Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Challa B, Yearsley MM. Cytomegalovirus (CMV). PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/coloncmv.html. Accessed April 25th, 2024.
Definition / general
- Cytomegalovirus (CMV) is a double stranded DNA virus and a member of human herpes virus family
- Also known as herpes virus type 5
- 3 patterns of CMV infection:
- Latent infection
- Most common, immunocompetent patients
- Mononucleosis-like syndrome
- Immunocompetent patients
- Tissue invasive disease
- Immunocompromised patients
- Latent infection
- Tissue invasive disease
- Gastrointestinal tract is most commonly involved (30% of tissue invasive cases) (Virol J 2008;5:47)
Essential features
- Double stranded DNA virus and a member of human herpes virus family
- Tissue invasive disease, usually seen in immunocompromised patients
- Most common sites of infection in gastrointestinal tract:
- Colon
- Esophagus
- Symptoms:
- Rectal bleeding (most common)
- Diarrhea
- Abdominal pain
- Fever
- Weight loss
- Microscopy:
- Cytomegalic cells with owl's eye intranuclear viral inclusions
- CMV immunohistochemistry is the gold standard for diagnosis
Terminology
- CMV infection
- CMV antigens or antibodies in blood
- CMV disease
- Clinical symptoms and end organ damage
- CMV colitis
- Identification of characteristic intranuclear / intracytoplasmic inclusions on H&E sections
- Identification of CMV specific antigens by immunohistochemistry (IHC) and clinical symptoms
