Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Frozen section images | Microscopic (histologic) description | Microscopic (histologic) images | Cytology description | Positive stains | Negative stains | Electron microscopy description | Electron microscopy images | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Abdelzaher E. Pilomyxoid astrocytoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/cnstumorpilomyxoidastro.html. Accessed April 25th, 2024.
Definition / general
- A variant of pilocytic astrocytoma composed of monomorphous bipolar piloid cells with an angiocentric pattern in a myxoid background (MedGenMed 2004;6:42)
Essential features
- A variant of pilocytic astrocytoma with distinct histologic and clinical features
- Predominantly affects infants and young children
- Preferentially located in the hypothalamic / chiasmatic region
- Histologically characterized by small monomorphous bipolar cells, a myxoid background and perivascular arrangement
- Generally has more aggressive behavior than pilocytic astrocytoma due to local recurrence and cerebrospinal fluid dissemination
Terminology
- Pilomyxoid astrocytoma (PMA)
ICD coding
- ICD-O: 9425/3 - pilomyxoid astrocytoma
Epidemiology
- Rare tumor (Brain Tumor Pathol 2019;36:52)
- Tends to occur during infancy and early childhood (median 10 months) (Einstein (Sao Paulo) 2012;10:236)
- Male predominance (Am J Surg Pathol 2010;34:1783)
Sites
- Most common: hypothalamic / chiasmatic region
- Other less common sites: thalamus, cerebellum, brain stem, cerebral cortex and spinal cord (Brain Tumor Pathol 2019;36:52, Brain Pathol 2015;25:429, Am J Surg Pathol 2010;34:1783)
Pathophysiology
- Cell of origin is unclear
- Pilocytic and pilomyxoid astrocytoma may be part of a single disease spectrum
- They share common genetic alterations (BRAF duplication / fusion); some pilomyxoid astrocytomas mature into classic pilocytic astrocytomas over time and intermediate forms exist (Annu Rev Pathol 2013;8:361, J Neurooncol 2007;81:191, Am J Surg Pathol 2010;34:1783)
