Table of Contents
Definition / general | Essential features | Epidemiology | Sites | Pathophysiology | Clinical features | Laboratory | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Molecular / cytogenetics description | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Mruthyunjayappa S, Leal SM. Histoplasma capsulatum. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/microbiologyhcapsulatum.html. Accessed April 25th, 2024.
Definition / general
- Taxonomy:
- Class: Ascomycetes
- Order: Onygenales
- Family: Ajellomycetaceae
- Common species
- Histoplasma capsulatum var capsulatum: most common cause of histoplasmosis
- Histoplasma capsulatum var duboisii: cause of African histoplasmosis
Essential features
- Dimorphic mold
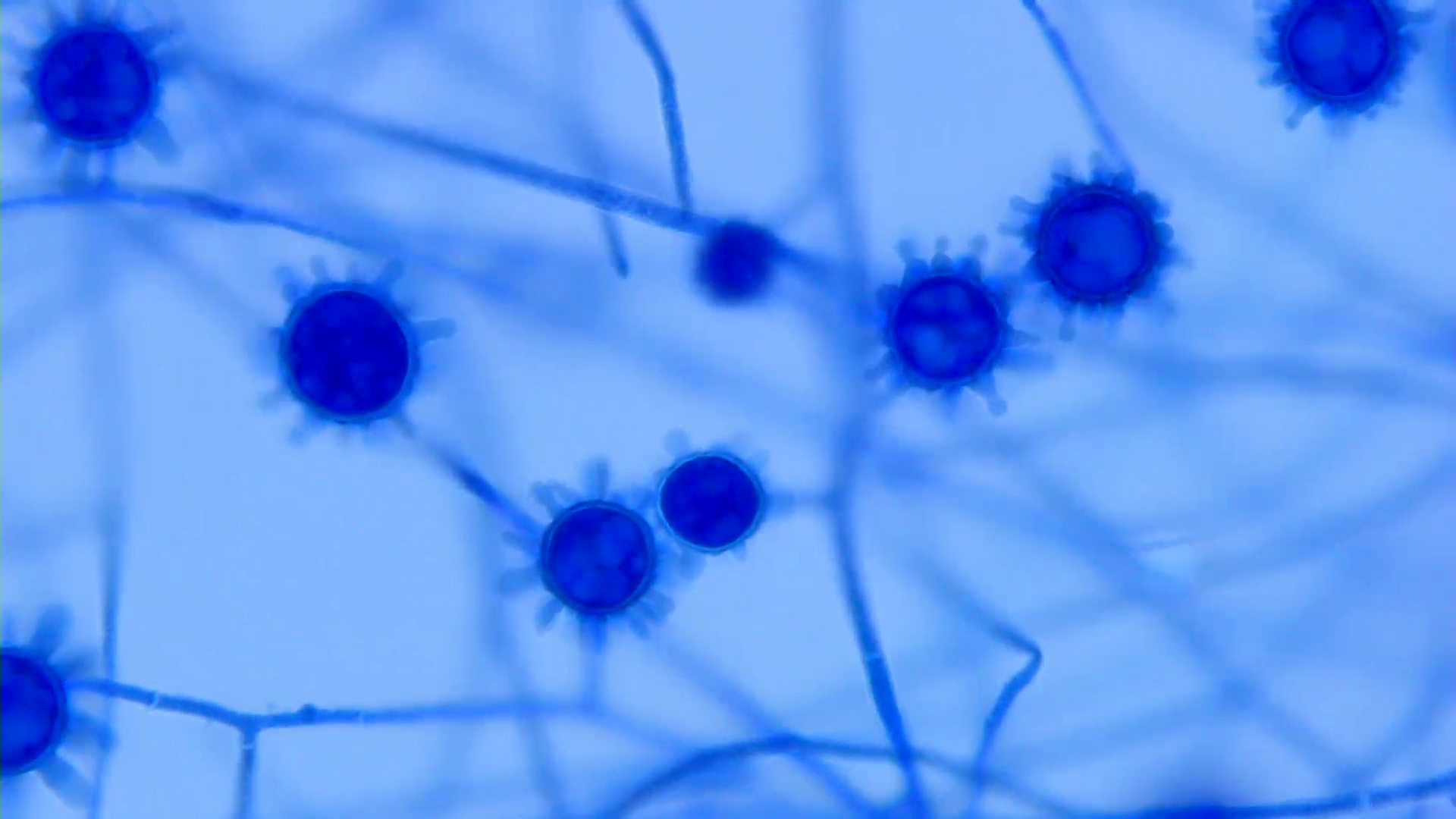
- Environmental: mold forming tuberculate macroconidia (ship's wheel)
- Body temperature: intracellular uniform small oval yeasts with rare narrow based budding
- Immunocompetent: tuberculosis-like illness with necrotizing granulomas
- Immunocompromised: disseminated disease with poor prognosis
Epidemiology
- Causal agent of histoplasmosis, a global disease, endemic to 6 continents
- Endemic in the valleys of the Ohio, Missouri and Mississippi rivers in the United States
