Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Cytology description | Cytology images | Positive stains | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Zhong E, Wen HY. Gynecomastia. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastgynecomastia.html. Accessed October 3rd, 2025.
Definition / general
- Benign enlargement of the male breast, typically presenting as a palpable subareolar mass
- Histologically identical gynecomastoid hyperplasia can be seen in female breast
Essential features
- Benign ductal and stromal proliferation with characteristic stromal cuffing, typically with 3 layered ductal lining and pseudoangiomatous stromal hyperplasia
Epidemiology
- Trimodal age distribution:
- Infancy and neonatal period
- Puberty (peak incidence age 13 - 14)
- Older males age 50 - 80 (likely due to increased adiposity, decreased testosterone, medications)
- Estimated lifetime prevalence of 32 - 65% of men, depending on method of assessment (Indian J Endocrinol Metab 2014;18:150)
Sites
- Most cases retroareolar and bilateral
- Rare cases of unilateral gynecomastia related to trauma or of unknown pathophysiology (Andrologia 2006;38:31, J Plast Reconstr Aesthet Surg 2011;64:1684, GMS Interdiscip Plast Reconstr Surg DGPW 2012;1:Doc01)
- Can be localized or generalized
Etiology
- Imbalance of estrogens and androgens by various mechanisms
- Idiopathic in > 40% of cases (Biomed Res Int 2018;2018:8364824)
- Physiologic: in newborns and infants, due to in utero estrogen exposure and tends to resolve spontaneously; hormonal changes in puberty (Pediatr Endocrinol Rev 2017;14:371)
- Drugs: finasteride, anabolic steroids, digitalis, spironolactone, metronidazole (Eur J Clin Pharmacol 2015;71:569, Biomed Res Int 2018;2018:8364824)
- Systemic disorders: obesity, hyperthyroidism, hypogonadism, cirrhosis, chronic renal failure, chronic pulmonary disease