Etiology
- Associated with neurofibromatosis type 1 in a minority of cases (Pediatr Blood Cancer 2006;46:377)
Diagrams / tables
Clinical features
- Most common: manifestations of increased intracranial pressure or parenchymal compression (MedGenMed 2004;6:42)
- Some present with diencephalic syndrome (Einstein (Sao Paulo) 2012;10:236)
Diagnosis
- MRI with contrast
- Definitive diagnosis requires tissue biopsy
Radiology description
- MRI findings (Neurol Res 2008;30:945, MedGenMed 2004;6:42):
- Well circumscribed
- The majority (84.6%) are solid
- T1: isointense or hypointense signal
- T2 / FLAIR: hyperintense signal
- No diffusion restriction
- Homogeneous or heterogeneous enhancement pattern
- No peritumoral edema
- Craniospinal imaging is advisable to detect dissemination
Radiology images
Prognostic factors
- Displays a more aggressive behavior with a higher rate of local recurrence, a substantial rate of cerebrospinal fluid dissemination and shorter survival than pilocytic astrocytoma (Neurosurgery 2004;54:72, Brain Tumor Pathol 2019;36:52)
- Some have a favorable prognosis, especially if completely resected
- Better prognosis than diffuse astrocytomas
Case reports
- 3 month old girl with disseminated pilomyxoid astrocytoma with novel MUTYH mutation (BMJ Case Rep 2016 Oct 26;2016)
- 4 month old child with pilomyxoid astrocytoma of the right temporal / suprasellar region (Cytopathology 2017;28:74)
- 13 month old girl with giant sellar pilomyxoid astrocytoma (Int J Clin Exp Med 2018;11:1038)
- 11 year old girl with pilomyxoid astrocytoma of the brainstem (Rare Tumors 2013;5:65)
- 22 year old woman with a left frontal lobe pilomyxoid astrocytoma (J Cancer Res Ther 2015;11:667)
Treatment
- Surgery
- Chemotherapy and radiotherapy for recurrent tumors
- Targeted therapy is promising (Pediatr Blood Cancer 2014;61:2099)
Gross description
- Well circumscribed, solid gelatinous mass (Scheinemann: Pediatric Neuro-oncology, 2015)
- May be infiltrative
Frozen section description
