Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Choy B. Prostatic type polyp. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bladderprostatepolyp.html. Accessed April 19th, 2024.
Definition / general
- Uncommon, nonneoplastic urothelial tract polyp comprised of prostatic glands and stroma
Essential features
- Polypoid or papillary lesion consists of nonneoplastic prostatic glandular epithelium with 2 distinct cell layers (luminal / secretory layer and basal layer) and corpora amylacea
- Immunoreactive for prostate specific antigen (PSA) and prostatic acid phosphatase (PAP)
- Most important differential to consider and exclude is prostatic ductal adenocarcinoma
Terminology
- Ectopic prostate
- Benign prostatic epithelial polyp
- Adenomatous polyp with prostatic type epithelium (historically used)
- Papillary adenoma with prostatic type epithelium (historically used)
ICD coding
- ICD-10: N32.9 - bladder disorder, unspecified
Epidemiology
- Broad age range: 19 - 89 years (J Int Med Res 2019;47:1787)
Sites
- Urothelial tract
- Most common in prostatic urethra, often in and around verumontanum
- In the bladder, most involves trigone (Int Urol Nephrol 1997;29:313, Histopathology 2011;58:750, J Int Med Res 2019;47:1787)
Etiology
- Different theories have been proposed, including (Histopathology 1987;11:789, Hinyokika Kiyo 1990;36:1463, Int J Urol 2005;12:1066)
- Metaplastic change
- Hyperplastic change
- Abnormal migration and misplacement of prostatic tissue
- Persistence of embryonic remnants
Clinical features
- Gross or microscopic hematuria (Histopathology 1987;11:789, Int Urol Nephrol 1997;29:313, J Int Med Res 2019;47:1787)
- Hematospermia
- Dysuria
- Urinary outflow obstruction
Diagnosis
- Cystoscopy with biopsy or transurethral resection
- Histologic examination of tissue
Radiology description
- Transrectal ultrasonography (Clin Imaging 2013;37:778)
- Homogeneous isoechogenicity, similar to the bladder wall
- No significant high blood flow on color Doppler ultrasound
Prognostic factors
- Nonneoplastic with low potential for recurrence (Int Urol Nephrol 1997;29:313, Int J Urol 2005;12:1066)
Case reports
- 15 year old boy with dysuria; cystoscopy showed a mass at the bladder neck (J Int Med Res 2019;47:1787)
- 45, 61 and 79 year old men with prostatic polyps (Int J Urol 2005;12:1066)
- 47 year old man with urothelial carcinoma and 52 year old man with hematuria (Urology 2014;83:535)
