Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Etiology | Clinical features | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Cytology images | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Tozbikian G. Lymphoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantlymphoma.html. Accessed April 19th, 2024.
Definition / general
- Lymphomas of the breast may be primary or secondary
- Primary breast lymphoma is generally defined as lymphoma limited to the breast, with or without axillary lymph node involvement, in a patient without evidence of distant disease at presentation and without prior history of lymphoma (Histopathology 1985;9:297, Cancer 1972;29:1705)
- Some accept lymphoma as primary if the initial presentation and the dominant mass or symptoms occur in the breast, even if other involved sites are identified (Am J Surg Pathol 2008;32:1299, Ann Surg 1987;205:144, Cancer 1990;66:2602)
- Most common types include diffuse large B cell lymphoma, extranodal marginal B cell lymphoma arising from mucosal associated lymphoid tissue (MALT lymphoma), follicular lymphoma and Burkitt lymphoma
- Implant associated anaplastic large cell lymphoma is discussed in a separate section
Essential features
- Lymphoma seen in close proximity to breast parenchyma, not limited to lymph nodes
- Primary breast lymphoma is uncommon and must be distinguished from secondary breast involvement from another primary site in the setting of widespread disease / relapse (more common)
- Must distinguish from mammary carcinoma, as therapeutic / surgical management is different; use of immunohistochemical panel (cytokeratins and lymphoid lineage markers) will confirm the diagnosis
Terminology