- Internationally, within river valleys in North and Central America, Eastern and Southern Europe and parts of Africa, Eastern Asia and Australia
- Environmental niche includes nitrogen rich soils and attics with bird or bat droppings
- Disseminated infections in immunocompromised individuals
- Reference: Clin Chest Med 2017;38:403
Sites
- Lungs: solitary nodules can mimic neoplasms
- Mediastinal lymph nodes: can mimic lymphoma
- Skin: resembles Molluscum contagiosum
- Tongue: ulcerative lesion with heaped edges
- Bone marrow: anemia of unknown cause
- Disseminated disease: immunocompromised
Pathophysiology
- Inhaled fungal spores germinate into yeasts
- Alveolar macrophages and neutrophils are unable to clear infection
- Yeasts persist within macrophages and spread to lymphatics
- If immunocompetent, T cell activation promotes effective granuloma formation
- If compromised, organism continues to proliferate within reticuloenothelial system and disseminates
- Reference: Infect Dis Clin North Am 2016;30:207
Clinical features
- Pulmonary histoplasmosis:
- Asymptomatic infection or self limited respiratory illness
- Acute disease is characterized by fever, chills, dyspnea and cough
- Subacute disease presents as persistent community acquired pneumonia, despite standard antibiotic treatment
- Chronic disease presents as productive cough, low grade fever, weight loss and night sweats (Infect Dis Clin North Am 2016;30:207)
- Mediastinal histoplasmosis:
- Mediastinal adenitis: most commonly asymptomatic and self limited, with fever and adenopathy
- Mediastinal granuloma: cluster of necrotic lymph nodes often paratracheal or subcarinal that are coalesced into a semiliquid conglomerate mass (caseation necrosis)
- Fibrosing mediastinitis: dense fibrotic mass with obstruction of pulmonary vessels or airways (Infect Dis Clin North Am 2016;30:207)
- Progressive disseminated histoplasmosis:
- Immunocompromised patients are at increased risk
- Fever, fatigue, night sweats, dyspnea and weight loss
- Dissemination to the liver, spleen, gastrointestinal tract and bone marrow (Infect Dis Clin North Am 2016;30:207)
Laboratory
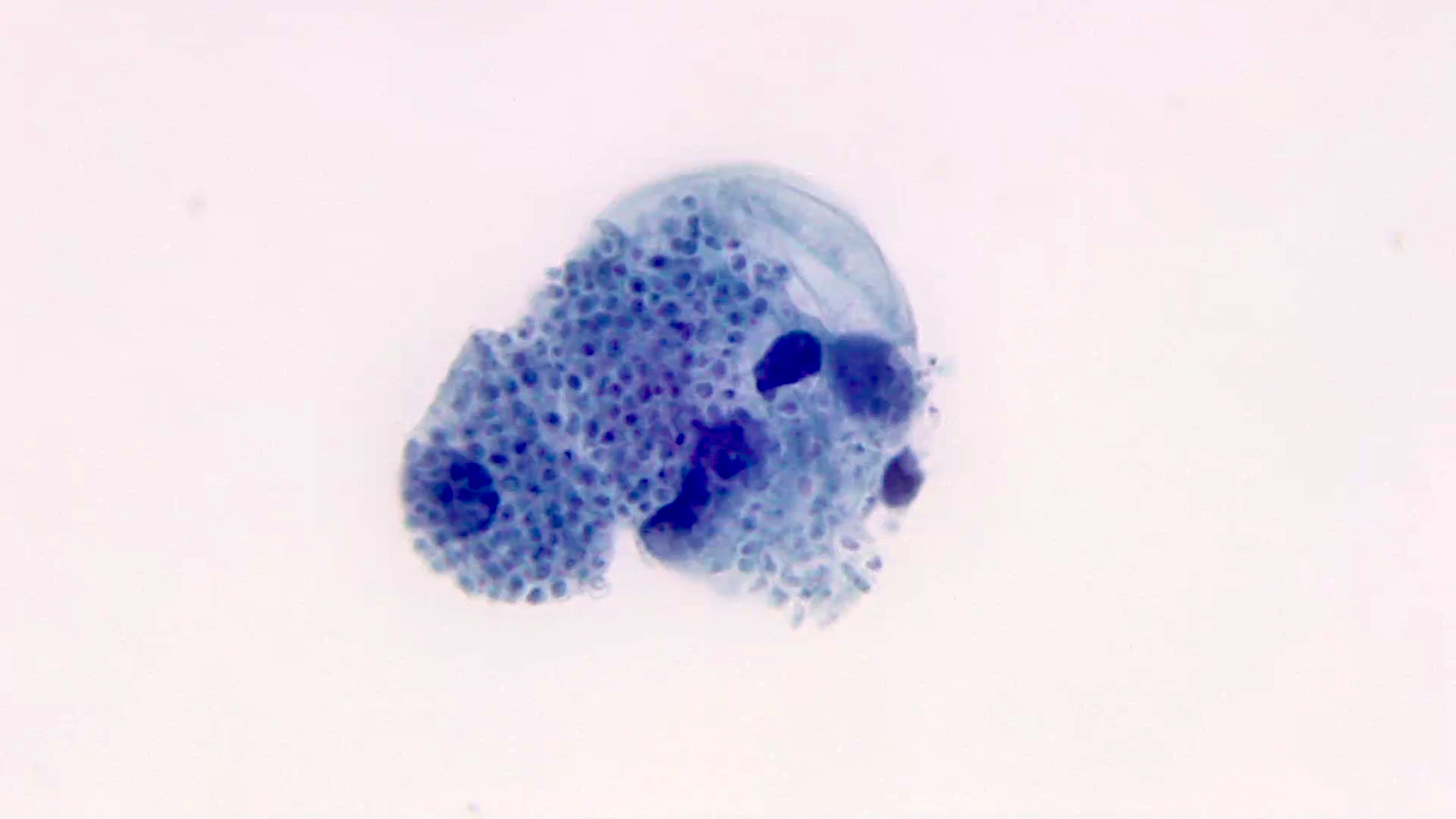
- Direct exam shows small uniform, narrow based budding yeasts in clusters within host cells
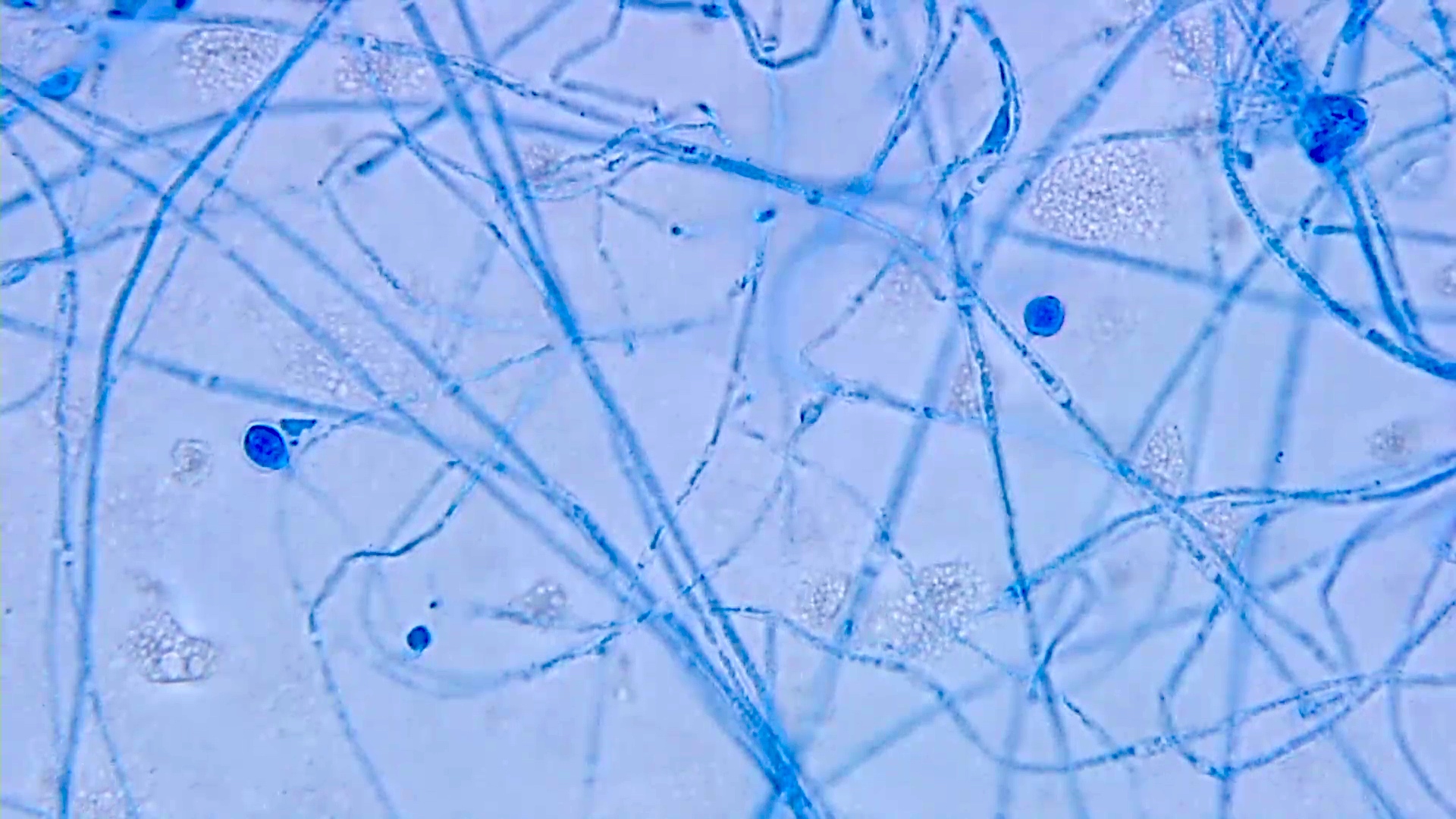
- Slow growing yeasts that transition to a fluffy white mold colony within 1 - 6 weeks