- 72 year old man with hematuria and smooth sessile mass at the bladder dome (World J Mens Health 2013;31:176)
Treatment
- Simple resection is often curative (J Int Med Res 2019;47:1787)
Clinical images
Gross description
- Usually small, polypoid or papillary (Int Urol Nephrol 1997;29:313)
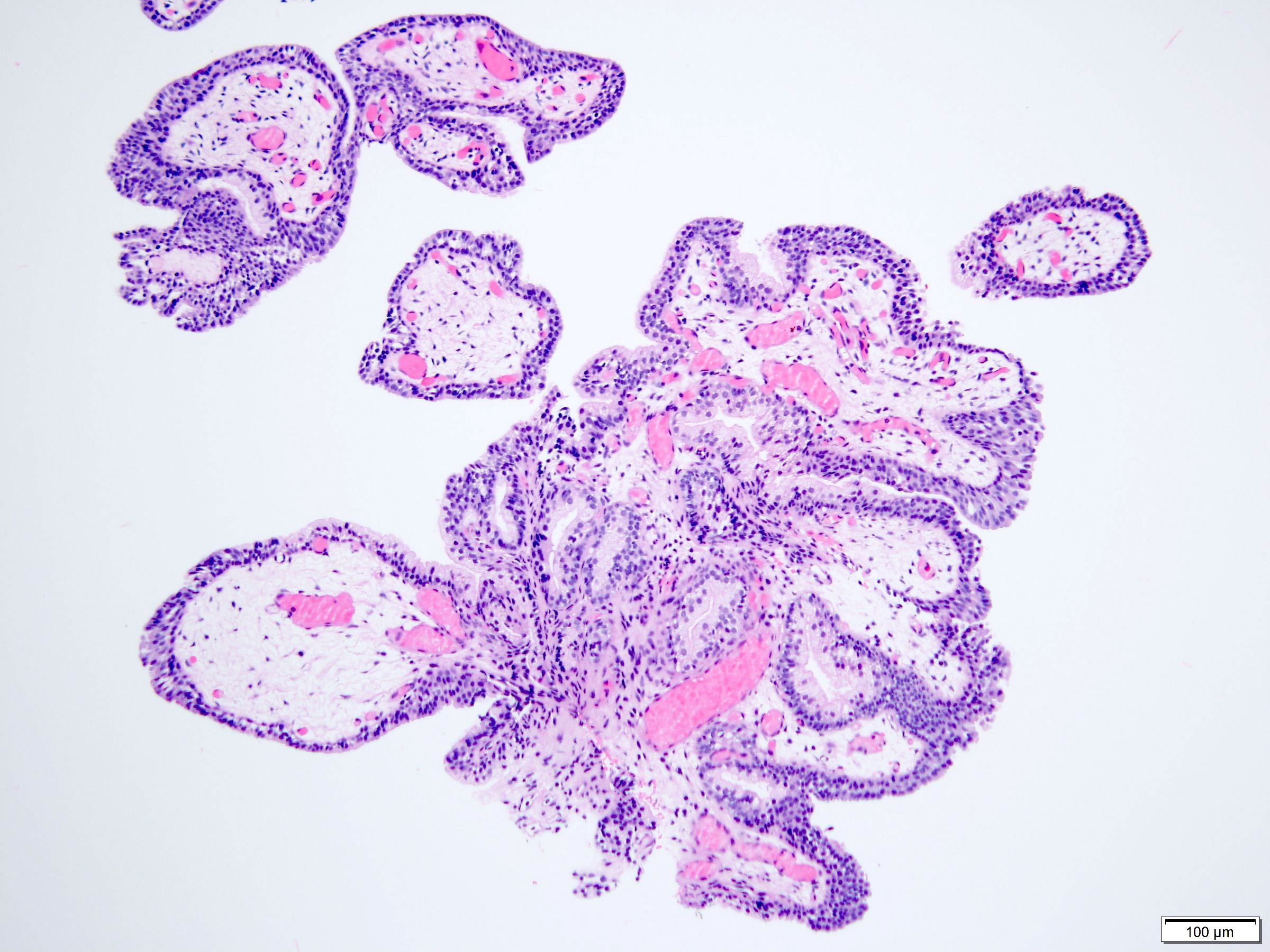
Microscopic (histologic) description
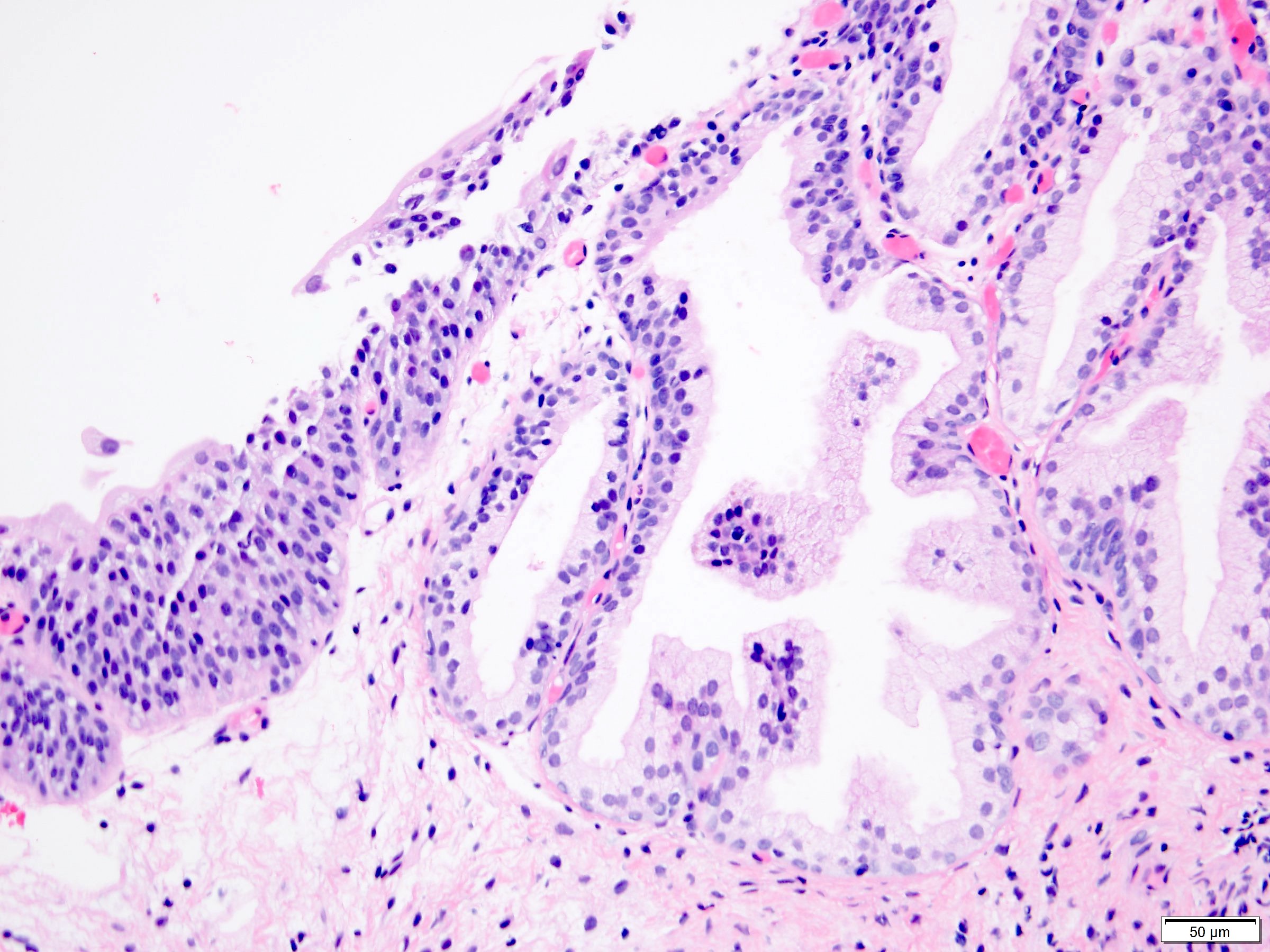
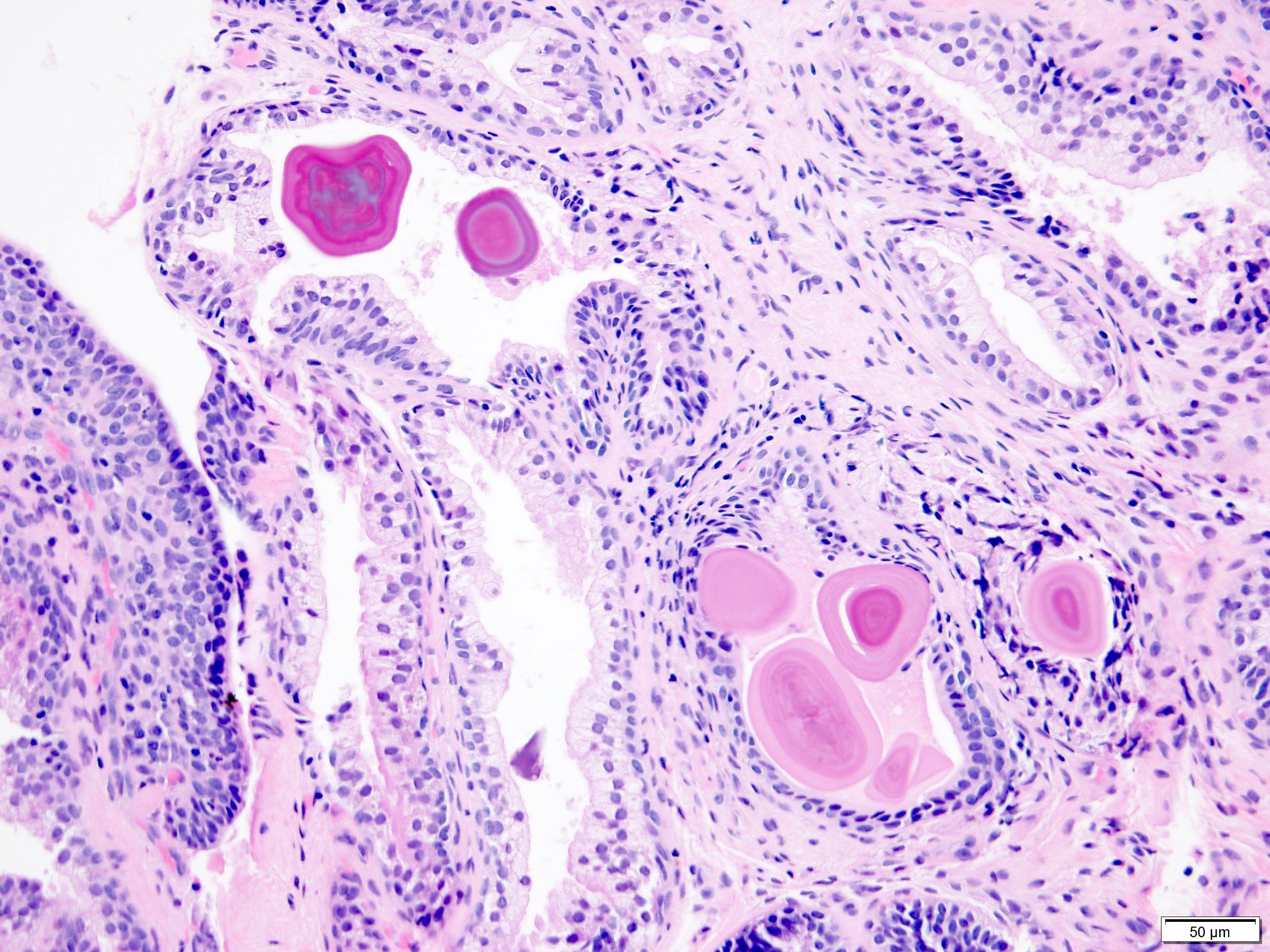
- Polypoid or papillary
- Nonneoplastic prostatic type glandular epithelium within stroma (Histopathology 1987;11:789, Am J Surg Pathol 1984;8:833, Int Urol Nephrol 1997;29:313, Histopathology 2011;58:750)
- Prostatic acini vary in number and may contain corpora amylacea
- 2 distinct cell layers: luminal epithelial cell layer and basal cell layer
- Luminal layer: cuboidal to columnar cells with round nuclei and frothy, faintly eosinophilic cytoplasm, some containing eosinophilic granules
- Basal cell layer: between luminal layer and basement membrane, typically elongated and flattened cells with slender nuclei and minimal cytoplasm
- Interspersed urothelium may be associated with cystitis cystica and cystitis glandularis
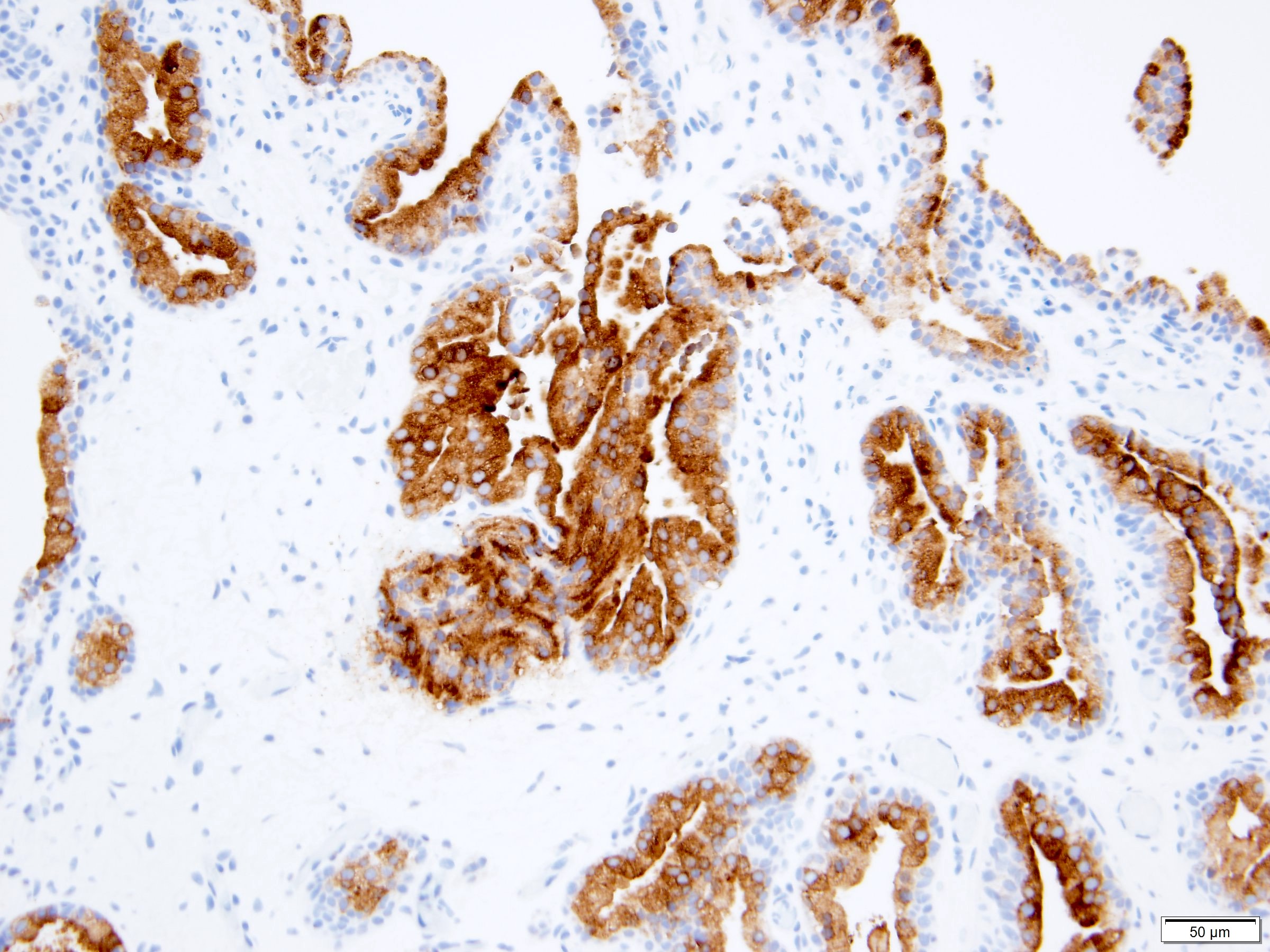