- Syndromes: androgen insensitivity, Klinefelter, Carney complex, Peutz-Jeghers, spinobulbar muscular atrophy (Andrology 2016;4:1178, Case Rep Pediatr 2015;2015:439239, Am J Transl Res 2017;9:2639, J Neurol 2018;265:1026)
- Paraneoplastic hormone production by various testicular germ cells, pulmonary and adrenocortical neoplasms
- Mechanical: repeated impact against the body as seen in male rifle shooters with unilateral gynecomastia (GMS Interdiscip Plast Reconstr Surg DGPW 2012;1:Doc01)
Clinical features
- Most common male breast lesion
- Mastalgia in 88% (J Family Med Prim Care 2021;10:648)
Diagnosis
- Histologic changes are necessary for the diagnosis; important to exclude malignancy
Laboratory
- Usually not needed, except to identify underlying causes
- Estrogen to testosterone ratio (E2/TTE), follicle stimulating hormone (FSH), luteinizing hormone (LH), prolactin, thyroid stimulating hormone (TSH), hCG, AFP, dehydroepiandrosterone (DHEA), cortisol, karyotyping
Radiology description
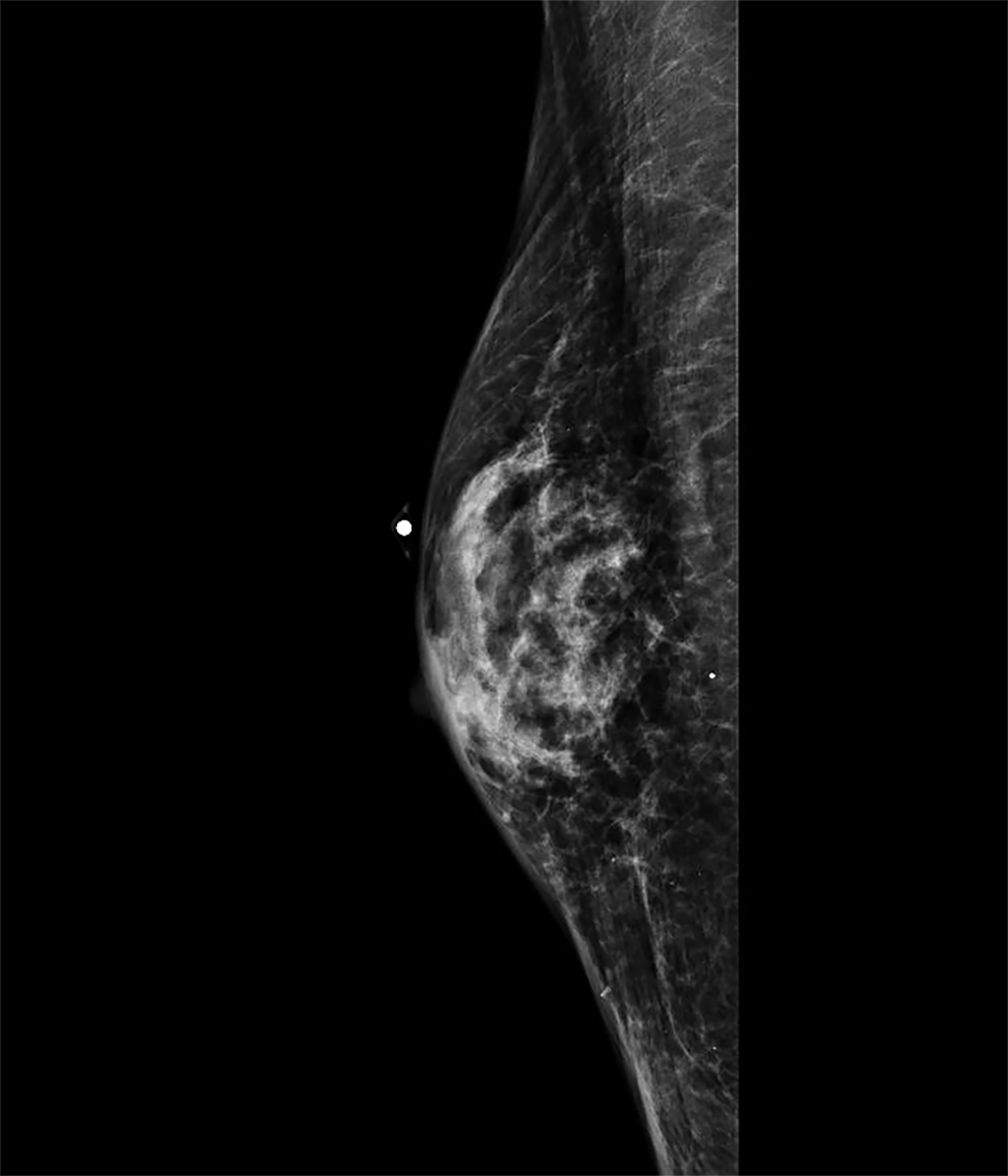
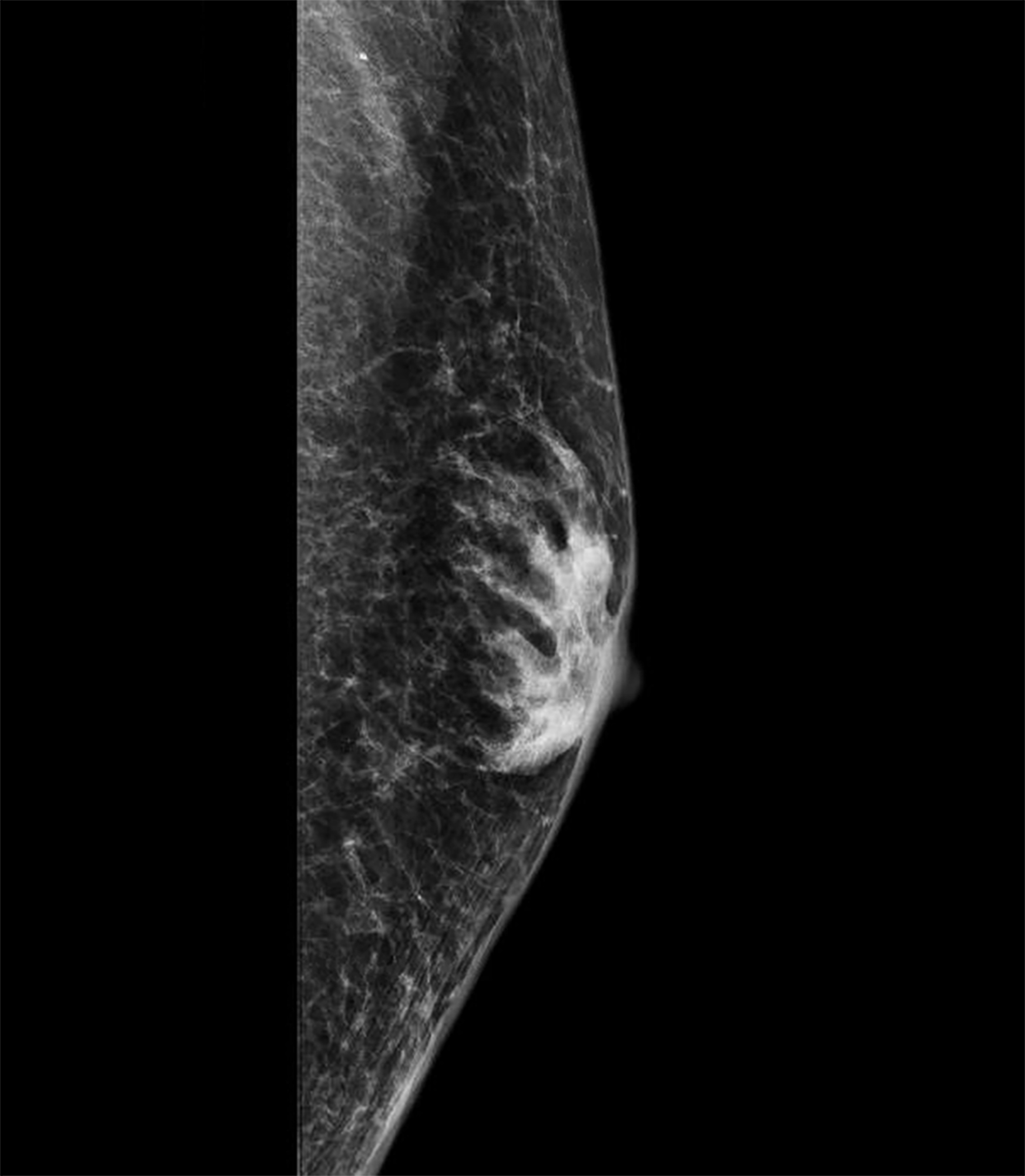
- 3 patterns of mammographic findings (Radiographics 1999;19:559, Andrology 2021 May 25 [Epub ahead of print])
- Nodular: 72%, corresponds to florid histologic phase; fan shape radiating from nipple into surrounding fat
- Dendritic: 18%, corresponds to fibrous histologic phase; flame shaped opacity with radiating projections penetrate surrounding fat / upper outer quadrant
- Diffuse: ~10%, typically in transgender females undergoing gender affirming hormonal therapy; resembles dense female breast but heterogeneous and without Cooper ligaments
- Imaging useful to exclude pseudogynecomastia and carcinoma
Prognostic factors
- May recur if underlying cause is not addressed
- No strong evidence of increased risk of breast carcinoma
- Present in 3 - 46% of male breast carcinoma (Cancer 2004;101:51, Cancer 1996;77:490)
