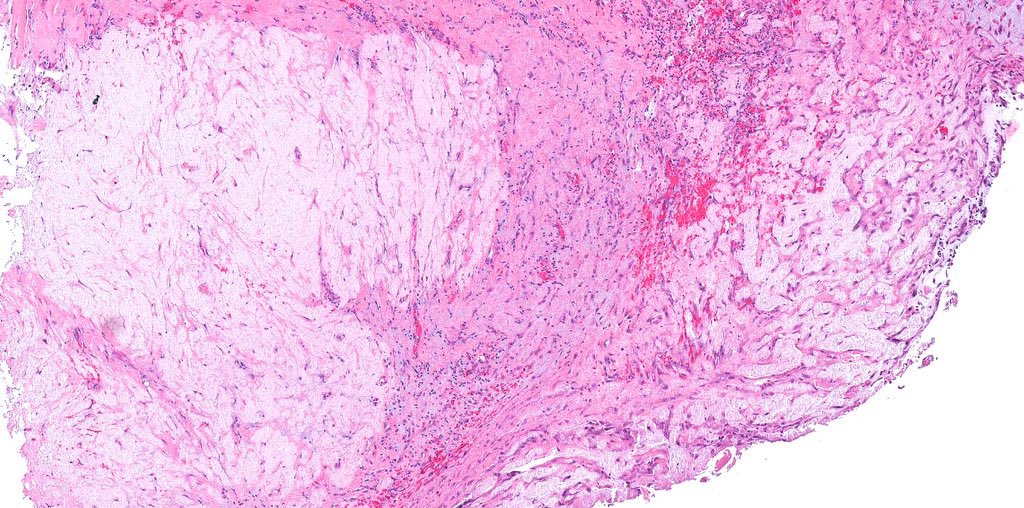
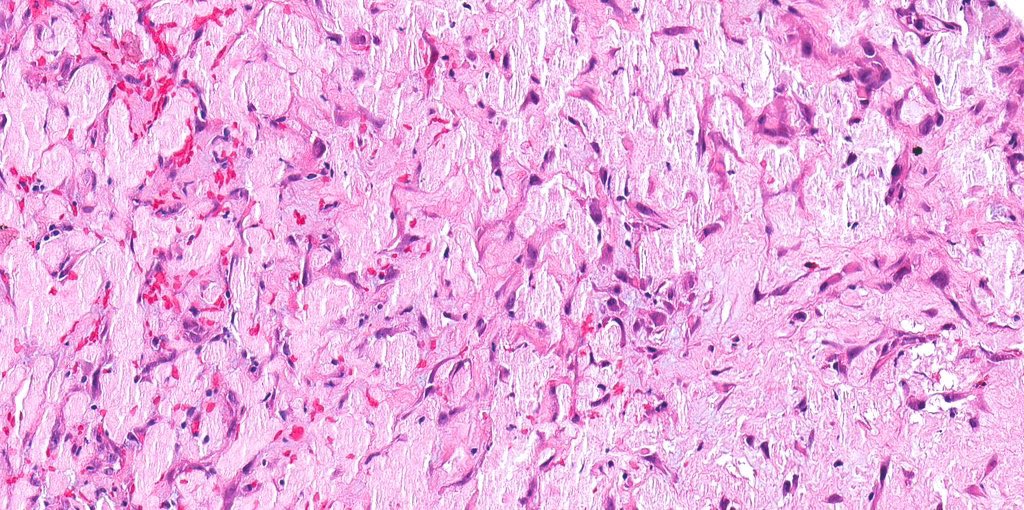
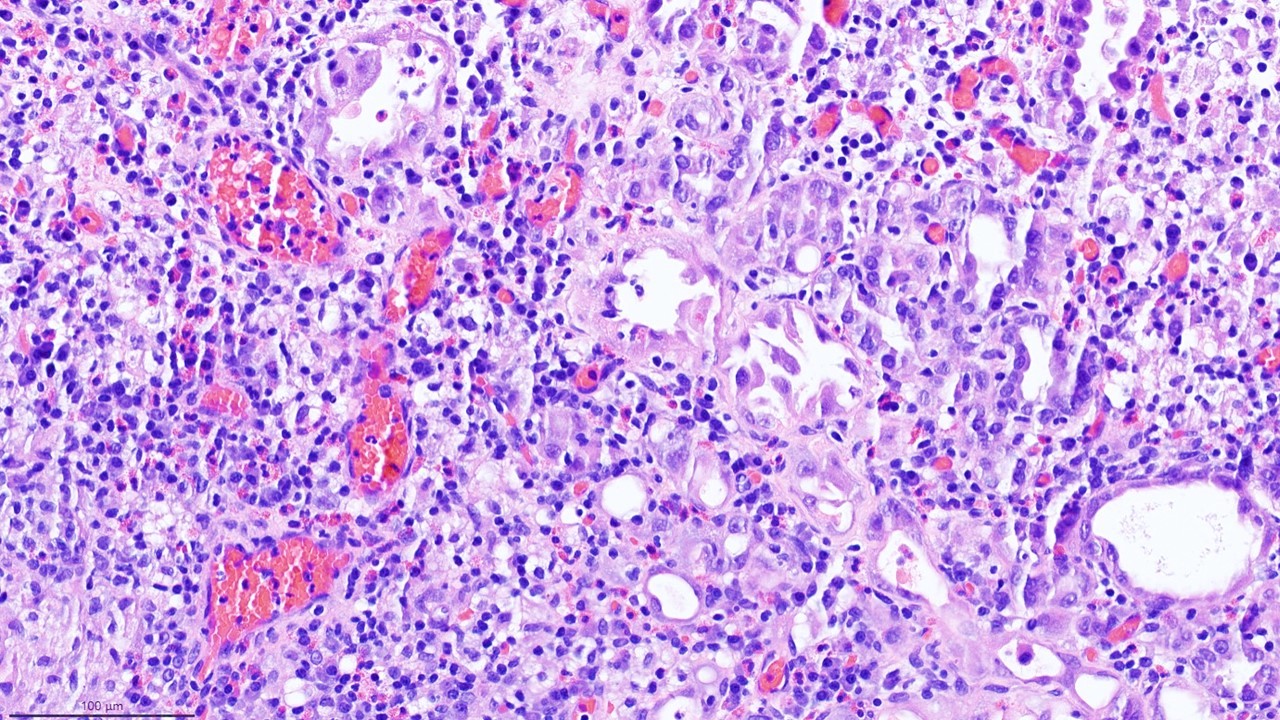
Microscopic (histologic) description
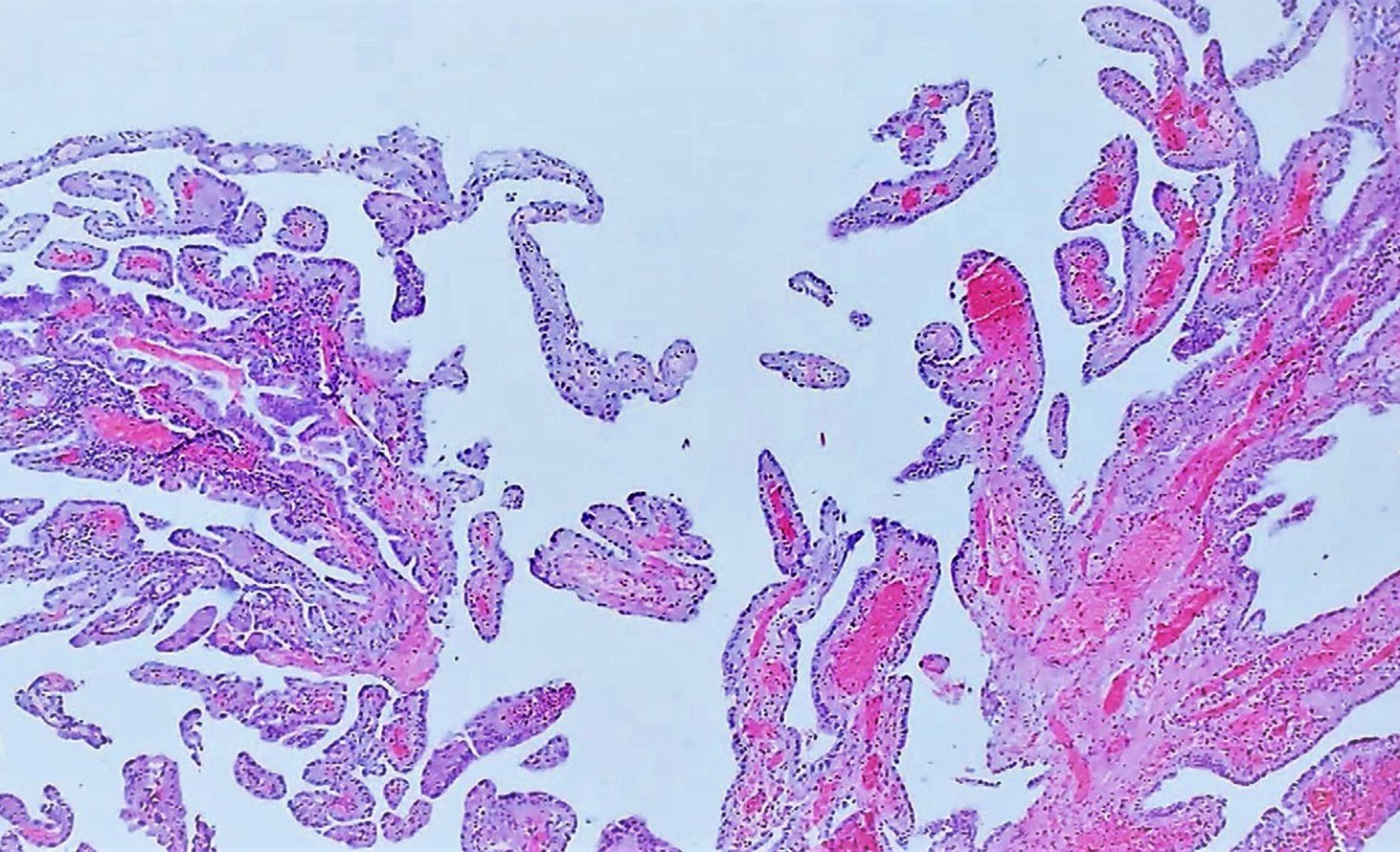
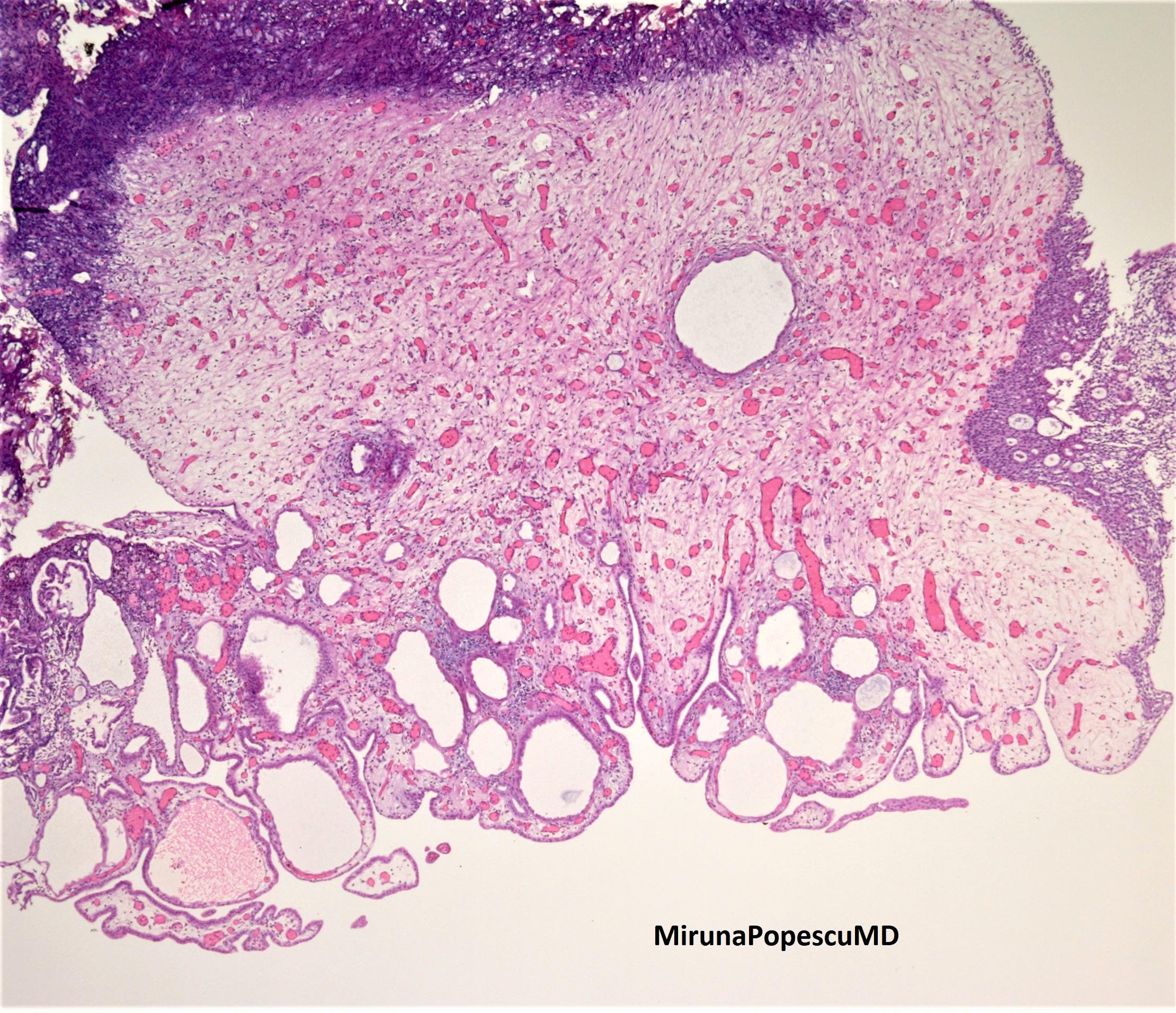
- Exhibit spectrum of mixed histologic patterns: tubular, tubulocystic, papillary, polypoid and less frequently, solid growth (Adv Anat Pathol 2006;13:247)
- Multiple small caliber tubules lined by cuboidal, low columnar and hobnail cells, exhibiting irregular smudged nuclei protruding into the lumen
- Intraluminal colloid-like eosinophilic secretions or blue tinged mucin
- Tubules often surrounded by a thickened hyalinized basement membrane
- Cytoplasm, in general eosinophilic but may focally have clear cytoplasm, especially in solid areas (Hum Pathol 1998;29:1451)
- Mostly limited to superficial lamina propria, lack a desmoplastic stromal response, necrosis, cytological atypia or brisk mitosis
