Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Molecular / cytogenetics description | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Diez Freire CC, Masood S. Male invasive. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/breastmalignantmalecarcinoma.html. Accessed April 20th, 2024.
Definition / general
- Male breast cancer is uncommon, accounting for < 1% of all male cancers and 0.1% of male cancer deaths
- Tends to occur at an older age group (60 - 70s) when compared to women (50 - 60s) and has a larger tumor size (J Clin Oncol 2010;28:232)
- Surveillance, Epidemiology and End Results (SEER) program shows a rise in the incidence across the U.S. (Cancer 2004;101:51)
Essential features
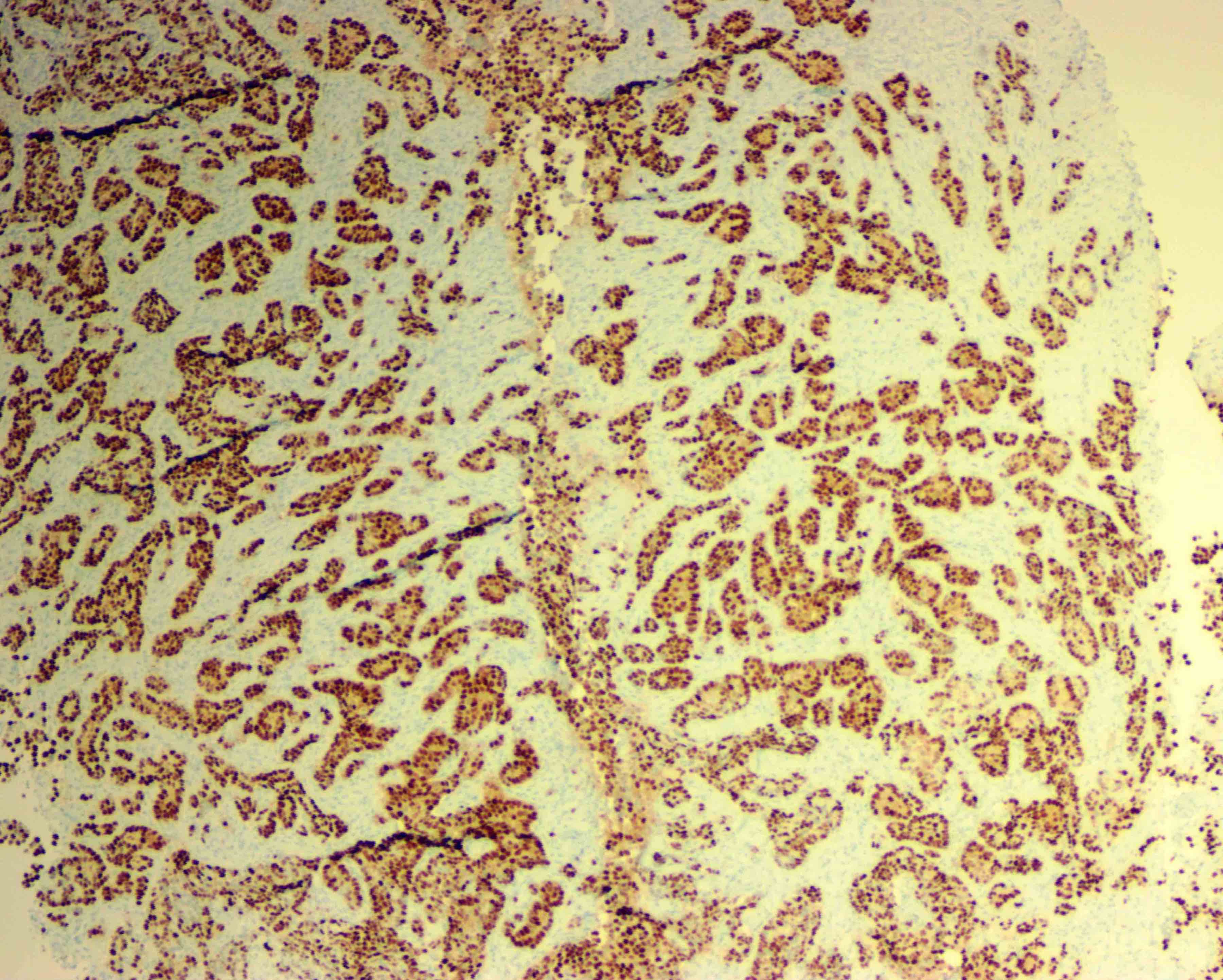
- Most are ductal carcinoma in situ or invasive ductal carcinoma
- Most are ER+ (Ann Oncol 2013;24:viii75)
- BRCA2 is the strongest familial risk factor in men (associated with 17% of male breast cancers) (Histopathology 2016;68:110)
Terminology
- Invasive ductal carcinoma, ductal carcinoma in situ
ICD coding