ICD coding
- ICD-10: B25.8 - other cytomegaloviral diseases
Epidemiology
- Affects 50 - 100% humans worldwide depending on age and race of the population tested
- Infects over half of adults by age 40 (CDC: About Cytomegalovirus (CMV) [Accessed 11 November 2021])
- CMV seroprevalence in the United States is 42 - 93% (Am J Kidney Dis 1991;17:719)
- Immunocompetent patients
- Mean age is 64 - 75 years (Clin Microbiol Infect 2015;21:1121.e1)
- Liver transplant patients
- Cumulative incidence is 4.9% (Transplant Proc 2014;46:832)
- Allogenic hematopoietic stem cell transplant patients
- Incidence is 15 - 25% (Biol Blood Marrow Transplant 2015;21:159)
- Inflammatory bowel disease
- Incidence is 1.5 - 4.5%
- Ulcerative colitis > Crohn’s disease (Eur J Gastroenterol Hepatol 2016;28:1329)
Sites
- Can involve any part of the gastrointestinal tract
- Most common sites:
- Colon
- Esophagus
Pathophysiology
- Spread by saliva, urine, respiratory droplets, sexual contact, breast milk and blood transfusions (Clin Microbiol Rev 1989;2:204, Nihon Rinsho 1998;56:179)
- After initial infection, CMV resides latently in monocytes, fibroblasts, myeloid cells and endothelial cells
- Tissue invasive disease in colon can lead to ulcerative changes, erosion into blood vessels (causing bloody diarrhea), inflammatory polyps, severe inflammation and vasculitis leading to ischemia and transmural necrosis
Etiology
- Cytomegalovirus (CMV)
- Most commonly in immunocompromised patients
