Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Electron microscopy description | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Asghari T, Wureshi M, Ud Din N. Tumoral calcinosis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/bonemetcalcification.html. Accessed September 16th, 2025.
Definition / general
- Tumor-like deposits of calcium hydroxyapatite in soft tissue surrounding major joints
Essential features
- Nonneoplastic condition, mimics osteocartilaginous tumors
- Can be primary (familial or sporadic) or secondary (tumoral calcinosis-like lesions) (World J Clin Cases 2014;2:409)
- Painless periarticular subcutaneous masses involving large joints and occurring in the first 2 decades
- Characterized by lobular deposits of amorphous granular material (hydroxyapatite crystals) with basophilic calcifications
- Histiocytic granulomatous response to crystals
- Treated with surgical excision, secondary form requires treatment of underlying cause
Terminology
- Coined by Inclan in 1943
- Synonyms: lipid calcinosis, tumoral lipocalcinosis, calcifying collagenolysis, calcifying bursitis, hip stone disease, Kikuyu bursa
Epidemiology
- Usually affects younger age groups in the first and second decades of life (Acta Orthop Belg 2008;74:837)
- Rare after 50 years
- Familial form has predilection for young black males (African Americans) (Genet Couns 2008;19:183)
- Secondary form is associated with trauma, scleroderma, osteoarthritis and diseases affecting calcium phosphate metabolism, including chronic renal failure, milk alkali syndrome, hypervitaminosis D, etc.