- ICD-10: C50 - malignant neoplasm of breast
Epidemiology
- Average age of onset of DCIS is sixth decade; for invasive carcinoma is seventh decade, although highest incidence occurs in the eighth decade of life (Breast Cancer Res Treat 2004;83:77)
- Incidence is lower in Japanese and higher in African Americans from West Africa and United States when compared to Caucasians from United States
- Death rate is higher among nonwhite men in the United States and lower among Japanese men in Japan (J Natl Cancer Inst 1978;60:1223, Am J Public Health Nations Health 1963;53:890)
- Despite the differences in the hormone receptor and HER2 status expression among the different races and ethnicities, no difference in the overall survival (Cancer 2013;119:1611)
- 2x increased risk among first degree relatives of male breast cancer patients
Sites
- Tend to be located centrally in retroareolar position and also in upper outer quadrants
Etiology
- Associated with increased serum estrogen: liver disease, obesity, exogenous therapy, antiandrogen therapy
- Associated with decreased serum androgen: Klinefelter syndrome, testicular injury / atrophy, occupational exposure to high temperatures
- Drugs, exogenous agents: digitalis, tricyclic antidepressants, marijuana, lavender oil, tea tree oil
- Radiation
- Pituitary gland dysfunction: hyperprolactinemia
- Hereditary: BRCA2 mutation carriers, PTEN mutation (Cowden syndrome), CHEK2 mutation carriers
Clinical features
- Invasive carcinoma:
- Average age of presentation is 60 to 70 years, although can present in younger men and children
- ~75% present with a palpable mass
- Can also present with nipple retraction, ulceration or nipple discharge (serous); may be nodular and cystic
- Time lapse between symptoms and clinical consultation varies from 6 months to 1 year
- Tends to present with larger size and at a higher stage in men than in women
- Lymph node metastases are more common in men than women
- Axillary nodal staging is done by sentinel lymph node biopsy
- History of breast cancer does not significantly affect the age or stage at time of diagnosis or the prognosis (Cancer 1999;86:821)
