Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Cytology - normal | Cytology - nonneoplastic findings | Cytology images | Positive stains | Negative stains | Sample pathology report | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Ren S. Normal and nonneoplastic findings. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cervixcytologybenignfeatures.html. Accessed October 5th, 2025.
Definition / general
- Normal and nonneoplastic findings in cervical components of Pap test for routine screening for cervical cancer
- Preparations: conventional and liquid based (ThinPrep and SurePath)
Essential features
- Normal cellular elements
- Squamous cells
- Superficial cells
- Intermediate cells
- Parabasal and basal cells
- Endocervical cells, endometrial cells and lower uterine segment cells
- Squamous cells
- Nonneoplastic findings
- Variations, reactive changes and inflammatory cells
Terminology
- Pap smear / test
ICD coding
- ICD-10: Z01.419 - encounter for gynecological examination (general) (routine) without abnormal findings
Cytology - normal
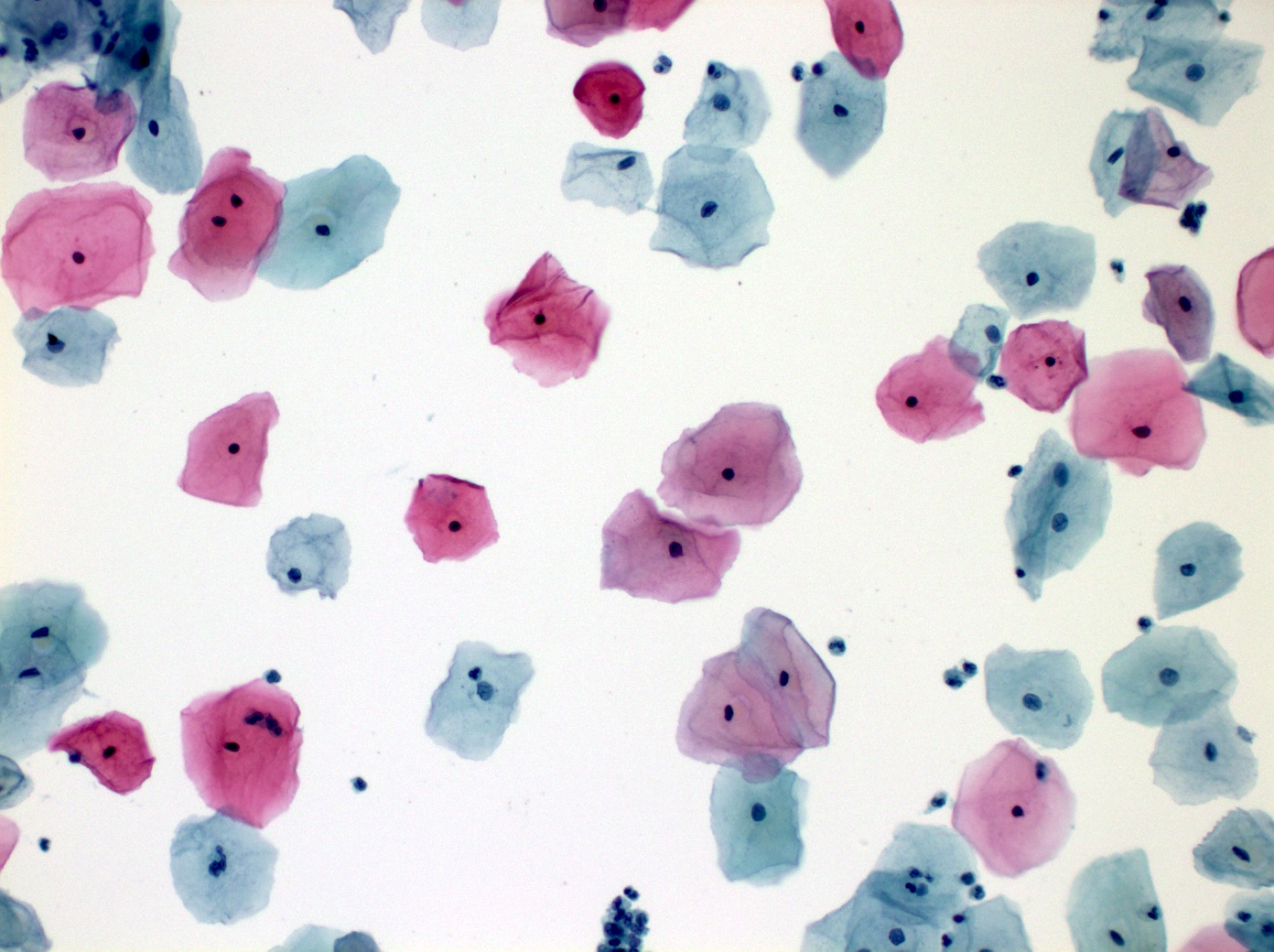
- Squamous cells: ectocervical stratified epithelium
- Superficial cells
- Outermost layer
- Small highly condensed / pyknotic nucleus
- Abundant, usually eosinophilic cytoplasm
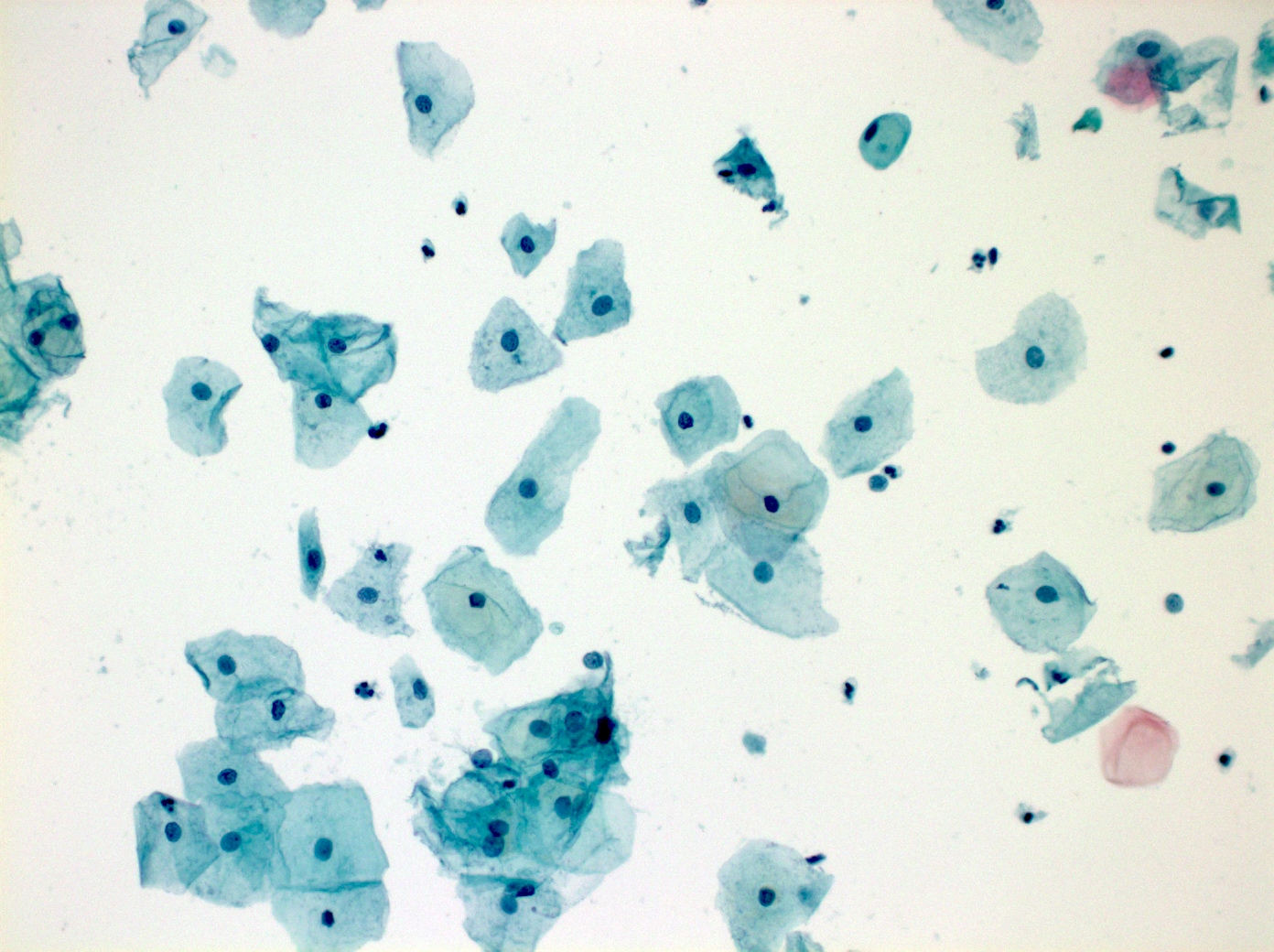
- Intermediate cells
- Middle layer
- Larger nucleus with finely granular chromatin and often longitudinal groove
- Abundant cytoplasm
- Parabasal and basal cells
- Also called immature squamous metaplastic cells
- Least mature cells
- Deep layer
- Nucleus larger than intermediate cells
