Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Molecular / cytogenetics description | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1Cite this page: Dunn ALJ, Gonzalez RS. Tubular adenoma. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/colontumortubularadenoma.html. Accessed September 16th, 2025.
Definition / general
- Neoplastic colon polyp with at least low grade dysplasia
- Precursor to invasive adenocarcinoma
Essential features
- Dysplastic nuclei (elongated and hyperchromatic pseudostratification)
- < 25% villous component
Terminology
- The word adenoma should not be used on its own, to avoid confusion with sessile serrated adenoma and traditional serrated adenoma
- > 25% villous component indicates tubulovillous adenoma or villous adenoma
Epidemiology
- Incidence increases with age; commonly encountered in patients over 50
- Estimated that 25% of men and 15% of women undergoing colonoscopy are found to have at least 1 adenoma (N Engl J Med 2006;355:2551)
- Men more commonly affected than women (Gastrointest Endosc 2011;74:135)
Sites
- Found more commonly in the left colon and rectum compared with other polyps
Pathophysiology
- Has a well documented adenoma to carcinoma sequence that involves mutations in KRAS, TP53, APC and beta catenin (Cell 1990;61:759)
- Activation of KRAS leads to downstream signaling that influences survival, antiapoptosis and proliferation, though this event is typically seen in advanced rather than early adenomas (J Gastroenterol Hepatol 2012;27:1423, PLoS One 2017 27;12)
