Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Ali RH. Avascular necrosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/boneasepticbonenecrosis.html. Accessed April 20th, 2024.
Definition / general
- Avascular necrosis (AVN) is a disease that results from temporary or permanent loss of blood supply to bone at watershed zones where collateral circulation is lacking
- Pathologically, AVN is characterized by death of bone cells and marrow elements and manifests as a localized area of bone infarction, usually at subchondral locations
Essential features
- Characterized by necrosis of bone and bone marrow cellular components due to ischemia
- Preferentially involves subchondral / epiphyseal ends of bone, particularly the femoral head
- Risk factors include traumatic and nontraumatic causes
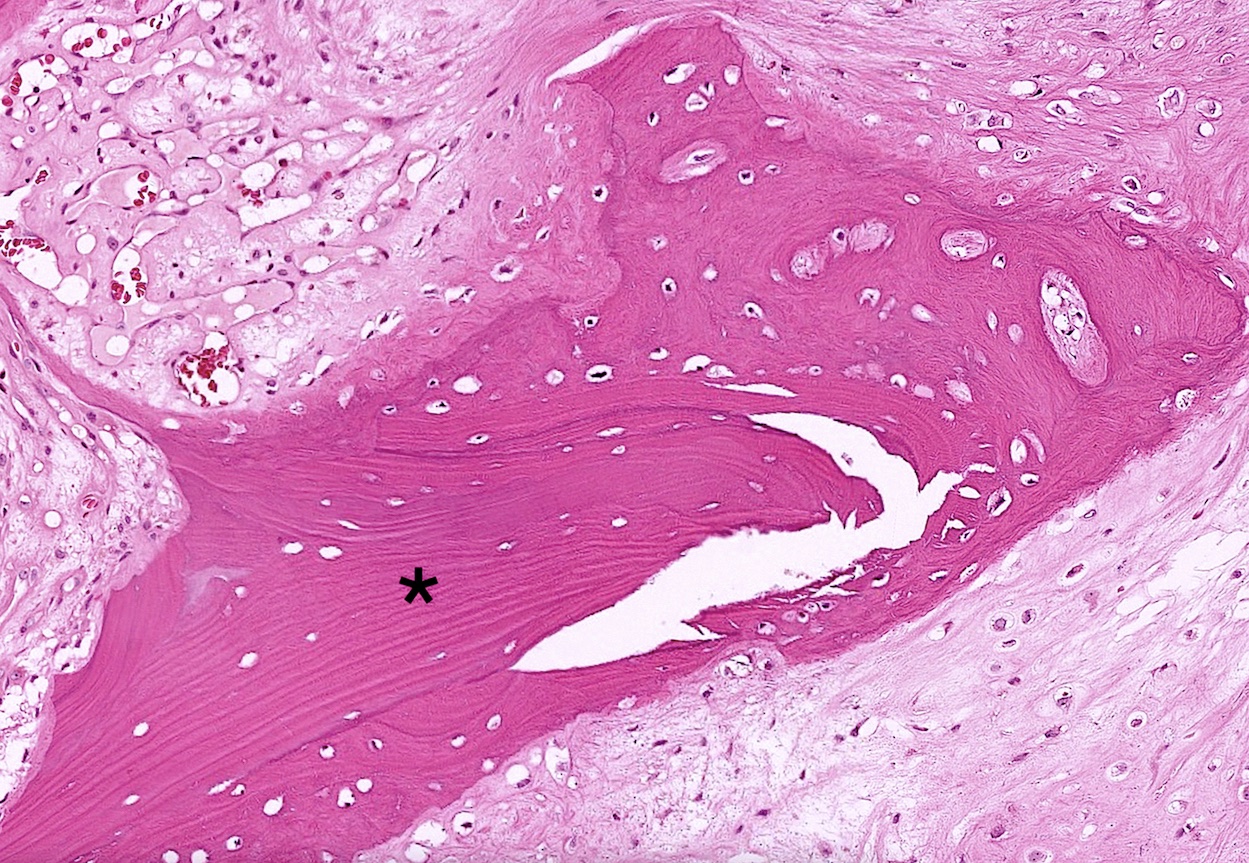
- Advanced disease results in cleavage of the subchondral bone from the overlying cartilage (crescent sign)
- Eventually culminates in the collapse of the joint and secondary degenerative joint disease / osteoarthritis
Terminology
- Synonyms: osteonecrosis (preferred term), aseptic necrosis, ischemic bone necrosis
- Variants
- Preiser disease: osteonecrosis of the scaphoid
- Keinbock disease: osteonecrosis of the lunate
- Legg-Calvé-Perthes disease: idiopathic osteonecrosis of femoral epiphysis in children
- Dysbaric osteonecrosis / caisson disease: osteonecrosis in undersea divers
ICD coding
- ICD-10: M87.00 - idiopathic aseptic necrosis of unspecified bone
Epidemiology
- Most common in the hip, ages 30 - 65 years, M > F