Case reports
- 4 year old boy with adrenocortical carcinoma, with gynecomastia as presenting symptom (Clin Pediatr Endocrinol 2018;27:9)
- 13 year old boy with gynecomastia secondary to imatinib related hypogonadism (Indian J Hematol Blood Transfus 2017;33:448)
- 38 year old male to female transgender individual with concern for breast malignancy following hormonal replacement therapy (Case Rep Oncol Med 2017;2017:5172072)
Treatment
- Some regress spontaneously within 2 years and do not require treatment
- Sudden or symptomatic gynecomastia may be treated medically
- Aromatase inhibitor, anti-estrogen, androgen therapy (tamoxifen, danazol) (Breast 2006;15:276, J Pediatr Endocrinol Metab 2013;26:803)
- Identify and treat any underlying causes
- Excision in adult patients to rule out malignancy and for cosmesis; however, recurrence is common if the underlying cause is not identified and treated
Clinical images
Gross description
- Soft, rubbery to firm gray-white subareolar mass
- Can be ill defined subareolar induration
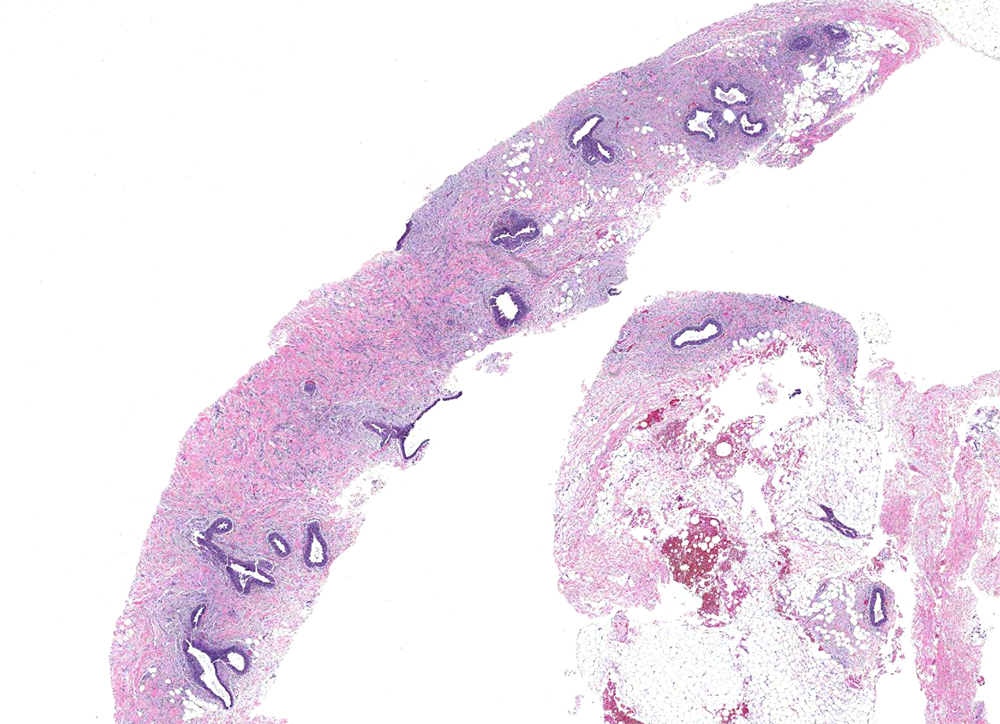
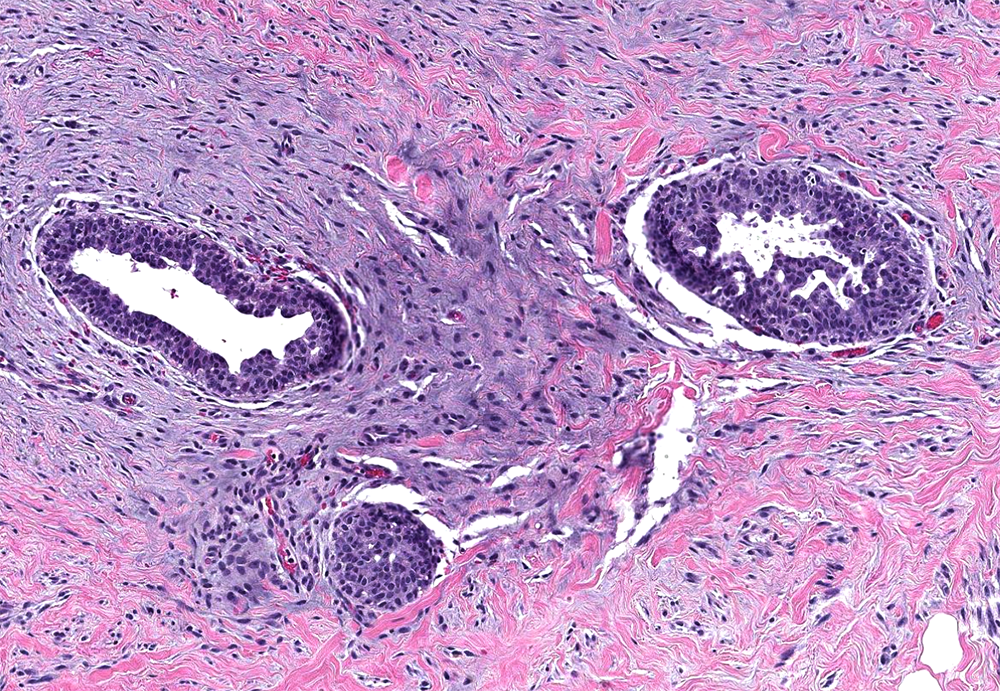
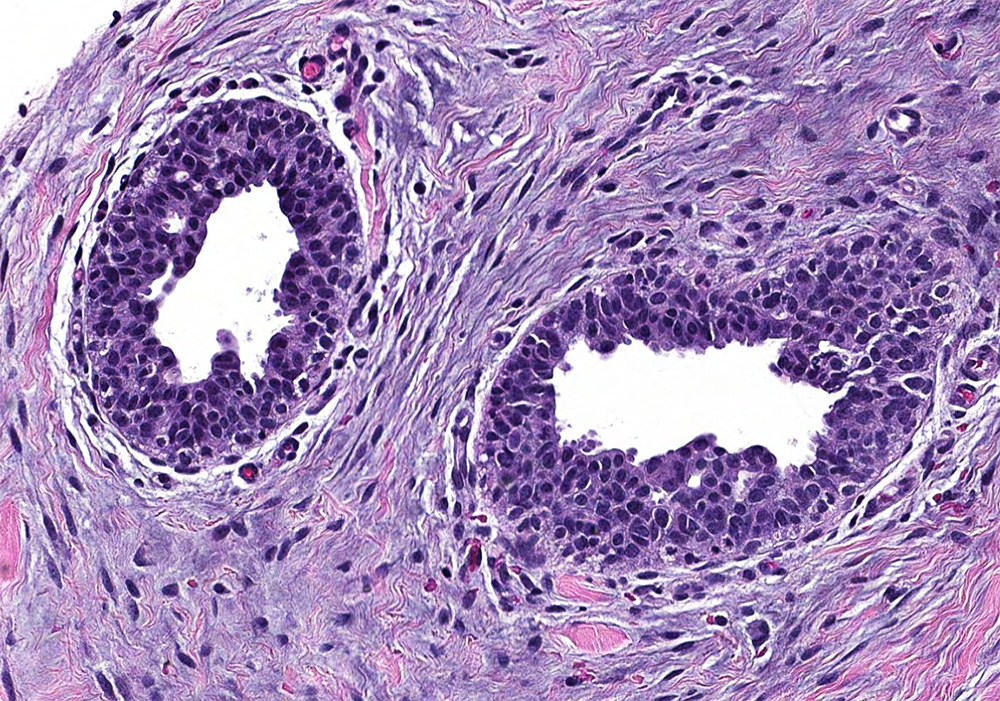
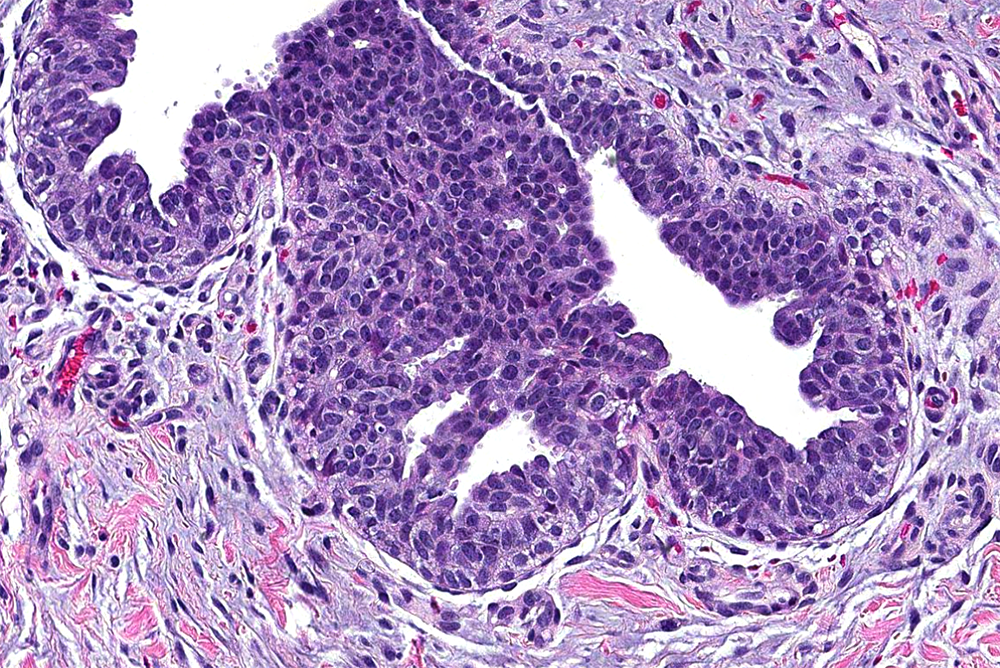
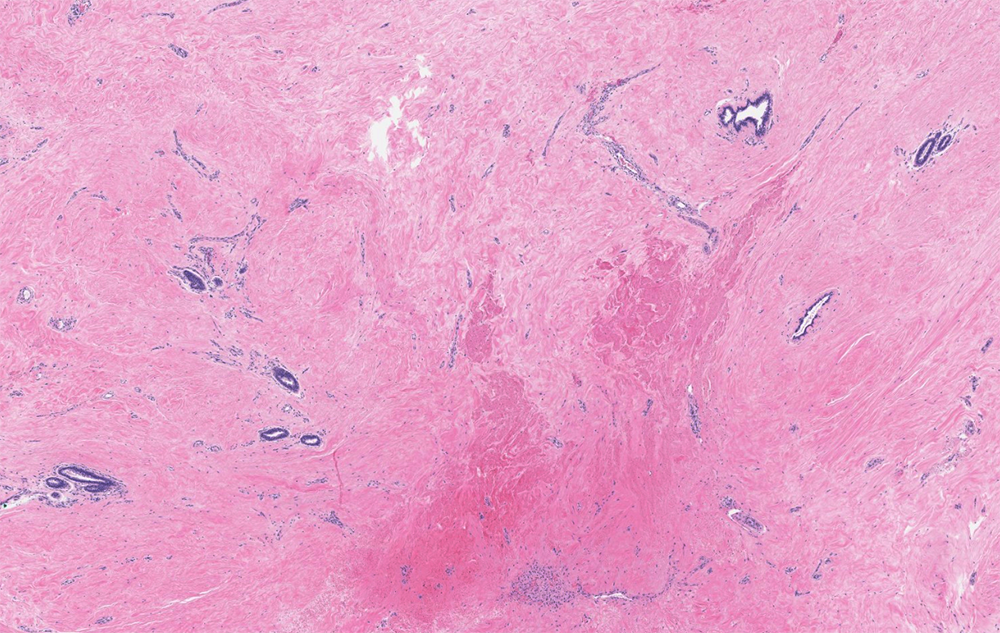
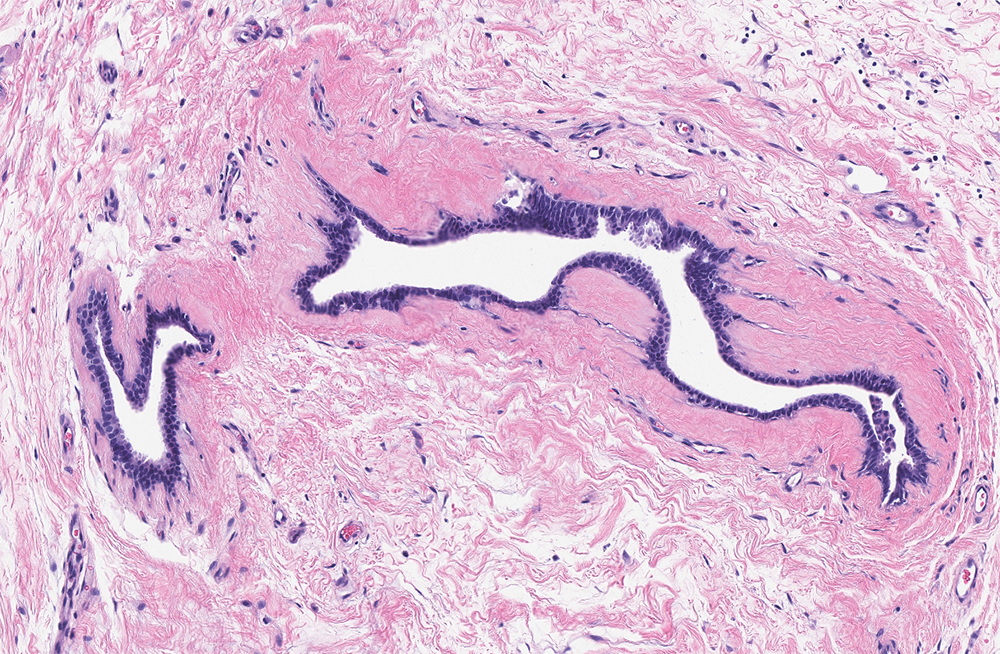
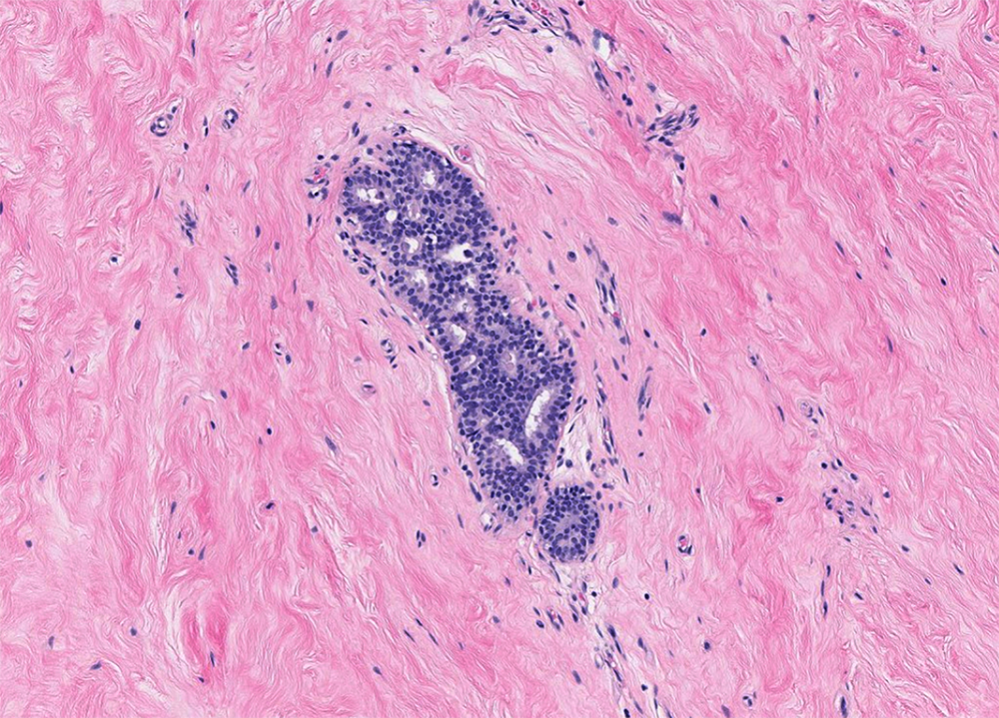
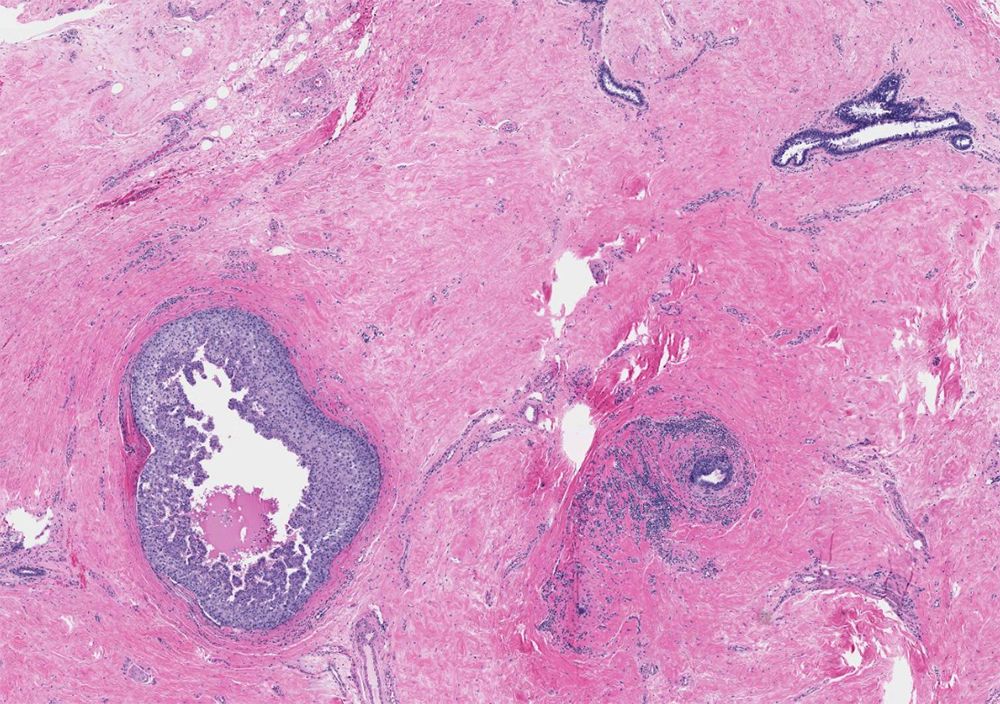
Microscopic (histologic) description
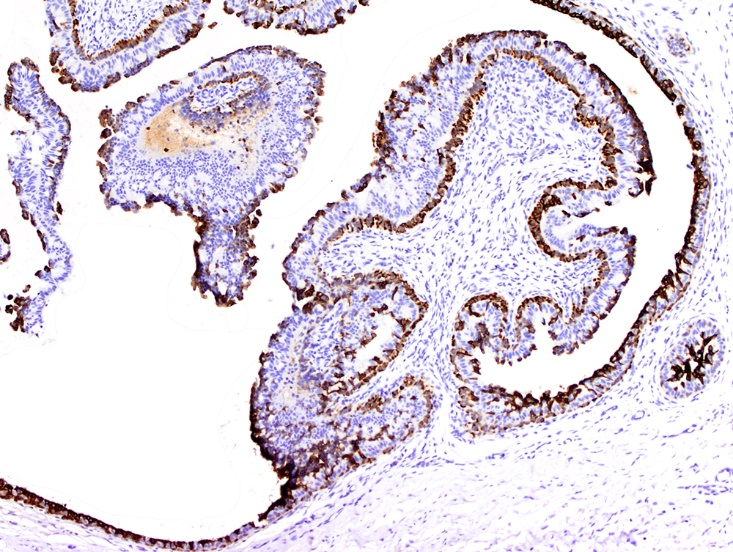
- Increased number of ducts with characteristic 3 layer epithelium (Am J Surg Pathol 2012;36:762):
- Luminal epithelium expressing CK5/6, CK14
- Intermediate cuboidal to columnar epithelium expressing ER, PR, AR
- Outer myoepithelium expressing CK5/6 and CK14
- 3 patterns of proliferative changes, without correlation to age or duration of lesion (Am J Clin Pathol 1972;57:431, J Plast Surg Hand Surg 2018;52:166)