- History of AIDS, organ transplantation, hematologic malignancy, cancer therapy and corticosteroid therapy
- Risk factors in immunocompetent patients:
- Renal disease
- Hemodialysis
- Neurological disease
- Rheumatic disease
- Exposure to antibiotics
- Antacids
- Corticosteroid
- Red blood cell transfusion within 1 month of diagnosis of colitis (Clin Infect Dis 2015;60:e20)
- Severe ulcerative colitis (patients treated with high dose corticosteroids)
Clinical features
- Rectal bleeding (most common)
- Diarrhea, abdominal pain, fever, weight loss (StatPearls: Cytomegalovirus Colitis [Accessed 12 November 2021])
Diagnosis
- Surgical resection specimen or biopsy: histopathologic diagnosis
- Clinical symptoms, endoscopic findings, serologic testing, polymerase chain reaction (PCR) and culture
Laboratory
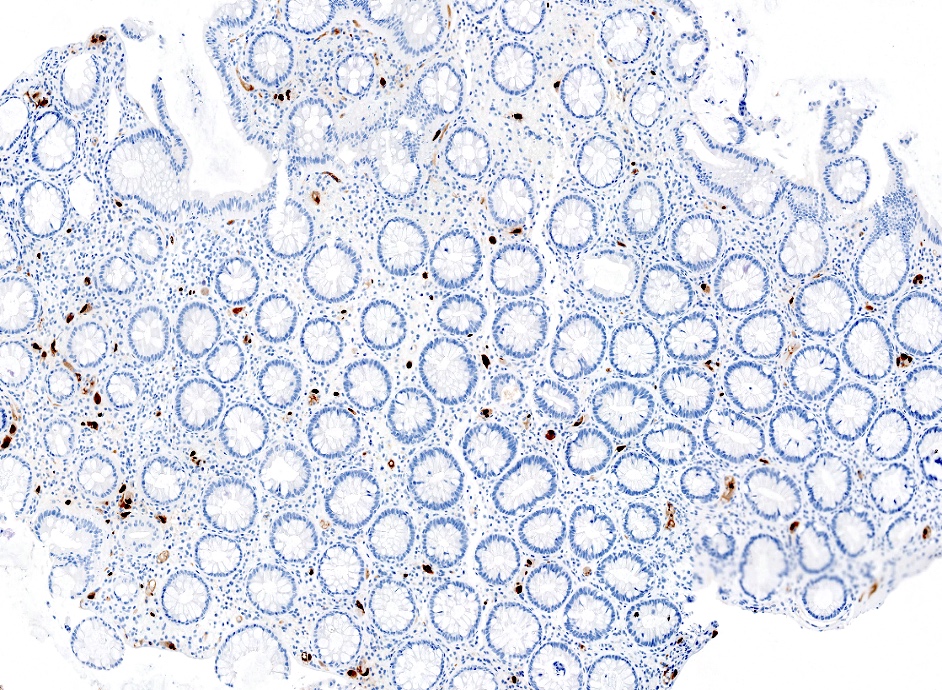
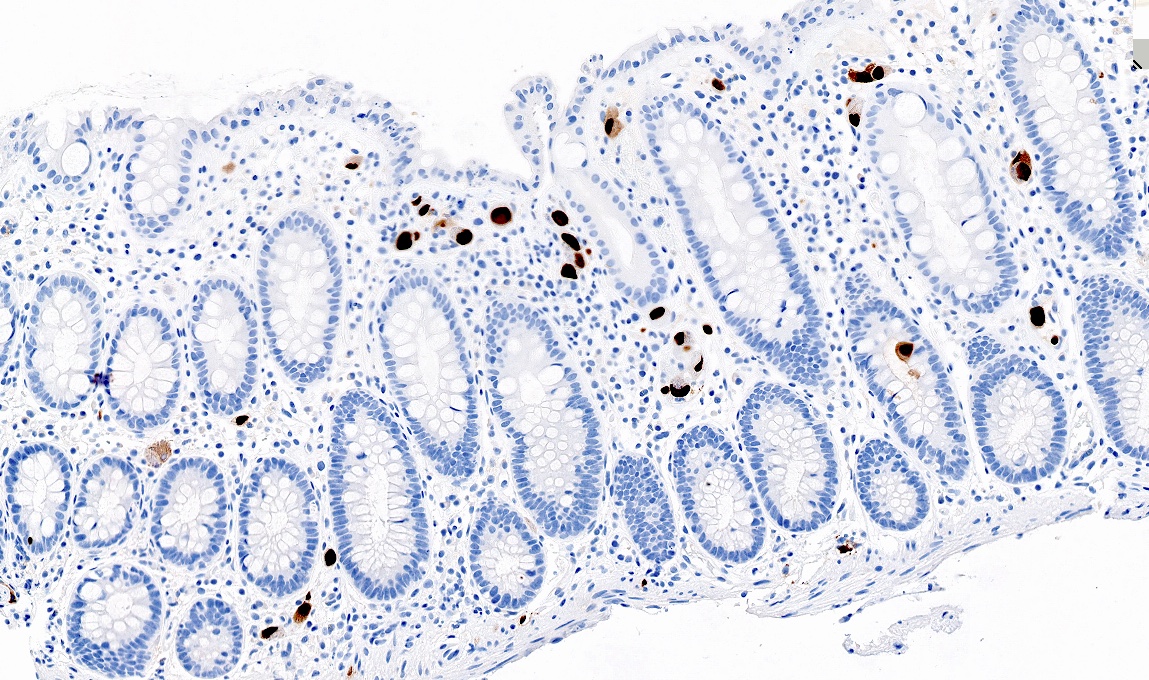
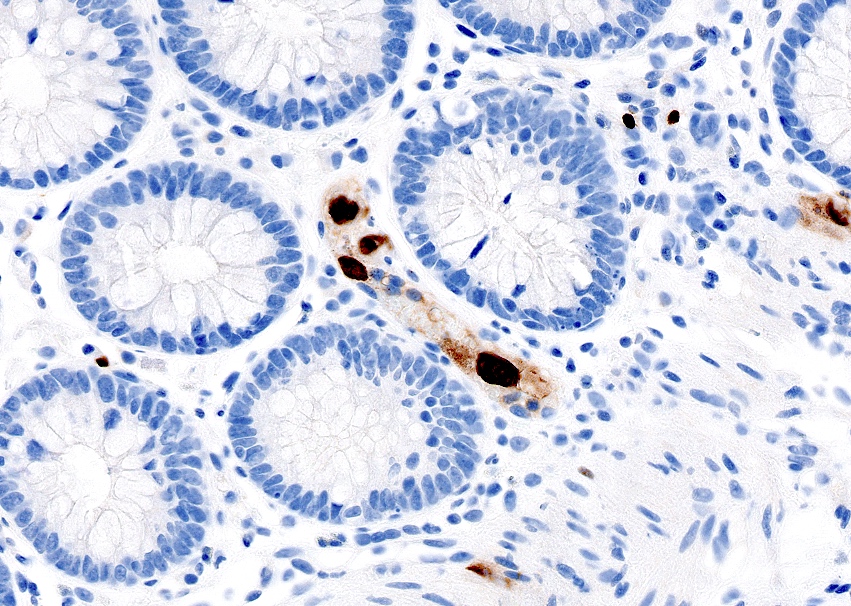
- Histology:
- Gold standard test
- Immunohistochemistry (IHC) for CMV
- Greater sensitivity than hematoxylin & eosin (H&E)
- H&E can detect CMV infected cells
- Cells larger than normal, containing intranuclear or intracytoplasmic inclusions
- CMV infected cells can be confirmed by IHC staining
- Immunohistochemistry (IHC) for CMV
- Gold standard test
- Serology:
- Acute infection
- CMV IgM antibodies
- 4 times increase in titer of CMV IgG specific antibodies 2 - 4 weeks apart
- CMV antigenemia
- Predictor of clinical outcomes