- Scant cytoplasm, more granular and dense
- High N:C ratio
- Hallmark of atrophy
- Low estrogen state: premenarche, postpartum, postmenopause, Turner syndrome and postoophorectomy
- Superficial cells
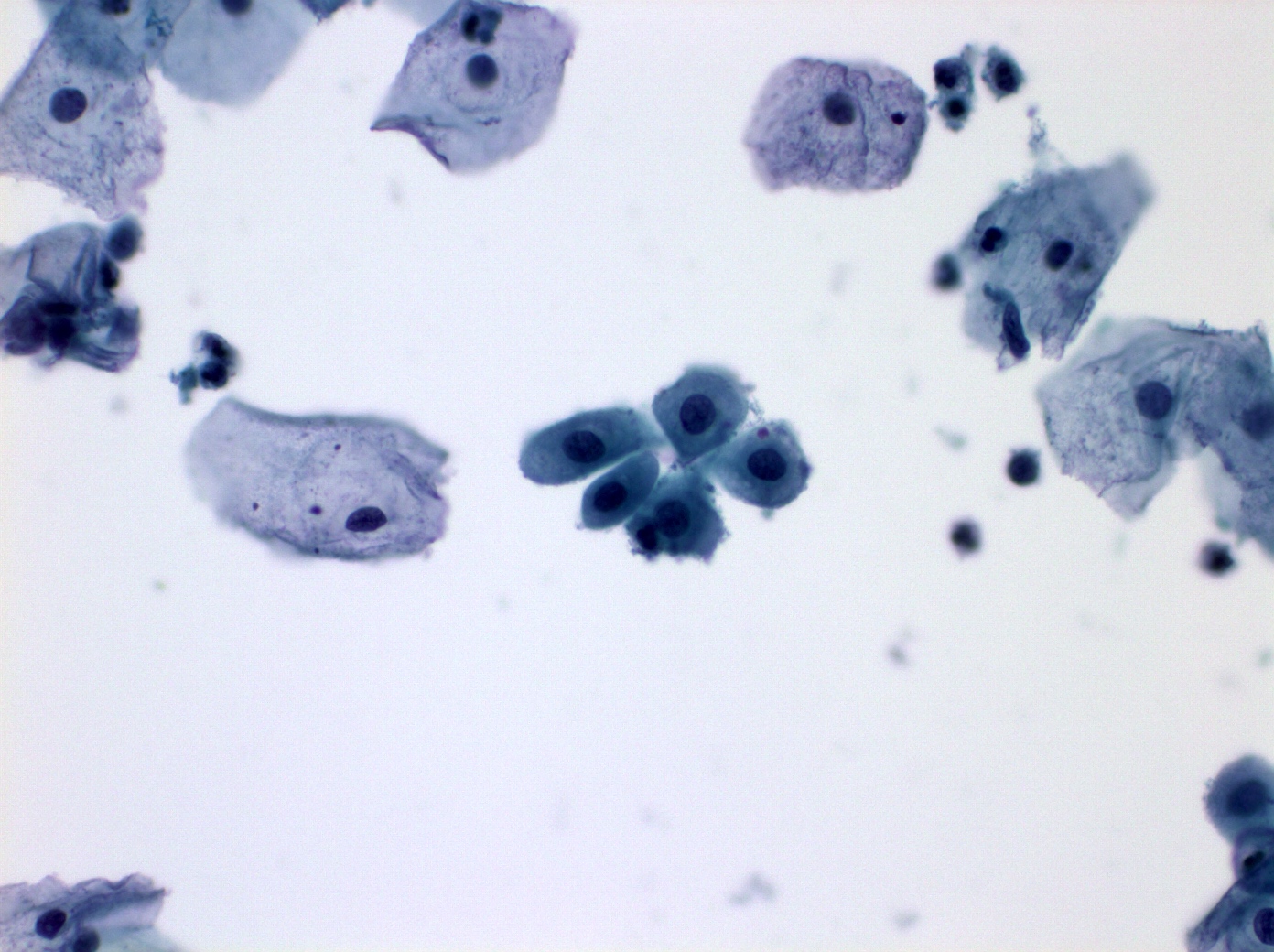
- Endocervical cells
- Picket fence or honeycomb configuration
- Mucin producing glandular cells with polarity, nuclei at one end and mucus at the opposite end
- Nucleus slightly larger than intermediate cell nucleus
- Nucleus with finely granular and even chromatin and small nucleoli
- Vacuolated or granular cytoplasm
- Endometrial cells and lower uterine segment cells
- Glandular cells, tight clusters or isolated
- Smaller than endocervical cells
- Nucleus equal or slightly smaller than intermediate cell nucleus, dense heterogeneous chromatin
- Scant cytoplasm, dense or vacuolated
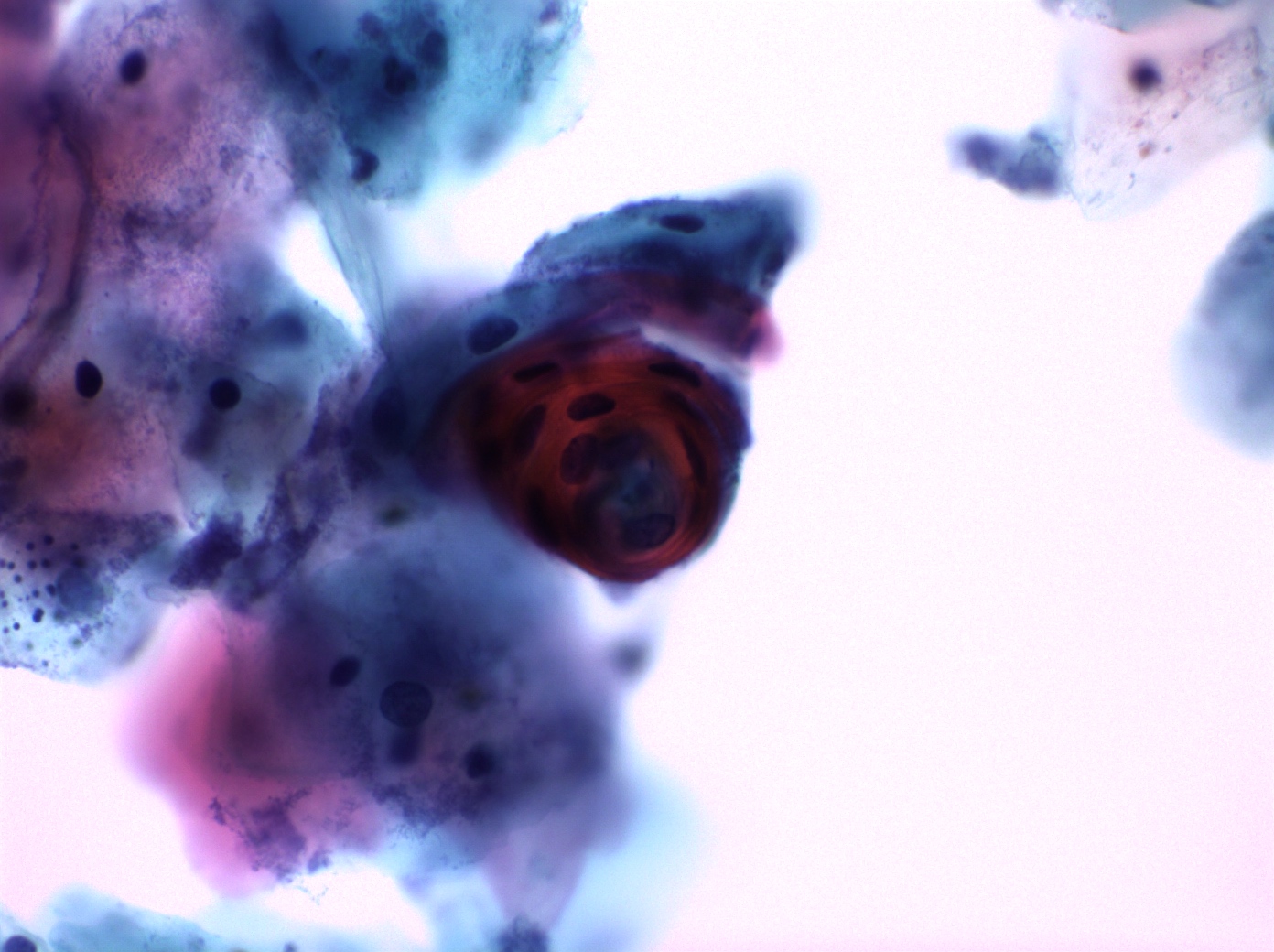
- Exodus: exfoliated dense aggregates of endometrial stromal cells with a surrounding layer of glandular epithelium
Cytology - nonneoplastic findings
- Variations
- Bland nuclear enlargement
- Squamous metaplasia: replacement of endocervical cells
- Stimulated by trauma, infection or inflammation
- Spectrum of morphologic changes
- Immature parabasal-like cells
- Intermediate / superficial cells-like squamous cells
- Hyperkeratosis
- Anucleate mature polygonal squamous cells
- Empty spaces or ghost nuclei
- Parakeratosis
- Miniature superficial squamous cells with dense eosinophilic cytoplasm
- Small and dense nuclei
- Tubal metaplasia (Diagn Cytopathol 1993;9:98)
- Replacement of endocervical epithelium by fallopian tube-like epithelium with cilia and terminal bar