- Wnt pathway: activation of Wnt pathway leads to beta catenin accumulation in the nucleus and subsequent transcription and cell proliferation
- Mutations include loss of function of APC or beta catenin mutations that resist degradation by APC (J Gastroenterol Hepatol 2012;27:1423)
Etiology
- Decreased risk of conventional colorectal adenomas is associated with
- Increased dietary fiber intake (Lancet 2003;361:1491)
- Fruit consumption in women (Cancer Res 2006;66:3942)
- Folate intake (J Nutr 2005;135:2468)
Clinical features
- < 1 cm: usually asymptomatic and detected by screening colonoscopy
- > 1 cm: may bleed, lead to iron deficiency anemia, obstruction; increased risk of progressing to carcinoma
- Mostly left sided in spontaneous polyps and in familial adenomatous polyposis; right sided in Lynch syndrome (Gut 2002;50:382)
Diagnosis
- Diagnosis is made by histologic confirmation
Case reports
- 36 year old woman with intussusception due to adenoma (Asian J Endosc Surg 2013;6:311)
- 52 year old man with tubular adenoma with coexisting multifocal MALT lymphoma (Int J Colorectal Dis 2011;26:1221)
- 53 year old man with infectious endocarditis from E. faecalis associated with tubular adenoma (Case Rep Infect Dis 2017;2017:3095031)
- 64 year old woman with signet ring cell carcinoma metastasizing to a tubular adenoma (Arch Pathol Lab Med 2003;127:1509)
- 85 year old woman with osseous metaplasia in adenoma (J Clin Pathol 2005;58:220)
Treatment
- Colonoscopy is diagnostic and potentially curative (via polypectomy)
- High grade dysplasia and large polyps may warrant endoscopic mucosal resection or partial colectomy