Sites
- Involves periarticular subcutaneous tissue of large joints
- Attached to the underlying fascia, muscle or tendon, unrelated to bone and joint
- Most commonly occurs in elbows, hips and shoulders (J Dermatol 1996;23:545)
- Solitary lesion in sporadic type
- Often multicentric and bilateral lesions in familial type
Pathophysiology
- Familial tumoral calcinosis has 2 types:
- Autosomal recessive hyperphosphatemic type:
- Characterized by germline mutations in the FGF23, GALNT3 or KL gene (J Invest Dermatol 2010;130:652)
- These mutations prevent degradation of fibroblast growth factor 23 (FGF23), which is involved in phosphate homeostasis
- Autosomal recessive normophosphatemic type:
- Characterized by SAMD9 genetic mutation
- Mutation results in deficiency of the associated interferon γ and tumor necrosis factor α responsive protein
- Autosomal recessive hyperphosphatemic type:
- Sporadic tumoral calcinosis is idiopathic (most common form)
- Secondary tumoral calcinosis is caused by underlying disorder (Am J Surg Pathol 2007;31:15)
Etiology
- Secondary form is associated with various predisposing conditions, including chronic renal failure (typically associated with secondary hyperparathyroidism), primary hyperparathyroidism, systemic sclerosis, scleroderma, dermatomyositis, sarcoidosis, osteoarthritis and congenital deformities (Rheumatol Int 2005;25:55)
Diagrams / tables
Clinical features
- Painless, firm, subcutaneous calcified masses in the periarticular soft tissues, especially along extensor surfaces (J Bone Joint Surg Am 1967;49:721)