- In the United States, 10% of total hip arthroplasties are due to AVN
- Reference: StatPearls: Avascular Necrosis [Accessed 3 November 2023]
Sites
- Femoral head is most common
- Humeral head is second most common, usually with concurrent hip involvement (Orthop Surg 2020;12:1340)
- Other: medial femoral condyle, talus, scaphoid and lunate
- Traumatic AVN is typically unilateral while nontraumatic is commonly bilateral (Radiographics 2014;34:1003)
- Multifocality (≥ 3 separate anatomic sites) also common in nontraumatic AVN (e.g., sickle cell disease, chronic corticosteroid use) but may be overlooked without radiological screening (Open Orthop J 2009;3:32, Sci Rep 2016:6:29576)
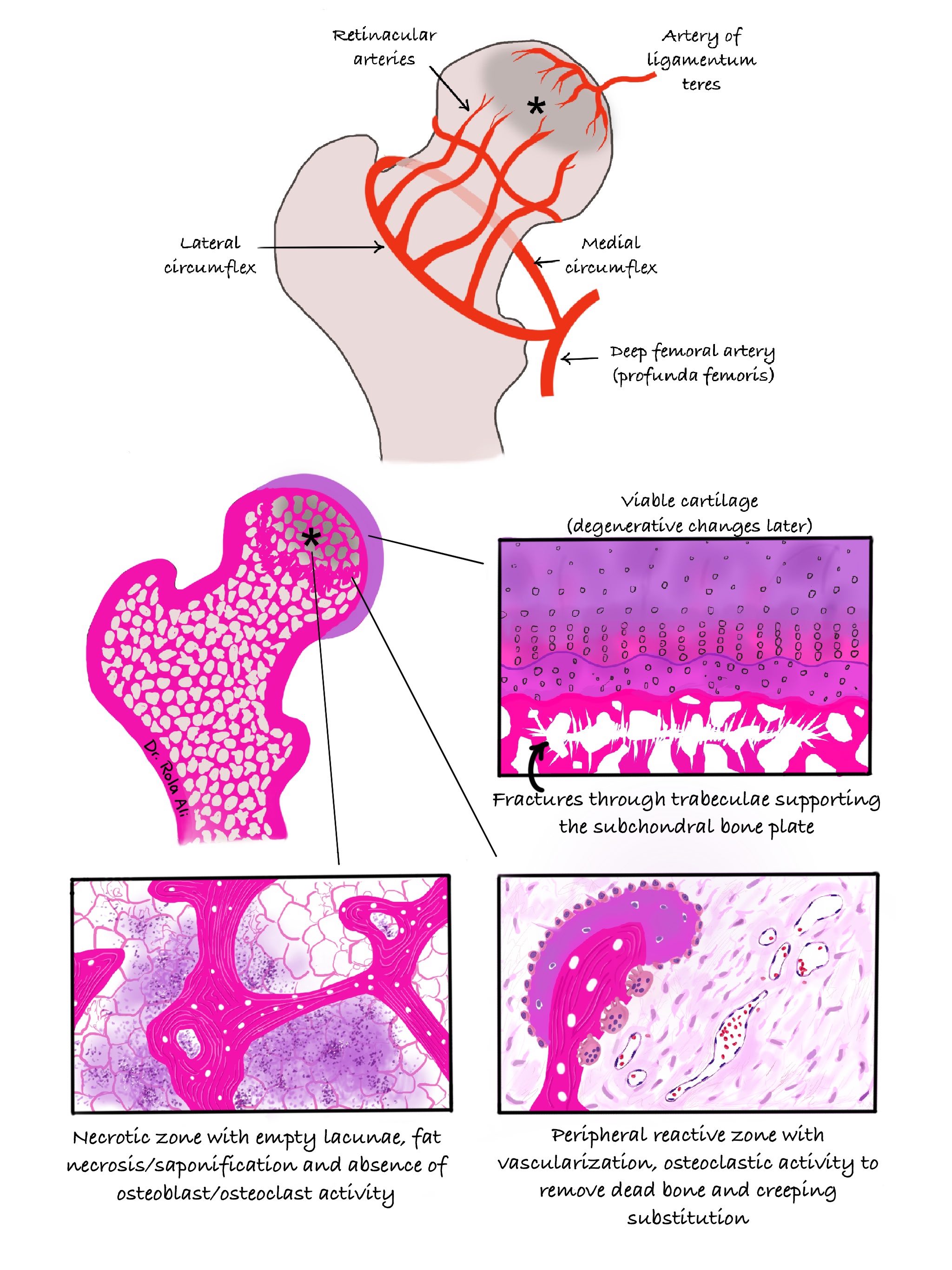
Pathophysiology
- Disruption of blood supply is a key event
- Subchondral microcirculation of the femoral head is particularly vulnerable (see Diagrams)
- Mechanisms (Curr Rev Musculoskelet Med 2015;8:201)
- Direct trauma to vessels: fractures, dislocation, surgery
- Intravascular occlusion: thrombi, sickle cell aggregations, nitrogen and lipid emboli, venous outflow occlusion
- Intraosseous compression of microcirculation: steroid induced adipogenesis and lipid deposition, Gaucher cells replacing bone marrow (Clin Orthop Relat Res 2000:370:295)
- Sequence of events (Curr Rev Musculoskelet Med 2015;8:201)
- Earliest: necrosis of hematopoietic marrow, interstitial marrow edema
- Osteocyte necrosis occurs ~2 - 3 hours from the beginning of anoxia, though histological evidence may become evident 24 - 72 hours later