- Less sensitive for diagnosis of CMV colitis
- Real time polymerase chain reaction (PCR) / CMV DNA quantification
- Positive in only 50% of patients with biopsy proven CMV colitis / enteritis
- CMV culture
- High sensitivity and specificity for diagnosis of CMV colitis
- Takes longer to obtain results (1 - 3 weeks)
- May delay diagnosis and timely treatment (J Clin Microbiol 1993;31:2851)
- Acute infection
Radiology description
- Computed tomography:
- Nonspecific findings
- Bowel wall thickening
- Mural edema
- Pericolonic fat stranding
- Free fluid, free air
- Lymphadenopathy (Radiology 1985;155:585)
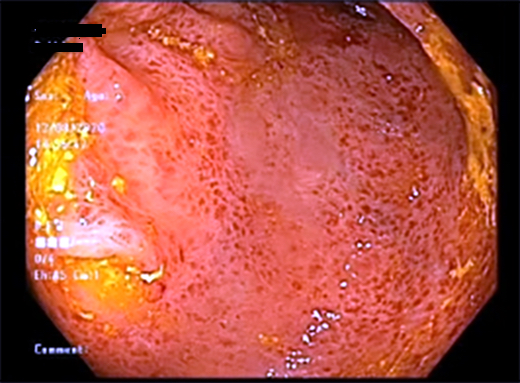
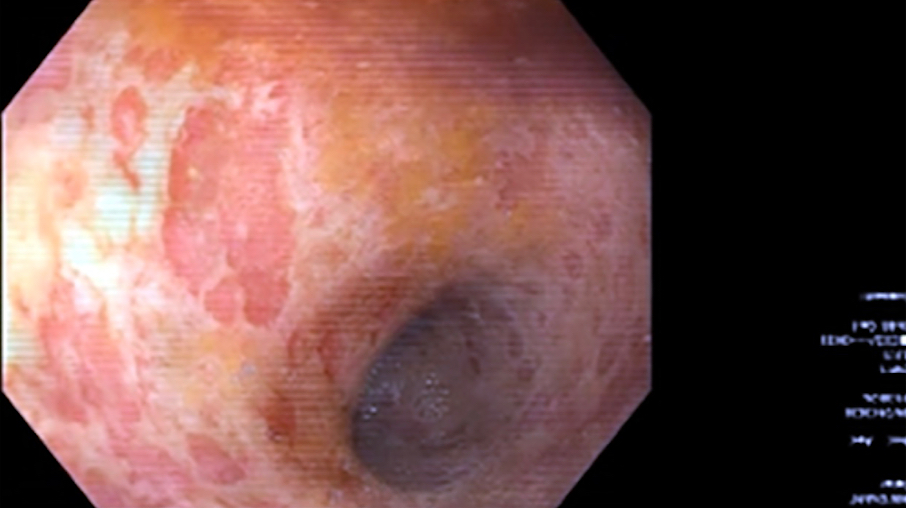
- Endoscopic findings:
- Easy bleeding, loss of vascular pattern, mucosal edema, erythema, mucinous exudate and wide mucosal defect
- Mucosal defects, punched out ulcers (most common), longitudinal ulcers, irregular ulceration or cobblestone appearance (Emerg Radiol 2020;27:277)
Prognostic factors
- Excellent overall prognosis
- Factors associated with poor prognosis and higher mortality (immunocompetent patients)
- M > F
- Age > 55 years
- Patients requiring surgery
- CMV colitis reactivation with ulcerative colitis, tends to have poorer prognosis
- Timely diagnosis and treatment greatly improves clinical outcomes (StatPearls: Cytomegalovirus Colitis [Accessed 12 November 2021])
Case reports