- Subcutaneous deposits tend to be large and dense
- May be associated with papular and nodular skin lesions
- Dermal deposits are multiple, small and globular in type
- Both familial forms of tumoral calcinosis may be associated with bony abnormalities, including calcifications in long bones and cranium, ocular and dental abnormalities
Diagnosis
- Plain Xray, CT scan and MRI are helpful imaging modalities in combination with clinical findings
Laboratory
- Normal / elevated serum phosphate levels in sporadic type
- Serum calcium levels are usually normal in sporadic type (J Endocrinol Invest 2020;43:173)
- Elevated serum phosphate and vitamin D levels in familial, hyperphosphatemic type
- Normal serum phosphate and vitamin D levels in familial, normophosphatemic (NFTC) type
- Secondary form has impaired calcium and phosphate levels depending on the type and extent of underlying metabolic disease
Radiology description
- Plain radiographs show rounded, multilobulated cloud-like calcifications in periarticular area (Skeletal Radiol 1995;24:573)
- CT scan reveals solid or cystic appearance with rounded opacities separated by radiolucent lines (fibrous septa) and multiple fluid calcium levels due to calcium layering (sedimentation sign) in some nodules (Acta Biomed 2019;90:587)
- MRI shows more prominent sedimentation sign and variable signal intensity (Br J Radiol 1974;47:734)
- Low intensity signal in more calcified portions and high intensity signal in cystic areas in T2 weighted sequences