- Early tape prep will show yeast cells (2 - 4 μm), some of which are transitioning into hyphal forms
- Early hyphae may show aleurioconidia (lollipop-like structures; 2 - 4 μm) similar to Blastomyces and Paracoccidioides
- Later cultures will show characteristic large tuberculate macrocondia (8 - 16 μm)
- Molecular confirmation using the Gen-Probe or other technique is essential to rule out nonpathogenic environmental molds that morphologically mimic Histoplasma, such as Sepedonium spp
- Histoplasma galactomannan antigen tests on urine and serum enable noninvasive diagnosis of active disease
- Enzyme immunoassay; quantitative result
- Best for acute or disseminated disease, including HIV patients without detectable antibodies against the fungus
- Very low sensitivity for old granulomas
- Known cross reactivity with Blastomyces, Paracoccidioides and antigens from several other fungi (Clin Chest Med 2017;38:403)
- Serology tests are available but have mostly been replaced by screening for antigen in urine
Case reports
- 22 year old HIV negative African woman with disseminated histoplasmosis caused by Histoplasma capsulatum var duboisii (J Mycol Med 2015;25:159)
- 41 year old immunocompetent man with acute pulmonary histoplasmosis infection (Rev Mal Respir 2020;37:422)
- 42 year old man with disseminated histoplasmosis infection presenting as adrenal insufficiency (Diagn Cytopathol 2011;39:446)
- 48 year old woman with psoriasis, developing cholestasis and disseminated histoplasmosis (BMC Gastroenterol 2020;20:141)
- 62 year old man with an untreated myeloproliferative neoplasm, presenting with an altered mental status (Cureus 2019;11:e4238)
Treatment
- Asymptomatic mild disease and incidental old granulomas (histococcomas) may not require treatment
- Treatment may last from 6 weeks to 12 months
- Immunosuppressed individuals may require lifelong treatment
- Itraconazole is first line therapy
- Liposomal amphotericin B is added for severe disease
- Reference: Semin Respir Crit Care Med 2015;36:729
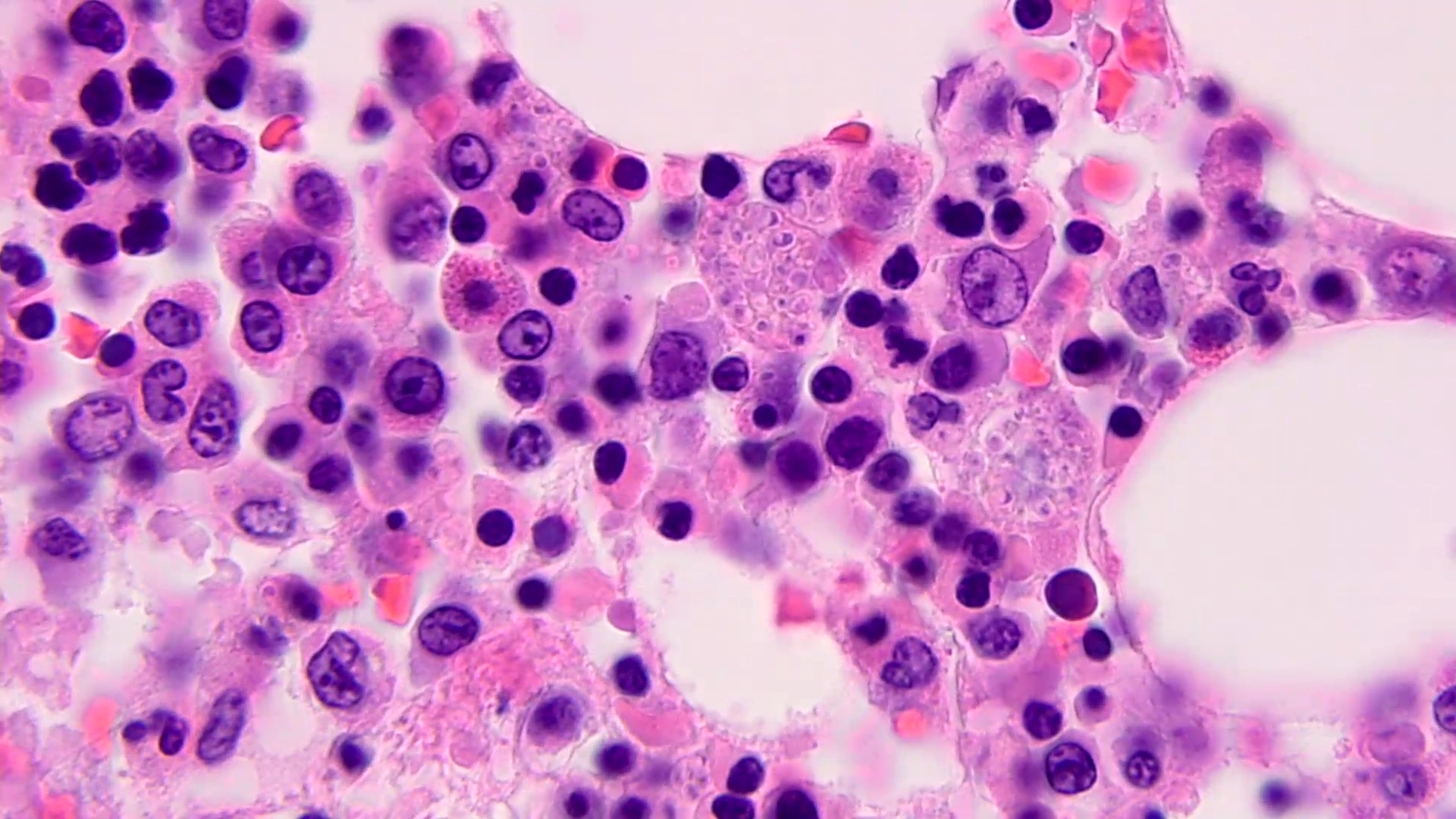
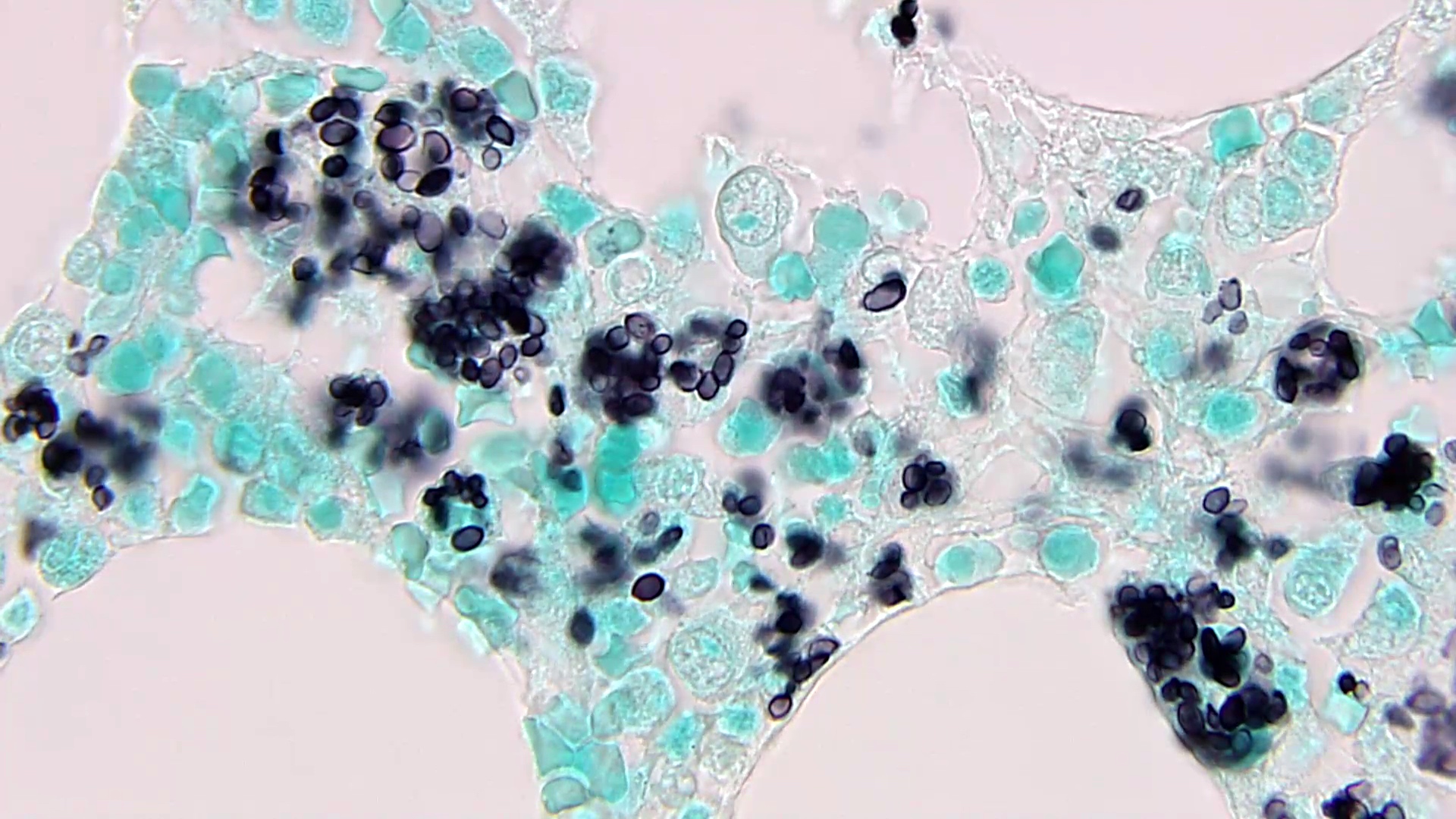
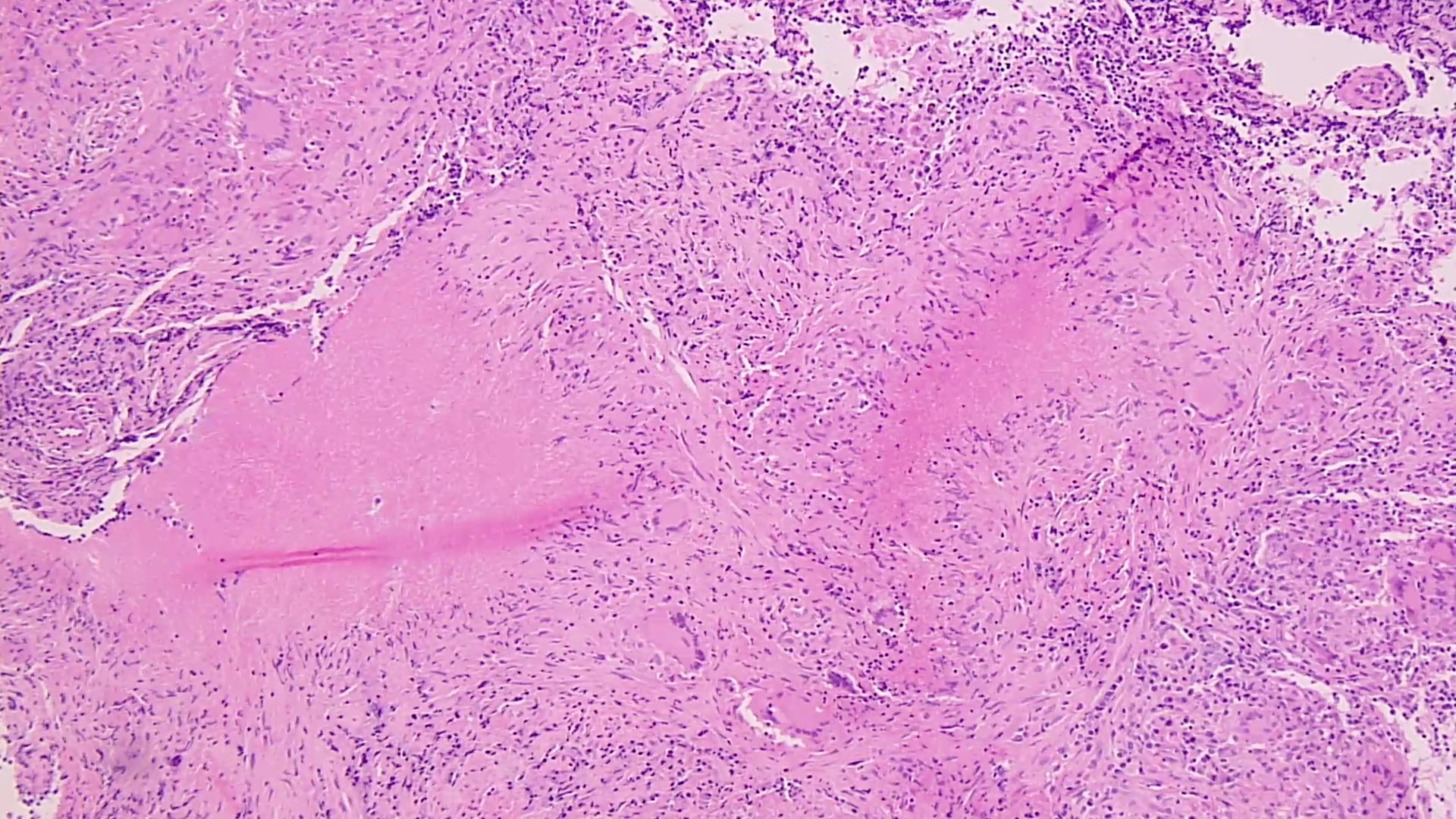
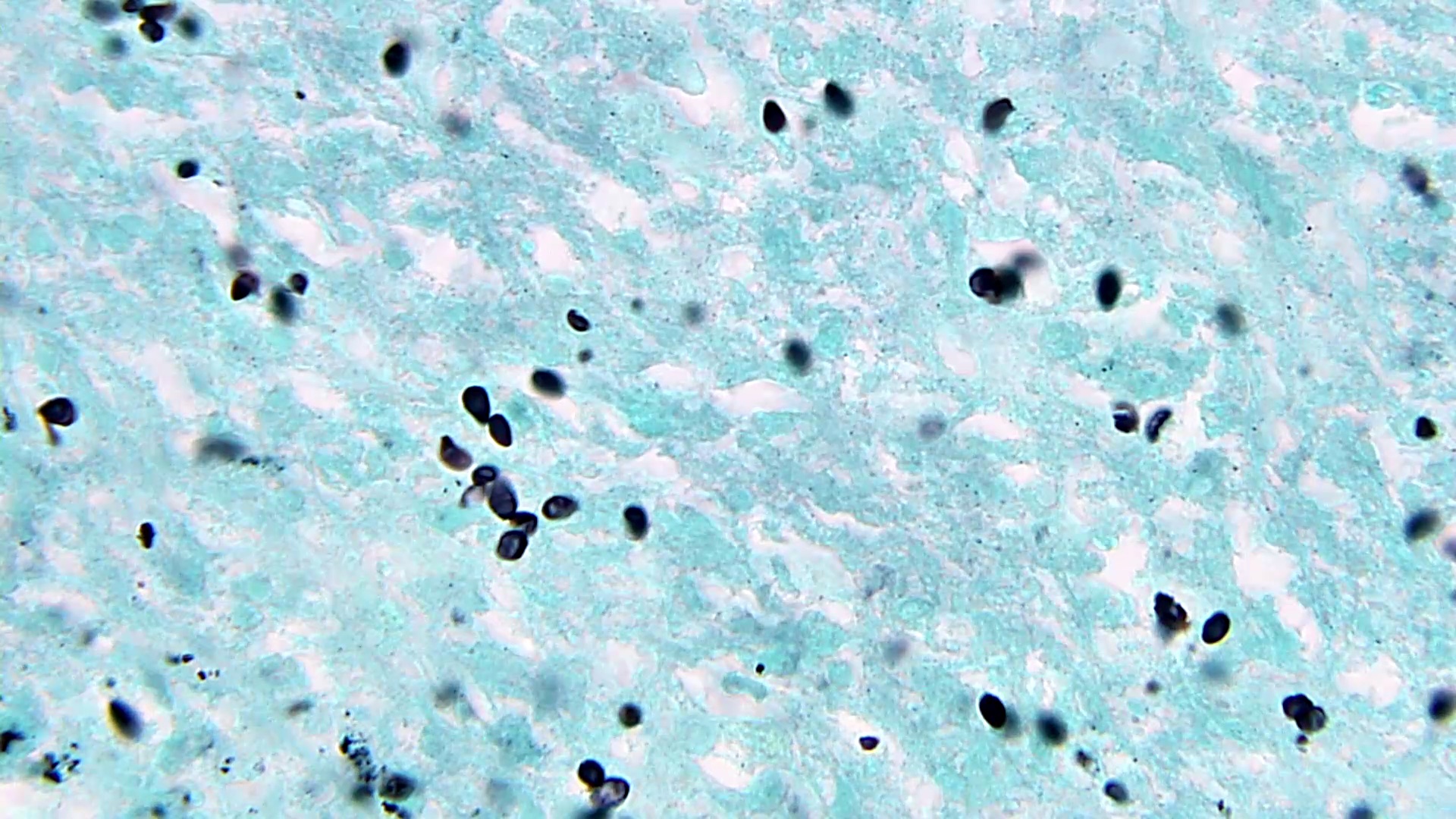
Microscopic (histologic) description
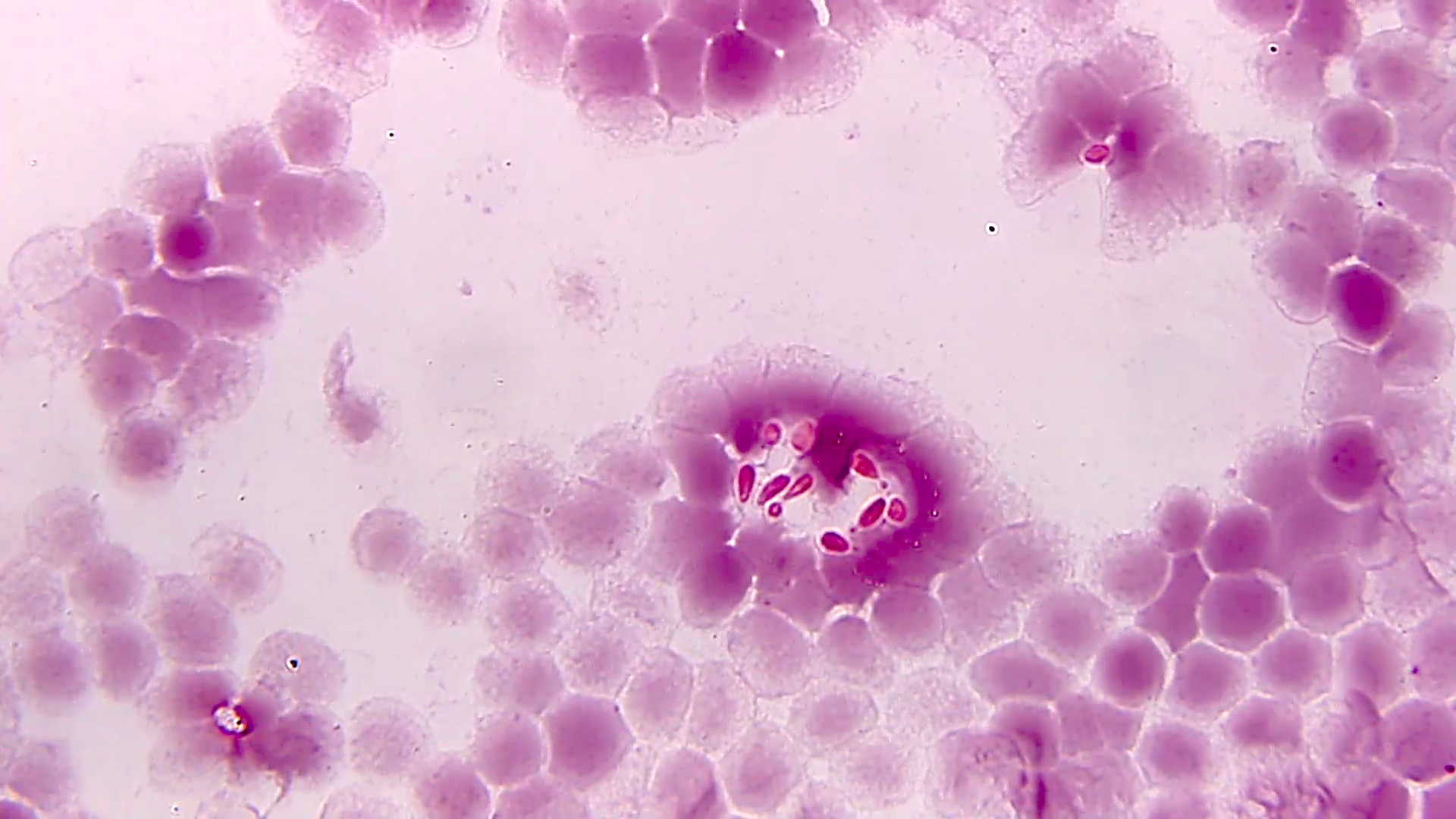
- Small uniform oval, narrow based budding yeasts with eccentric acorn-like nuclei clustered within histiocytes (intracellular)
- Granulomatous immune response, ranging from nonexistent in immunocompromised individuals to large necrotizing forms