- Background stroma may be variable depending upon the etiology and display edematous changes, mixed inflammatory infiltrates, reparative type fibrosis, granulomas or fibromyxoid changes
- Atypical nephrogenic metaplasia is a term reserved for cases with unexpected nuclear enlargement, hyperchromasia and abnormally prominent nucleoli (Cancer 2000;88:853)
- Uncommon patterns include:
- Pseudoinfiltrative growth pattern composed of small tubules lacking a basal cell layer; may mimic neoplasia
- Signet ring-like appearance with intraluminal blue tinged mucin and compressed tubules
- Cystic pattern which may resemble atrophic renal tubules
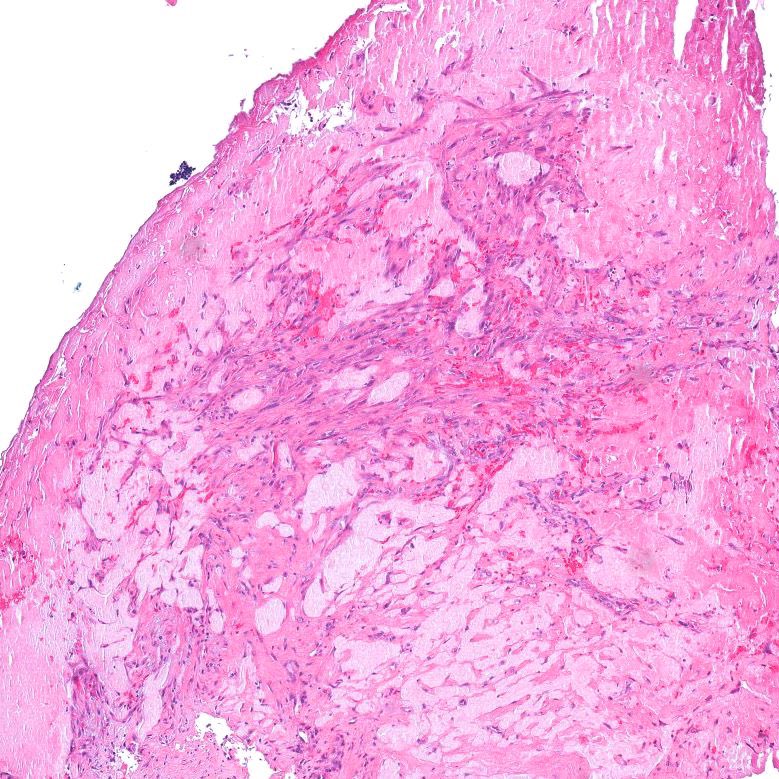
- Fibromyxoid variant:
- Composed of compressed spindled cells and irregular epithelial cords within a fibromyxoid stroma
- Scanty classic tubular pattern