- Mild contrast enhancement in areas of septation
- Radionuclide bone scan may show intense uptake in the calcific masses
Radiology images
Prognostic factors
- Benign condition with good prognosis (Arch Craniofac Surg 2018;19:287)
- Recurrence may occur in familial forms
- Prognosis in secondary type depends on the treatment of causative systemic condition
Case reports
- 8 year girl presented with multiple skin nodules over lateral aspects of both feet (BMJ Case Rep 2019;12:e227083)
- 11 year girl presented with recurrent multiple subcutaneous masses around the right elbow and hip regions (Osteoporos Int 2022;33:309)
- 55 year old woman presented with limited range of motion in the right upper extremity (J Med Case Rep 2017;11:304)
- 58 year old man presented with painless, palpable solid mass restricting the range of motion of both elbows (Acta Orthop Traumatol Turc 2021;55:281)
- 59 year old woman with painful swelling over the right preauricular region (BMC Oral Health 2019;19:138)
Treatment
- Surgical excision is the primary treatment for sporadic and familial forms (Am J Orthop (Belle Mead NJ) 2011;40:E170)
- Medical treatment to control the hyperphosphatemia (e.g., a low phosphate diet and oral administration of phosphate binders) is an important adjunct to surgical excision (Front Endocrinol (Lausanne) 2020;11:293)
- Targeted therapies to decrease intestinal absorption and increase renal excretion of phosphate are helpful in familial type (JBMR Plus 2019;3:e10185)
- Secondary form also requires medical treatment of underlying disease