- Pregnancy related changes
- Navicular cells
- Variant of intermediate cells with boat-like appearance
- Incomplete maturation of the squamous epithelium associated with pregnancy, postpartum, contraceptive use, androgenic atrophy and estrogen in men (Diagn Cytopathol 2000;23:161, Cancer 2002;96:74)
- Ellipsoid (boat shaped) squamous epithelial cells with cyanophilic / eosinophilic cytoplasm due to intracytoplasmic glycogen (golden, refractile and granular)
- Eccentric nuclei and thickened folded cell borders
- Can form dense clusters
- Decidual cells (Diagn Cytopathol 2013;41:886)
- Present in pregnancy, during the postpartum period, oral contraceptives and progestin releasing intrauterine devices (IUDs)
- Derived from hormonally stimulated endocervical or endometrial stroma containing abundant glycogen and glycoprotein
- Singly and rarely small clusters, the size of mature squamous cells
- Ill defined cytoplasm is abundant, granular or finely vacuolated
- Nuclear with prominent basophilic nucleoli, fine granular evenly distributed chromatin and smooth membrane
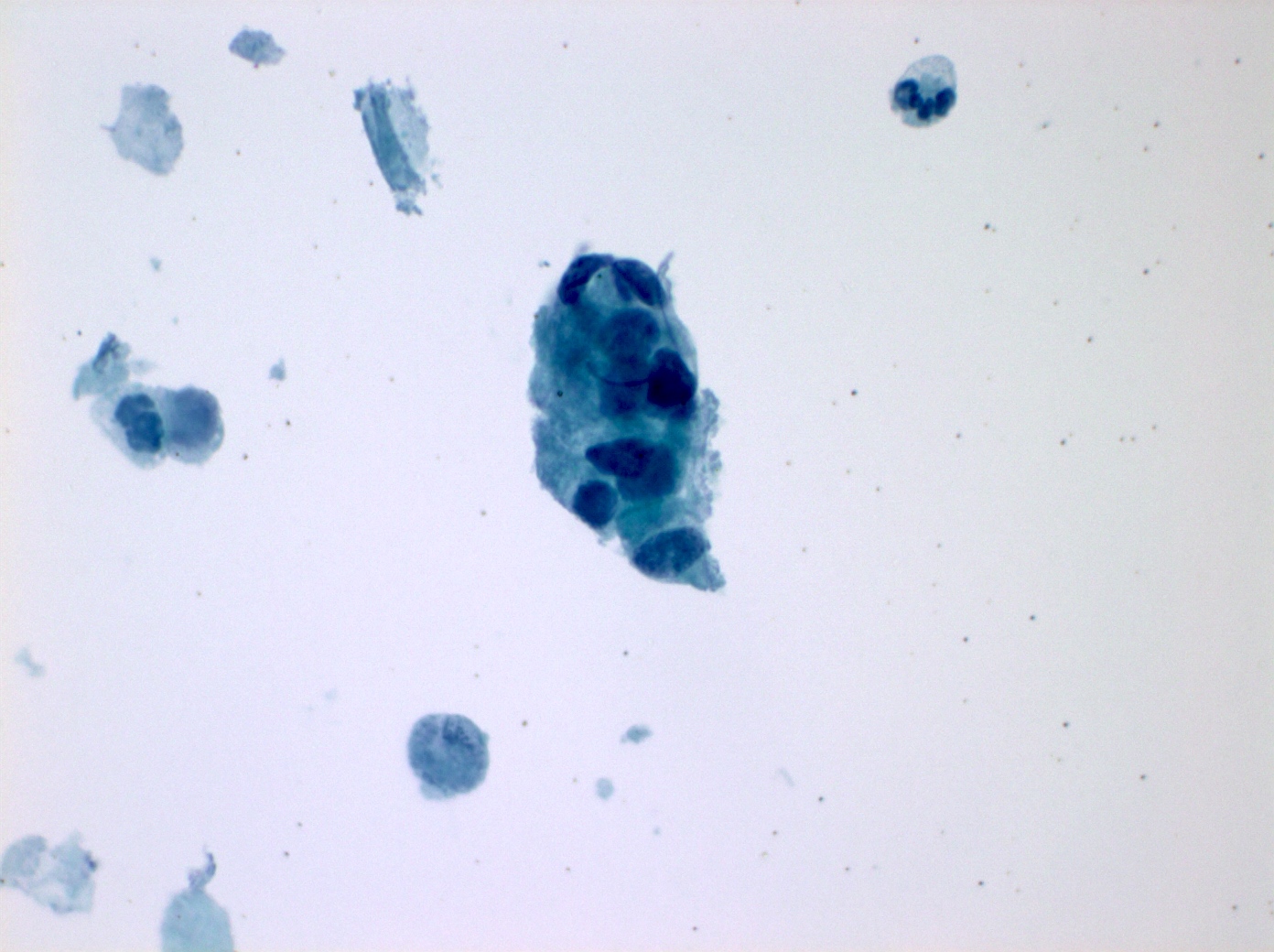
- Cytotrophoblast and syncytiotrophoblast
- Cytotrophoblastic cells
- Derived from the placenta in late pregnancy and postpartum
- Typically single cells, occasionally in small clusters
- May resembling small squamous metaplastic or endometrial cells, as well as high grade squamous intraepithelial lesion cells
- Small cells with enlarged nuclei, high N:C ratios, hyperchromasia with evenly distributed chromatin
- Scant dense cytoplasm with prominent vacuoles
- Syncytiotrophoblastic cells