- Background with a light pinkish / lavender colored stroma, which is negative for amyloid (Congo red stain) and Tamm-Horsfall protein (Am J Surg Pathol 2007;31:1231)
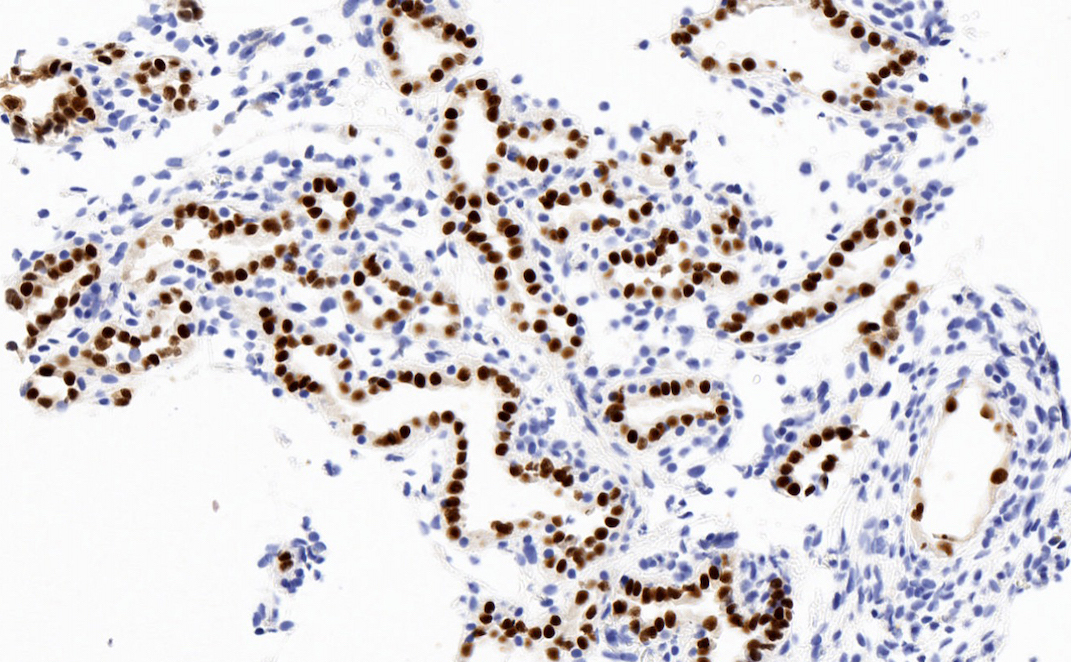
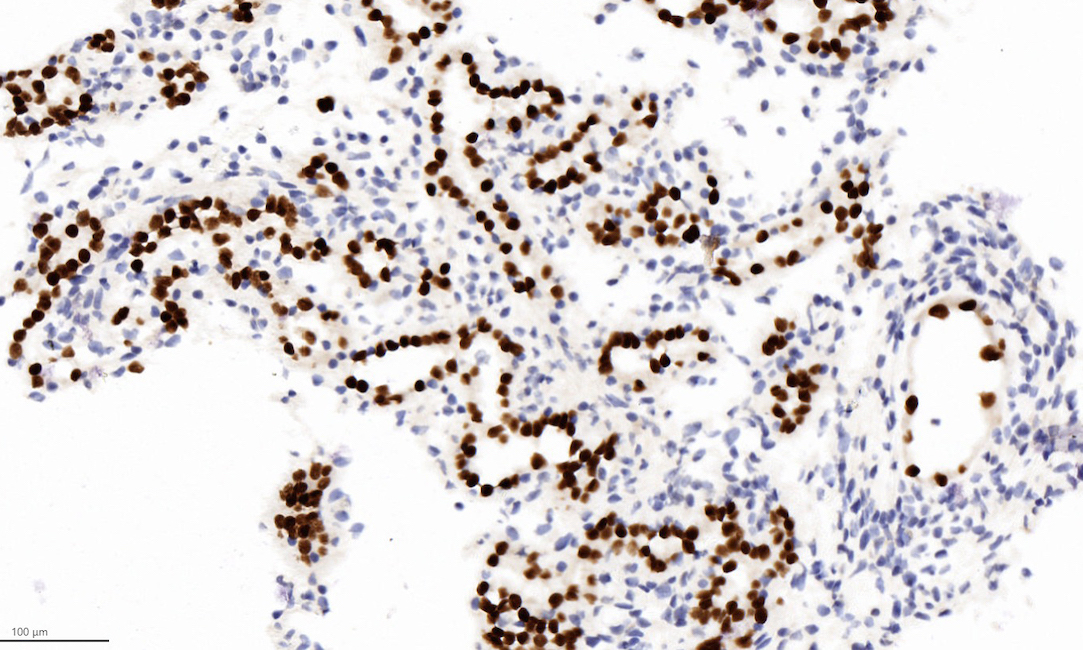
Microscopic (histologic) images
Contributed by Jatin S. Gandhi, M.B.B.S., M.D., @MirunaPopescu13 on Twitter and @katcollmd on Twitter
Cytology description
- Variable sized clusters composed of cuboidal cells with high N/C ratio (Diagn Cytopathol 2008;36:47)
- Nuclei are centrally or eccentrically located, have finely distributed chromatin with small nucleoli and regular nuclear membranes
- Cytoplasm is granular or vacuolated resembling a signet ring cell appearance
Positive stains
Negative stains
- Ki67: range 0 - 5% (average ~2%)
- p63 (up to 7% and mostly focal), PSA, PSAP (rare exceptions), NKX3.1 (Histopathology 2017;71:669, Am J Surg Pathol 2014;38:1664)
- HNF1 beta (~25%), (Hum Pathol 2011;42:1613)
- GATA3 (~40%) (Am J Surg Pathol 2014;38:1664)