- Perivascular bipolar cells in a mucoid background (J Ayub Med Coll Abbottabad 2014;26:611)
Frozen section images
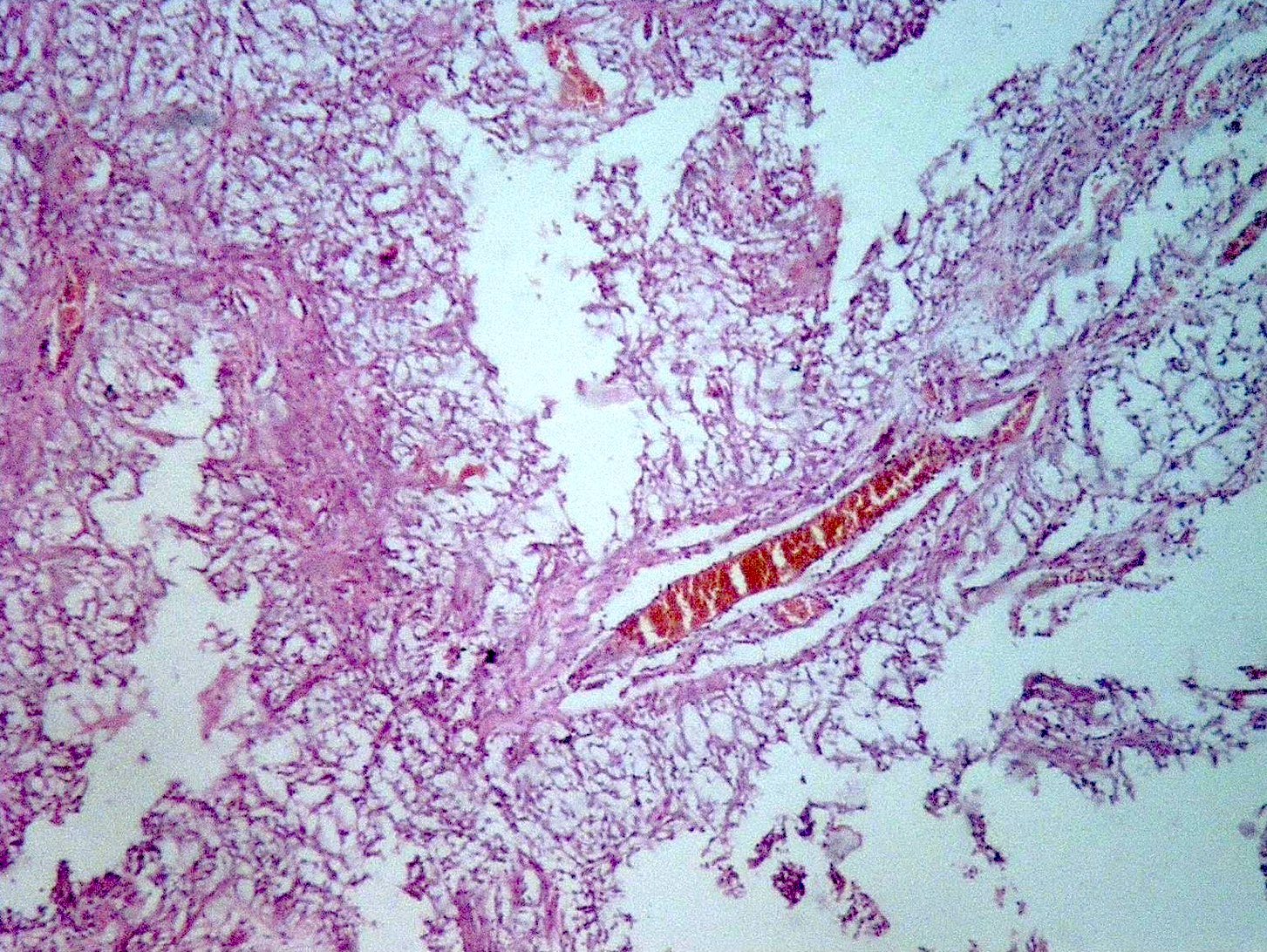
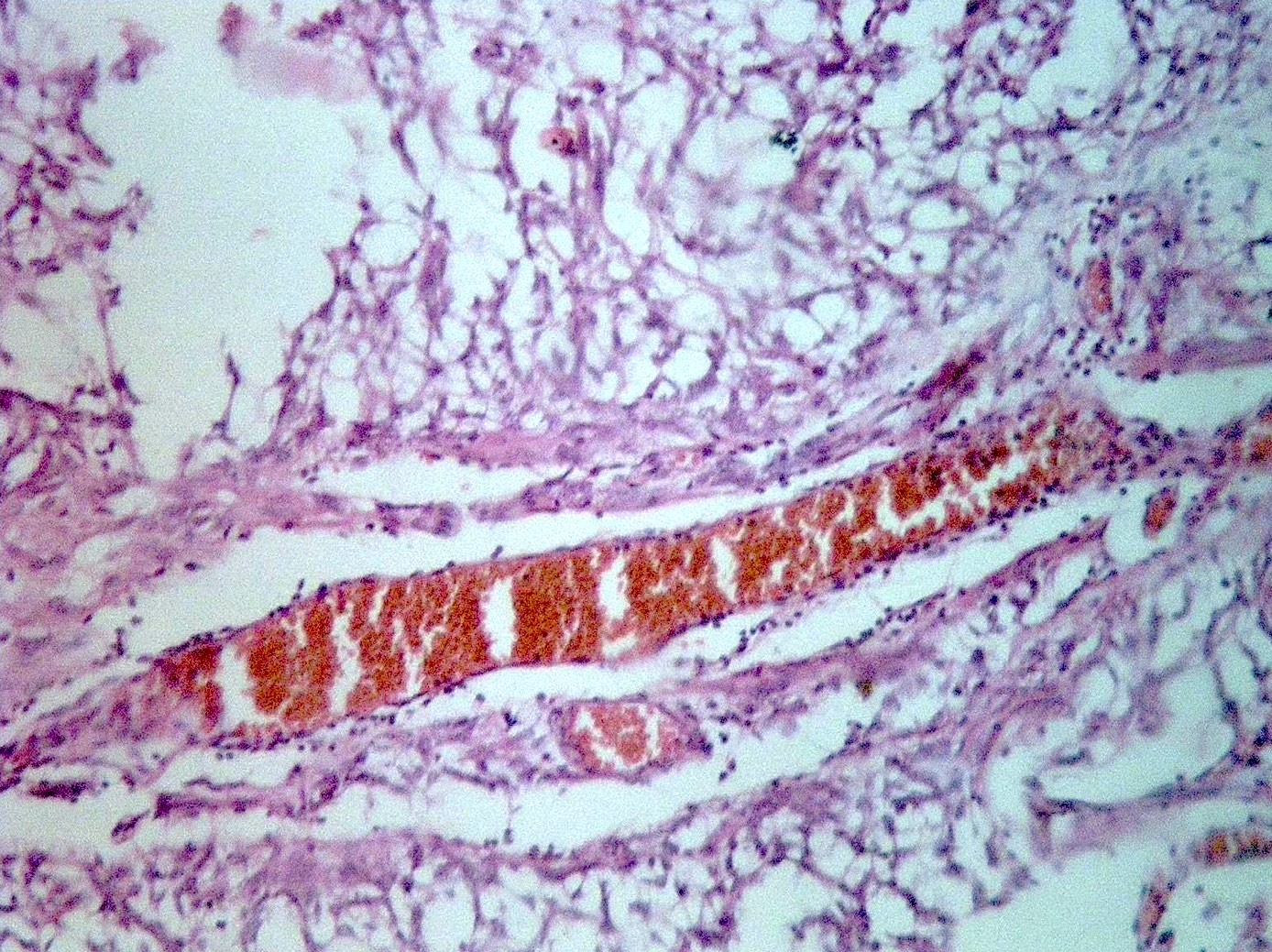
Microscopic (histologic) description
- Well demarcated, may be infiltrative (Brain Tumor Pathol 2019;36:52, Am J Surg Pathol 2010;34:1783)
- Solid and compact (i.e. the tumor is devoid of axons with negative staining for neurofilaments) (Acta Neuropathol 2015;129:775)
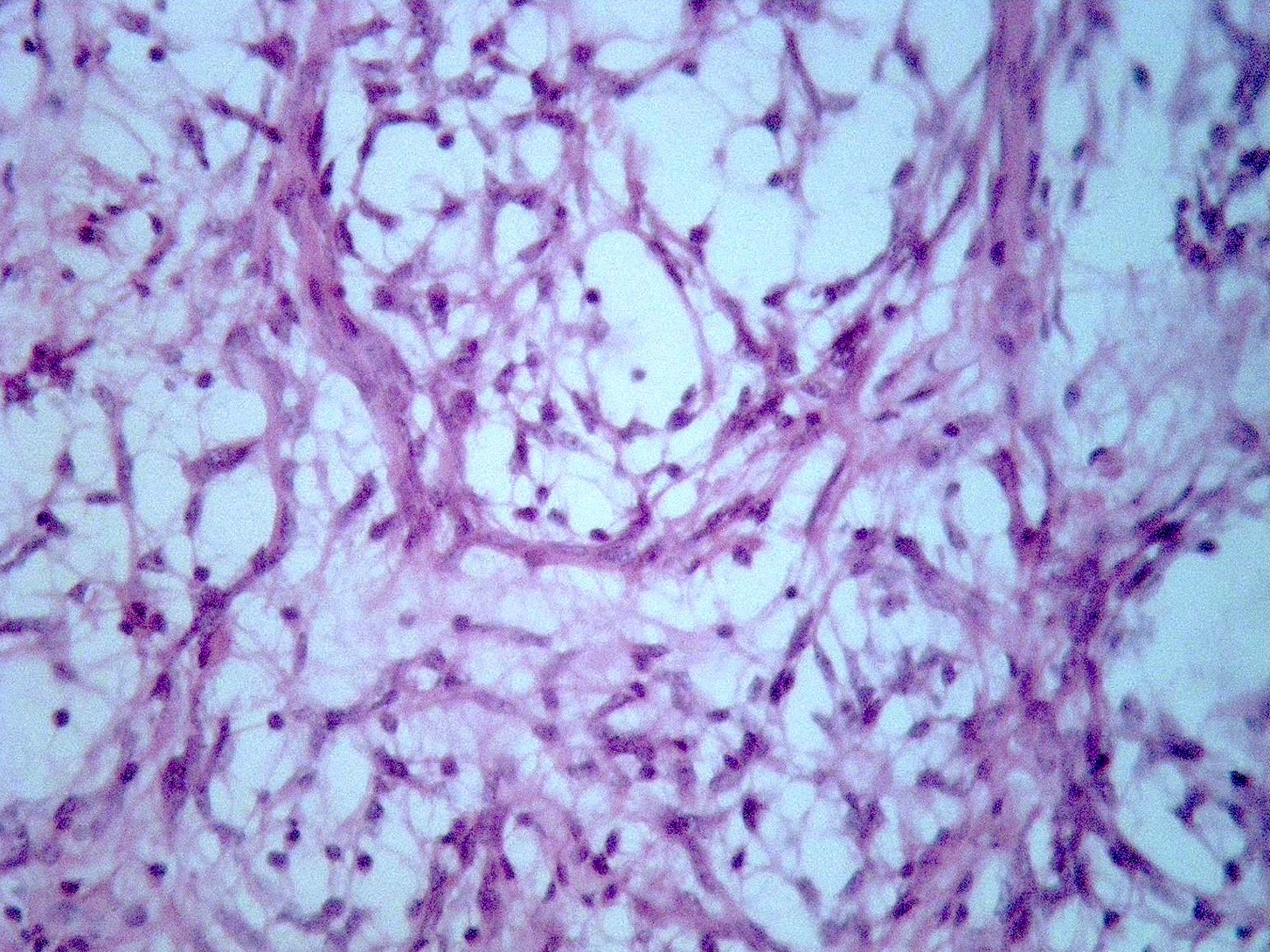
- Highly monomorphous, small bipolar piloid cells
- Angiocentric arrangement of tumor cells (perivascular pseudorosettes) with formation of pseudopapillary structures is typical (Acta Neuropathol 2015;129:775)
- Markedly myxoid matrix
- Low mitotic activity (Am J Surg Pathol 2010;34:1783)
- Uncommon: glomeruloid vascular proliferation, necrosis, eosinophilic granular bodies (Brain Tumor Pathol 2019;36:52, Am J Surg Pathol 2010;34:1783)
- Absence of classic pilocytic astrocytoma features such as biphasic (solid / microcystic) pattern or Rosenthal fibers (Brain Pathol 2015;25:429)
- See table above summarizing the histologic features of pilocytic and pilomyxoid astrocytoma (Neurosurgery 2004;54:72)
- Classic pilocytic astrocytomas with focal pilomyxoid changes should not be diagnosed as pilomyxoid astrocytomas
- Intermediate tumors with hybrid features of pilocytic and pilomyxoid astrocytoma were reported and tend to occur at older age than pilomyxoid astrocytomas (median = 36 months)
- This might represent a maturational effect as some pilomyxoid astrocytomas and intermediate tumors mature into pilocytic astrocytoma-like neoplasms over time (Am J Surg Pathol 2010;34:1783)
- According to WHO 2016 classification, a definite grade assignment for pilomyxoid astrocytoma is not recommended (Brain Tumor Pathol 2019;36:52)
Microscopic (histologic) images
Cytology description
- Similar to pilocytic astrocytoma but no Rosenthal fibers (Brain Tumor Pathol 2019;36:52)