- Derived from fusion of cytotrophoblastic cells in late pregnancy and postpartum period
- Large multinucleated cells with up to 50 or more nuclei in the center
- Normal chromatic nuclei, even chromatin distribution and irregular nuclear membranes
- Tapering / tail of granular cytoplasm at one end of the cell
- Cytotrophoblastic cells
- Arias-Stella reaction (Diagn Cytopathol 1996;14:349)
- In association with pregnancy or occasionally in nonpregnant hormonally stimulated individuals
- Reactive changes involving endocervical or endometrial glandular cells singly or in clusters in a clean background
- Large pleomorphic nuclei with irregular contour, granular to smudgy chromatin, multiple prominent nucleoli, no or very rare mitotic figures
- Variable cytoplasm, abundant, secretory
- Navicular cells
- Reactive changes (Nayar: The Bethesda System for Reporting Cervical Cytology, 3rd Edition, 2015, DeMay: The Art & Science of Cytopathology, 2nd Edition, 2011, DeMay: The Pap Test, 1st Edition, 2005)
- See also actinomycosis, bacterial vaginosis, Candida / fungi, Chlamydia trachomatis
- Atrophy
- Associated with lack of hormone stimulation, thin epithelium consisting of immature basal / parabasal cells
- Flat monolayer cells with preserved nuclear polarity and little nuclear overlap
- Slightly increased N:C ratio, naked nuclei, mild hyperchromasia and elongated nuclei, evenly distributed chromatin and smooth nuclear contour
- Blue blobs
- Pseudoparakeratosis: degenerated orangeophilic eosinophilic parabasal cells with nuclear pyknosis
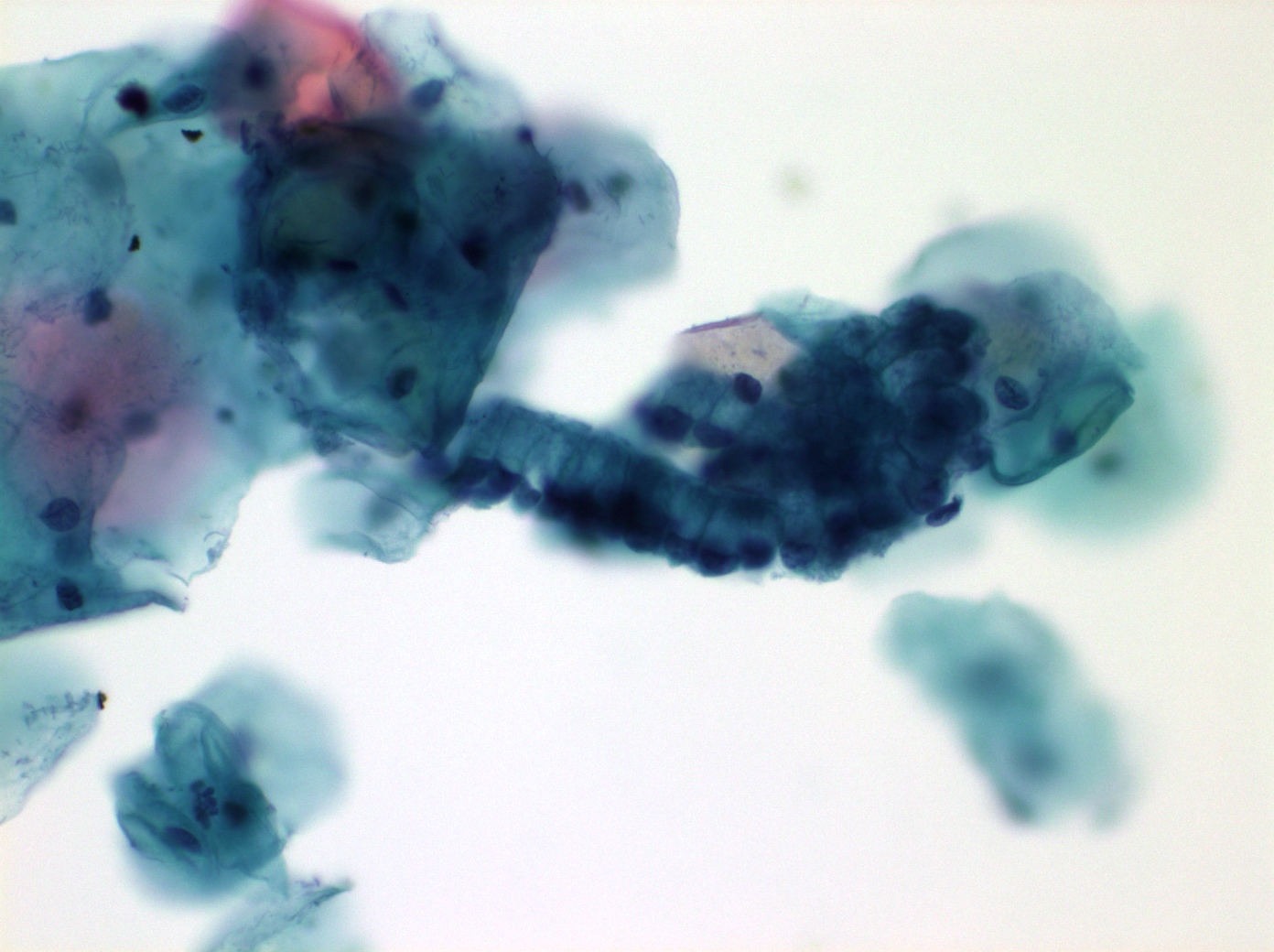
- Repair / regeneration with inflammation