- Reparative process begins at the periphery of the necrotic zone and involves bone resorption and production (yet the new bone is composed of weak woven bone)
- Net result: ineffective repair, increased bone resorption relative to production and loss of structural integrity
- Necrotic zone
- Ischemia → loss of oxygen / nutrient supply → osteoblastic / osteoclastic activity is no longer supported → no bone remodeling → loss of bone compliance and structural integrity → fracturing occurs especially with weight bearing → articular collapse
- Peripheral reparative zone
- Growth of vascularized granulation tissue → osteoblastic / osteoclastic activity is supported → progressive yet ineffective remodeling at the interface between necrotic and viable bone (creeping substitution) with the formation of an outer sclerotic rim
Etiology
- Frequently idiopathic: when no cause is apparent
- Traumatic risk factors: femoral head fractures and dislocation, surgical interventions of bone
- Nontraumatic risk factors: corticosteroids, alcohol abuse, sickle cell disease, systemic lupus erythematosus, antiphospholipid antibody syndrome, Gaucher disease, caisson disease (Clin J Sport Med 2015;25:153)
- Other associations: pancreatitis, HIV, radiation therapy, renal transplantation, leukemia / lymphoma
- Reference: Int J Environ Res Public Health 2022;19:7348
Clinical features
- Slowly progressive groin pain, which may radiate to the buttock or knee and a limited range of motion
- Asymptomatic cases can be found incidentally on imaging
Diagnosis
- Diagnosis is based on careful history, physical exam and imaging studies
- Bone pain in patients with known risk factors should prompt investigations for AVN