- Florid: irregular branching ducts, mild to moderate epithelial hyperplasia, cellular / myxoid / edematous stroma cuffing around ducts; can have papillary or cribriform architecture, myoepithelial hyperplasia
- Intermediate: mixture of florid and fibrous patterns
- Fibrous: quiescent epithelium, hyalinized hypocellular stroma
- Other findings can include pseudoangiomatous stromal hyperplasia (PASH), apocrine or squamous metaplasia
- Atypical ductal hyperplasia (ADH) in 0.4 - 5.4% (Ann Plast Surg 2015;74:163, Histopathology 2015;66:398)
- Not clearly precancerous (Breast Cancer Res Treat 2019;175:1)
Microscopic (histologic) images
Virtual slides
Cytology description
- Biphasic epithelial and stromal fragments in a background of scattered single bipolar nuclei, similar to fibroadenoma
- Spindle cells, apocrine cells, foamy macrophages can be present
Positive stains
Sample pathology report
- Breast, retroareolar; core biopsy:
- Gynecomastia, (florid, intermediate or fibrotic) stage.
Differential diagnosis
- Male breast cancer:
- Histology identical to carcinoma of the female breast
- Atypical ductal hyperplasia:
- Monomorphic intraductal cells in rigid cribriform, micropapillary or solid formations
- Myofibroblastoma:
- Mass forming spindle cell proliferation that may entrap normal glandular elements
- Variable morphology and cellularity
- Mammary hamartoma:
- Circumscribed mass
- Additional mesenchymal elements (smooth muscle, adipose tissue, cartilage, etc.) may be present
- Fibroadenoma:
- Circumscribed mass
- Uniform stroma without significant periductal cuffing
- Intracanalicular or pericanalicular pattern of glandular elements
Additional references
Practice question #1
Which of the following is the most common etiology in the development of gynecomastia?
- Cirrhosis
- Estrogen exposure in utero
- Hyperthyroidism
- Idiopathic
- Klinefelter syndrome
Practice answer #1
Practice question #2
Practice answer #2