- Enlarged cohesive sheets of cells with "school of fish" architecture
- Variable nuclear enlargement, not overlapping, may be binucleation or multinucleation
- Smooth nuclear contour, vesicular and hyperchromatic nuclei, evenly distributed chromatin, prominent nucleoli or bare nuclei (loss of cytoplasm)
- Cytoplasm showing polychromasia, vacuolization, perinuclear halos and well defined cytoplasmic boundaries
- Dirty background with inflammatory cells, granular debris and fibrin (Arch Pathol Lab Med 2001;125:134)
- Radiation effect
- Markedly enlarged cells, may be bizarre shaped, without increased N:C ratio
- Variable nuclear size, common binucleation or multinucleation, degenerative nuclear changes with nuclear pallor, wrinkling or smudging chromatin, and nuclear vascularization, nucleoli
- Cytoplasmic vascularization (earliest effect), polychromatic and intracytoplasmic polymorphonuclear leukocytes
- Reactive changes with intrauterine contraceptive device
- Reactive endometrial or endocervical columnar cells exfoliated singly or in clusters present in a clean background
- Cytoplasm with large vacuoles, displacing the nucleus
- Degenerated nuclei with wrinkled chromatin and cracking, prominent nucleoli
- Calcifications may resembling psammoma bodies
- Actinomyces-like organisms present in up to 25% of cases
- Perimenopausal (PM) cells
- Squamous cells from perimenopausal women
- Significant cause of atypical squamous cell (ASC) overdiagnosis in women ages 40 - 55 years, may be attributable in part to air drying artifact and subtle atrophic changes (Cancer 2001;93:100, Am J Clin Pathol 2005;124:58)