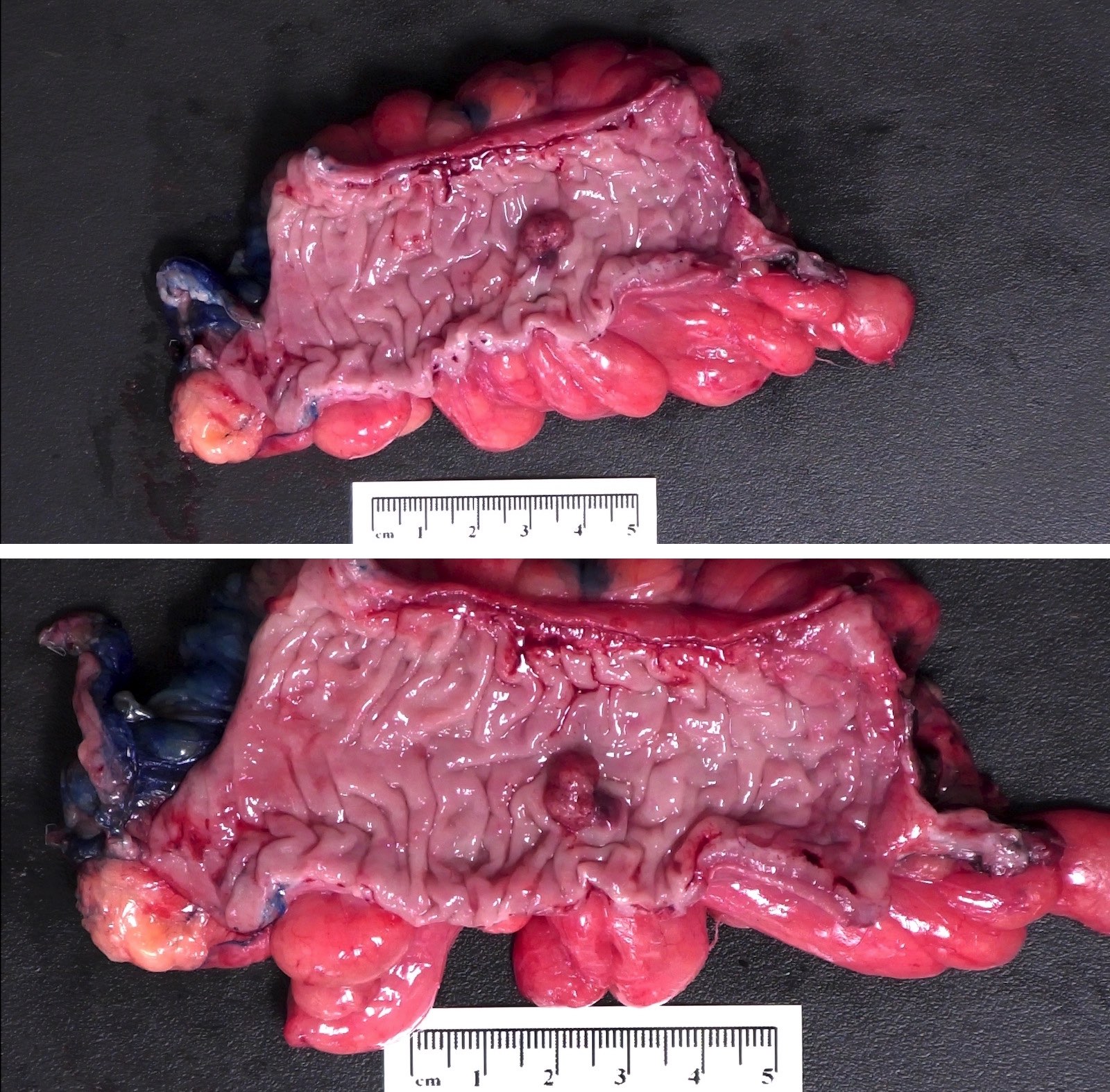
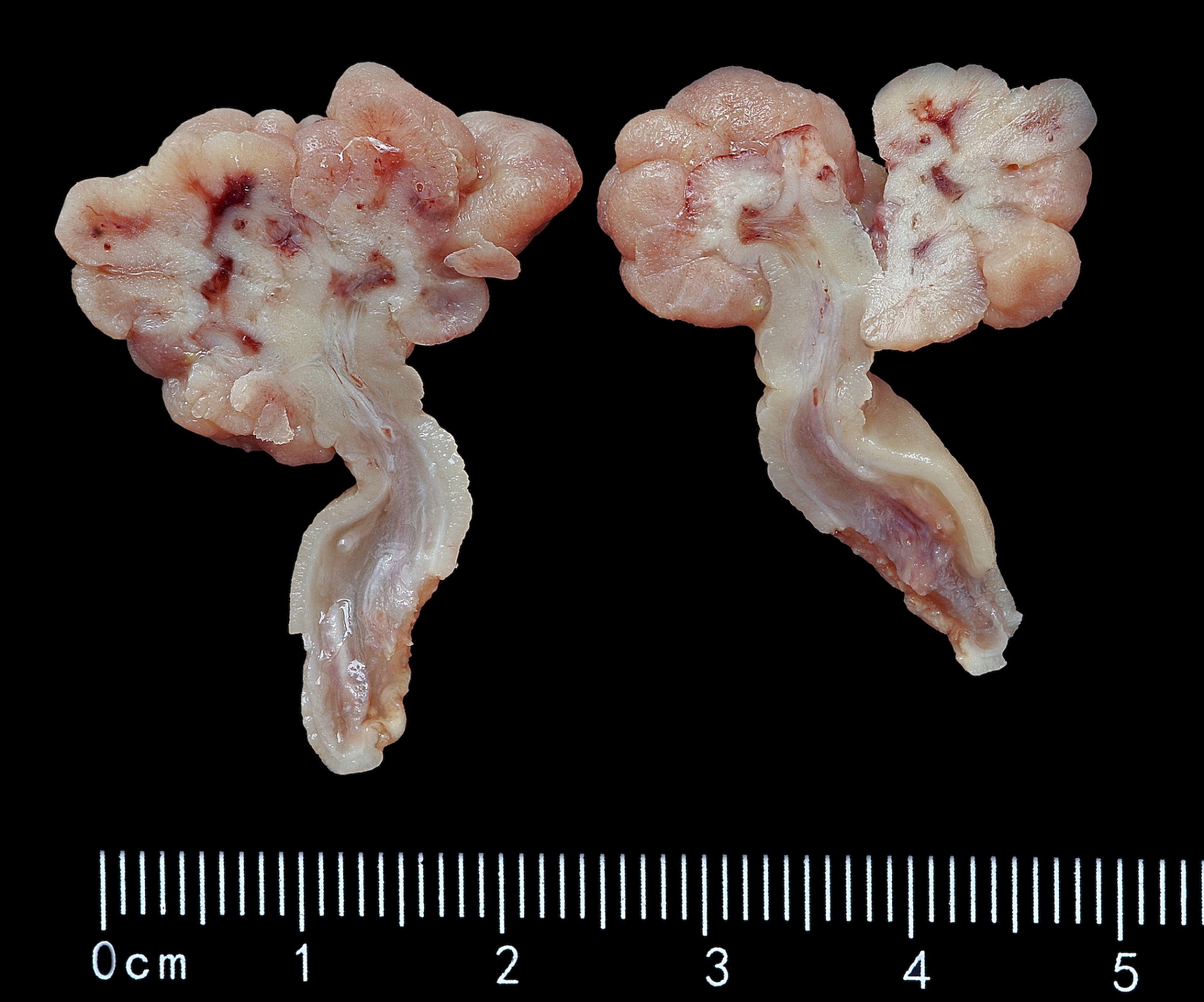
Gross description
- May be sessile or pedunculated
- Typically dark red compared with mucosa
- Features concerning for high grade dysplasia or malignancy include size > 1 cm, villous architecture and ulceration / friability
Gross images
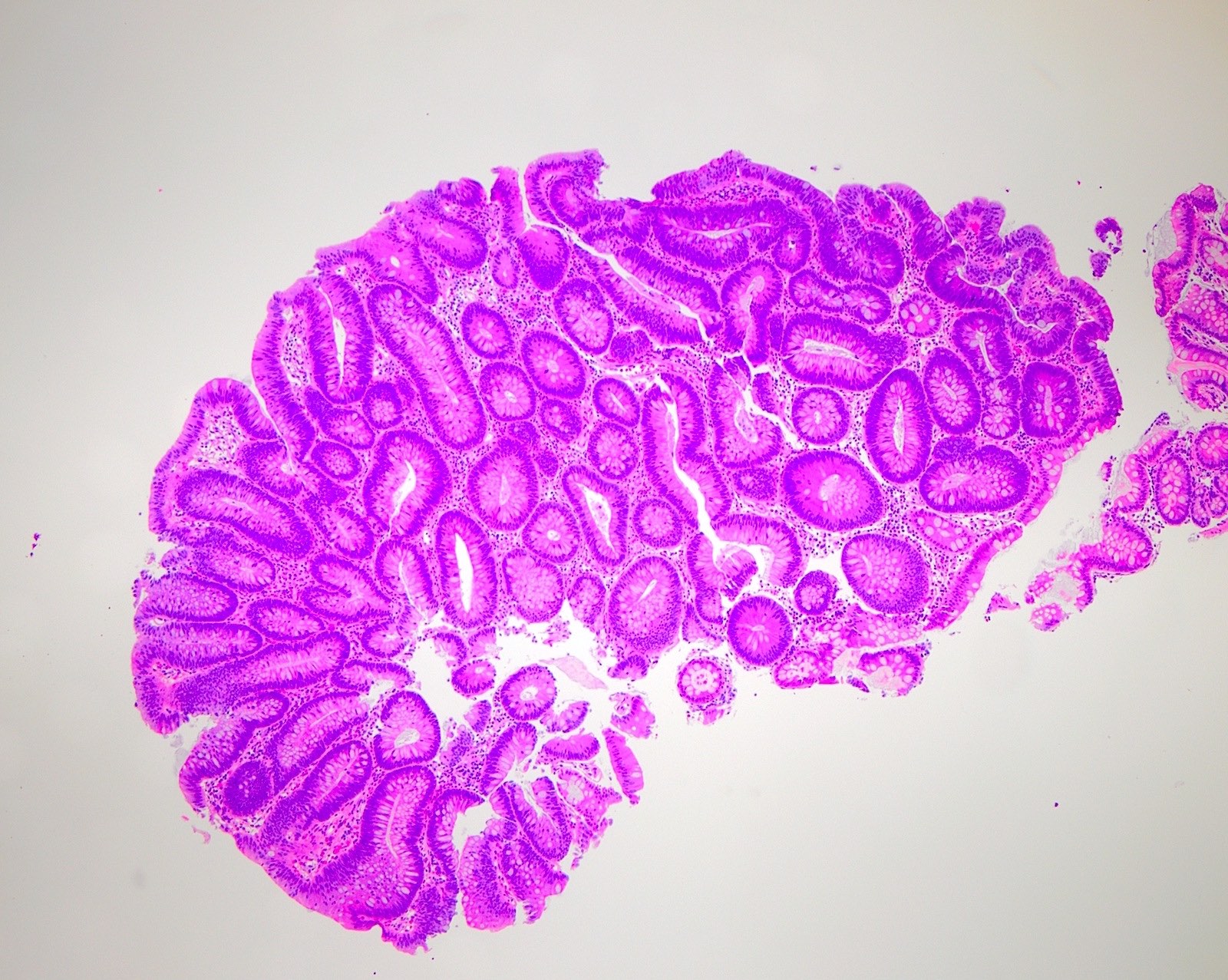
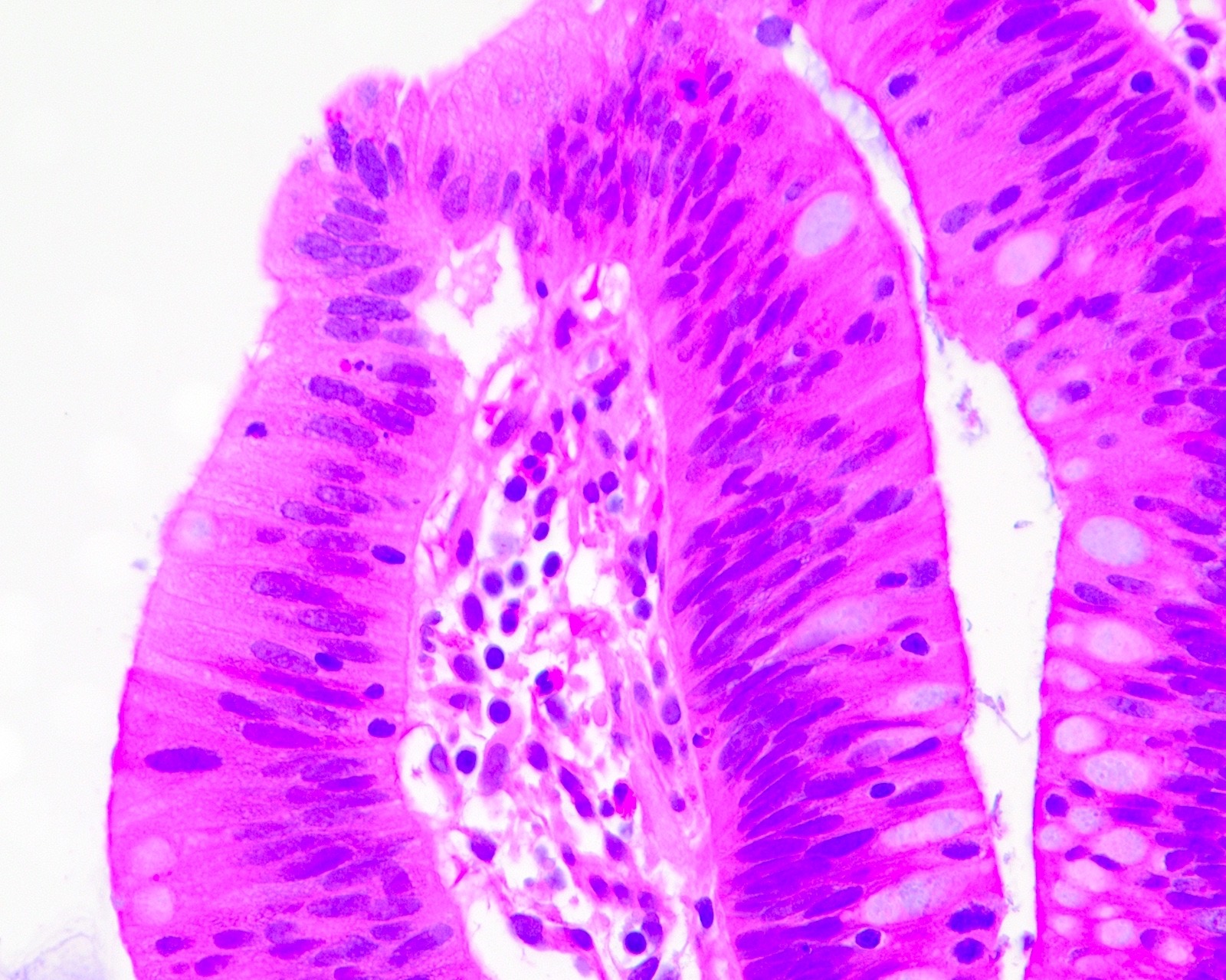
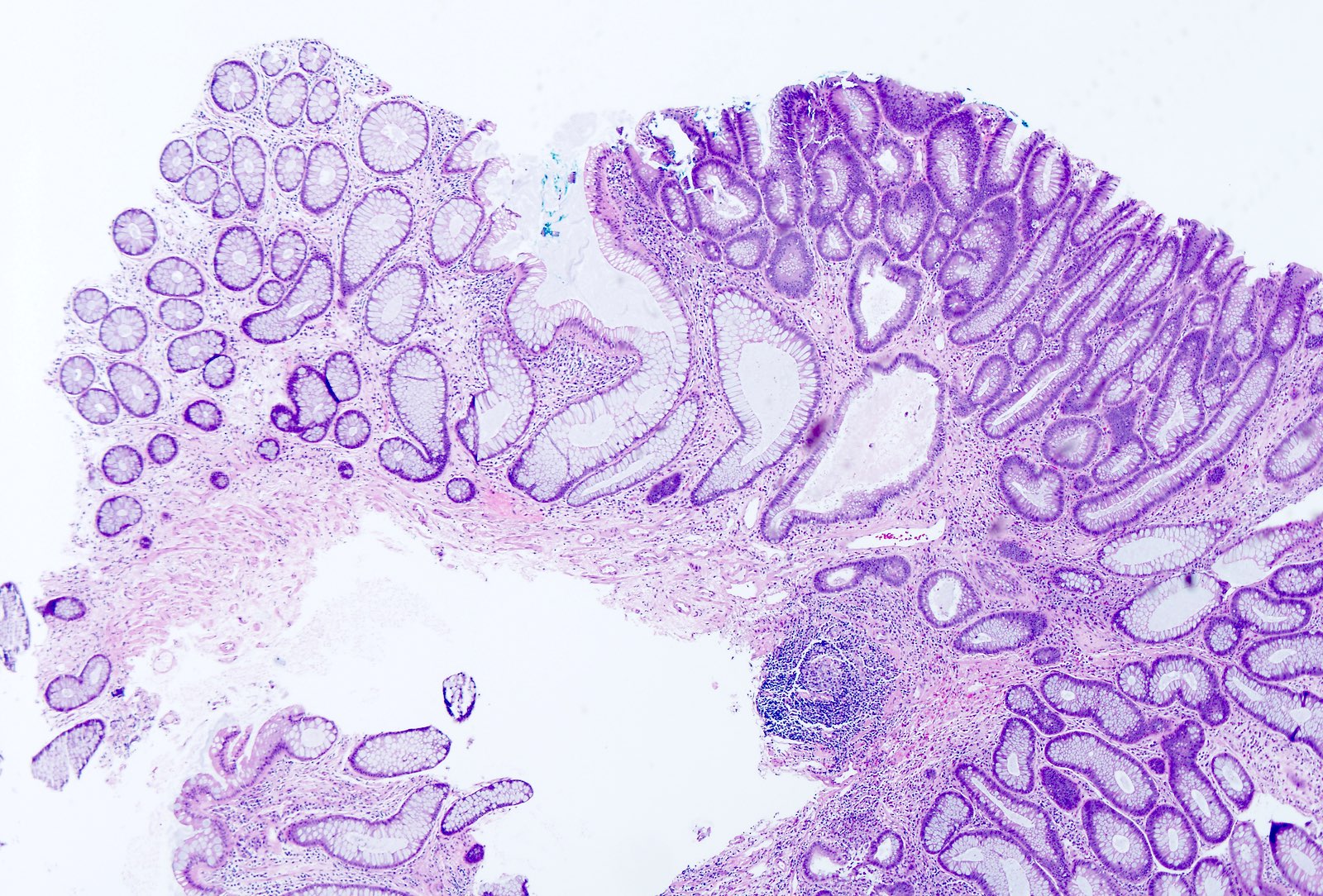
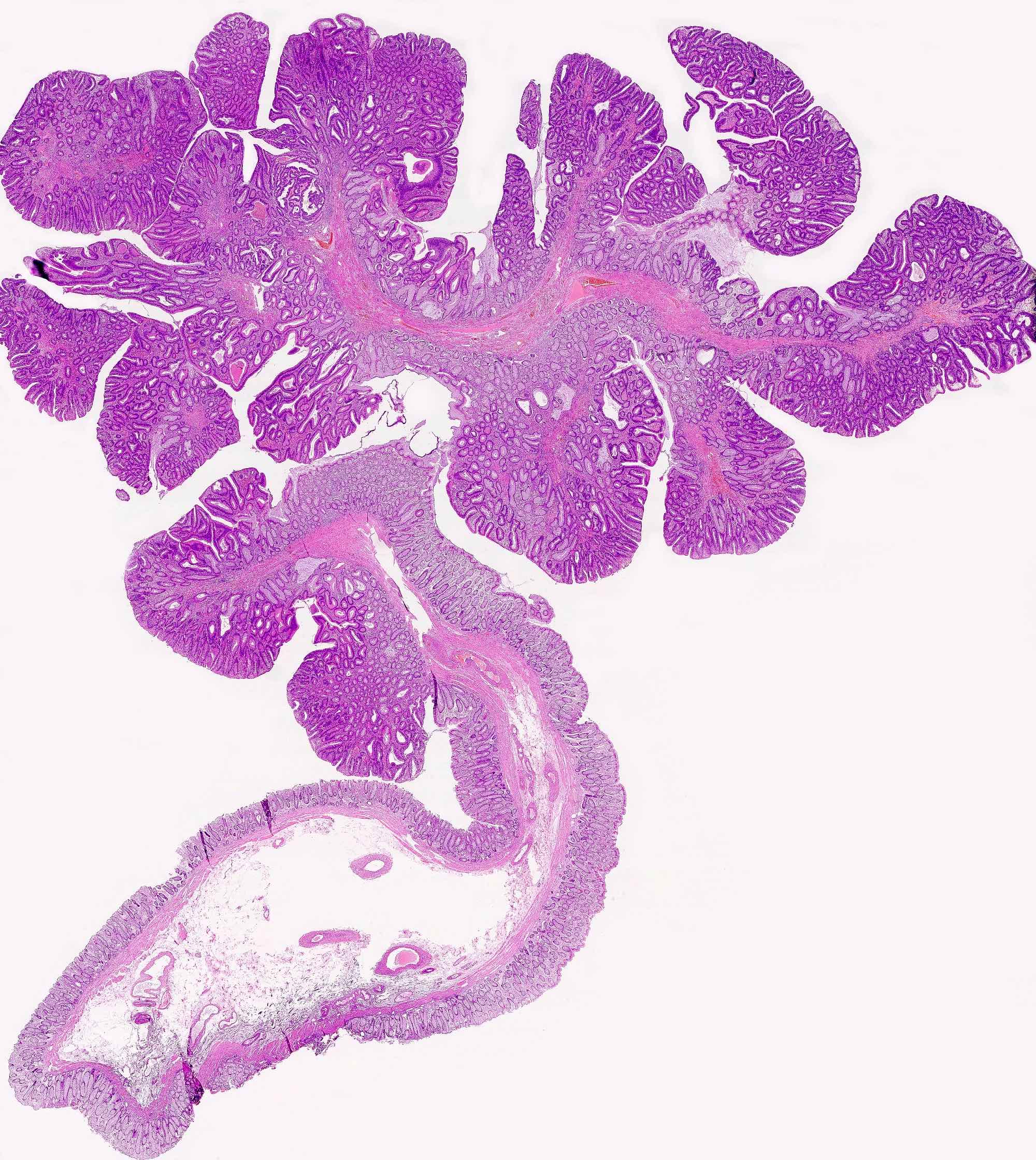
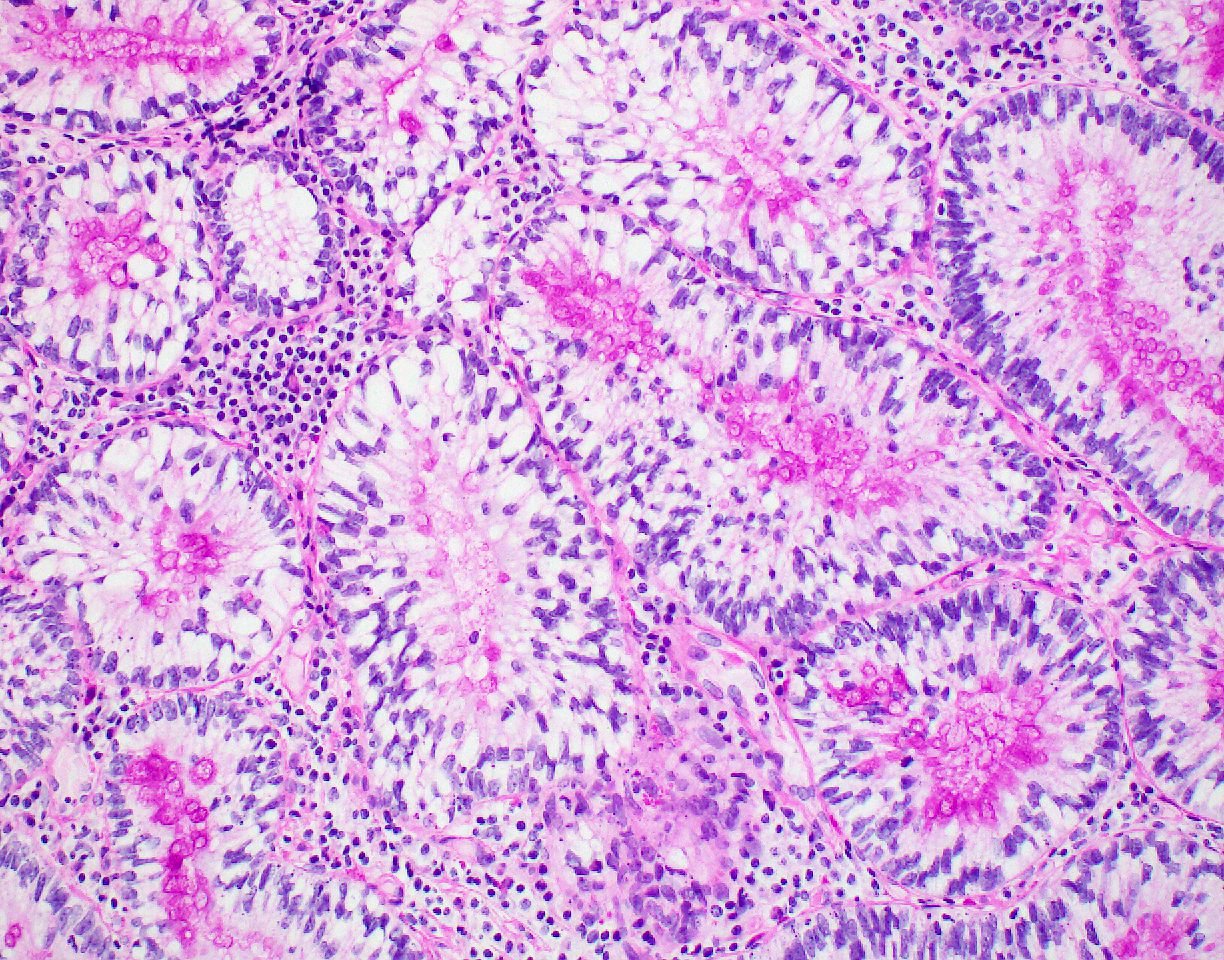
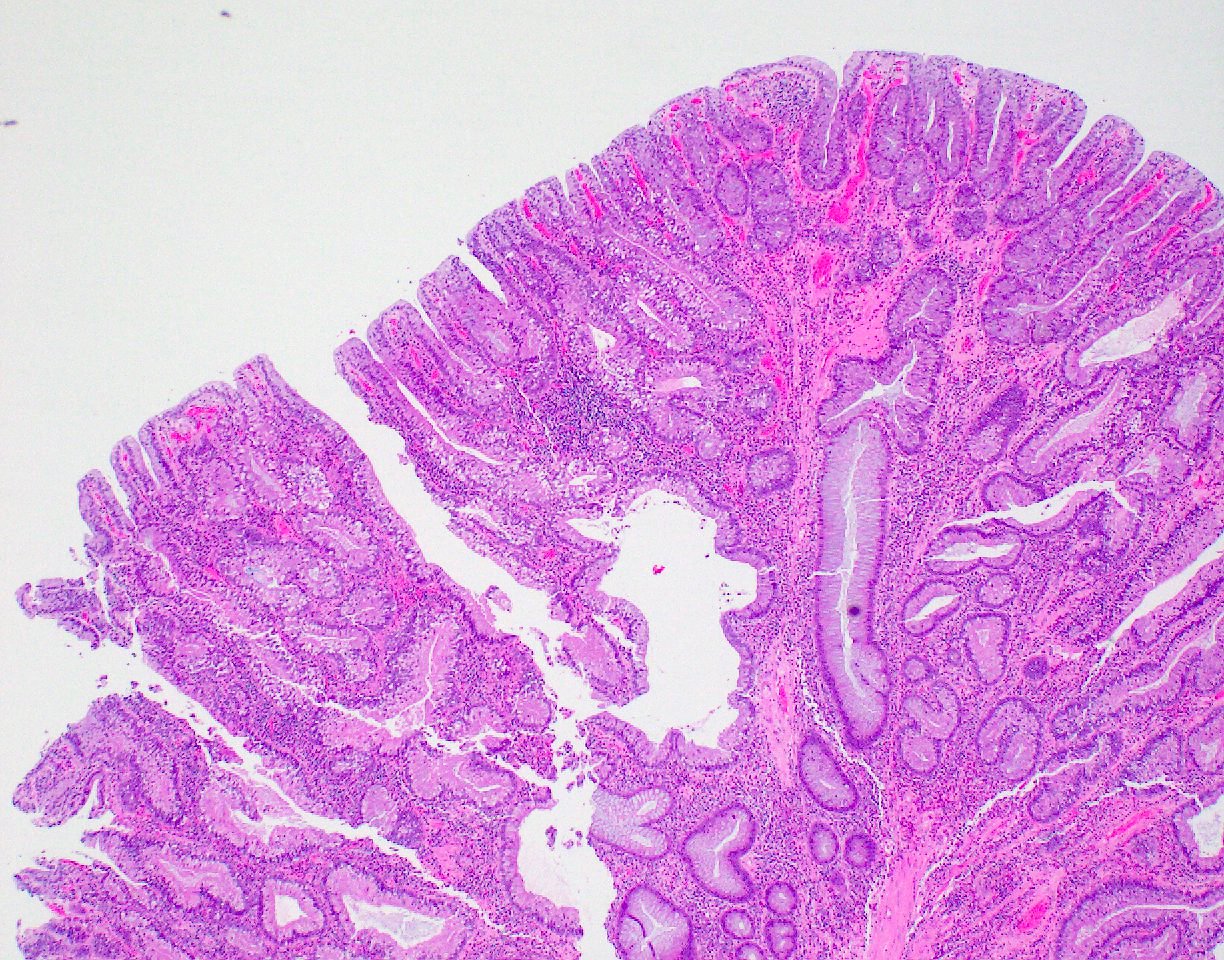
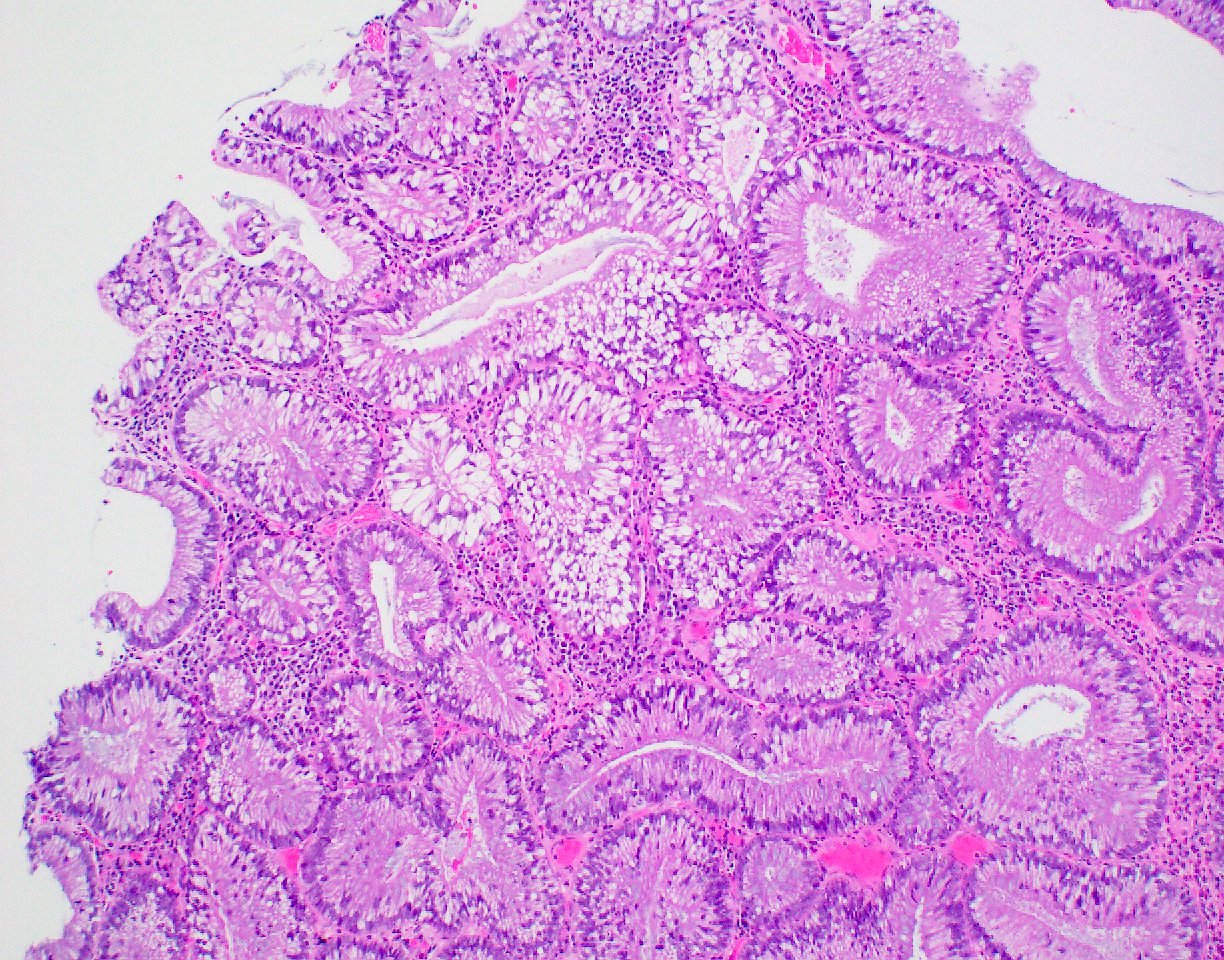
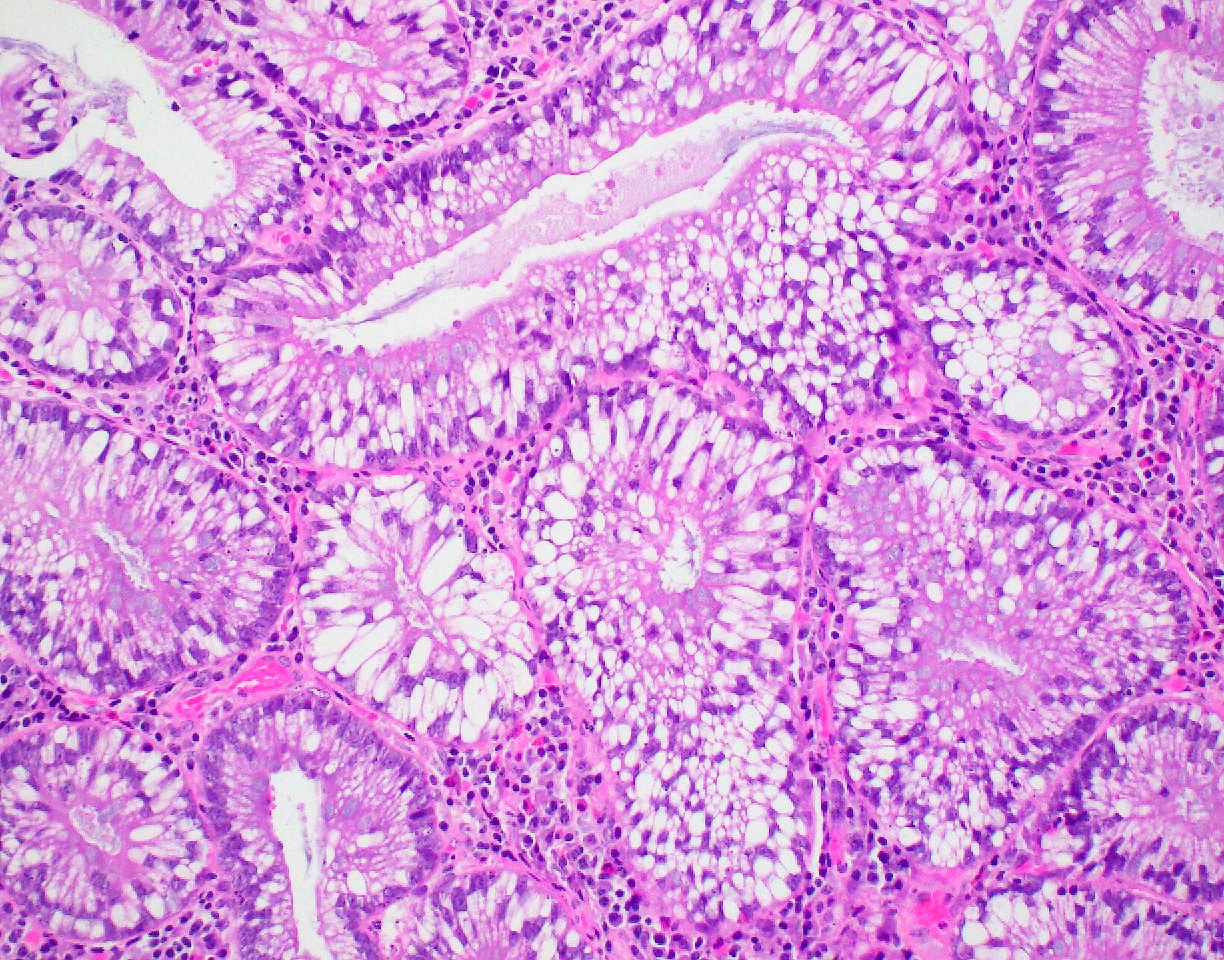
Microscopic (histologic) description