Clinical images
Gross description
- Firm, rubbery, unencapsulated, multinodular to multicystic mass
- Size varies from 5 - 30 cm
- Cut surface shows cystic spaces filled with chalky, milky liquid or semisolid gritty material
- Fibrous tissue separates cavities
Frozen section description
- Can be diagnosed on frozen section in correlation with complete clinical, radiological and serological information (Neurosurgery 2005;57:E596)
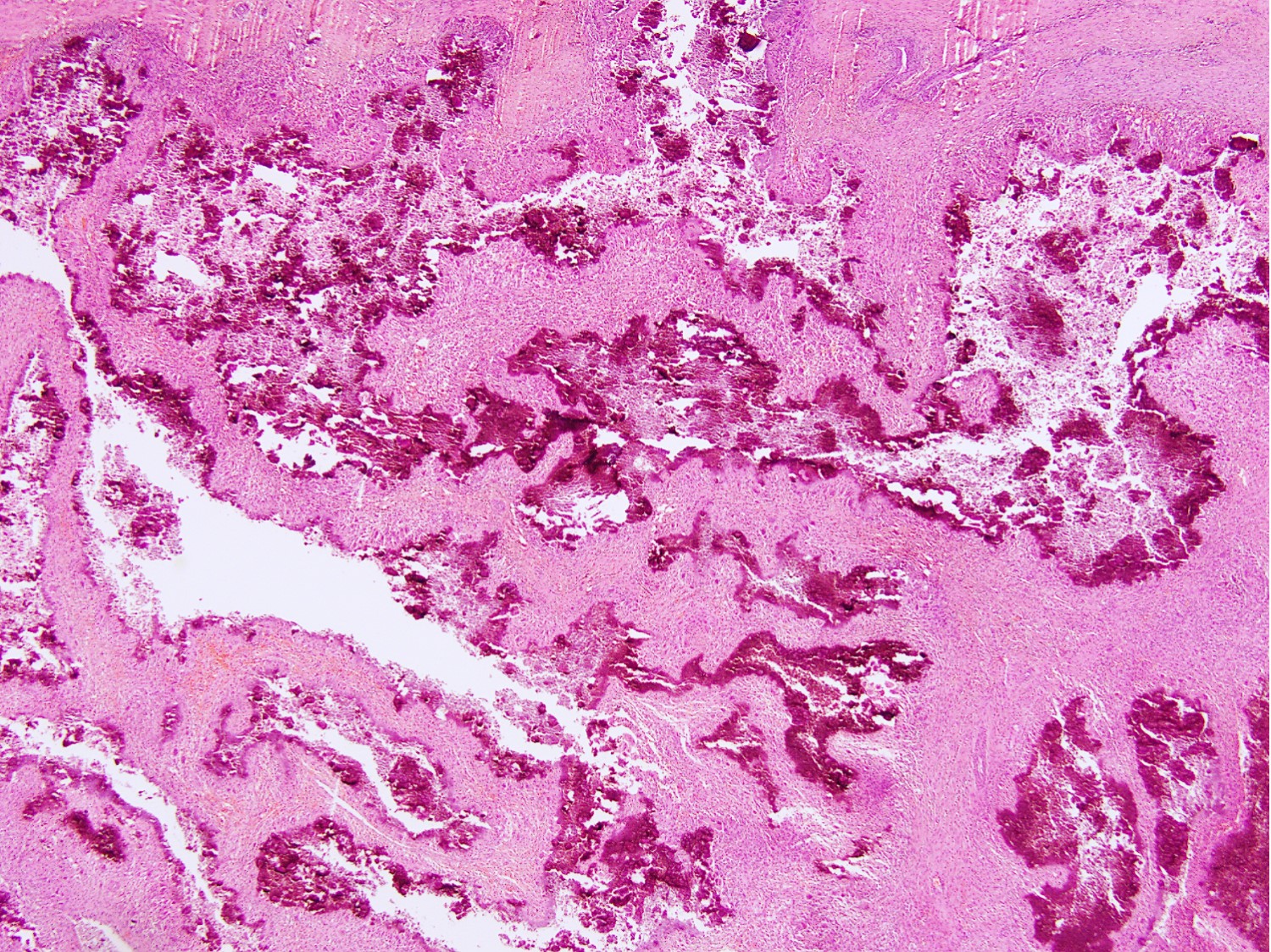
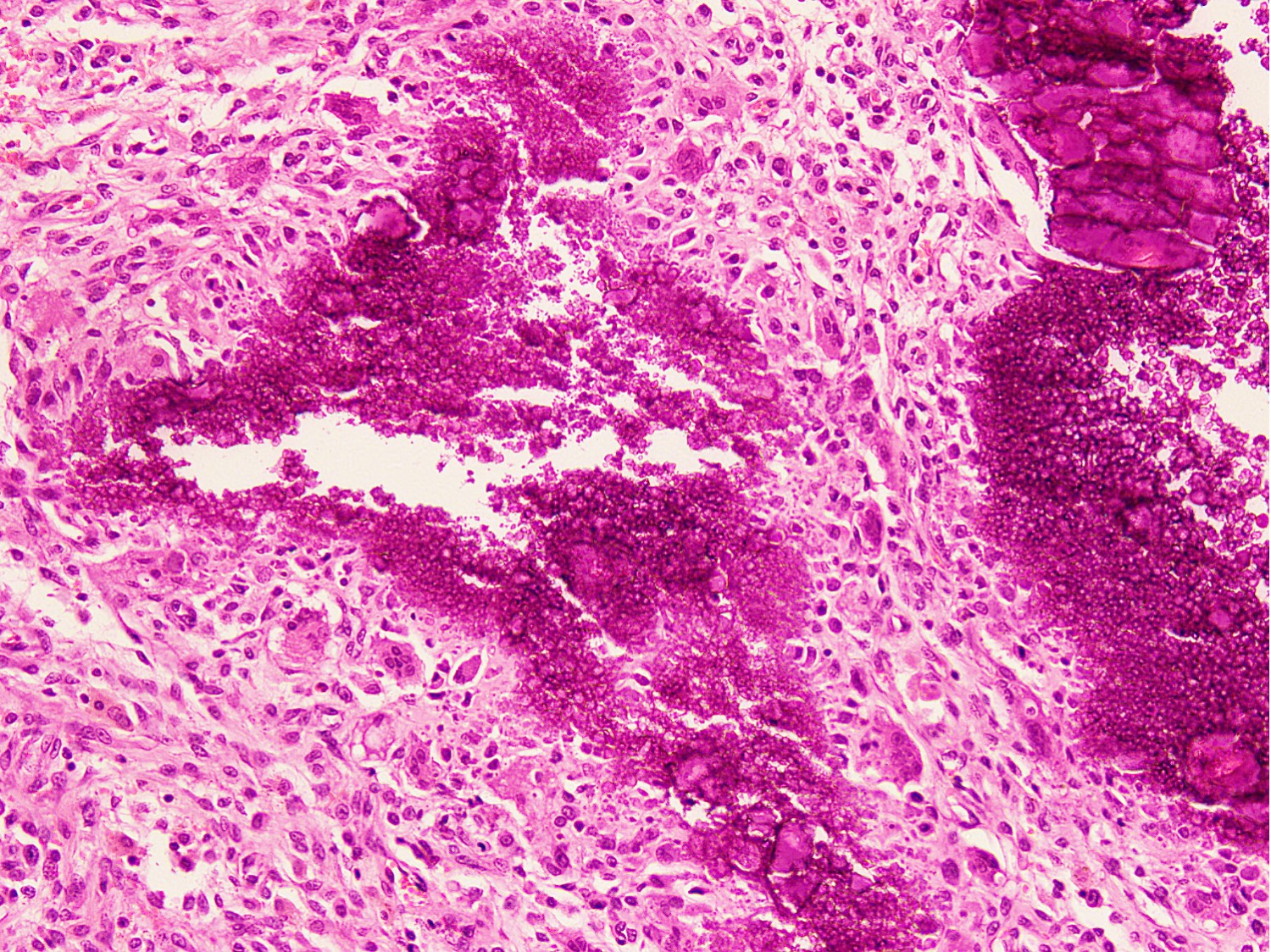
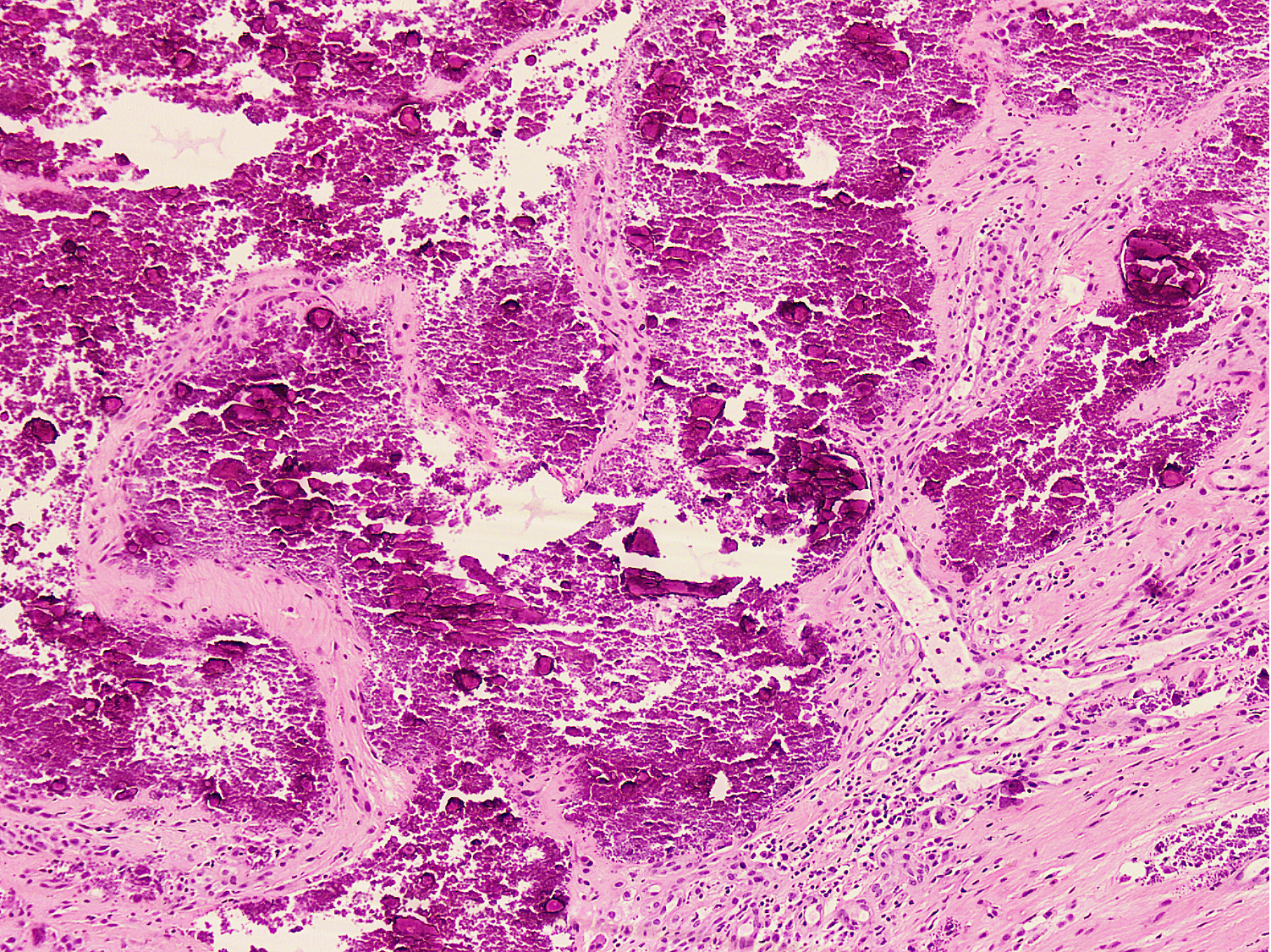
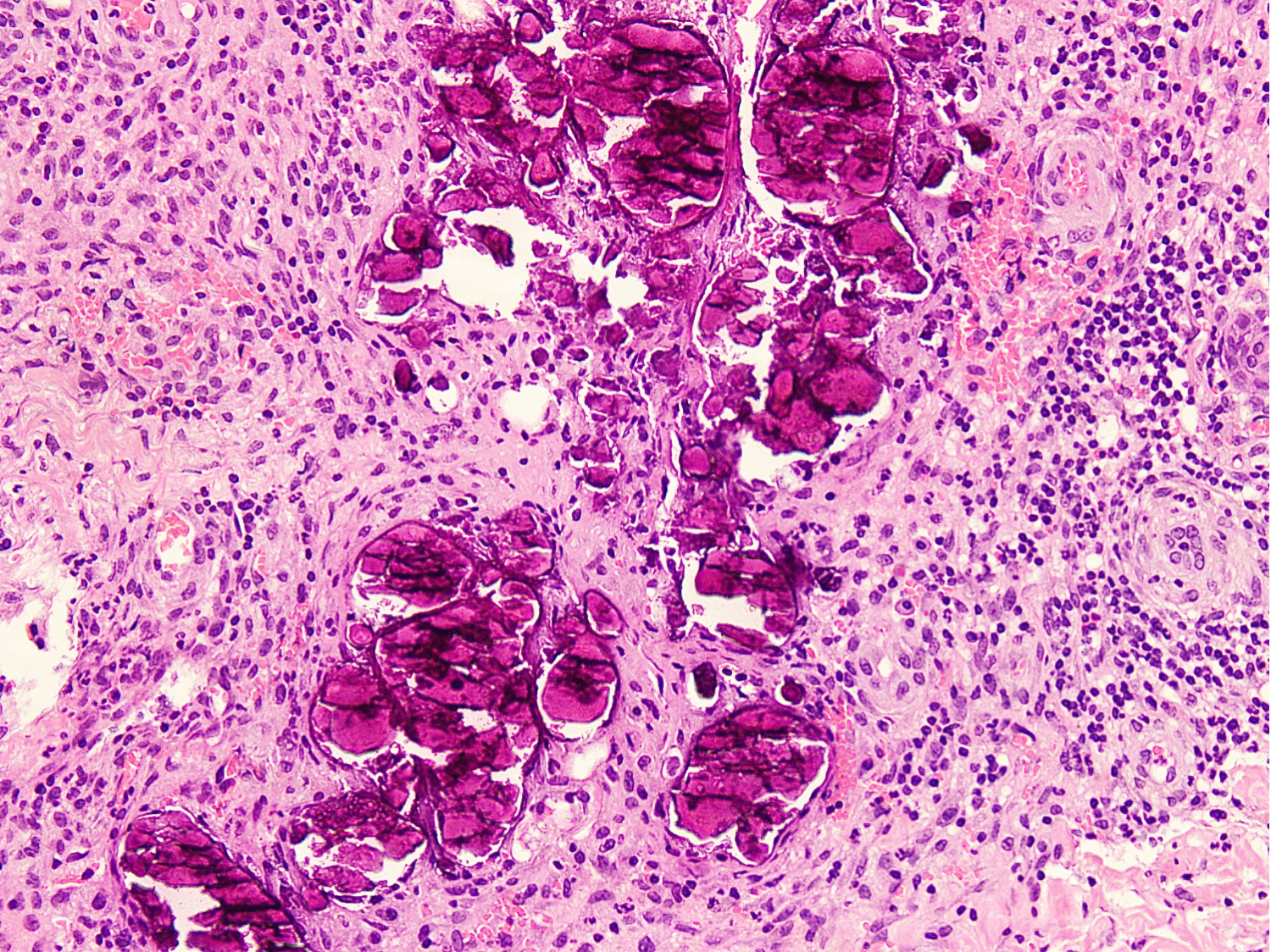
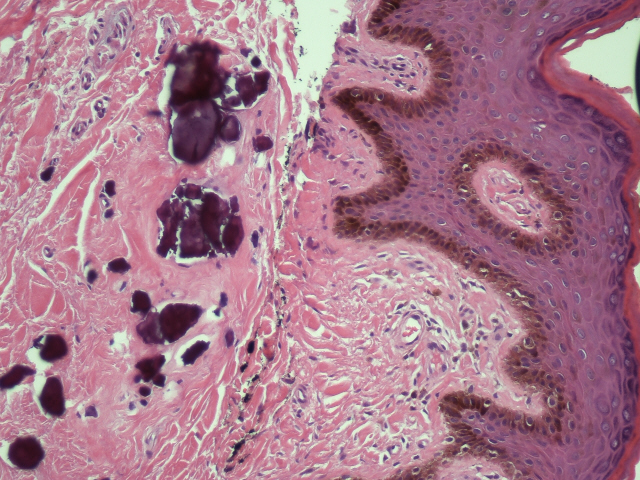
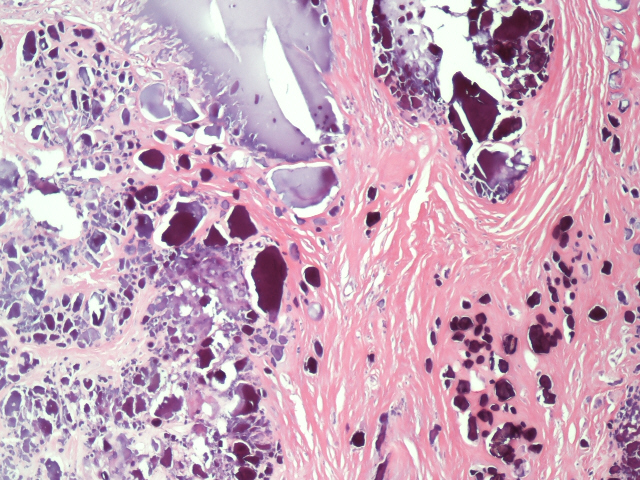
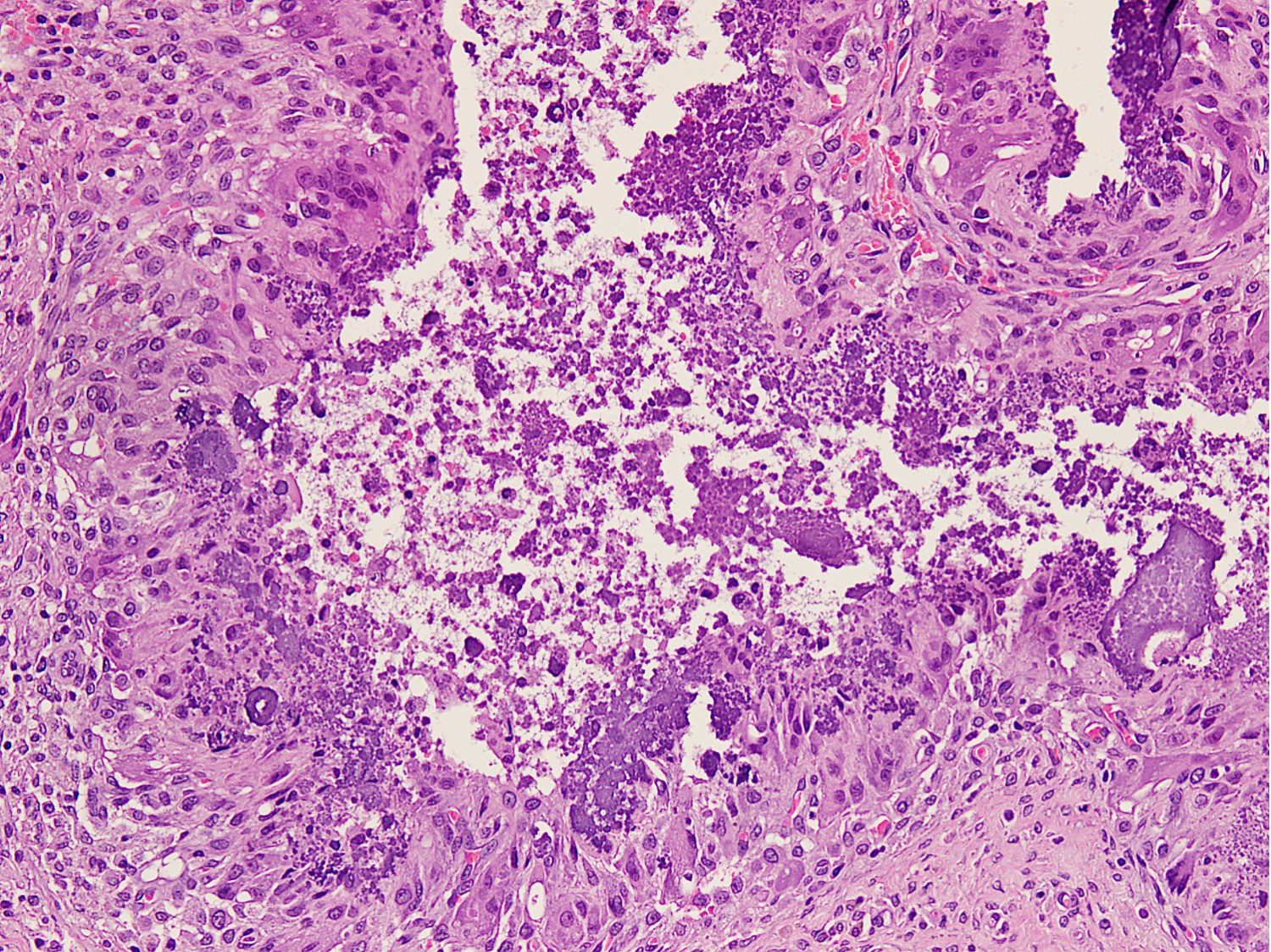
Microscopic (histologic) description
- Histology is same regardless of the type, primary or secondary (Am J Surg Pathol 1993;17:788)
- Lobular to irregular deposits of amorphous calcium crystals (hydroxyapatite crystals) within cystic spaces, surrounded by foreign body giant cell reaction
- Deposits of calcium are present within collagen fibrils and ground substance
- Calcification may be chunky basophilic or may form psammoma body-like calcospherites
- Foreign body giant cell reaction comprises of histiocytes, multinucleated foreign body giant cells, osteoclast-like giant cells and chronic inflammatory cells
- Foreign body giant cell reaction may show granulomatous appearance
- Histological features depend upon the stage of evolution of the lesion (Int J Surg Pathol 2012;20:462)
- In early stage, cystic spaces contain eosinophilic debris undergoing calcification with histiocytic reaction