- 42 year old HIV+ man with progressive abdominal pain, palpable right umbilical mass, fever, asthenia and weight loss (Radiol Case Rep 2018;14:273)
- 48 year old woman with severe abdominal pain and constipation (World J Clin Cases 2021;9:5631)
- 60 year old man with history of sarcoidosis and chronic kidney disease with lower abdominal pain and diarrhea (Indian J Nephrol 2021;31:73)
- 71 year old man with history of posttuberculous aspergilloma admitted to ICU with acute respiratory distress syndrome (Clin Case Rep 2020;9:e03600)
Treatment
- Intravenous (IV) ganciclovir (5 mg/kg twice daily)
- After 3 - 5 days of IV ganciclovir, oral valganciclovir (900 mg, twice daily) (Clin Gastroenterol Hepatol 2015;13:949)
- Foscarnet in ganciclovir resistant or tolerant cases
Clinical images
Gross description
- Nonspecific findings
- Inflamed mucosa, hyperemia, mucosal sloughing
- Punched out ulcers, aphthous ulcers, exudate
- Pseudomembrane formation (Arch Pathol Lab Med 2016;140:854)
Gross images
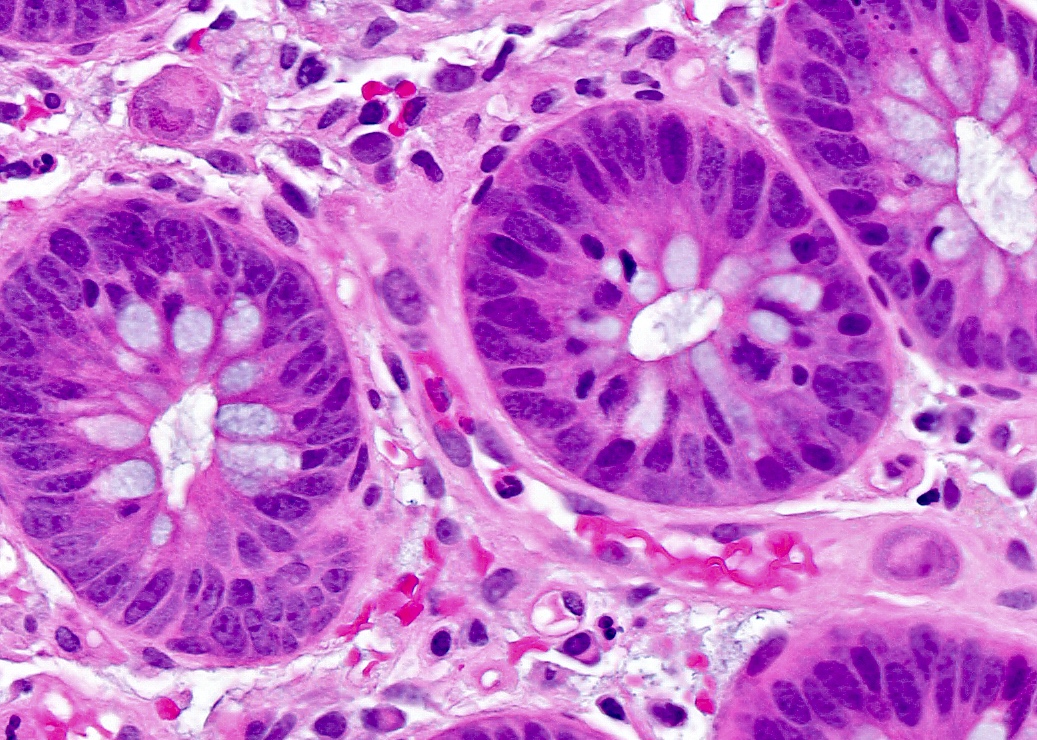
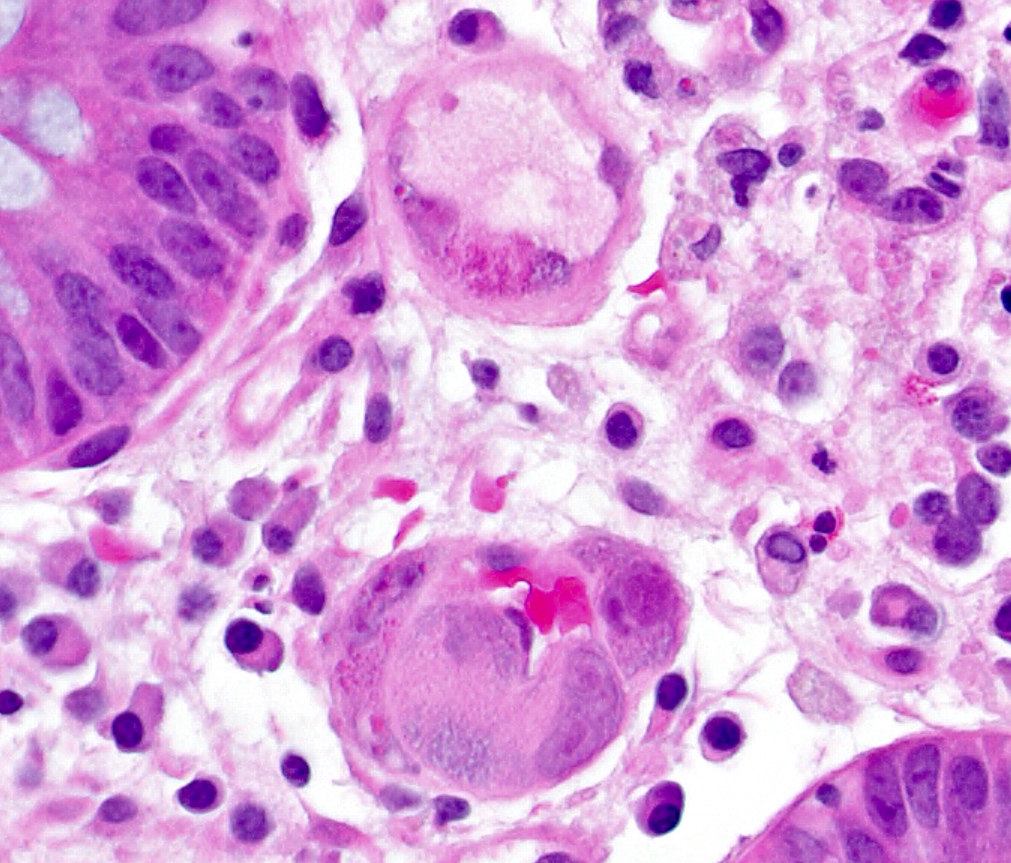
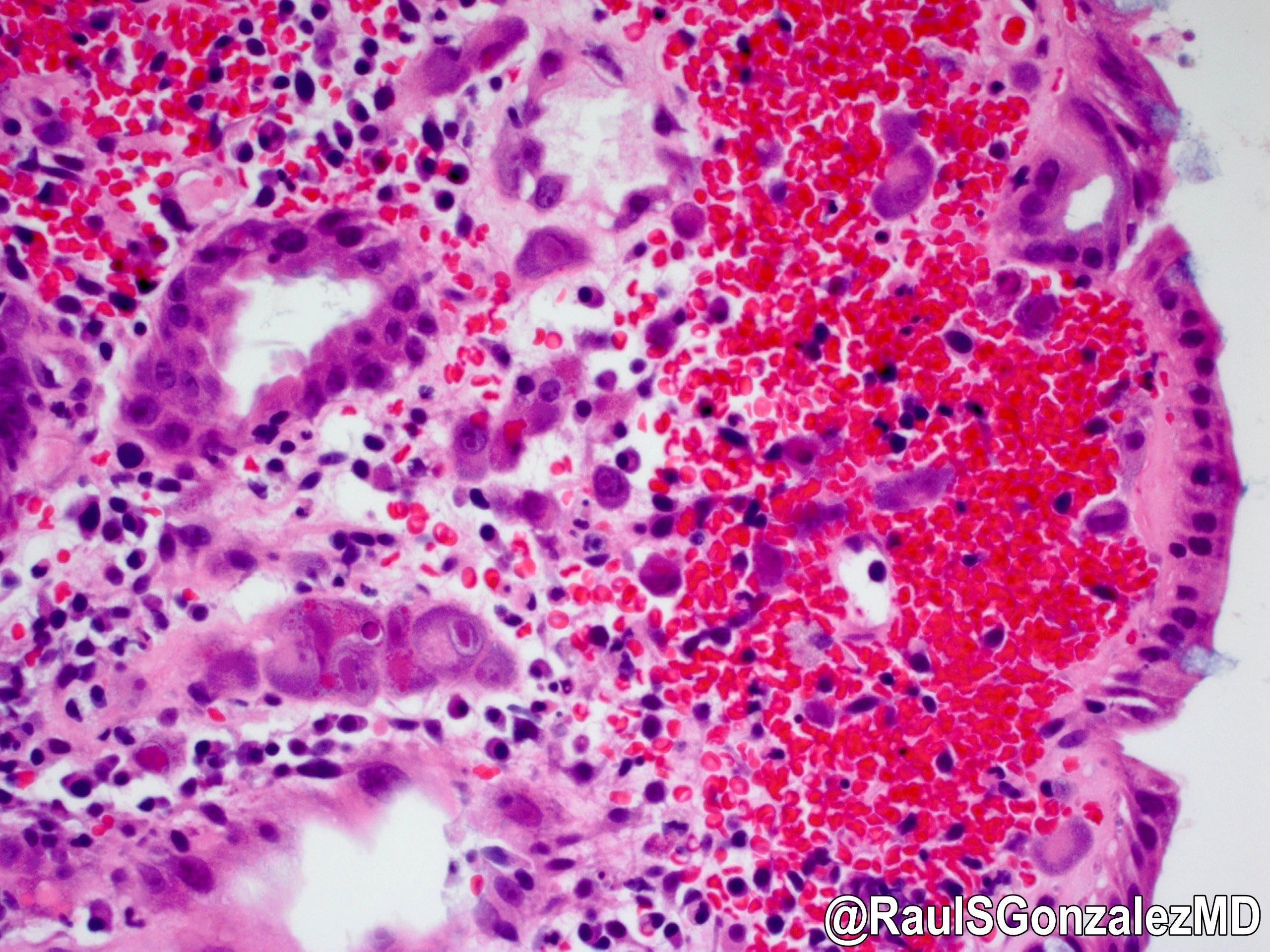
Microscopic (histologic) description
- Most commonly affected cells:
- Endothelial cells
- Mesenchymal cells
- Macrophages
- Larger (cytomegalic) cells:
- Usually 25 - 35 micrometers
- Typically 2 - 4 times larger than normal
- Owl’s eye:
- Large ovoid or pleomorphic nucleus with basophilic intranuclear inclusions (Cowdry bodies) surrounded by a clear halo (Arch Pathol Lab Med 2016;140:854)
- Thickened nuclear membrane