Microscopic (histologic) images
Cytology description
- Papillary clusters of bland cuboidal to columnar glandular cells (Diagn Cytopathol 2003;29:356, Arch Pathol Lab Med 2000;124:1047)
- Cells with uniform, ovoid nuclei, vesicular chromatin, occasional small single inconspicuous nucleoli and pale granular cytoplasm
Positive stains
- PSA, PAP / PSAP (Hinyokika Kiyo 1990;36:1463, Int Urol Nephrol 1997;29:313, Histopathology 2011;58:750)
- Prostein / P501S: basal aspect (Histopathology 2011;58:750)
- CD10: luminal pattern (Histopathology 2011;58:750)
- Cytokeratin (CK18) (Histopathology 2011;58:750)
- Basal cells: cytokeratin 34 beta E12, p63 (Urology 2014;83:535, Histopathology 2011;58:750)
Negative stains
- Racemase: no overexpression (Pathology 2007;39:476, Histopathology 2011;58:750)
- Ki67 proliferative index: low (Pathology 2007;39:476)
- CK7 (Urology 2014;83:535)
- CK20 (Urology 2014;83:535)
Sample pathology report
- Urinary bladder, biopsy:
- Prostatic type polyp (see comment)
- Comment: Immunohistochemistry for PSA and PSAP highlight the glandular epithelium within the polypoid lesion, confirming prostatic origin.
Differential diagnosis
- Prostatic ductal adenocarcinoma:
- Urothelial carcinoma with glandular differentiation:
- Papillary urothelial neoplasm:
- Benign prostatic hyperplasia:
- Variable amounts of benign prostatic glands and spindle cells
- May form polypoid mass protruding into the bladder near the bladder neck
- Nephrogenic metaplasia (adenoma):
- Polypoid / papillary cystitis:
- Cystitis cystica / glandularis:
Board review style question #1
A 40 year old man with gross hematuria is found to have a polypoid mass in the bladder trigone on cystoscopy. A transurethral resection of the bladder mass shows the above histologic features. Immunohistochemistry for PSA was performed. What is the likely diagnosis?
- Nephrogenic adenoma
- Polypoid cystitis
- Prostatic ductal adenocarcinoma
- Prostatic type polyp
Board review style answer #1
D. Prostatic type polyp. Prostatic type polyp consists of benign prostatic acini admixed with urothelium. PSA positivity confirms prostatic origin. Nephrogenic adenoma can demonstrate mixed papillary, polypoid, tubular and tubulocystic patterns lined by a single cuboidal layer of epithelial cells, unlike the 2 cell layers present in prostatic glands. Polypoid cystitis may have similar architecture as prostatic type polyp. However, polypoid cystitis does not contain prostatic glands and is negative for PSA. While PSA is immunoreactive in both prostatic type polyp and prostatic ductal adenocarcinoma, morphologic features, such as complex architecture, pseudostratified columnar epithelium and prominent nucleoli (not seen in the above image), support the latter.
Comment Here
Reference: Prostatic type polyp
Comment Here
Reference: Prostatic type polyp
Board review style question #2
Which of the following is true regarding prostatic type polyp?
- Behaves in benign fashion, with low recurrence rate
- Marked cytologic atypia present
- Most commonly seen at anterior wall of the bladder
- Patients often present with elevated PSA
Board review style answer #2
A. Behaves in benign fashion, with low recurrence rate. Prostatic type polyp is a nonneoplastic process, with low potential for recurrence. Patients most frequently present with hematuria. Other presenting symptoms include hematospermia, dysuria and urinary outflow obstruction. In the urinary bladder, the most common site is the trigone. Morphologic features show benign prostatic type glandular epithelium admixed with urothelium.
Comment Here
Reference: Prostatic type polyp
Comment Here
Reference: Prostatic type polyp