- Organisms may remain clustered beyond the death of their host cell
- Difficult to see organisms on H&E; retraction artifact characteristically present
- GMS, PAS stains are helpful to highlight organisms
- Tissue mimics include Candida glabrata, Talaromyces marneffei and amastigotes of Leishmania and Trypanosoma spp
- Yeasts that do not form pseudohyphae elicit neutrophilic inflammation; T. marneffei yeasts undergo fission characterized by septations separating dividing cells; Leishmania and Trypanosoma amastigotes exhibit a second dot (kinetoplast) within each cell
- Reference: Clin Chest Med 2017;38:403
Microscopic (histologic) images
Contributed by Sixto M. Leal, Jr., M.D., Ph.D.
Molecular / cytogenetics description
- Hologic Gen-Probe hybridization assay (AccuProbe) is routinely used to confirm diagnosis from culture
- Nucleic acid hybridization technique: single-stranded DNA probe with a chemiluminescent label binds to fungal rRNA to form a stable DNA:RNA hybrid
- Internal transcribed spacer (ITS) / 28S rRNA sequencing may identify organisms to the species level
- Reference: J Fungi (Basel) 2019;6:1
Differential diagnosis
- Acute illness:
- Other causes of community acquired pneumonia
- Chronic illness:
- Tuberculosis, infection with nontuberculous mycobacteria:
- Acid fast organisms
- Blastomycosis:
- Broad based budding yeasts with refractile double layered cell walls
- Coccidioidomycosis:
- Thick walled spherules with endospores in tissue
- Sarcoidosis:
- Diagnosis of exclusion after ruling out all the infectious agents
- Tuberculosis, infection with nontuberculous mycobacteria:
Board review style question #1
An outdoor enthusiast in the Midwest United States develops flu-like symptoms with fever, headache, muscle pain and a cough. Azithromycin (Z pack) treatment for community acquired pneumonia does not alleviate symptoms. An Xray shows diffuse bilateral pneumonia and CBC shows anemia. After 2 weeks, sputum cultures show small tan-white yeast-like colonies with peripheral mold-like features. A tape prep shows a mixture of small uniform oval yeast and hyphae with rare aleurioconidia. What is the most likely cause of respiratory illness?
- Aspergillus fumigatus
- Candida glabrata
- Coccidioides immitis
- Histoplasma capsulatum
Board review style answer #1
D. Histoplasma capsulatum. Coccidioides and Aspergillus species do not form characteristic yeast-like colonies. Candida glabrata only forms yeasts without hyphae or pseudohyphae.
Comment Here
Reference: Histoplasma capsulatum
Comment Here
Reference: Histoplasma capsulatum
Board review style question #2
A patient with a prior history of histoplasmosis presents with a recurrent inflammatory bowel disease flare requiring corticosteroids and immunosuppression with biologic agents. While on treatment, she develops dyspnea, ulcerative lesions on the tongue and Molluscum contagiosum-like lesions on the skin. You are concerned about disseminated histoplasmosis and would like to consider noninvasive diagnostic options. What test may meet this niche?
- Beta (D) glucan test
- Cryptococcal GXM antigen test
- Fungal culture performed on bronchoalveolar lavage fluid (BAL)
- Urine galactomannan antigen test
Board review style answer #2
D. Urine galactomannan antigen test. BAL specimens are invasive, beta glucan is a panfungal marker lacking specificity for Histoplasma and the cryptococcal antigen test has high specificity for Cryptococcus spp. Urine Histoplasma galactomannan antigen test can be helpful in this situation to determine the presence or absence of the organism and quantitatively track treatment progression.
Comment Here
Reference: Histoplasma capsulatum
Comment Here
Reference: Histoplasma capsulatum