Laboratory
- Only relevant to identify conditions that may predispose to AVN
Radiology description
- Imaging appearances correspond to the underlying pathology
- Plain Xray (insensitive in early stages)
- Patchy areas of lucency (bone resorption) and sclerosis (partly due to saponification of fatty acids released from necrotic adipocytes in the marrow)
- Sclerosis at the rim (new bone formation)
- Curvilinear subchondral lucency (crescent sign) indicative of subchondral fracture and impending articular collapse
- Secondary degenerative changes
- MRI (most sensitive and specific): area of yellow marrow surrounded by a low signal intensity rim with all pulse sequences or a double line sign
- CT: more sensitive than plain Xray particularly when assessing articular collapse
- Reference: Radiographics 2014;34:1003
Prognostic factors
- Prognosis depends on the stage and location of the disease (Orthop Surg 2020;12:1340)
- Clinical course is progressive with patients eventually requiring surgical intervention
Case reports
- 14 year old boy with transfusion dependent thalassemia and hepatitis C who developed bilateral avascular necrosis of the femoral head (J Orthop Case Rep 2017;7:38)
- 17 year old boy with Kienböck disease who underwent experimental treatment with hyperbaric oxygen (BMJ Case Rep 2018;2018:bcr2018226090)
- 37 year old man with systemic lupus erythematosus who developed multifocal avascular osteonecrosis in both hips and shoulders and subsequent new osteonecrotic events following hip replacement (BMJ Case Rep 2018:2018:bcr2018225532)