- Polypoid colonic mucosa covered with dysplastic epithelium comprised of hyperchromatic, elongated nuclei arranged in a pseudostratified manner
- Dysplasia is typically low grade but may also be high grade, with architectural (cribriforming, luminal necrosis) and cytologic changes (vesicular chromatin, nucleoli, loss of basal polarity)
- Abrupt transition from normal to dysplastic mucosa is commonly present
- Variable amounts of mucin loss
- Metaplasia may be present: osseous, squamous or Paneth cells (J Clin Pathol 2005;58:220, J Surg Oncol 1984;26:130)
- Pseudoinvasion can mimic progression to adenocarcinoma but displaced glands are benign and surrounded by lamina propria and often hemosiderin (Mod Pathol 2015;28:S88)
- May rarely show clear cell features (Am J Surg Pathol 2010;34:1344)
Microscopic (histologic) images
Contributed by Andrew L.J. Dunn, M.D. and Christopher Hartley, M.D.
Contributed by @Andrew_Fltv and @liverwei on Twitter
Images hosted on other servers:
Negative stains
- p53 (usually)
Molecular / cytogenetics description
- 33% are aneuploid
- Depending on the villous component, 2 types of tubular adenomas can be identified (Am J Surg Pathol 2011;35:212):
- TA1: less than 1% villous component, lower rate of p53 overexpression, KRAS mutation and MGMT loss
- TA2: 1 - 20% villous component, higher rate of TP53 and KRAS mutation and MGMT loss
- KRAS mutations may account for up to 60% of mutations in tubular adenomas (J Gastroenterol Hepatol 2012;27:1423)
Sample pathology report
- Colon, splenic flexure, polypectomy:
- Tubular adenoma
Differential diagnosis
- Inflammatory polyp:
- Nuclei can become elongated like a tubular adenoma but nuclei are typically vesicular with round borders
- Tubulovillous adenoma, villous adenoma:
- Surface architecture has > 25% villous component
Additional references
Practice question #1
Which of the following gene mutations is implicated in a majority of tubular adenomas?
- ALK
- BAP1
- KRAS
- MDM2
Practice answer #1
C. KRAS mutations are implicated in up to 60% of adenomas and adenocarcinomas. BAP1 mutations are present in a subset of melanocytic tumors and mesotheliomas. MDM2 is amplified in liposarcoma and some of its variants. ALK mutations can be seen in inflammatory myofibroblastic tumor, anaplastic large cell lymphoma and a subset of lung adenocarcinomas.
Comment here
Reference: Tubular adenoma
Comment here
Reference: Tubular adenoma