- Diffuse large B cell lymphoma (DLBCL) / DLBCL not otherwise specified (NOS)
- Extranodal marginal B cell lymphoma arising from mucosal associated lymphoid tissue (MALT lymphoma) / marginal zone lymphoma MALT type / MALT lymphoma
- Follicular lymphoma / follicular center cell lymphoma
- Burkitt lymphoma
ICD coding
- ICD-O:
- ICD-10:
Epidemiology
- Uncommon, accounts for 0.1 - 0.15% of primary breast malignancies (Cancer 1972;29:1705, Cancer 1990;66:2602, Cancer 2002;94:6)
- Most patients are older or postmenopausal; however, younger patients have been reported (especially with Burkitt lymphoma)
- Usually presents with painless lump; regional lymph nodes are involved in 50% of cases (Am J Surg Pathol 1993;17:574)
Etiology
- Diffuse large B cell lymphoma (DLBCL):
- Activated B cell type (IRF4+, FLIP+, BCL2+), germinal center type (BCL6+, CD10+, CD38+) or neither
- Commonly arises de novo or can occur through progression / transformation of a less aggressive non-Hodgkin lymphoma
- Extranodal marginal B cell lymphoma arising from mucosal associated lymphoid tissue (MALT lymphoma):
- Less association with underlying autoimmune disease compared to MALT lymphomas of other sites
- Follicular lymphoma:
- Originates from germinal / follicular center B cells
- Burkitt lymphoma:
- 3 variants: endemic (> 95% Epstein-Barr virus [EBV]+), immunodeficiency associated (often HIV+) and sporadic (less frequently EBV+)
- c-Myc translocation
Clinical features
- Middle age to elderly, median in sixth to seventh decade (Am J Surg Pathol 2008;32:1299, Leuk Lymphoma 2005;46:1321)
- Reports of younger patients in pregnant or lactating women (Burkitt lymphoma)
- Most present with painless palpable mass, with or without ipsilateral lymphadenopathy (11 - 50%) (Am J Surg Pathol 1993;17:574)