- Coarse red intracytoplasmic granules (Int Med Case Rep J 2011;4:55)
- Increased apoptotic bodies
- Expansion of lamina propria by mixed inflammatory plasma cell rich infiltrate
- Neutrophilic inflammation
- Should raise suspicion for CMV infection in graft versus host disease and mycophenolate injury (Int J Surg Pathol 2018;26:347, J Clin Pathol 2013;66:8)
- Deep fissuring ulcers, cryptitis, crypt abscess, architectural distortion and pseudopolyp formation
- May mimic inflammatory bowel disease (Am Surg 2007;73:58)
- Submucosal vasculitis and thrombosis of microvessels
Microscopic (histologic) images
Positive stains
- Immunohistochemistry for CMV
Negative stains
- Immunohistochemistry for adenovirus, HSV1, HSV2
Molecular / cytogenetics description
- Real time DNA PCR amplification method:
- Rapid results, high negative predictive value
- Contradictory reports regarding sensitivity
- CMV DNA load > 250 copies/mg tissue may predict resistance to steroid treatment in ulcerative colitis (Am J Gastroenterol 2011;106:2001)
Videos
CMV colitis in ulcerative colitis and immunocompromised states
Sample pathology report
- Colon, random, biopsy:
- CMV colitis
- Immunohistochemical stain for CMV is positive
- Colon, colectomy:
- CMV colitis in the background of severely active ulcerative pancolitis
- Immunohistochemical stain for CMV is positive
- Negative for dysplasia
Differential diagnosis
- Infectious colitis:
- Adenovirus:
- Commonly infects surface epithelial cells