- Annual clinical screening exam recommended in men with BRCA mutations
Diagnosis
- Clinical presentation, imaging findings and ultimately image guided biopsies of the lesion provide tissue for an accurate pathologic diagnosis
Radiology description
- No guidelines recommending mammographic screening for men have been established, even with documented genetic predisposition
- Mammographic findings in men with breast cancer reveal distinct lesions with invasive margins that contrast sharply with the surrounding fatty tissue
- Microcalcifications found in 9 - 30%
- Ultrasound: round mass with calcifications and papillary components like those seen in cystic or encapsulated papillary carcinoma
- Can be used to differentiate gynecomastia from carcinoma
- Inflammatory carcinoma of the male breast produces diffuse enlargement and thickening of the skin that can be detected by MRI
Prognostic factors
- Poor prognostic factors: lymphatic tumor emboli, tumor size over 2 cm, poor histologic differentiation, HER2 overexpression, p53 expression, amplification of CCND1 (11q13)
- Men with a prior diagnosis of breast carcinoma have a 30x increased risk of invasive carcinoma in the contralateral breast, increasing to 110x if the original diagnosis was before age 50
- Death rate is higher among nonwhite U.S. men and lower among Japanese men
- Most investigators believe men and women with the same stage disease have similar prognosis, but some believe men have poorer prognosis
- AR+ luminal type A male breast cancer (ER+ HER2-, tumor grade 1/2) has better overall survival at 5 years but not 10 years compared to female breast cancer (Breast Cancer Res Treat 2012;133:949)
Case reports
- 40 year old man with occult breast cancer first manifesting as axillary lymph node metastasis (Medicine (Baltimore) 2015;94:e1038)
- 72 year old man with acromegaly and breast cancer (BMC Cancer 2015;15:397)
- 75 year old man with bilateral synchronous breast cancer (Saudi Med J 2015;36:359)
Treatment
- Treatment recommendations for male breast cancer are based on guidelines established for female breast cancer
- Most men are treated with mastectomy and axillary lymph node dissection