Electron microscopy description
- Complex ultrastructural features resemble proximal convoluted tubules, Henle loop and collecting tubules (J Natl Med Assoc 1985;77:201)
Molecular / cytogenetics description
- Currently no known disease defining recurrent cytogenetic alterations
Sample pathology report
- Urinary bladder, transurethral resection:
- Nephrogenic metaplasia and chronic and granulomatous inflammation
- Muscularis propria identified
Differential diagnosis
- Clear cell adenocarcinoma:
- Papillary urothelial carcinoma:
- Multilayered urothelial cells with variable atypia
- IHC: p63+, Uroplakin 2+, GATA3+
- Urothelial carcinoma nested / microcystic variant:
- Small, crowded, tightly packed, multilayered, irregular nests with bland cytology and without any associated stromal changes
- Usually deeply infiltrative
- IHC: p63+, Uroplakin 2+, GATA3+
- Prostatic adenocarcinoma of bladder:
Board review style question #1
A 60 year old man presented with a bladder lesion. A transurethral resection of bladder tumour was performed. Which of the following statements is true regarding the lesion shown in the above image?
- Associated with endometriosis
- Associated with renal transplant
- Cytological atypia is common
- Generally infiltrates muscularis propria
Board review style answer #1
B. Associated with renal transplant
Nephrogenic metaplasia is commonly seen in the superficial lamina propria, is cytologically bland and may be associated with post renal transplant. Endometriosis is commonly associated with clear cell adenocarcinoma.
Comment Here
Reference: Nephrogenic metaplasia
Nephrogenic metaplasia is commonly seen in the superficial lamina propria, is cytologically bland and may be associated with post renal transplant. Endometriosis is commonly associated with clear cell adenocarcinoma.
Comment Here
Reference: Nephrogenic metaplasia
Board review style question #2
Which of the following combination of immunostains can be useful to differentiate nephrogenic metaplasia from prostatic adenocarcinoma?
- PAX8, HNF1 beta, AMACR
- PAX8, Napsin A, AE1/3
- PAX8, Napsin A, NKX3.1
- PAX8, Napsin A, GATA3
Board review style answer #2
C. PAX8, Napsin A, NKX3.1
Nephrogenic metaplasia is commonly positive for PAX8 and Napsin A and less commonly for HNF1 beta and GATA3. NKX3.1 is expressed almost exclusively in prostatic adenocarcinoma. Both nephrogenic metaplasia and prostatic adenocarcinoma express AMACR and AE1/3.
Comment Here
Reference: Nephrogenic metaplasia
Nephrogenic metaplasia is commonly positive for PAX8 and Napsin A and less commonly for HNF1 beta and GATA3. NKX3.1 is expressed almost exclusively in prostatic adenocarcinoma. Both nephrogenic metaplasia and prostatic adenocarcinoma express AMACR and AE1/3.
Comment Here
Reference: Nephrogenic metaplasia