- 55 year old woman who developed Preiser disease after repeated local glucocorticoid injections (Medicine (Baltimore) 2018;97:e12413)
Treatment
- Initial nonsurgical options: pharmacological agents, shock wave therapies (Indian J Orthop 2023;57:410)
- Joint preserving surgical options in early stages: core decompression, bone grafting, osteotomy (J Shoulder Elbow Surg 2023;32:2192, Orthop Surg 2021;13:742)
- Total hip arthroplasty in advanced stages with articular collapse and secondary osteoarthritis
- References: Int J Environ Res Public Health 2022;19:7348, EFORT Open Rev 2019;4:85
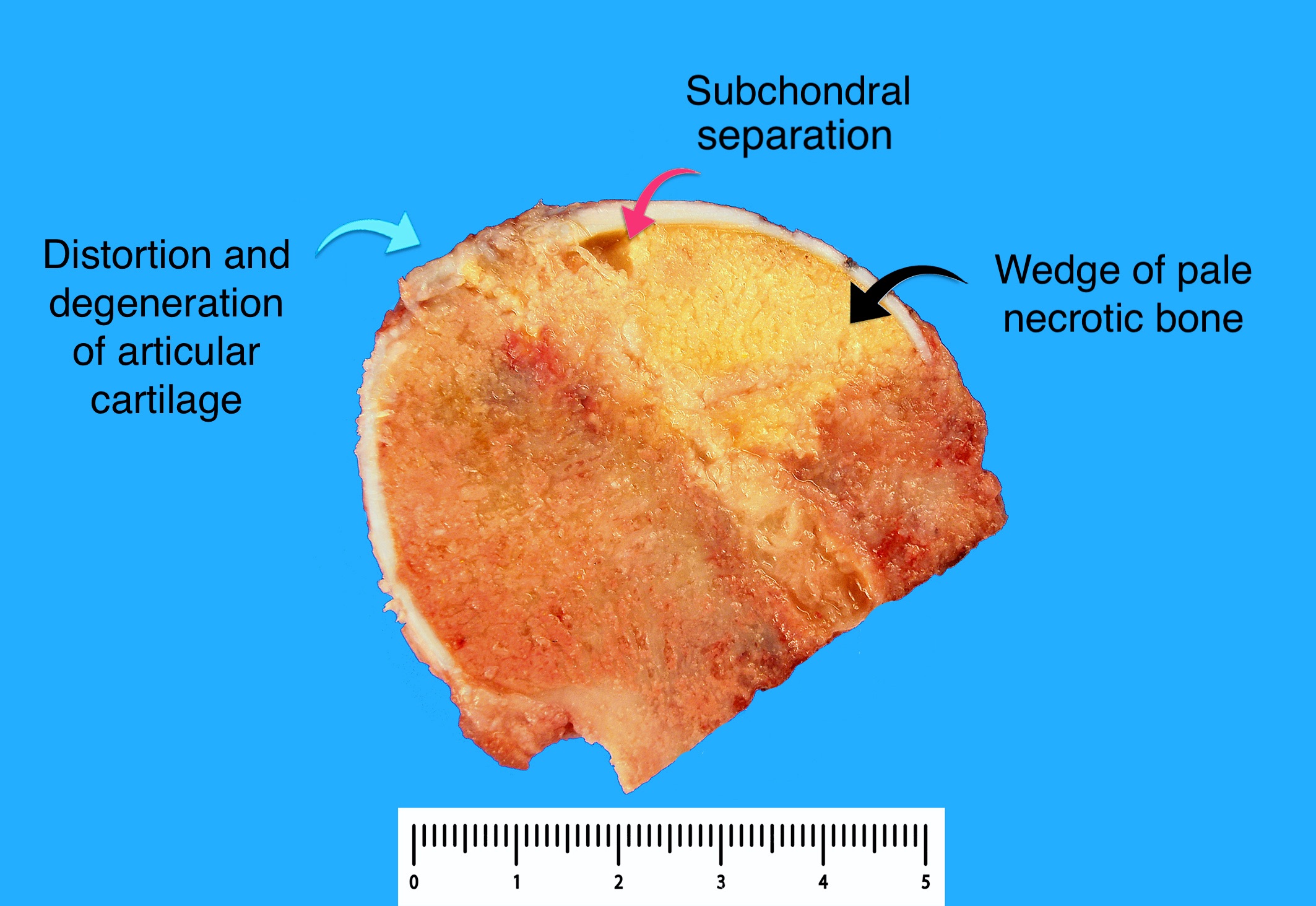
Gross description
- Wedge shaped infarct in the subchondral area that is dull yellow in color
- Peripheral hyperemic border may be appreciated with or without osteosclerosis
- Overlying articular cartilage may be buckled and separated from the infarcted bone
- Gross pathological manifestations are not apparent in early stages
- Reference: Rom J Morphol Embryol 2012;53:557
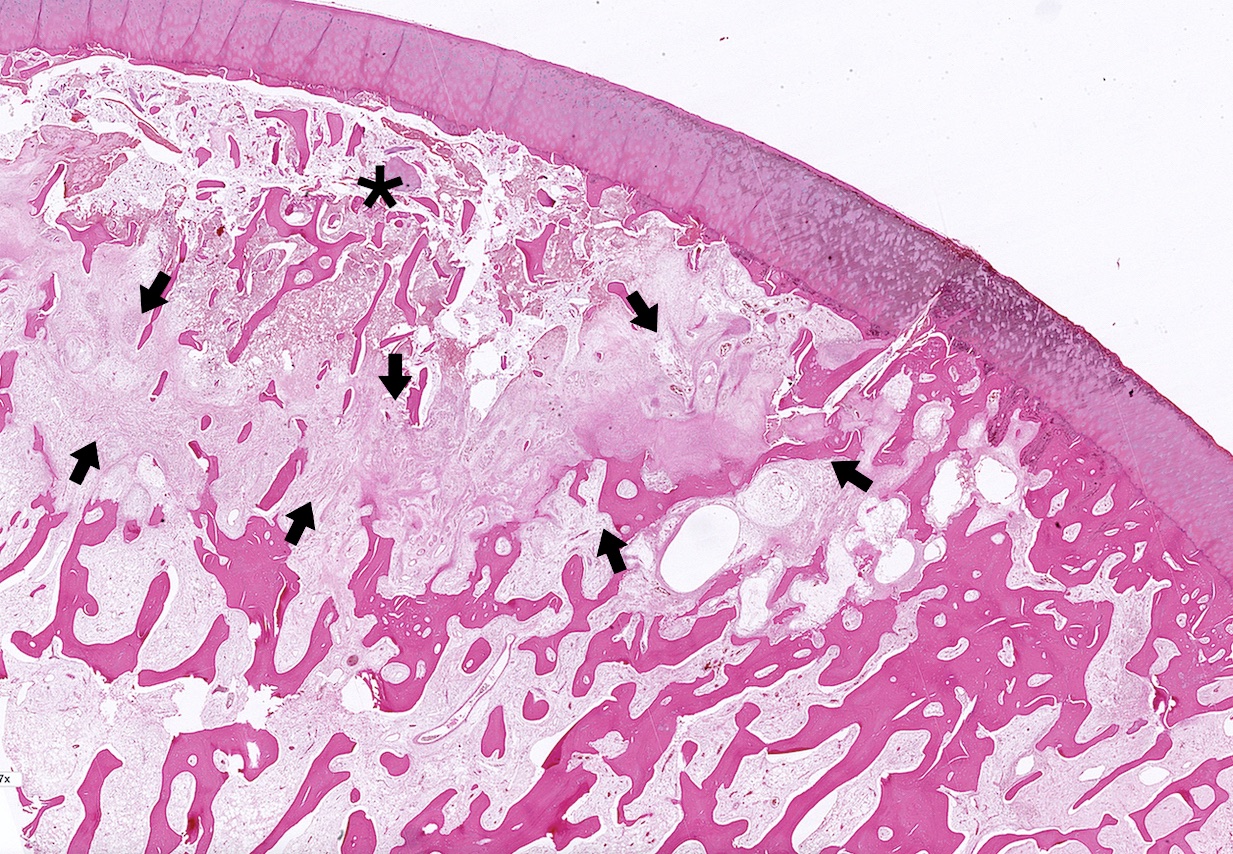
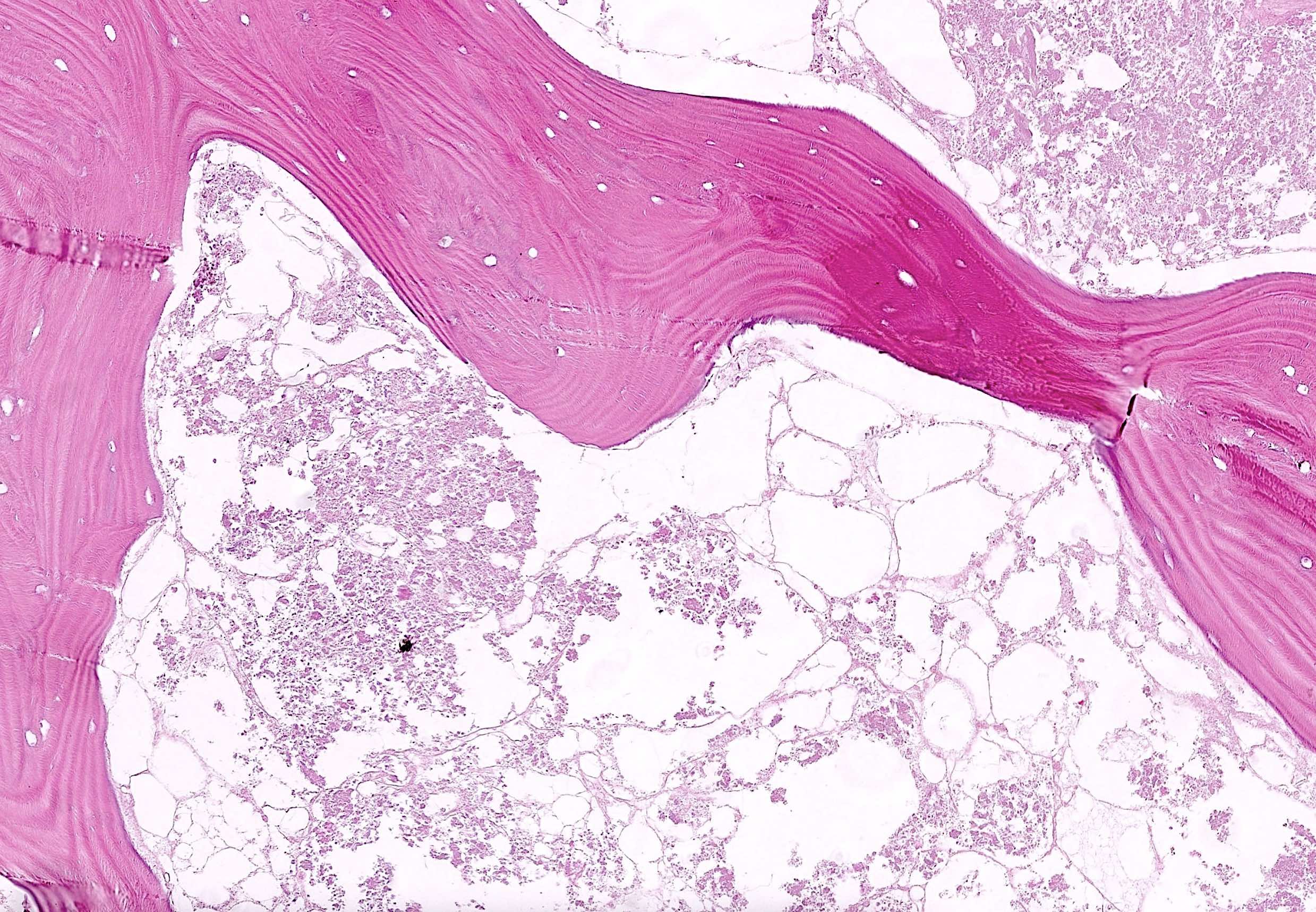
Microscopic (histologic) description
- Microscopic changes depend on stage of the ischemia (see Pathophysiology and Diagrams)
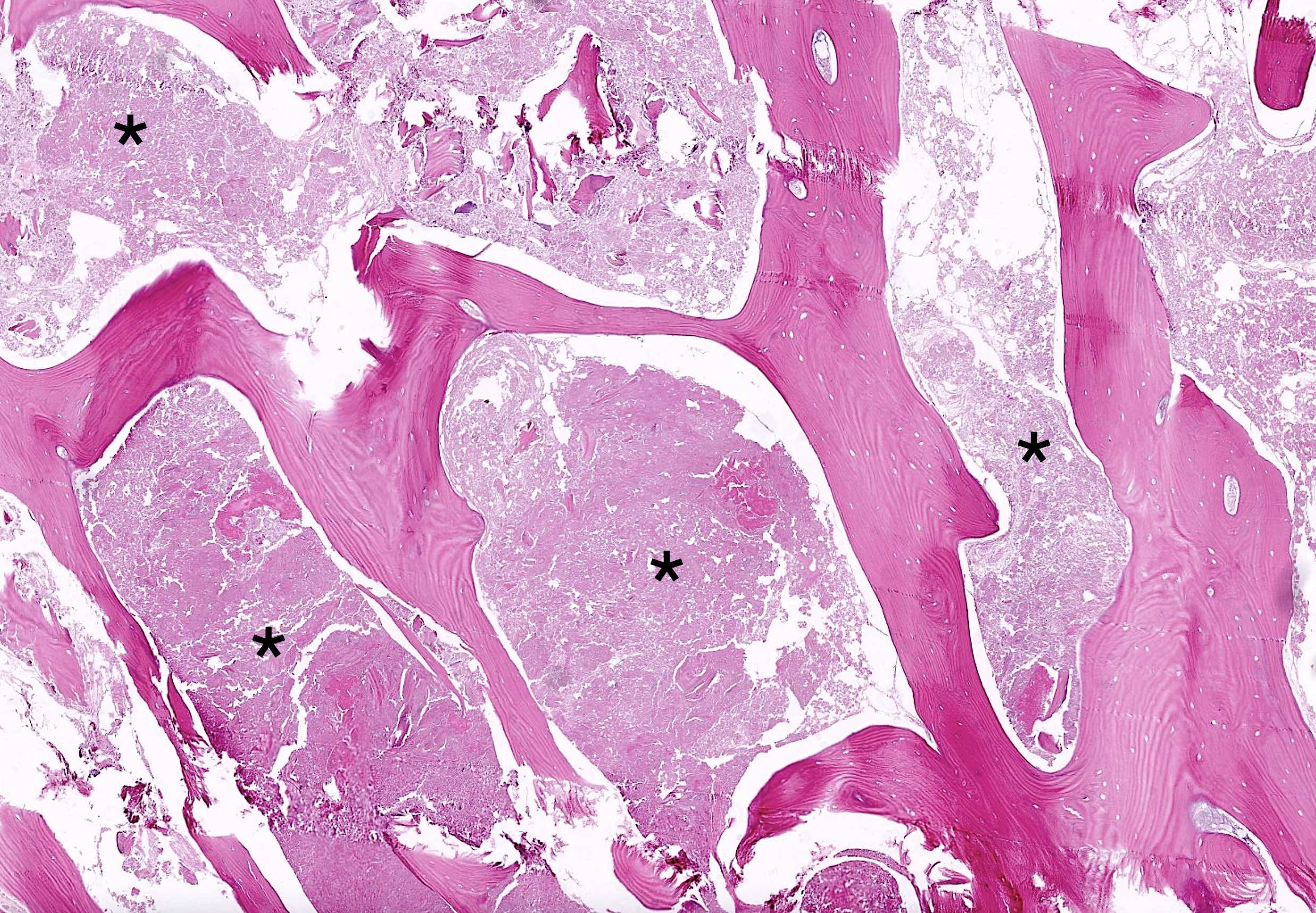
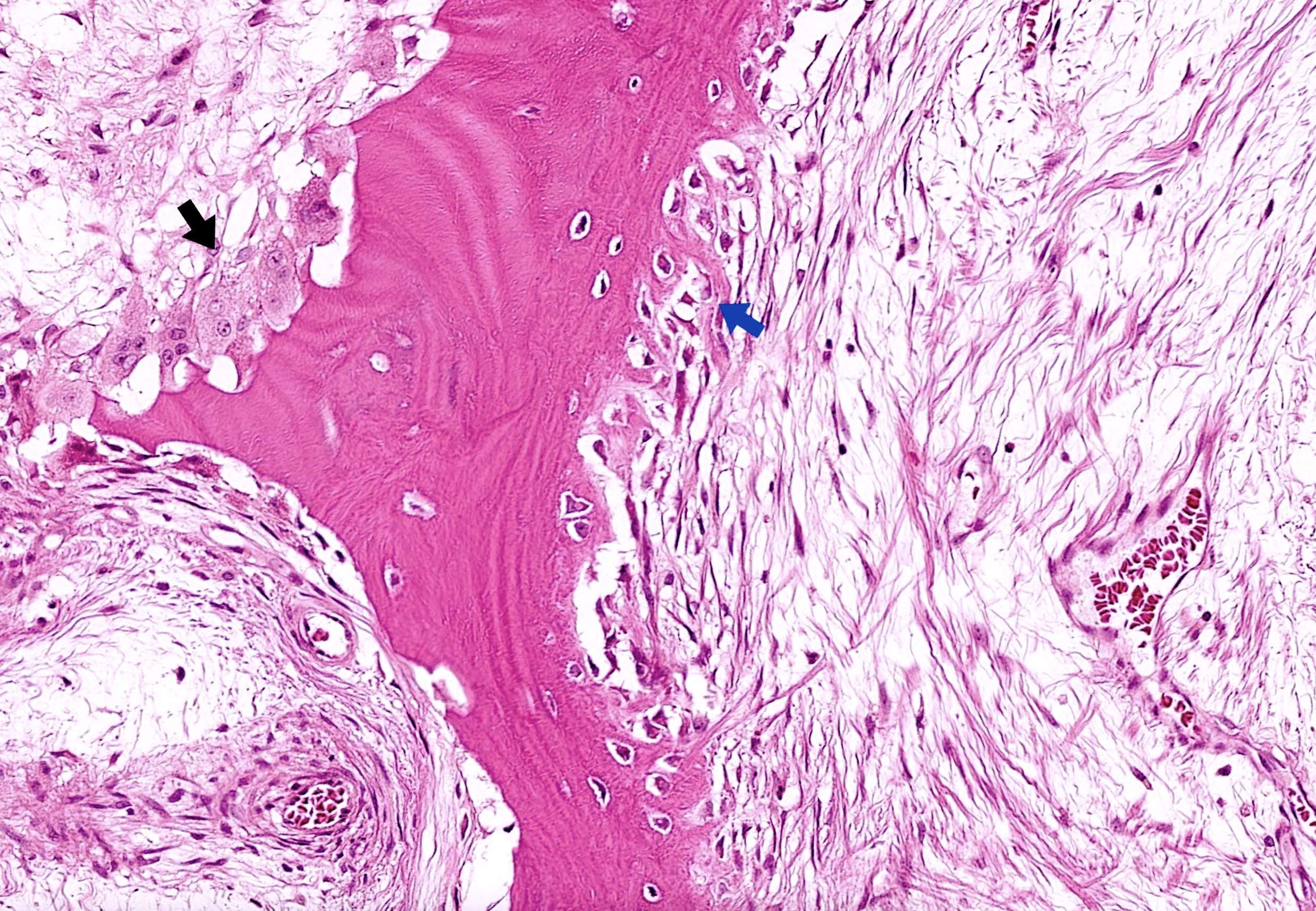
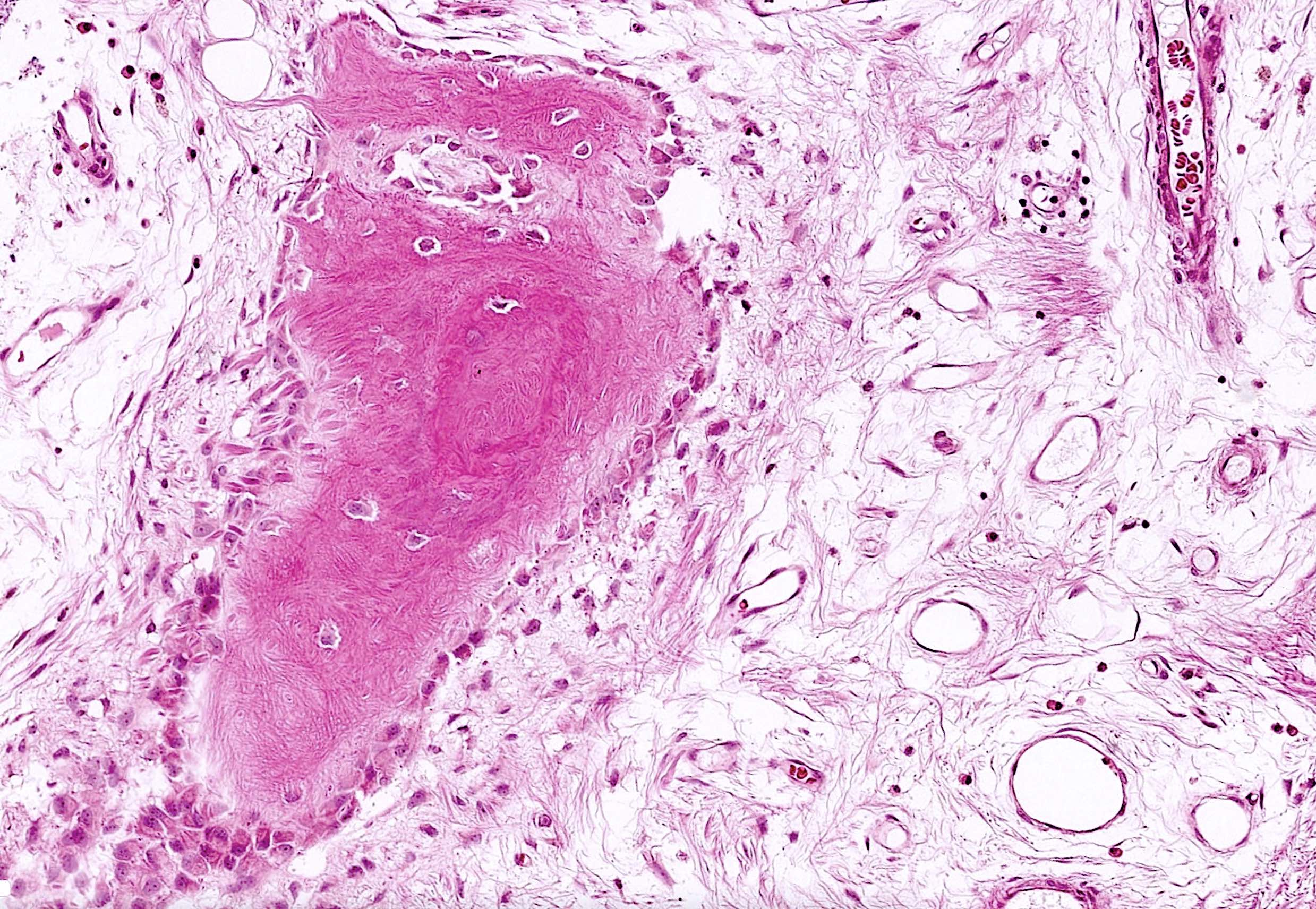
- Necrotic zone
- Earliest histological sign: diffuse coagulative necrosis of marrow elements including hematopoietic cells, adipocytes and endothelial cells
- Later, purplish aggregates of amorphous material appear in the marrow representing fat saponification (due to binding of released fatty acids with calcium)