- In advanced stage, heavily calcified material is surrounded by densely hyalinized connective tissue
- 3 stage classification scheme:
- Early (proliferative) phase: fibrohistiocytic nodules composed of fibroblast-like cells, foamy histiocytes, mononuclear macrophages and hemosiderin laden macrophages
- Active (cellular) phase: amorphous or granular calcified material surrounded by exuberant proliferation of macrophages, fibroblasts, osteoclast-like giant cells and chronic inflammatory cells
- Inactive phase: heavily calcified material, bordered by dense fibrosis or a cystic space, enclosed by calcium deposits
Microscopic (histologic) images
Cytology description
- Diagnosis can be made on cytology with clinical, serological and radiological correlation
- Cytology smears show coarse to fine calcific debris (Diagn Cytopathol 1995;13:339, Turk Patoloji Derg 2015;31:145)
- Clumps of dark, basophilic, amorphous calcium deposits are present
- Few ill defined granulomas may be seen
Cytology images
Electron microscopy description
- Not required for diagnosis
- Many ultrastructural studies have implicated intramitochondrial calcification in histiocytes as the principal calcifying process in tumoral calcinosis (Int J Surg Pathol 2012;20:462, Clin Orthop Relat Res 1983;178:258)
Molecular / cytogenetics description
- Identification of biallelic germline loss of function variants in FGF23, GALNT3 or KL by molecular genetic testing, is helpful when clinical and laboratory findings are inconclusive in familial type (Nat Genet 2004;36:579, J Clin Endocrinol Metab 2005;90:2424)