- Bilateral in 10%
- Treatment and prognosis are related to specific type of lymphoma:
- Diffuse large B cell lymphoma (DLBCL):
- Most common primary breast lymphoma (50 - 65%) (Cancer 2007;110:25, Am J Hematol 2009;84:133)
- Wide age range, median in sixth decade
- Median size 4 - 5 cm, may present as rapidly enlarging mass, few present with diffuse breast enlargement
- Aggressive clinical behavior, most common sites of relapse include ipsilateral or contralateral breast and central nervous system
- Must be distinguished from poorly differentiated carcinomas
- Extranodal marginal B cell lymphoma arising from mucosal associated lymphoid tissue (MALT lymphoma):
- Sixth to seventh decade
- Typically unilateral
- Indolent, > 90% 5 year survival (Ann Oncol 2009;20:1993)
- Large cell transformation reported
- Follicular lymphoma:
- Middle aged and older women
- Usually unilateral
- Similar prognosis compared to nodal follicular lymphoma, some have reported worse prognosis (Ann Oncol 2009;20:1993)
- Burkitt lymphoma:
- Uncommon, younger to middle aged females, some pregnant or postpartum at presentation
- Endemic variant is the most common presentation in the breast
- May present with massive bilateral breast enlargement
- Aggressive B cell lymphoma has more favorable prognosis with aggressive therapy
- Diffuse large B cell lymphoma (DLBCL):
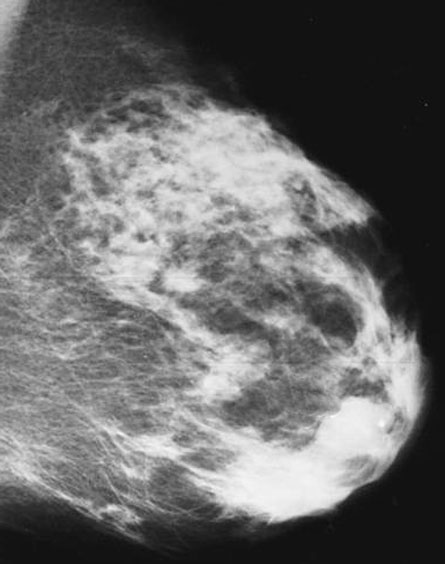
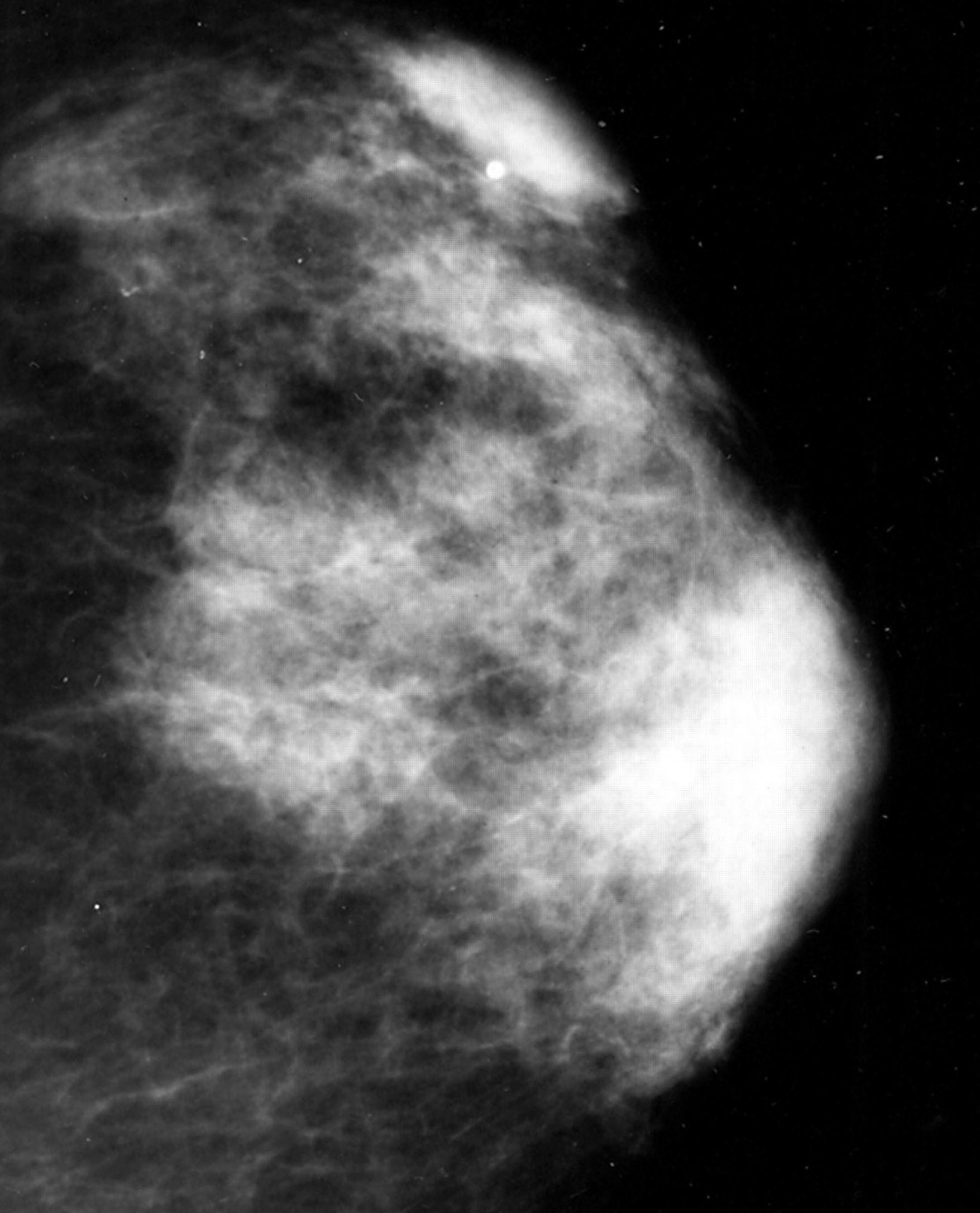
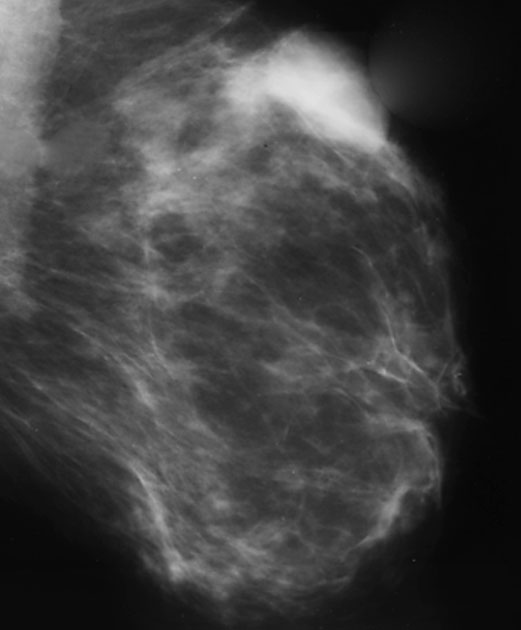
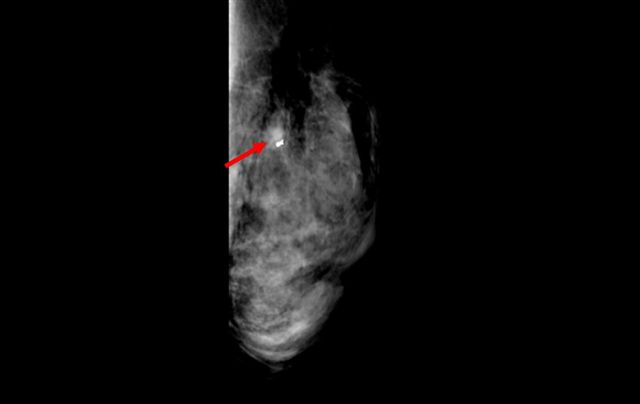
Radiology description
- On mammography, primary breast lymphomas have been reported to present as unilateral diffuse involvement (25%), bilateral diffuse involvement (8%), solitary masses (58%) or as multiple masses (8%) (Breast J 2002;8:294)