- This contributes to the radiodensity on radiographs
- Osteocyte necrosis in cancellous bone trabeculae (Clin Cases Miner Bone Metab 2007;4:21)
- Manifests initially as pyknotic nuclei and later as uniformly empty osteocyte lacunae
- Loss of osteocytes may not be complete until 2 - 4 weeks after the onset of ischemia
- Pitfall: occasional empty lacunae are expected in interstitial lamellae of normal cortical bone with increasing age
- Another pitfall: overdecalcification of specimen results in artifactual loss of osteocytes
- Osteoblastic / osteoclastic activity is absent in the death zone due to the lack of blood supply
- Peripheral reparative zone
- Hyperemic border develops at the periphery of the necrotic zone as vascularized granulation tissue grows around the infarct and progresses into a rim of reactive bone
- Double line sign on MRI corresponds to the inner granulation tissue zone and outer rim of reactive bone
- Increased osteoclastic activity is evident, supported by the neovascularization
- Osteoblastic activity also evident with appositional bone formation seen over necrotic nonresorbed trabeculae (creeping substitution)
- This contributes to increased radiodensity on imaging
- Hyperemic border develops at the periphery of the necrotic zone as vascularized granulation tissue grows around the infarct and progresses into a rim of reactive bone
- Overlying articular cartilage
- Usually intact and smooth in early stages (in contrast to primary degenerative joint disease with secondary subchondral osteonecrosis)