- Monomorphous piloid cells with bipolar fibrillary processes and hyperchromatic, elongated nuclei (Brain Tumor Pathol 2019;36:52)
- Angiocentric arrangement
- Myxoid background
Positive stains
- GFAP, Olig2, S100, vimentin
- Synaptophysin (of variable extent, in > 50%) (Am J Surg Pathol 2010;34:1783)
- Ki67: variable (2 - 20%) (Neurosurgery 2003;53:544)
Negative stains
Electron microscopy description
- Bipolar tumor cells with elongated thin processes extending to rest upon the basal lamina of blood vessels
- Abundant intermediate (glial) filaments can be seen in some cells
- Apical surfaces may show microvilli, blebs and occasional cilia
- Vesicles and coated pits, as well as dense core granules and synaptoid complexes may be seen (Adesina: Atlas of Pediatric Brain Tumors, 2010)
Electron microscopy images
Molecular / cytogenetics description
- Similar genetic alterations as in pilocytic astrocytomas (J Neuropathol Exp Neurol 2013;72:2, Neuropathol Appl Neurobiol 2013;39:693)
- Most common alteration is the BRAF duplication / fusion resulting in activation of the MAPK pathway (Brain Tumor Pathol 2019;36:52, Annu Rev Pathol 2013;8:361)
- KIAA1549-BRAF fusion in half of cases by FISH (J Neuropathol Exp Neurol 2013;72:2, Neuropathol Appl Neurobiol 2013;39:693)
- The majority show no genetic susceptibility; rare cases occur in the context of neurofibromatosis type 1 and Noonan syndrome (Pediatr Blood Cancer 2006;46:377, Pediatr Blood Cancer 2015;62:1084)
Sample pathology report
- Brain, suprasellar region, biopsy:
- Pilomyxoid astrocytoma
- Ancillary tests:
- Strong positive GFAP staining
- Focally positive for synaptophysin
- Ki67 proliferation index: 3%
Differential diagnosis
- Pilocytic astrocytoma:
- Biphasic pattern, Rosenthal fibers, more often cystic, myxoid areas and angiocentric pattern only focal
- Ependymoma:
- More cellular and less myxoid, true rosettes, well developed perivascular pseudorosettes
- Olig2-, synaptophysin-
- Angiocentric glioma:
- Corticocentric, minimal or no myxoid background
- EMA+
Board review style question #1