- Masses may have either irregular, partially defined or well defined borders (Clin Imaging 2007;31:234)
- Useful MRI features may include strong enhancement with penetrating vessels on early images of dynamic MR imaging, strong high signal intensity on diffusion weighted imaging, a cerebroid appearance and septal enhancement on delayed contrast enhanced images (Jpn J Radiol 2013;31:668)
- Often mimic primary breast cancer
Radiology images
Contributed by Mark R. Wick, M.D. and Julia Braza, M.D.
Images hosted on other servers:
Prognostic factors
- Prognosis is dependent on stage and type of lymphoma
Case reports
- 23 year old postpartum woman with bilateral breast swelling and Burkitt lymphoma (J Res Med Sci 2012;17:1188)
- 38 year old HIV+ woman and 55 year old woman diagnosed with primary breast non-Hodgkin lymphoma (Diagn Cytopathol 2016;44:235)
- 46 year old man with follicular lymphoma of the breast (Cancer Res Treat 2014;46:104)
- 59 year old woman with extranodal marginal zone lymphoma (MALT) of the breast (Case Rep Hematol 2016;2016:1831792)
- 59 year old woman with 2 breast nodules diagnosed as diffuse large B cell lymphoma (DLBCL) (Int J Surg Case Rep 2017;40:1)
Treatment
- Depends on diagnosis; is the same as lymphoma at any other site
Clinical images
Gross description
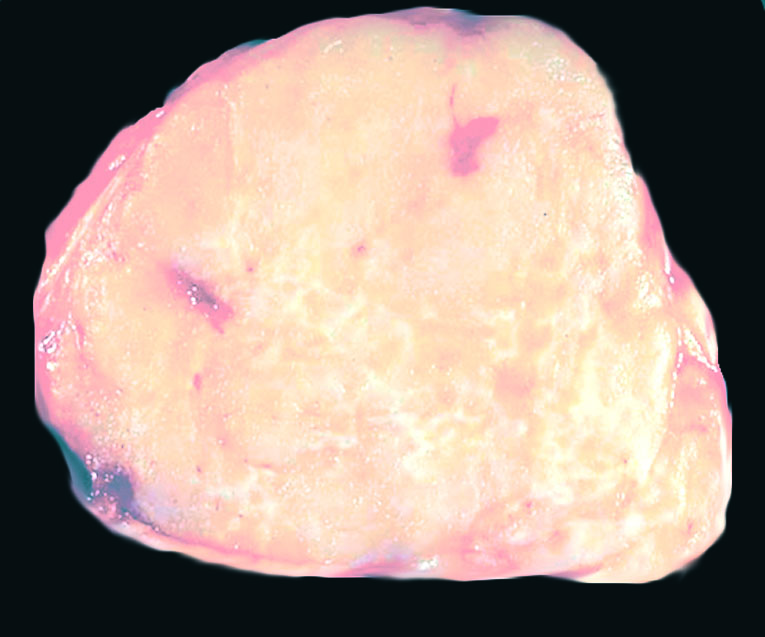
- Grossly circumscribed mass, tan-white, fleshy cut surface
- Focal hemorrhage or necrosis may be present
Gross images
Microscopic (histologic) description
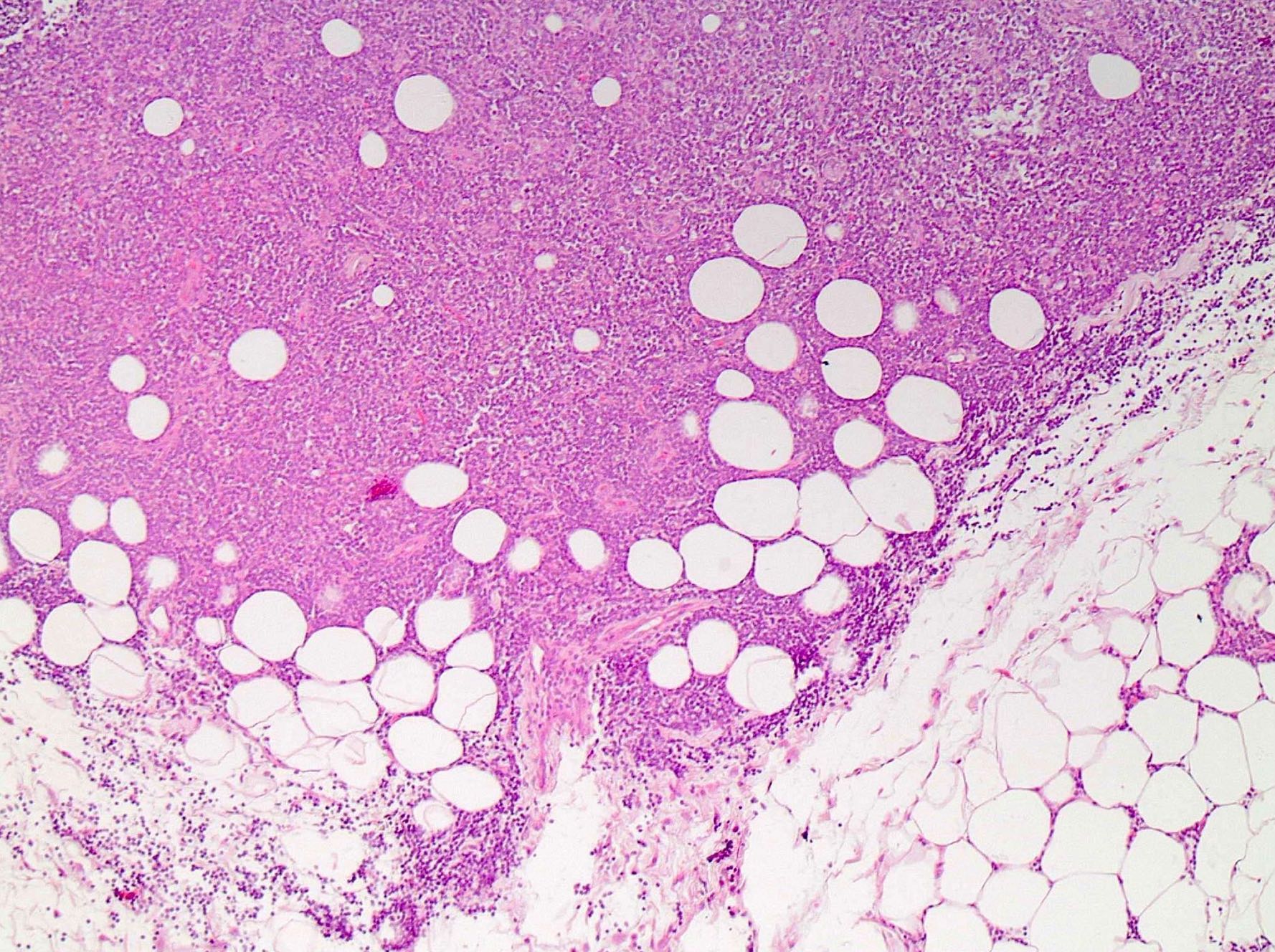
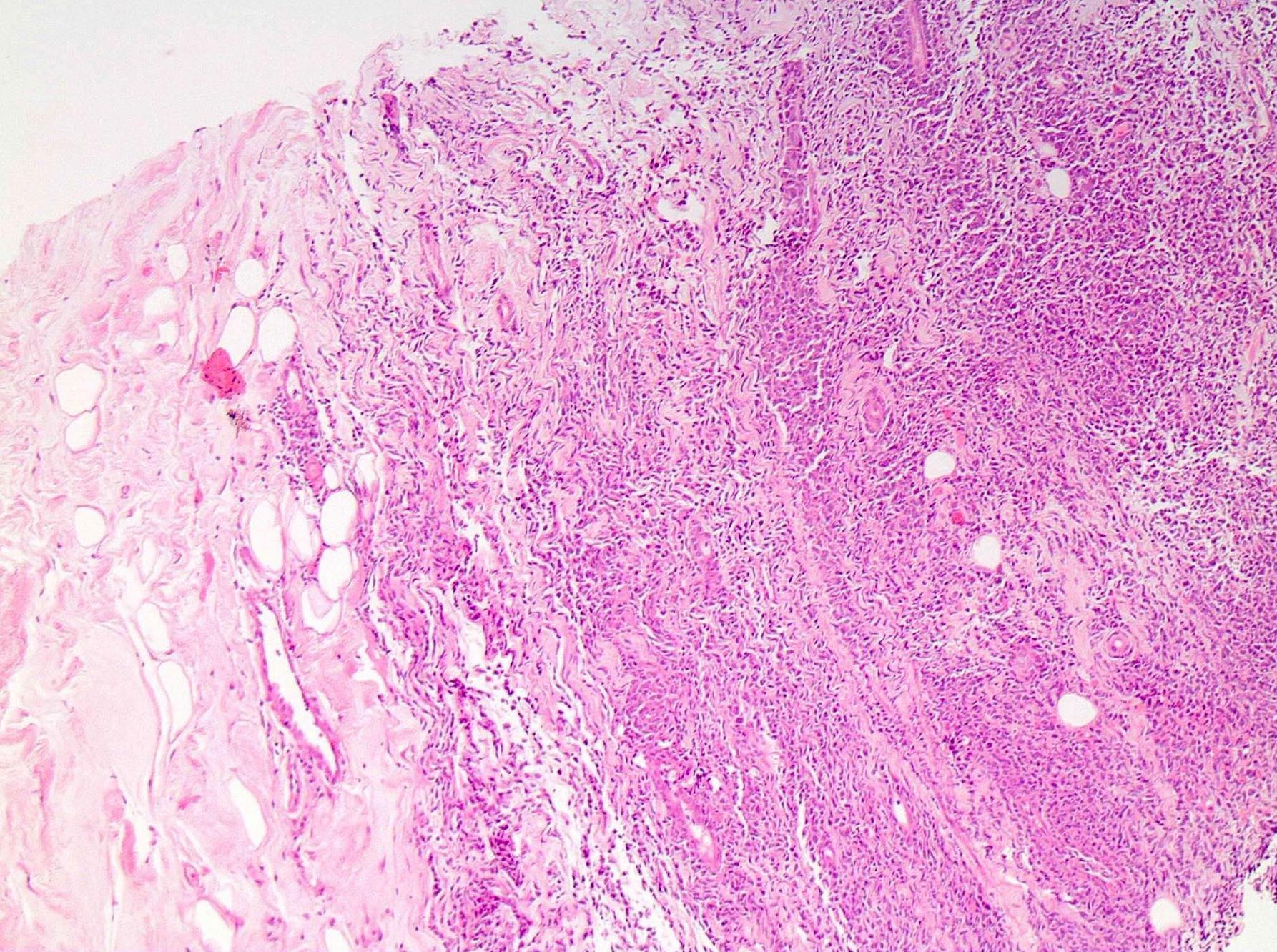
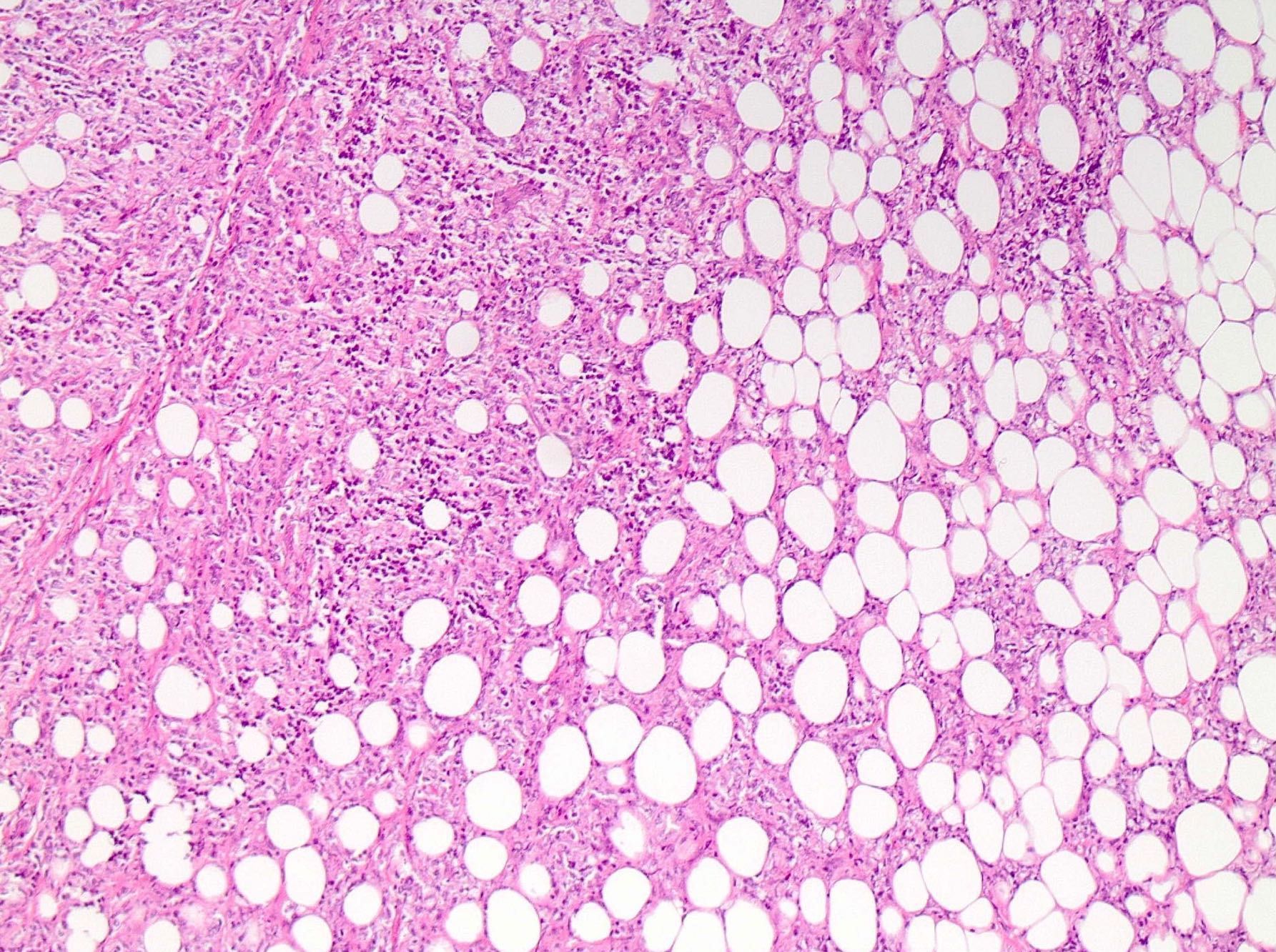