- Later could be detached from the underlying necrotic bone (creating the crescent sign on radiology)
- Secondary degenerative joint disease eventually develops in advanced stage
- References: Radiographics 2014;34:1003, Clin Cases Miner Bone Metab 2007;4:21
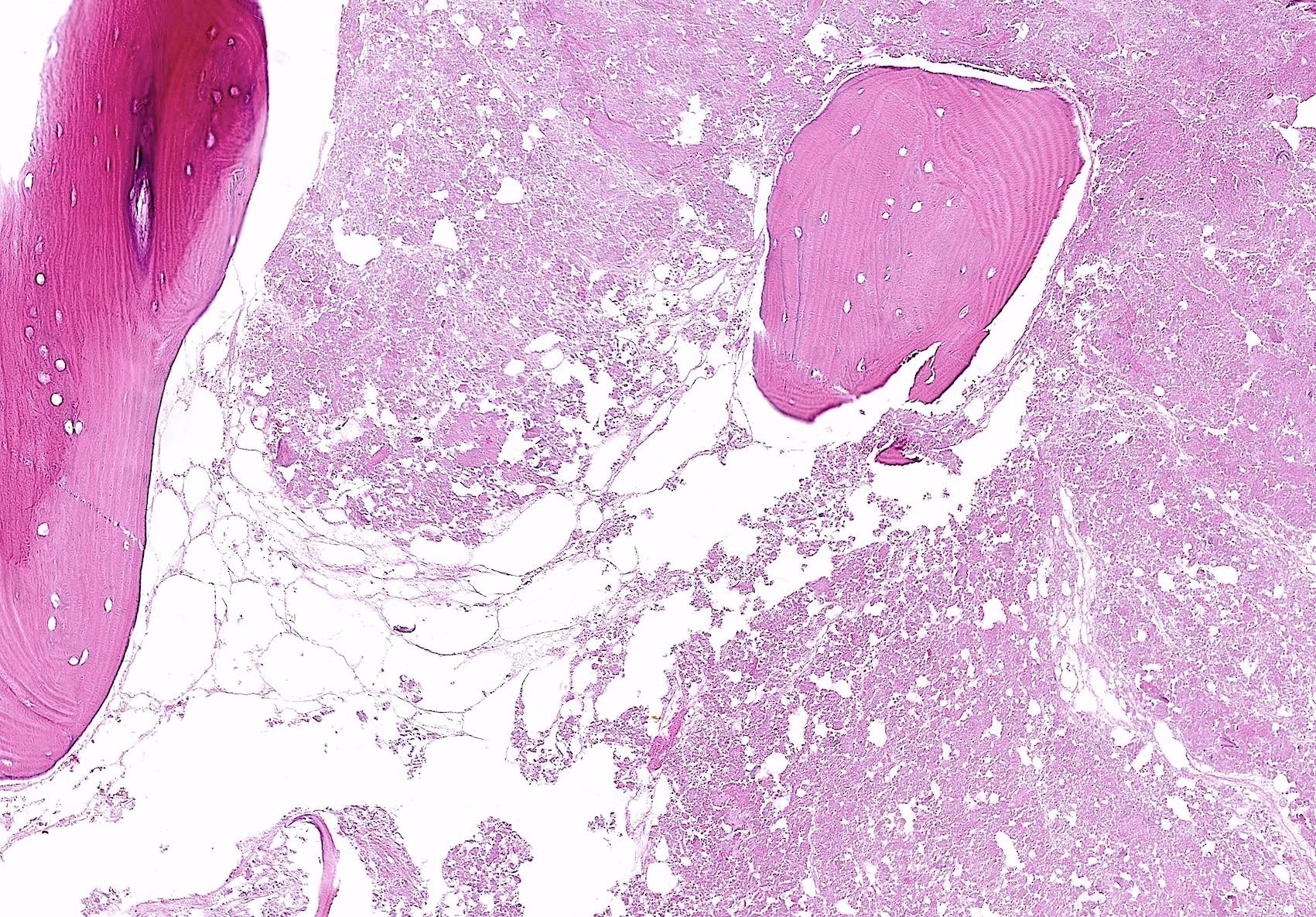
Microscopic (histologic) images
Positive stains
- Immunostains are not required for diagnosis
- Von Kossa stains the saponified fat black (may be compromised in decalcified sections)
Negative stains
- Not required for diagnosis
Sample pathology report
- Right head of femur, total hip replacement:
- Osteonecrosis of the femoral head (see comment)
- Subchondral fracture
- Comment: The morphological features corroborate the radiological findings.
Differential diagnosis
- Subchondral insufficiency fracture (Jpn J Radiol 2022;40:443):
- Sudden onset of hip or knee pain since it is a fracture
- Related to excessive stress to subchondral bone
- Risk factors include osteoporosis and overweight status
- Older term: spontaneous osteonecrosis of the knee (SONK)
- Osteonecrosis occurs as a secondary finding
- Degenerative joint disease:
- Older patients
- Progressive damage and loss of articular cartilage, subchondral bone thickening, osteophyte formation
- Large subarticular cysts may cause collapse of articular plate and secondary focal osteonecrosis
- Septic arthritis:
- Usually young adults and children
- Acute onset monoarticular joint pain with fever and swelling
- Infectious etiology from hematogenous spread or direct inoculation
- Neutrophilic collections within tissue and synovial fluid
- Neuropathic joint (Charcot joint):