A 10 month old boy presents with a solid enhancing hypothalamic mass on MRI. Biopsy shows a highly myxoid tumor with perivascular arrangement of monomorphous cells. What is the most likely genetic alteration in this tumor?
- BRAF duplication / fusion
- H3F3A K27M mutation
- IDH1 and IDH2 mutations
- SMARCB1 / INI1 mutations
Board review style answer #1
A. BRAF duplication / fusion. The histology shows pilomyxoid astrocytoma. BRAF duplication / fusion is a frequent event in this tumor. IDH1 / 2 mutations are frequent in diffusely infiltrating gliomas. SMARCB1 / INI1 mutations are the hallmark of atypical teratoid / rhabdoid tumor. H3F3A K27M mutation is associated with diffuse midline gliomas, H3 K27M mutant.
Comment Here
Reference: Pilomyxoid astrocytoma
Comment Here
Reference: Pilomyxoid astrocytoma
Board review style question #2
A 13 month old infant presented with failure to thrive. MRI showed a suprasellar enhancing mass. Intraoperative frozen section showed monomorphous bipolar tumor cells in an abundant myxoid background. Which of the following statements describes this tumor?
- Has a favorable prognosis with no reported risk of recurrence
- Preferentially located in the cerebellum with rare cases involving other sites
- Shares common genetic alterations with pilocytic astrocytoma
- Tends to affect adults
Board review style answer #2
C. Shares common genetic alterations with pilocytic astrocytoma. Pilomyxoid astrocytoma is considered a variant of pilocytic astrocytoma. They may be part of a single disease spectrum. They share common genetic alterations (BRAF duplication / fusion), some pilomyxoid astrocytomas mature into classic pilocytic astrocytomas over time and intermediate forms exist. Pilomyxoid astrocytomas tend to affect young children and are preferentially located in the hypothalamic / chiasmatic region. They are well known to exhibit a more aggressive behavior compared to pilocytic astrocytoma.
Comment Here
Reference: Pilomyxoid astrocytoma
Comment Here
Reference: Pilomyxoid astrocytoma