- Squamous cells with enlarged, smooth, bland nuclei, no hypochromasia
- In early menopause, there is an intermediate cell maturation pattern (DeMay: The Pap Test, 1st Edition, 2005)
- Small blue cells (Nayar: The Bethesda System for Reporting Cervical Cytology, 3rd Edition, 2015)
- Mimic of exfoliated endometrial cells, increase with age
- Clusters of naked nuclei, likely of parabasal squamous or reserve cell origin
- Some loose nuclear contour, evenly distributed granular chromatin, sometimes molding
- Inflammatory cells
- Present in different conditions
- Neutrophils, lymphocytes, plasma cells and histiocytes
- Artifact
- Barr body: darkly stained body attached to nuclear membrane
- Inactive X chromosome, present on nuclear margin, formed by telomere association (Proc Natl Acad Sci USA 1991;88:6191)
- Blue blobs: dark blue, rounded, amorphous masses
- Condensed mucus, degenerated bare nuclei or precipitating hematoxylin
- In postmenopausal women, represent parabasal / intermediate squamous cells with various degrees of degeneration (Acta Cytol 2000;44:547)
- May have string of pearls appearance on ThinPrep in postmenopausal atrophy (Diagn Cytopathol 2010;38:233)
- Cornflakes
- Brown artifact of air bubbles trapped on superficial squamous cells resulting in obscuring of nuclei
- More common on conventional than liquid based preparations
- It can be reversed by returning the slides through xylene and alcohol to water then restaining and recoverslipping
- Degeneration / air drying artifact
- Degenerative type changes due to delay in transfer of cells to the slide, inflammation or atrophy