- Homogenous glassy amphophilic nuclear inclusions
- HSV1, HSV2:
- Chromatin margination, multinucleation, nuclear molding
- Adenovirus:
- Graft versus host disease:
- Crypt apoptosis
- Crypt dropout
- Ulceration
- No cytomegalic inclusions
- May coexist with CMV infection
- Inflammatory bowel disease:
- No inclusions
- Ulcerative colitis, Crohn's disease
- Mycophenolate mofetyl induced colitis:
- No inclusions
- Increased apoptosis
- Increased lamina propria eosinophils
Additional references
Board review style question #1
A 71 year old man presents with abdominal pain and diarrhea. Colonoscopy showed diffuse mucosal erythema and irregular ulcerations. The patient undergoes biopsy of the lesion. What is the infected cell and organism causing the histopathologic findings?
- Endothelial cell, adenovirus
- Endothelial cell, cytomegalovirus
- Epithelial cell, adenovirus
- Epithelial cell, cytomegalovirus
Board review style answer #1
B. Endothelial cell, cytomegalovirus. The images show cytomegalic endothelial cells with inclusions. Adenovirus typically affects epithelial cells and shows amphophilic nuclear inclusions.
Comment Here
Reference: Cytomegalovirus (CMV)
Comment Here
Reference: Cytomegalovirus (CMV)
Board review style question #2
What is the gold standard method for diagnosing CMV colitis?
- CMV culture
- CMV DNA polymerase chain reaction (PCR) amplification method
- CMV serology
- Immunohistochemistry for CMV
Board review style answer #2