- Radiation, hormonal therapy and chemotherapy are also used
- Breast conservation therapy may be possible, especially in older patients
- Tamoxifen has less mortality when compared to aromatase inhibitors in men with stage I - III ER+ carcinoma (Breast Cancer Res Treat 2013; 137:465)
Gross description
- Male breast cancers are grossly identical to female breast cancers; cystic papillary carcinomas can be striking
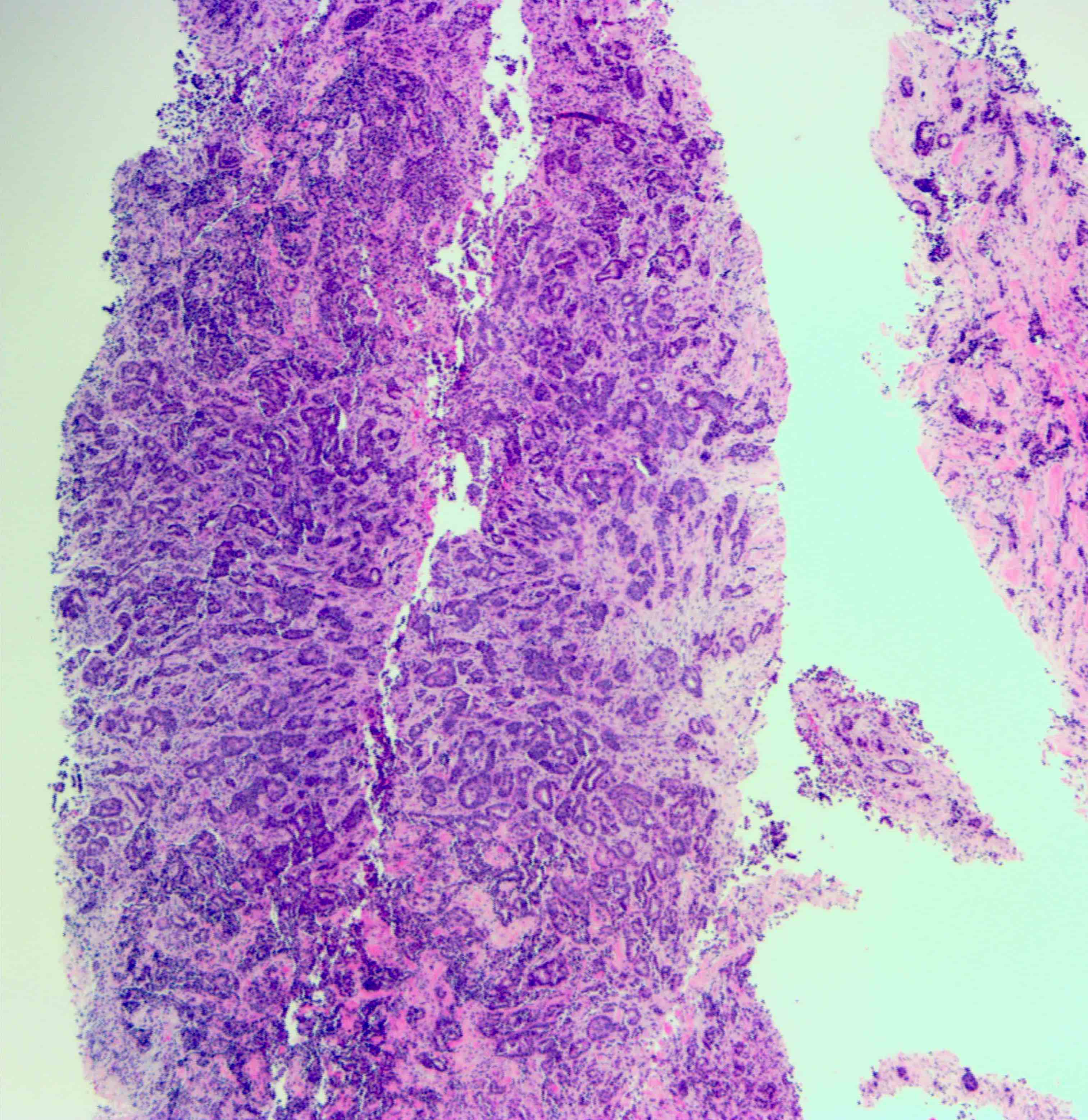
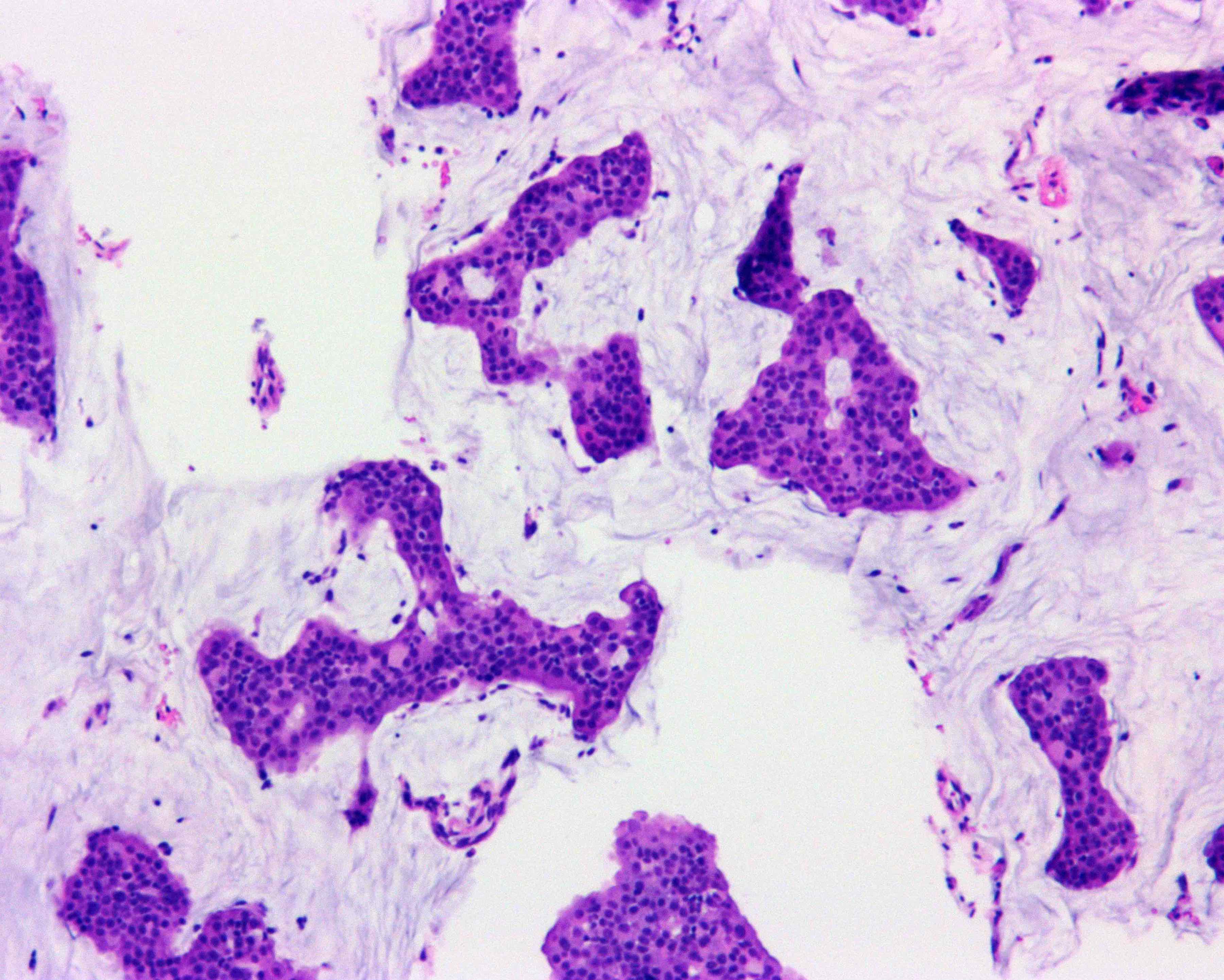
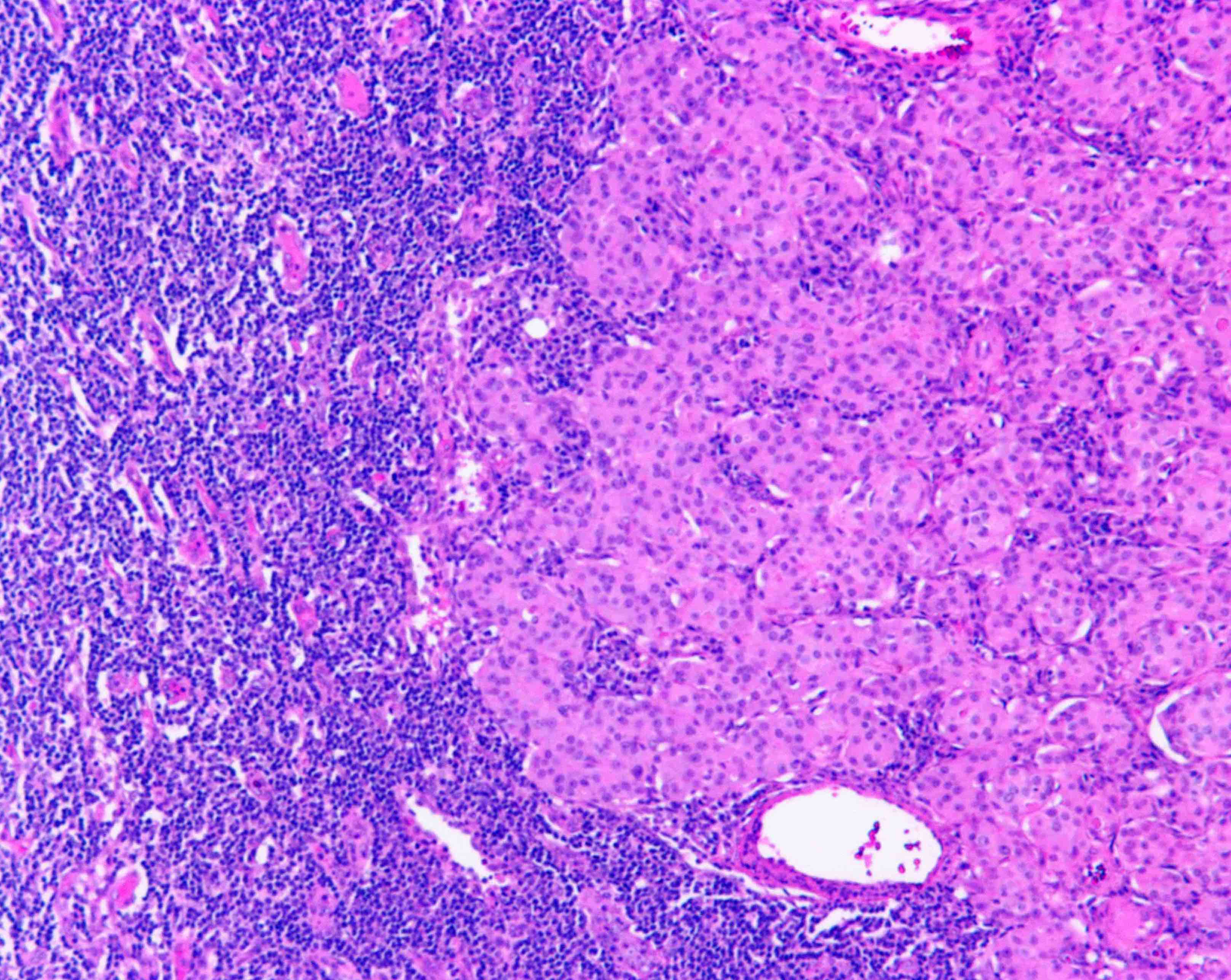
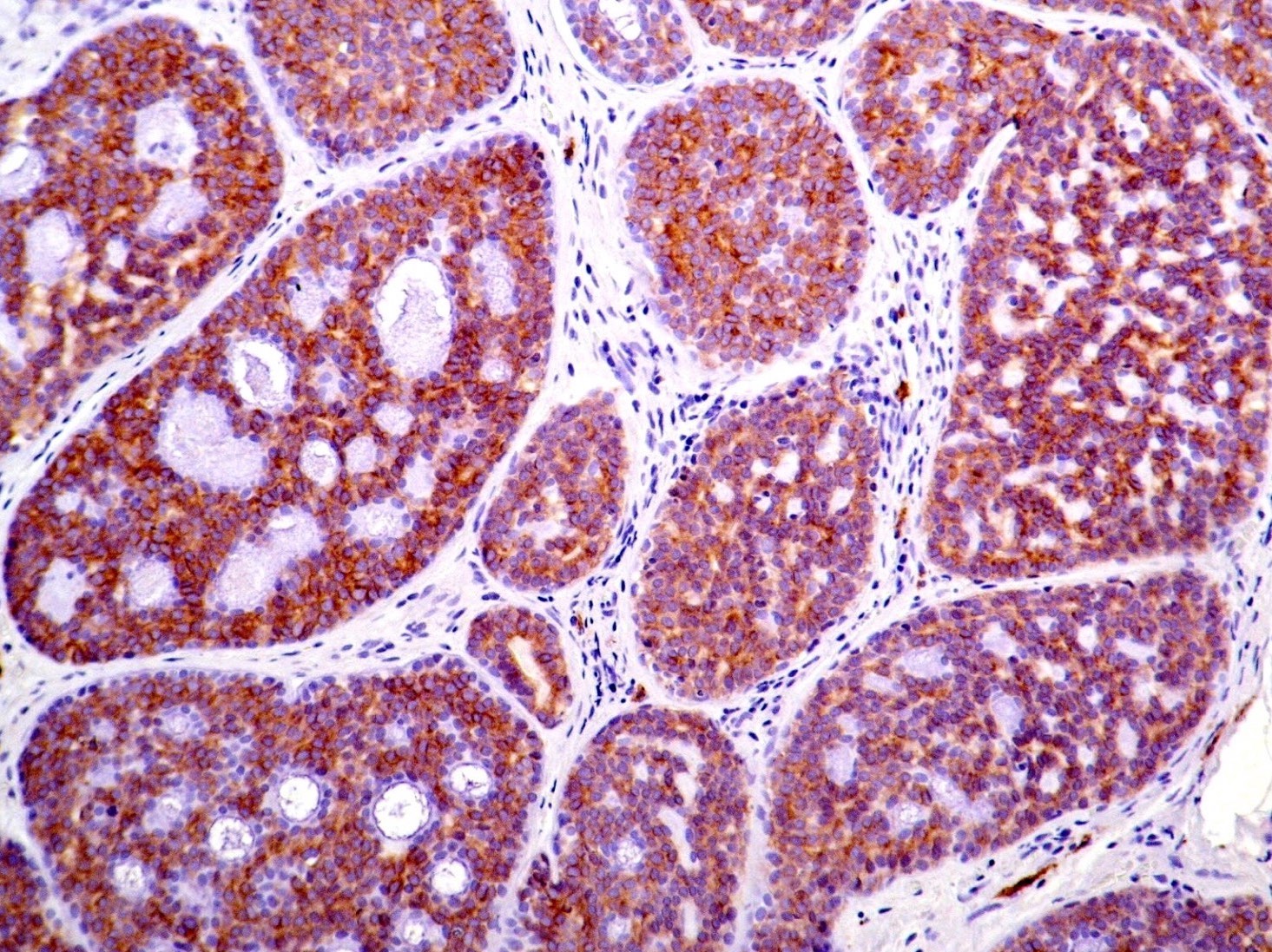
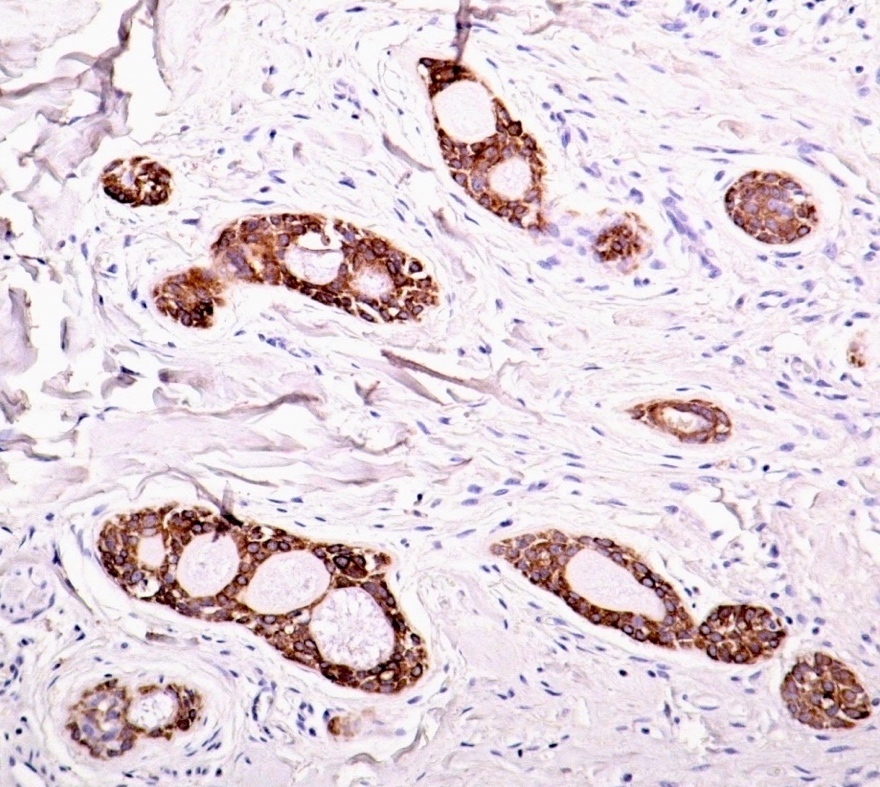
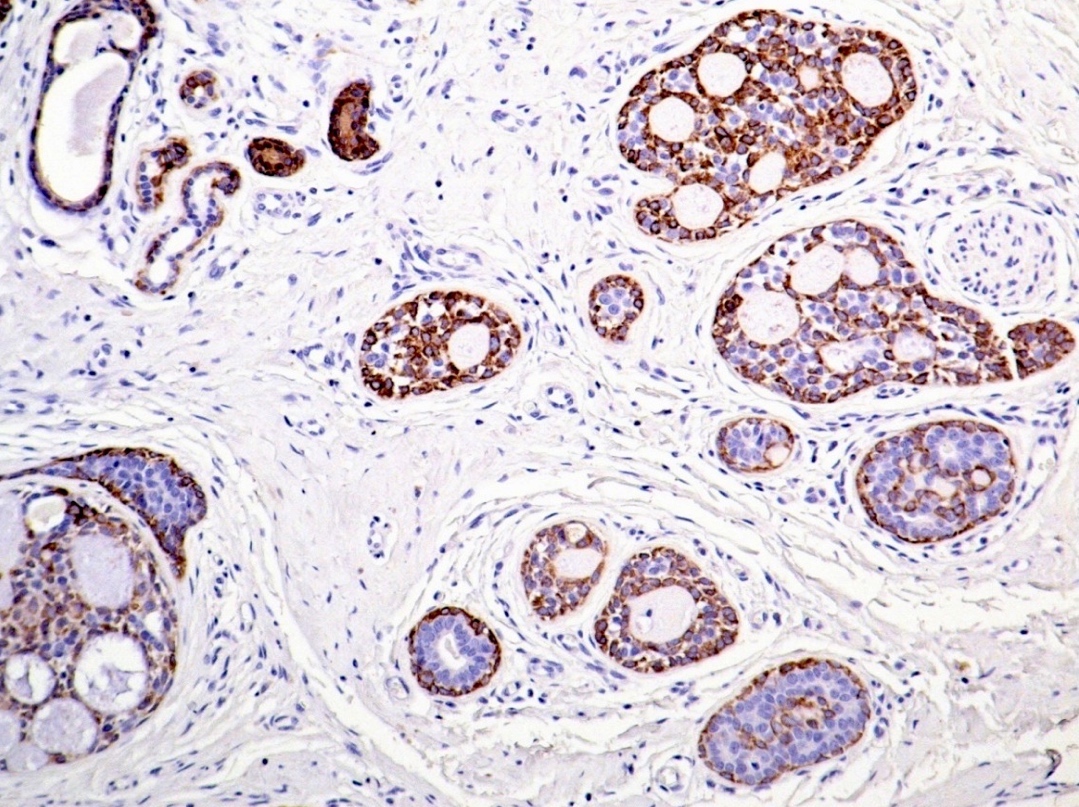
Microscopic (histologic) description
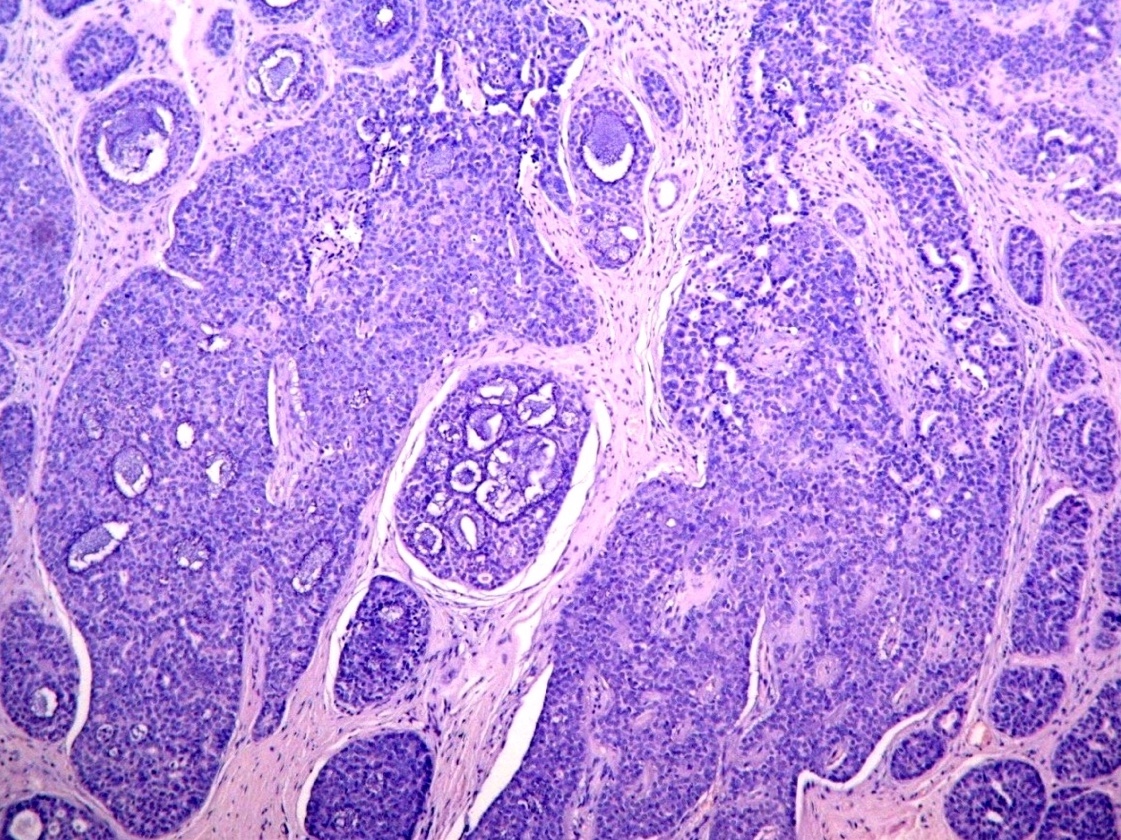
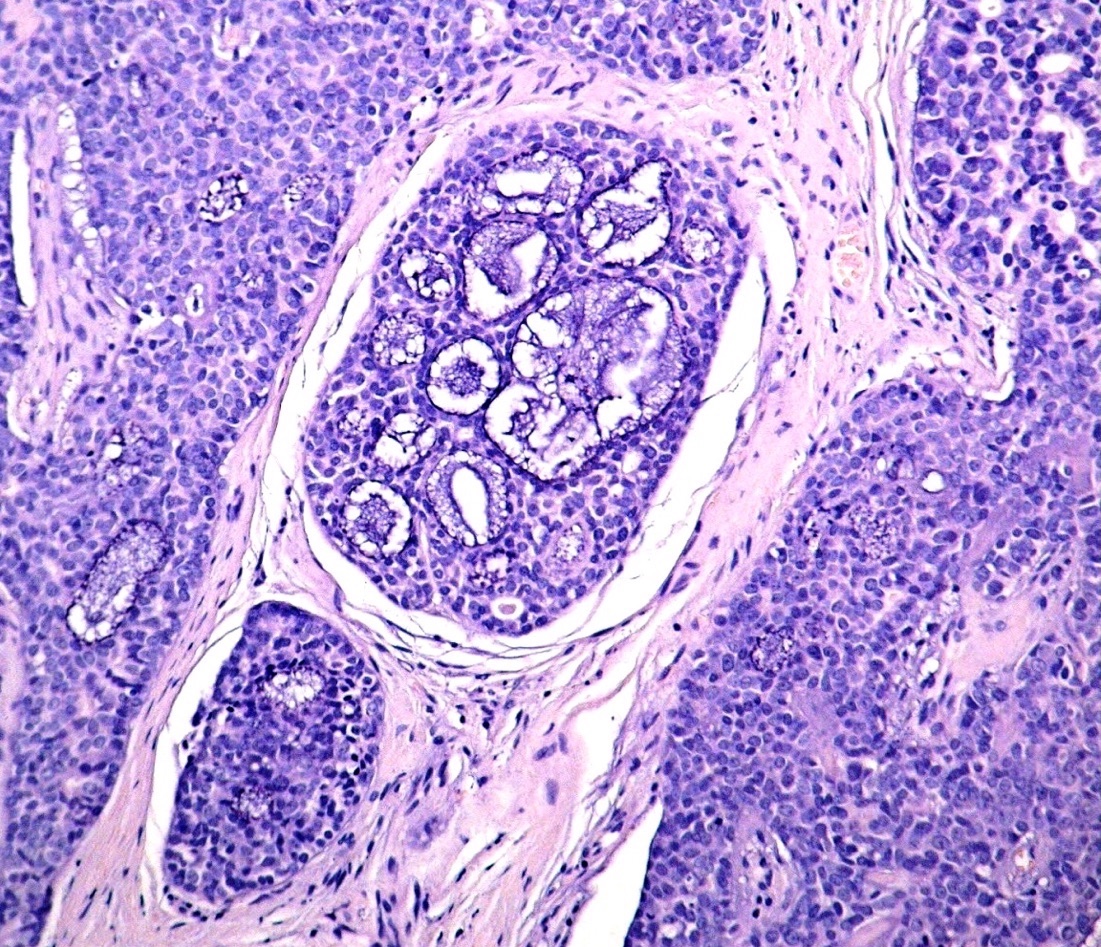
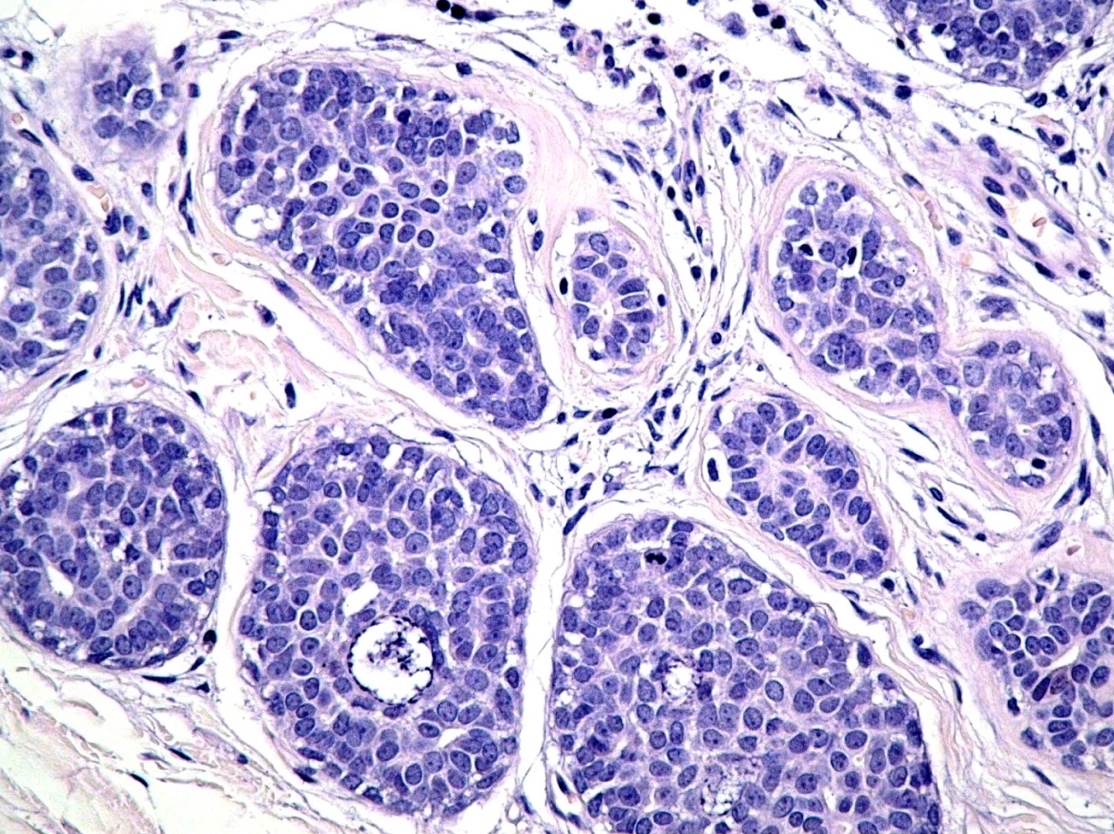
- In situ carcinoma with papillary architecture is the most common pattern; also cribriform, micropapillary and solid patterns
- Most (~85%) male breast carcinoma is poorly differentiated infiltrating ductal carcinoma, followed by papillary carcinoma and other types similar to female breast cancer