- Cytoplasm is lost and moth eaten with vacuolization
- Chromatin is clumped, hazy, smudged or indistinct
- Chromatin rim has variable thickness and irregular contours but no sharp angles of malignancy
- Barr body: darkly stained body attached to nuclear membrane
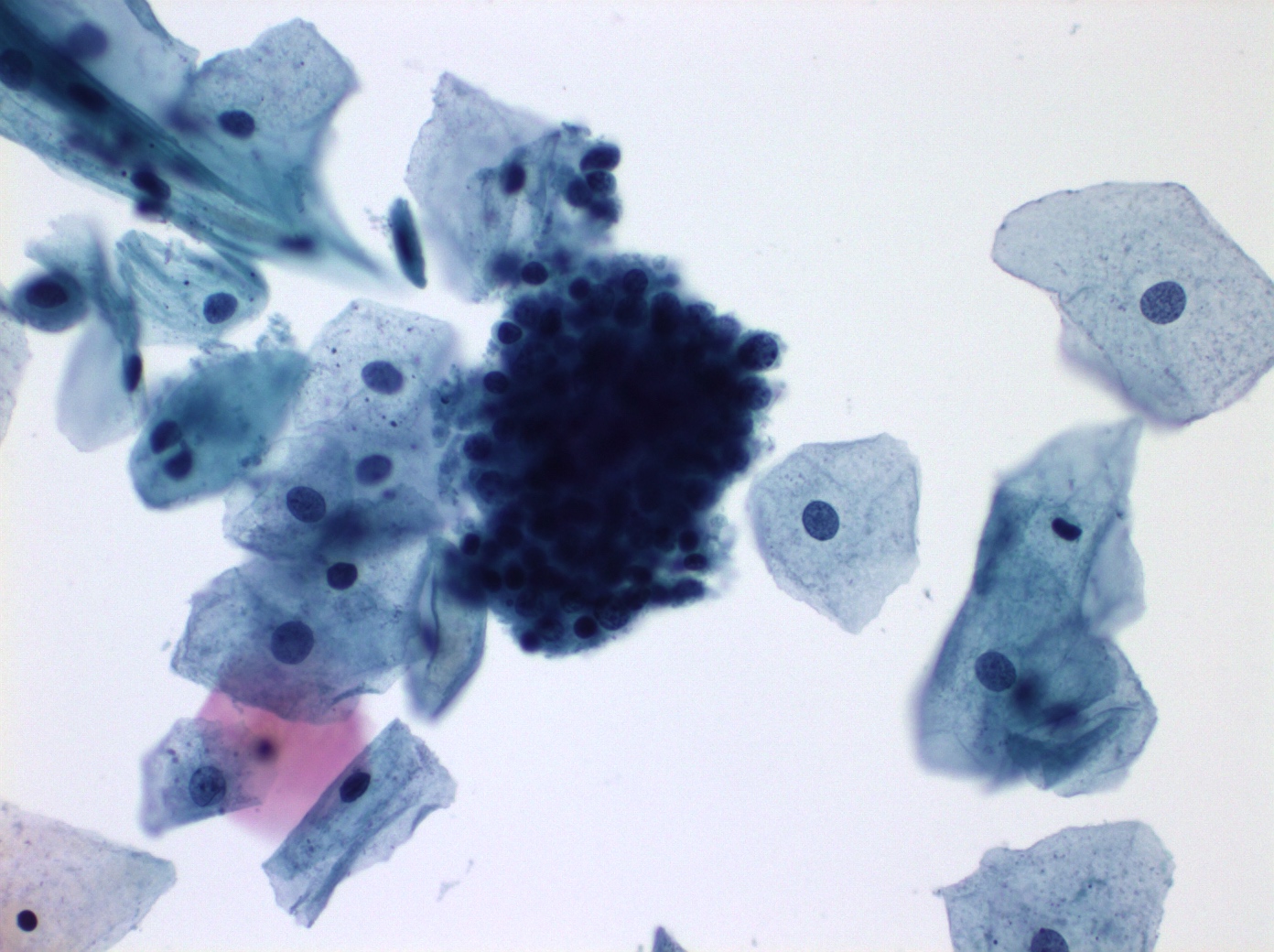
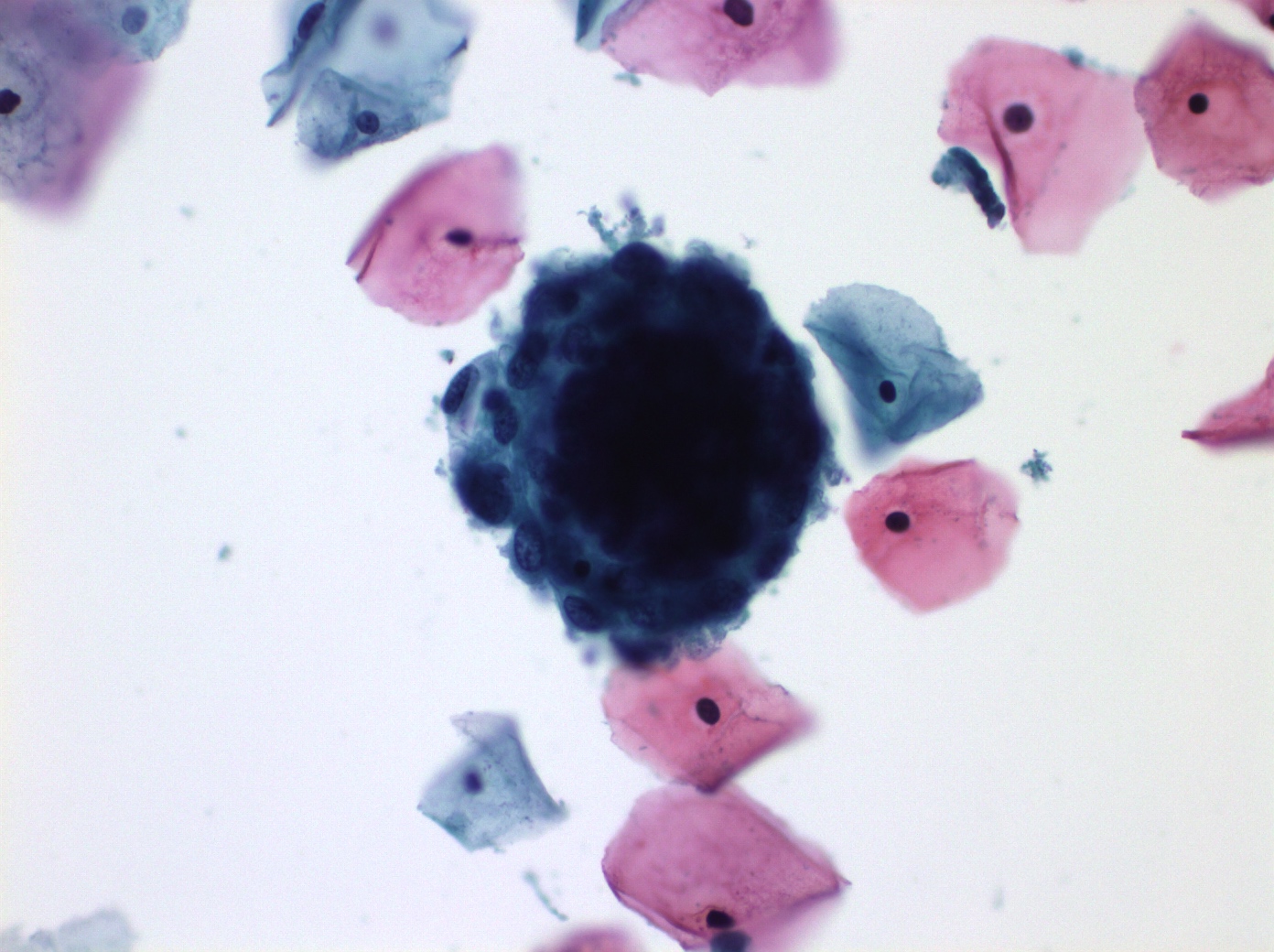
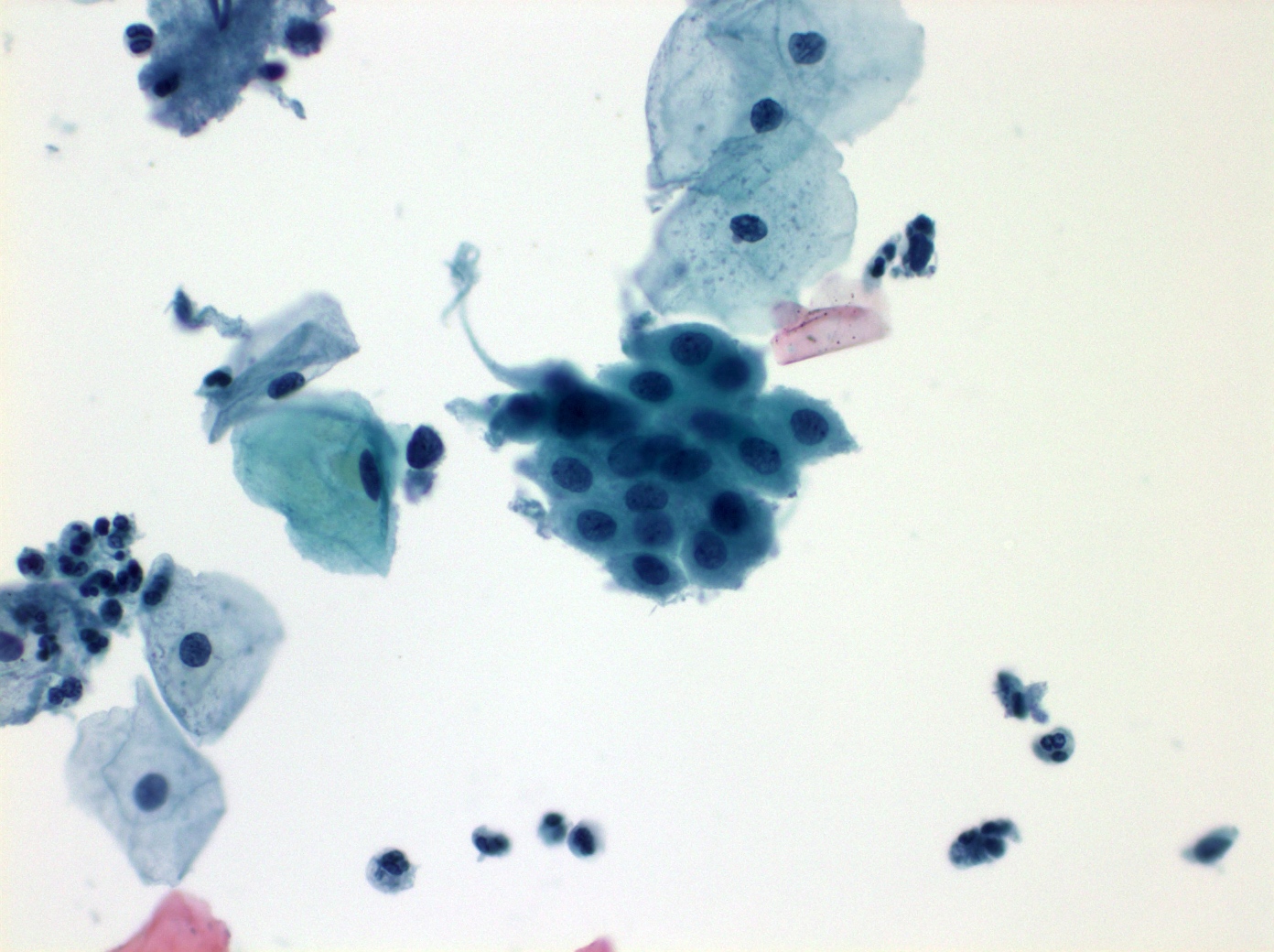
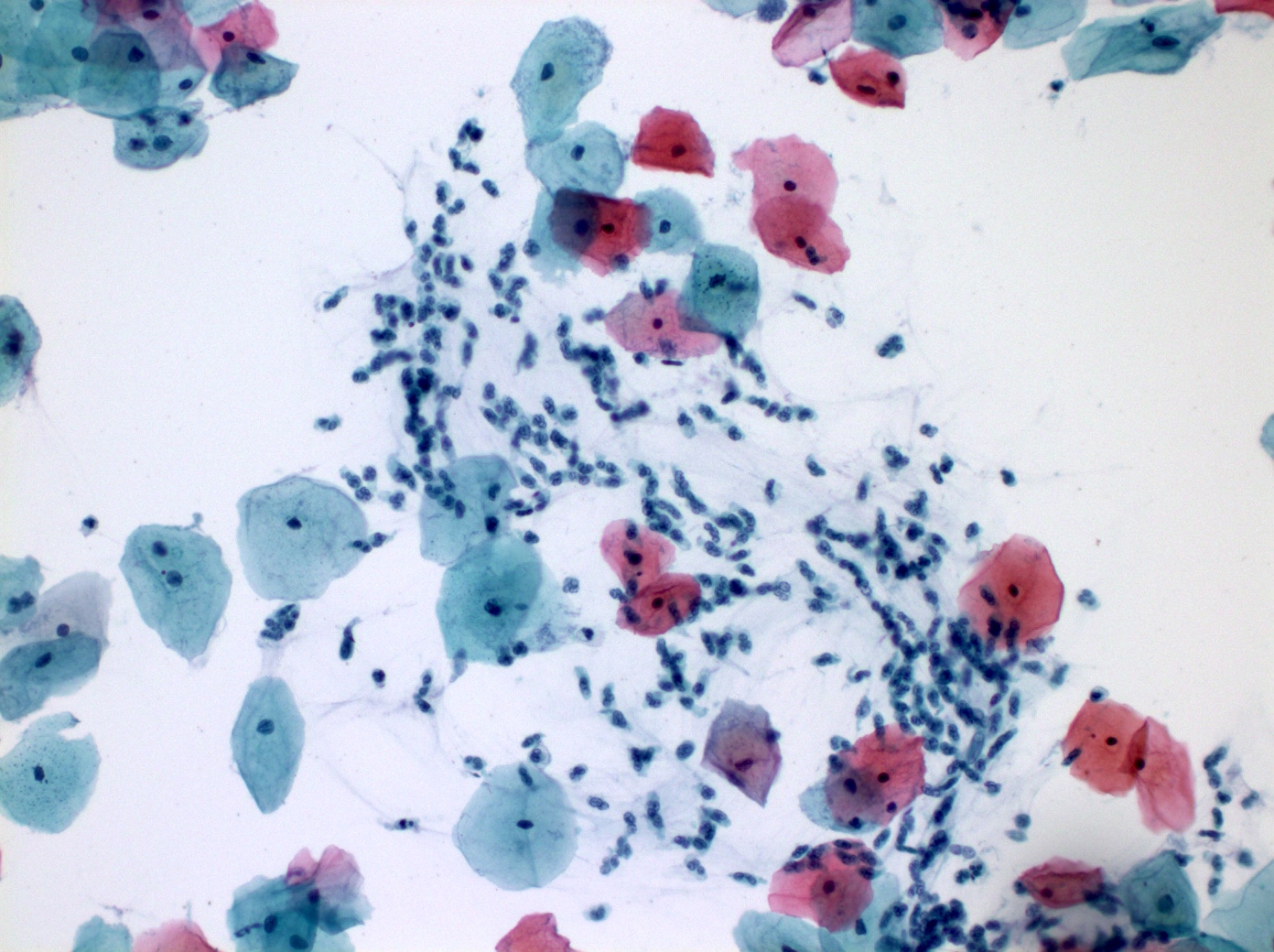
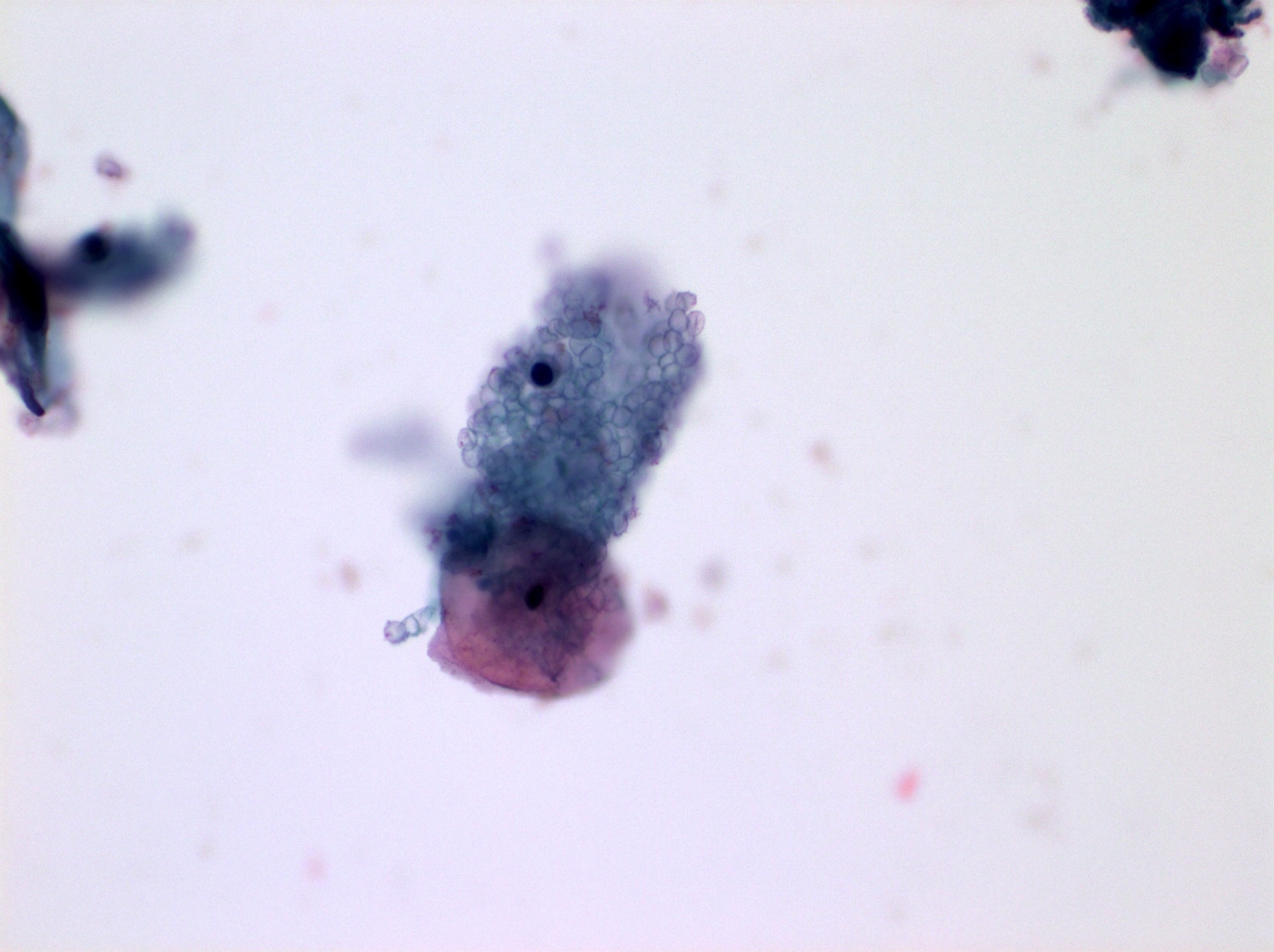
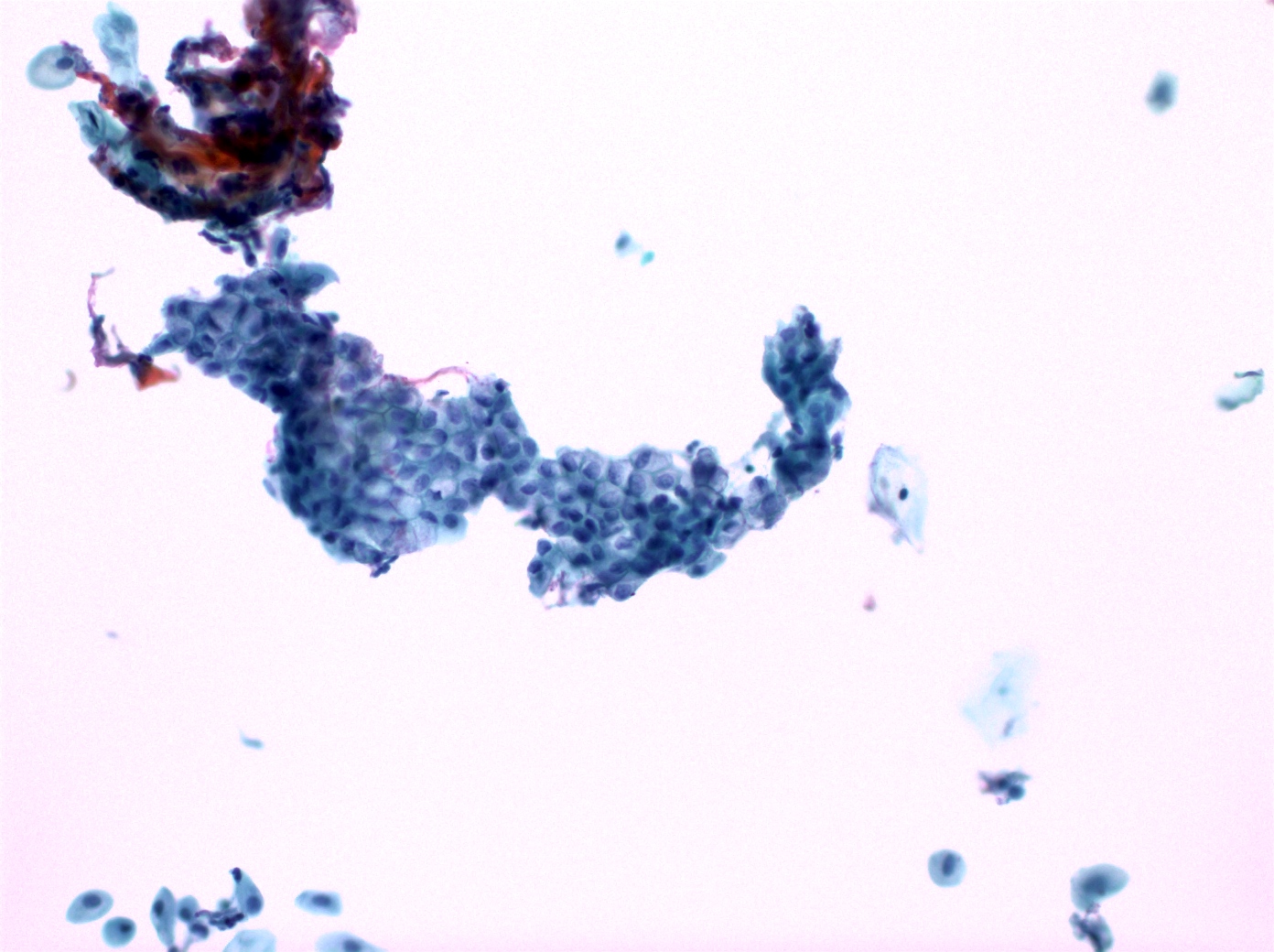
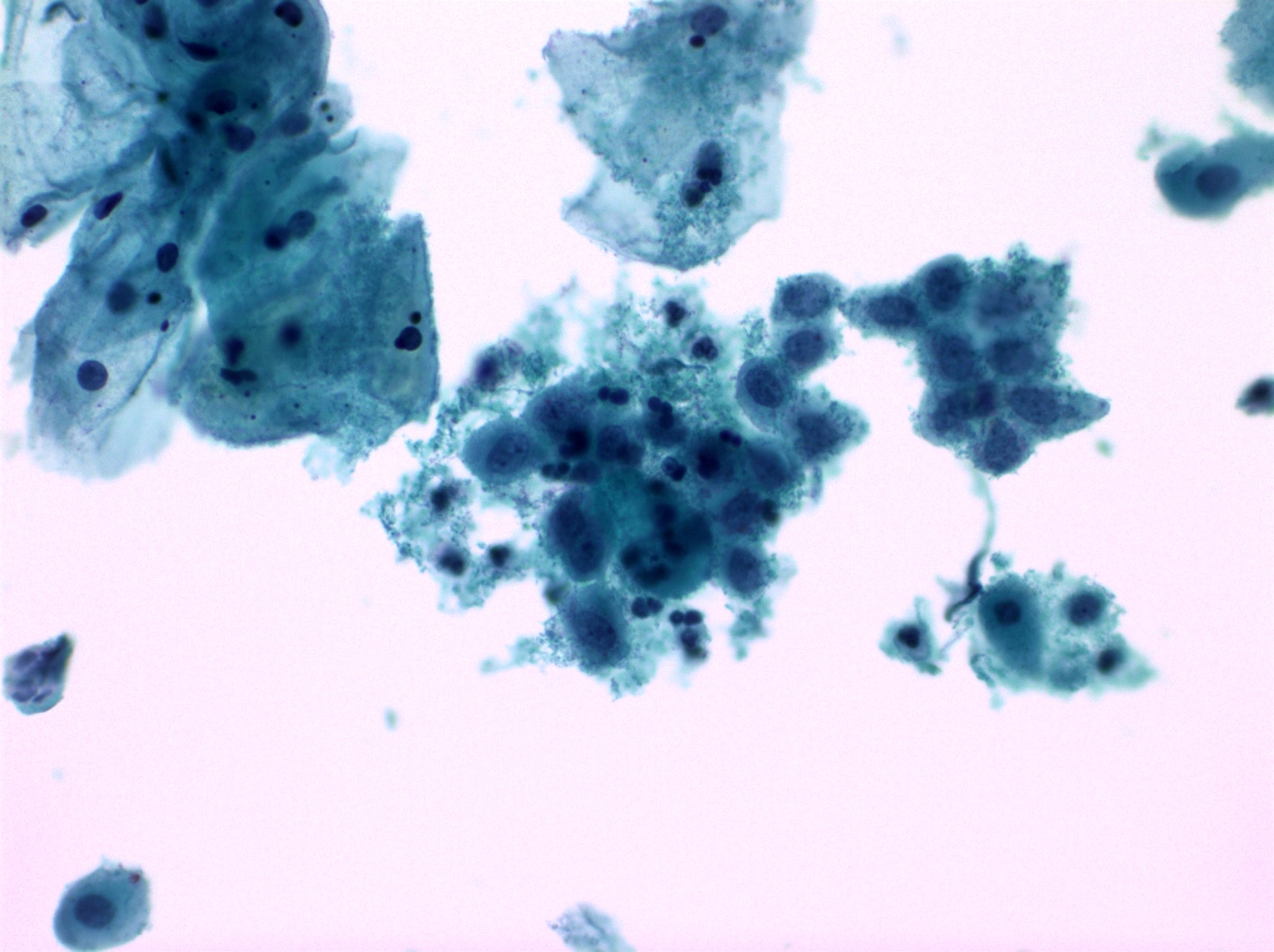
Cytology images
Contributed by Shuyue Ren, M.D., Ph.D.
Negative stains
- Benign squamous cells: p16
Sample pathology report
- Specimen adequacy:
- Satisfactory for evaluation; endocervical cells / transformation zone component present
- General categorization:
- Negative for intraepithelial lesion or malignancy
Additional references
Practice question #1
A 35 year old woman presents for routine gynecological examination and Pap test is performed. What kind of squamous cells are predominantly present?
- Basal cells
- Intermediate cells
- Parabasal cells
- Superficial layer cells
Practice answer #1
D. Superficial layer cells. Superficial squamous cells are typically observed in young women and abundant during the ovulatory phase of the menstrual cycle when estrogen levels are high. Answer A is incorrect because basal cells are immature squamous cells typically found in the deepest layer of the cervical epithelium. They are rarely seen in Pap smears, unless there is severe atrophy. Answer B is incorrect because intermediate squamous cells are immature