- Molecular testing approaches include serial single gene testing, multiple gene panel or comprehensive genomic testing (J Endocrinol Invest 2020;43:173)
Videos
Scrotal calcinosis - pathology mini tutorial
Sample pathology report
- Elbow, excision:
- Histologic features are consistent with tumoral calcinosis (see comment)
- Comment: Histology of the lesion shows nodular to irregular aggregates of amorphous to basophilic calcium deposits surrounded by foreign body giant cell reaction, features classic of tumoral calcinosis. It is a benign condition that can be primary (idiopathic or familial) or secondary due to metabolic disorders and systemic conditions like chronic renal insufficiency, hyperparathyroidism, milk alkali syndrome, hypervitaminosis D, systemic sclerosis, scleroderma, dermatomyositis, sarcoidosis, osteoarthritis, congenital deformities and trauma. Clinical and serological correlation is recommended.
Differential diagnosis
- Soft tissue chondroma:
- Occurs in middle age group with male predominance
- Involves distal extremities including digits, hands and feet
- Hyaline cartilage is present with secondary dystrophic calcification
- Gout:
- More commonly affects men between the ages of 30 - 50
- Women usually affected after menopause
- Polarizable needle shaped urate crystals show negative birefringence (Arthritis Rheumatol 2020;72:1408)
- Less calcification
- May have hyperuricemia
- Bone erosion may be seen
- Pseudogout (calcium pyrophosphate dihydrate crystal deposition disease):