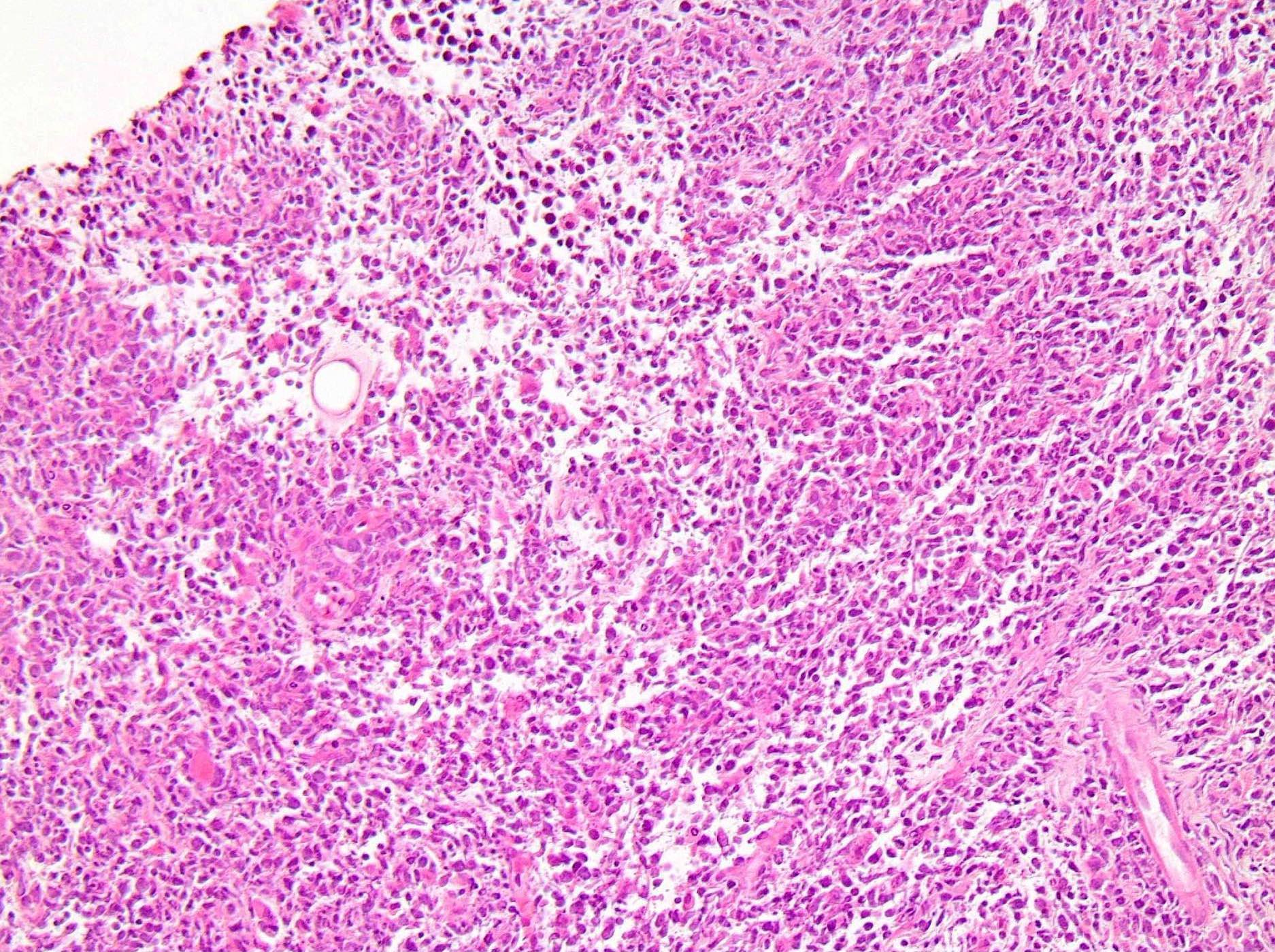
- Despite gross circumscription, microscopically these are diffusely infiltrative with invasion into surrounding breast parenchyma
- Infiltrates around and occasionally obliterates mammary gland structures
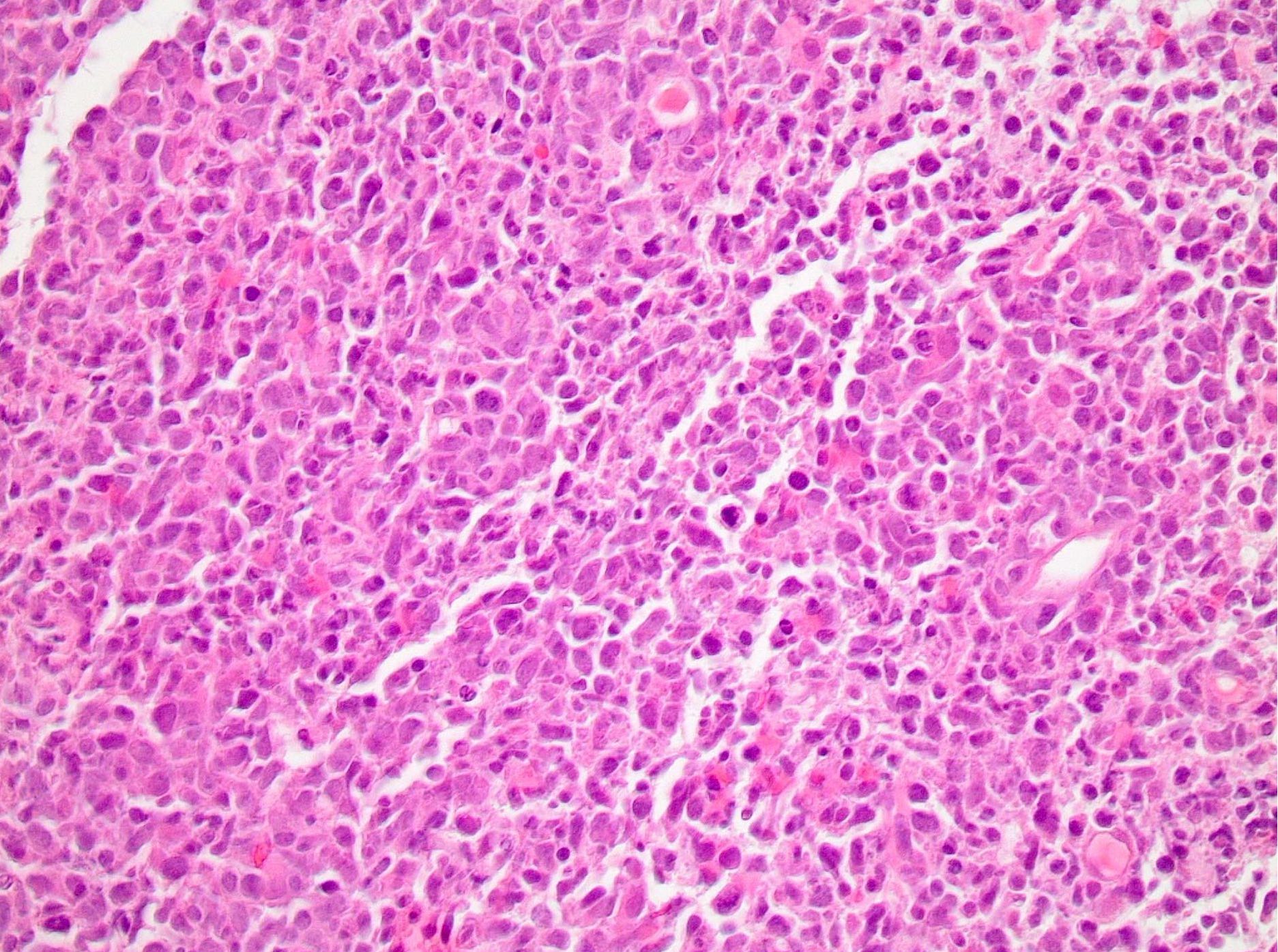
- Diffuse large B cell lymphoma (DLBCL):
- Diffuse infiltration by large lymphoid cells, centroblastic > immunoblastic, activated B cell type > germinal center type
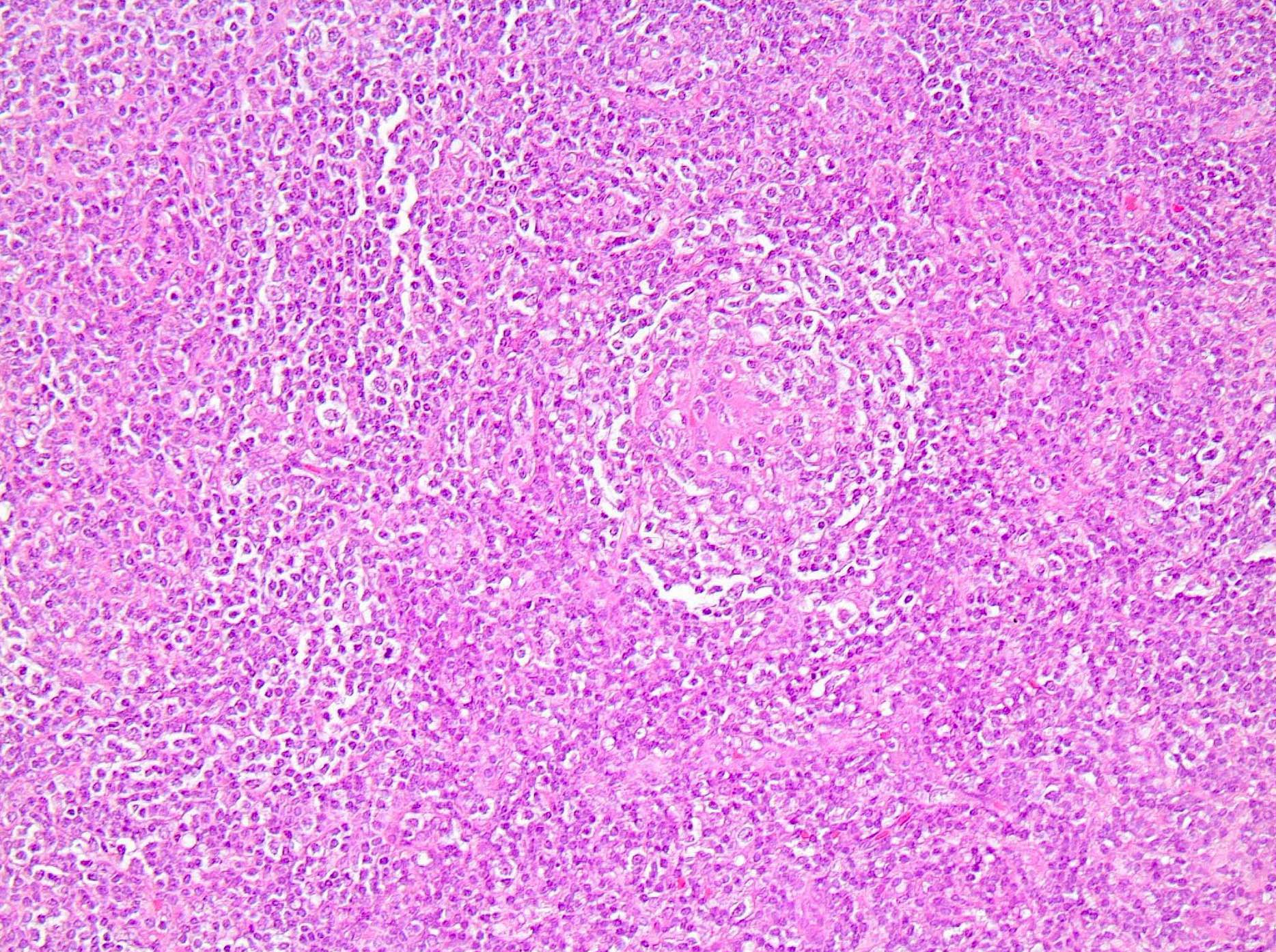
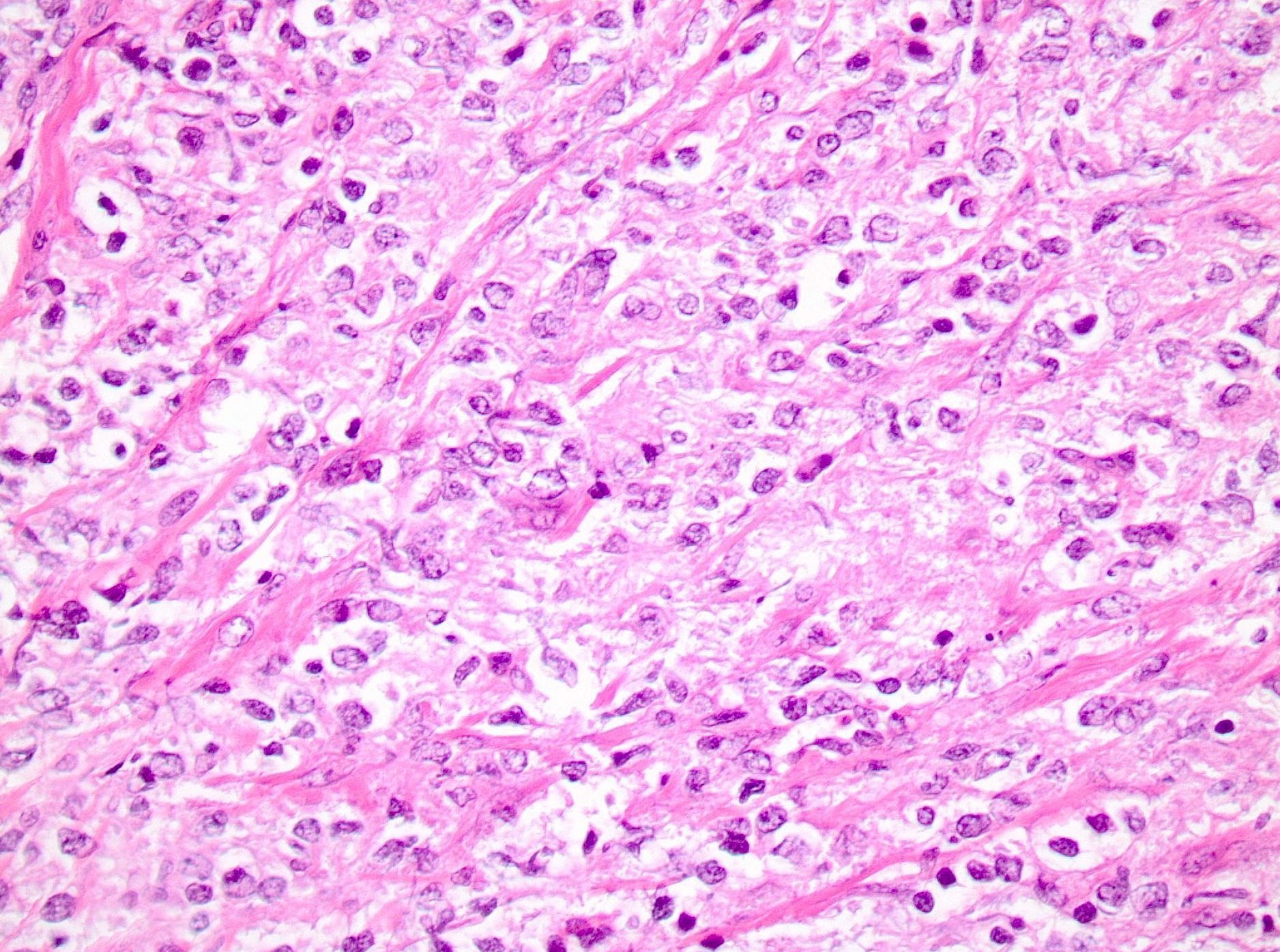
- Extranodal marginal B cell lymphoma arising from mucosal associated lymphoid tissue (MALT lymphoma):
- Median size 3 cm
- Vaguely nodular growth pattern, neoplastic cells occupy the marginal zone surrounding the B cell follicle mantle zone but can have diffuse growth pattern if follicles infiltrated / replaced
- Marginal zone B cells, variable plasma cells, reactive follicles (±), lymphoepithelial lesions not conspicuous
- Monocytoid-like cells: medium sized lymphocytes with slightly irregular nuclei, dispersed chromatin, inconspicuous nucleoli, variable amounts of pale cytoplasm
- Variable scattered large transformed immunoblasts can be present
- Reactive follicles with infiltration by neoplastic marginal zones in some cases
- Plasmacytic differentiation in up to 75% (Arch Pathol Lab Med 2007;131:1673)
- Low mitotic rate
- Lymphoepithelial lesions may be seen if glands / ducts present but are usually not prominent, less conspicuous than MALT lymphoma in other sites
- Transformation into large B cell lymphoma described (Arch Pathol Lab Med 2007;131:1673)
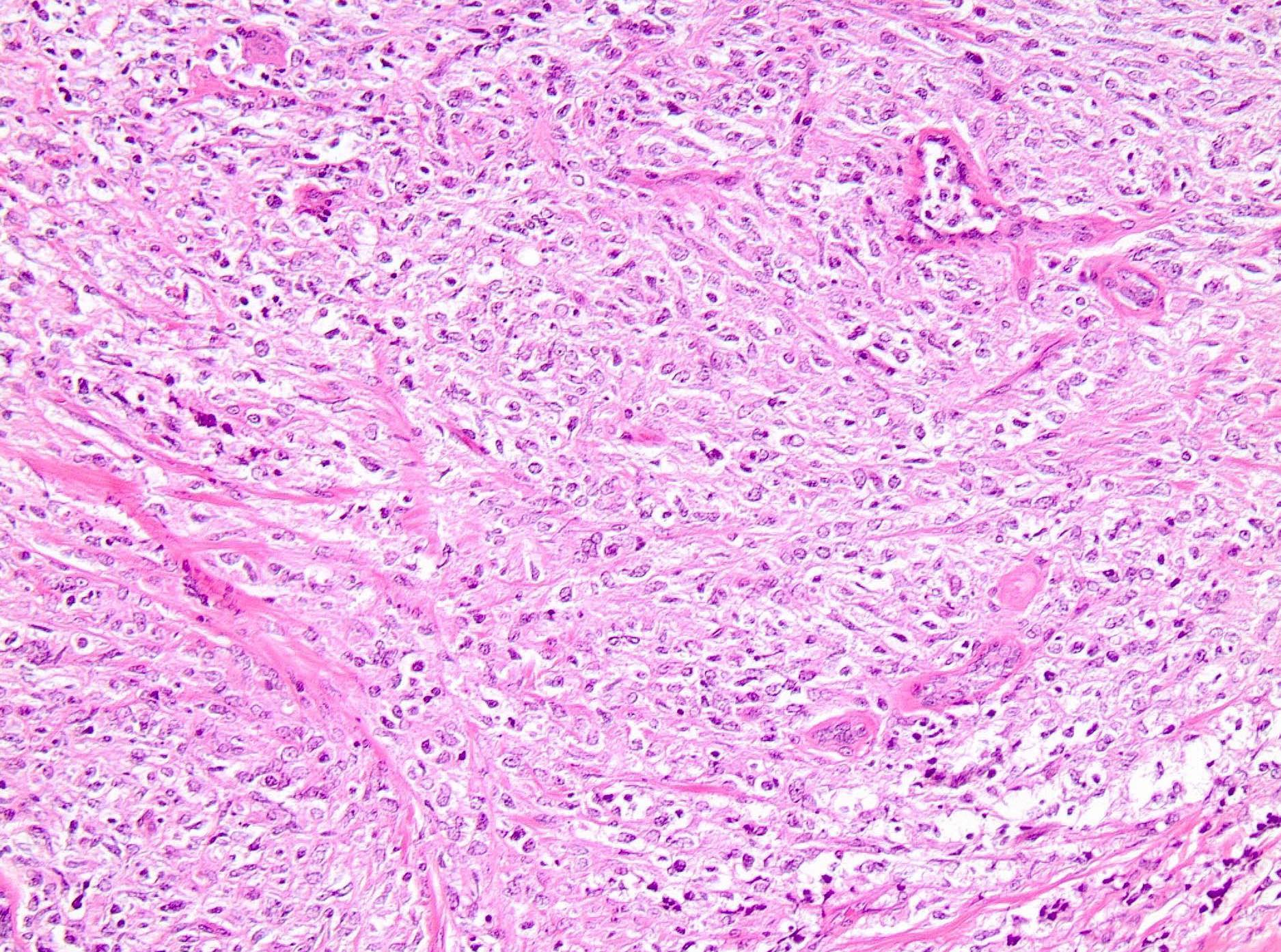
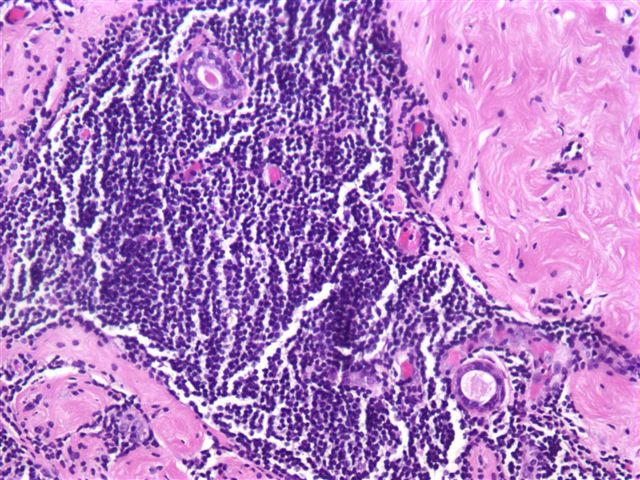
- Follicular lymphoma:
- Median size 2 - 3 cm
- Morphology similar to nodal follicular lymphomas; follicular and diffuse architectural patterns, grade 1 or 2 > grade 3
- Monotonous population of small cleaved cells (centrocytes) and variable numbers of centroblasts (large noncleaved cells)
- Associated sclerosis can cause single file infiltration pattern
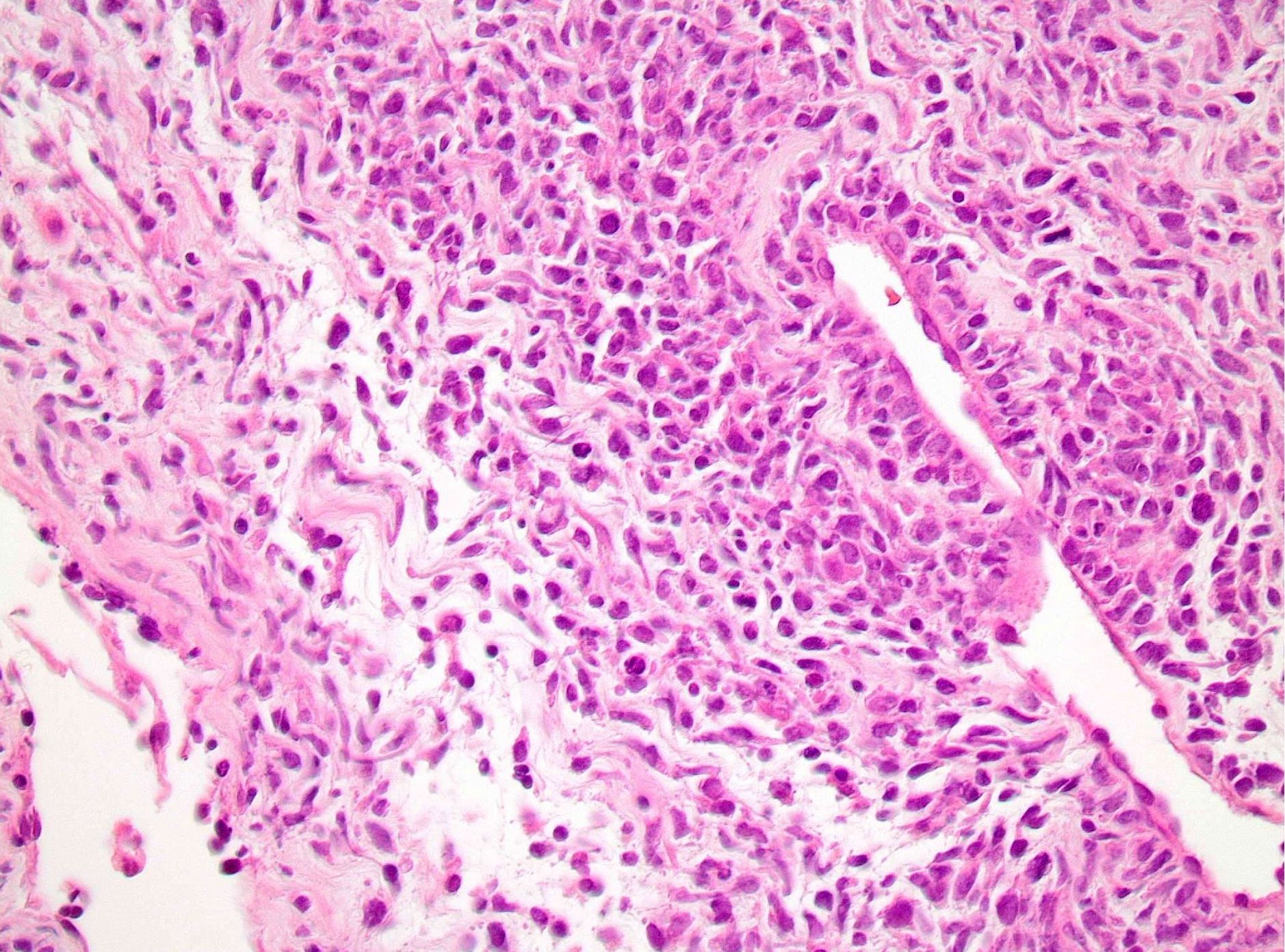
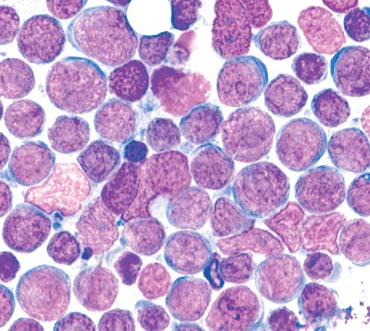
- Burkitt lymphoma:
- Sheets of uniform medium sized lymphocytes with round nuclei, multiple basophilic nucleoli, course chromatin, scant to moderate basophilic cytoplasm, minimal intervening stroma
- High mitotic rate
- Tingible body macrophages containing apoptotic debris produce a "starry sky" appearance
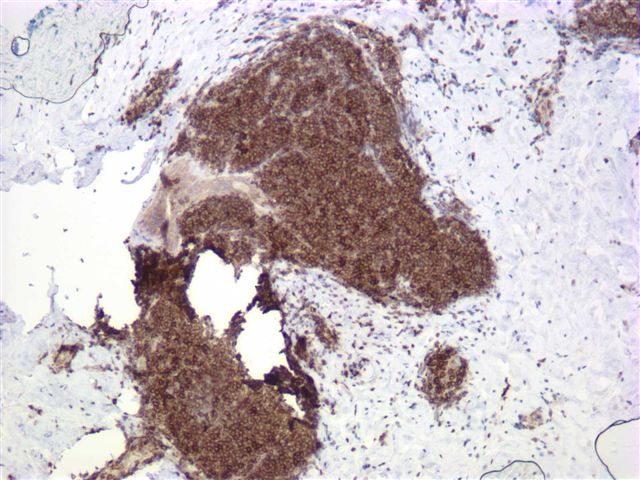
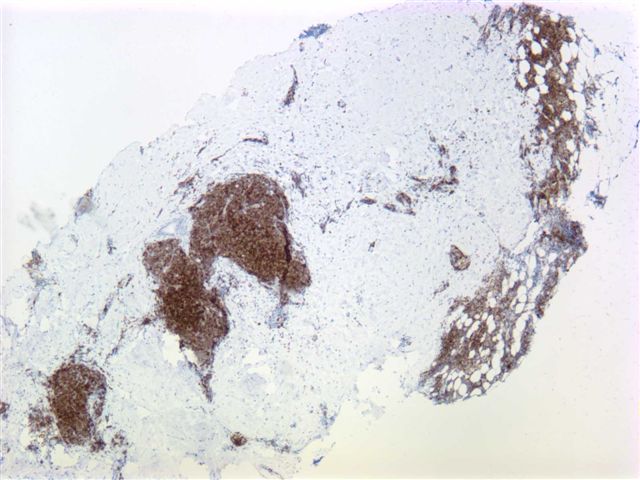
Microscopic (histologic) images
Contributed by Gary Tozbikian, M.D. and Julia Braza, M.D.
Images hosted on other servers:
Cytology description
- Primary cytomorphologic features include the presence of dissociated monomorphic cells with high nuclear cytoplasmic ratio, finely granular lymphoid chromatin and the presence of lymphoglandular bodies in the background of the cytologic smear (Diagn Cytopathol 2013;41:53)
- Differential diagnosis includes lobular carcinoma, small cell carcinoma, lesions with prominent lymphoid population including medullary carcinoma, chronic mastitis and intramammary lymph node (Diagn Cytopathol 2016;44:235)
- Lobular carcinoma: intracytoplasmic lumina, signet ring cells, intracytoplasmic mucin secretions
- Small cell carcinoma: cell clustering, cell molding, lacks lymphoglandular bodies, positive keratin and neuroendocrine immunohistochemistry staining