- Lobular carcinoma represents 2% of cases
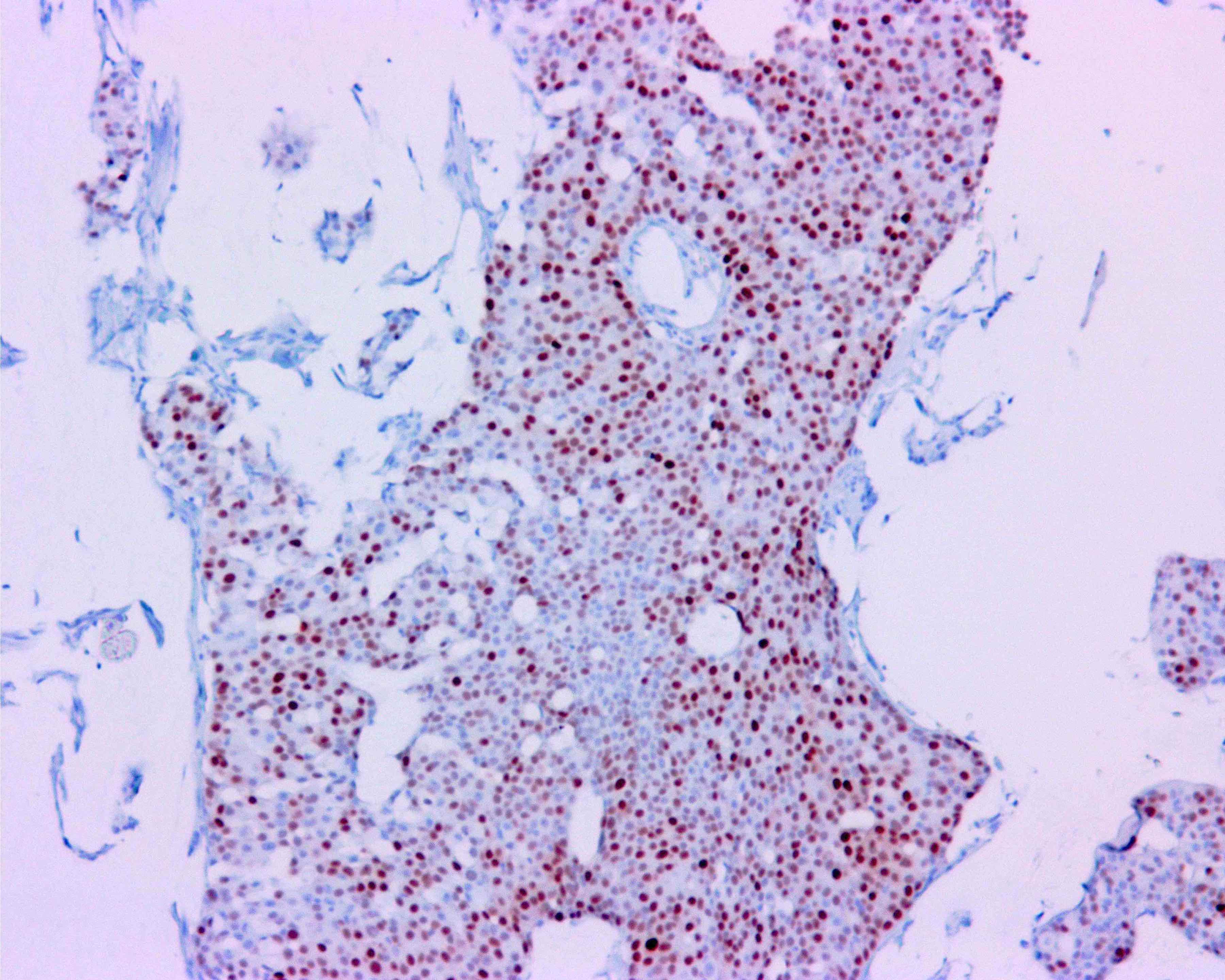
Microscopic (histologic) images
Cytology description
- Reliable but underused
- Dispersed epithelial cells with atypical features and high N/C ratio
- Cell clusters can be present in papillary tumors
- Gynecomastia present with sparsely cellular aspirate with loosely cohesive sheets of cells
Positive stains
Negative stains
- HER2 (usually)
Molecular / cytogenetics description
- p53 mutations in exon 6 found in over 90% of male cases compared to 33% of females with p53 mutations in exon 5 and 6 (Neoplasma 1996;43:305)
- Gene expression performed in 66 male breast cancer tumors revealed 2 unique subgroups (luminal M1 and M2) that were different in biologic features and outcome when compared to female breast cancers (Breast Cancer Res 2012;14:R31)
- EGFR and CCND1 genes are amplified more in male than female breast cancers
- High methylation status of MSH6, WT1, PAX5, PAX6, GATA5 and CDH13 correlates with more aggressive phenotype and poor survival
- Male and female breast cancers share many of these methylated genes but many genes are less frequently methylated in males
- Methylation of RASSF1A (downregulation of ER alpha and micro RNAs) is more common in male than female breast carcinomas
Differential diagnosis
- Gynecomastia: especially with radiation induced changes
Additional references
Board review style question #1
What is the most common type of male breast carcinoma?
- Invasive lobular carcinoma
- Invasive papillary carcinoma
- Mucinous carcinoma
- Poorly differentiated invasive ductal carcinoma
- Well differentiated invasive ductal carcinoma
Board review style answer #1
D. Poorly differentiated invasive ductal carcinoma. Approximately 85% of male breast carcinomas are poorly differentiated infiltrating ductal carcinomas, followed by papillary carcinomas and other forms similar to those found in female breast cancer. Lobular carcinomas represent 2% of cases.
Comment Here
Reference: Male invasive breast carcinoma
Comment Here
Reference: Male invasive breast carcinoma