squamous cells. These cells are often seen in response to hormone changes, like during pregnancy or postpartum. Answer C is incorrect because parabasal cells are immature squamous cells, often seen in conditions including atrophy, inflammatory change or hormonal imbalances.
Comment Here
Reference: Cervix cytology - Normal and nonneoplastic findings
Comment Here
Reference: Cervix cytology - Normal and nonneoplastic findings
Practice question #2
A 40 year old woman presents for routine gynecological examination and Pap test is performed. A tight cluster of bland 3D endometrial cells are noted. By 2015 Bethesda system, how do you report the cluster of cells?
- Endocervical cells, reported
- Exfoliated endometrial cells, not reported
- Exfoliated endometrial cells, reported
- Exodus ball, reported
Practice answer #2
B. Exfoliated endometrial cells, not reported. Exfoliated endometrial cells are not reported. By 2015 Bethesda system, exfoliated bland 3D endometrial cells should be reported in a woman ≥ 45 years of age. Answer A is incorrect because benign endocervical cells are not required to report. Answer D is incorrect because an exodus ball is a collection of peripheral glandular and central stromal endometrial cells, typically seen between day 6 and 10 of the menstrual cycle. Exodus is not required to report in a woman < 45 years of age. Answer C is incorrect because exfoliated endometrial cells are not required to report in a woman < 45 years of age.
Comment Here
Reference: Cervix cytology - Normal and nonneoplastic findings
Comment Here
Reference: Cervix cytology - Normal and nonneoplastic findings