- Destructive arthropathy in patients with peripheral neuropathies
- Rapid joint erosion with destructive features of osteoarthritis
Board review style question #1
A 38 year old woman, who is on long term glucocorticoid therapy for systemic lupus erythematosus (SLE), has undergone a total hip replacement. The microscopic appearance of her femoral head is shown in the image above. What is the diagnosis?
- Avascular necrosis
- Enchondroma
- Fracture callus
- Osteomyelitis
- Tumoral calcinosis
Board review style answer #1
A. Avascular necrosis. Systemic lupus erythematosus (SLE) and long term steroid use are known risk factors for avascular necrosis. Histologically, the marrow space contains saponified necrotic fat and the bone shows empty lacunae. The clinical context and morphology are wrong for the other options. Answer B is incorrect because of the absence of hyaline cartilage within the medullary cavity. Answer C is incorrect because of the absence of granulation tissue and bone remodeling. Answer D is incorrect because of the absence of acute inflammation. Answer E is incorrect because it is deposition of granular material in periarticular subcutaneous tissue.
Comment Here
Reference: Avascular necrosis
Comment Here
Reference: Avascular necrosis
Board review style question #2
Board review style answer #2
A. Femoral head. The image shows features of avascular necrosis, which is most common in the head of femur. Answers B, C, D and E are incorrect because these sites are less common.
Comment Here
Reference: Avascular necrosis
Comment Here
Reference: Avascular necrosis