- High grade carcinomas with medullary features: admixture of pleomorphic epithelial cells as well as reactive lymphoid and plasma cells
- Intramammary lymph nodes and mastitis can show reactive lymphoid infiltrate and pose a diagnostic problem (Diagn Cytopathol 2013;41:53)
- Final categorization generally requires flow cytometric immunophenotyping / immunohistochemistry on cell blocks to allow morphologic and immunohistochemical evaluation (Diagn Cytopathol 2016;44:235)
Positive stains
- Diffuse large B cell lymphoma (DLBCL):
- Extranodal marginal B cell lymphoma arising from mucosal associated lymphoid tissue (MALT lymphoma):
- Follicular lymphoma:
- Burkitt lymphoma:
Negative stains
Molecular / cytogenetics description
- Diffuse large B cell lymphoma (DLBCL):
- Rare MALT1 rearrangements, trisomy 18 in some, possible NFκB activation in minority (Mod Pathol 2006;19:1402, Mod Pathol 2013;26:421)
- Extranodal marginal B cell lymphoma arising from mucosal associated lymphoid tissue (MALT lymphoma):
- Clonal rearrangements of immunoglobulin genes
- Often trisomy of 3, 12, 18
- Usually negative for characteristic MALT1 rearrangements t(11;18)(q21;q21) and t(14;18)(q32;q21) (Mod Pathol 2006;19:1402, Mod Pathol 2013;26:421, Oncol Rep 2012;28:1211)
- Follicular lymphoma:
- Presence of t(14;18)(q32;q21) translocation has not been systematically assessed in primary breast follicular lymphoma
- Burkitt lymphoma:
- t(8;14)(q24;q32) c-Myc and IgH translocation is most frequent
- t(2;8)(p12;q24) IgΚ and c-Myc
- t(8;22)(q24;q11) c-Myc and Igλ
Differential diagnosis
- Invasive ductal carcinoma:
- Poorly differentiated carcinoma mimics high grade lymphoma