- Affects older adults and the elderly
- Involves weight bearing joints, such as knees, hips, shoulders, wrists and ankles
- Polarizable rhomboid shaped calcium pyrophosphate crystals show positive birefringence (Mod Pathol 2001;14:806)
- Response is more fibroblastic than histiocytic
- Calcific tendinitis:
- Age range is between 30 - 60 years
- Women are more affected than men
- Shoulder > hip > elbow > wrist > knee
- Deposition of calcium hydroxyapatite crystals in tendons
- No sedimentation of calcium
- Calcifying synovial sarcoma:
- Arises in deep soft tissue of extremities of young adults
- Knee is most commonly affected
- Distinct tumor fascicles of plump spindle cells
- Less calcification
- Cytokeratin, EMA: focal / patchy positive
- TLE1: diffuse nuclear positive
Additional references
Practice question #1
A 20 year old woman presented with painless bilateral hip swellings. Gross specimen was comprised of skin covered fibroadipose and fibromuscular tissue with an unencapsulated multicystic lesion in subcutaneum. Microscopy revealed large basophilic calcium deposits surrounded by foreign body giant cell reaction with intervening areas of fibrosis. No atypical cells were seen. What is the most likely diagnosis?
- Chondroma
- Gout
- Osteolipoma
- Pseudogout
- Tumoral calcinosis
Practice answer #1
Practice question #2
Which of the following is a cause of secondary tumoral calcinosis?
- Chronic renal failure
- FGF23 gene mutation
- GALNT3 gene mutation
- Idiopathic
- SAMD9 gene mutation
Practice answer #2