- Presence of cohesive growth, identification of gland / tubule formation and presence of in situ component favor a diagnosis of ductal carcinoma
- Cytokeratin+, CD45-, CD20-, CD3-
- Invasive lobular carcinoma:
- Mimics low grade lymphoma
- Cytokeratin+, CD45-, CD20-, CD3-; usually ER+
- Chronic inflammatory infiltrates (e.g. diabetic mastopathy):
- Mimics low grade lymphoma
- Immunohistochemistry and flow cytometry will not identify a clonal B cell population
- Diabetic mastopathy shows perilobular / periductal / perivascular infiltrate with reactive lymphoid follicles, keloidal fibrosis and lobular atrophy
- Nodal lymphoma:
- Differentiation of lymphoma within a lymph node from a primary breast lymphoma may be difficult in small biopsy specimens if breast parenchyma is not identifiable
Additional references
Board review style question #1
A 22 year old woman presents with bilateral breast swelling. Breast biopsy shows diffuse sheets of uniform medium sized cells with round nuclei, multiple nucleoli, coarse chromatin, a thin rim of basophilic cytoplasm and interspersed tingible body macrophages. The tumor cells are positive for CD45, CD20, CD10 and BCL6. The Ki67 proliferation index is nearly 100%. The tumor cells are negative for CD5, CD23 and BCL2.
What molecular / cytogenetic abnormality may be associated with this lymphoma?

What molecular / cytogenetic abnormality may be associated with this lymphoma?

- Deletion of 13q14
- t(8;14)(q24;q32)
- t(11;14)(q13;q32)
- t(14;18)(q32;q21)
- Trisomy of 3, 12, 18
Board review style answer #1
Board review style question #2
What is the most common type of primary breast lymphoma?
- Burkitt lymphoma
- Diffuse large B cell lymphoma
- Follicular lymphoma
- Hodgkin lymphoma
- MALT lymphoma
Board review style answer #2