Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Clinical images | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Virtual slides | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Dettrick A, Gupta R. Keloid. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/earkeloid.html. Accessed April 24th, 2024.
Definition / general
- Abnormal proliferation of scar tissue that extends beyond the boundaries of the initial injury and does not regress (Sci Rep 2021;11:9390)
- Forms at the site of cutaneous injury (often minor) (Sci Rep 2021;11:9390)
Essential features
- Excessive scar tissue that extends beyond the boundaries of the initial injury
- Very common in dark skinned people (Fitzpatrick skin types 4 - 6) (Cureus 2022;14:e23503)
- Recurrence after excision is common (Burns Trauma 2020;8:tkaa031)
- Characteristic broad, pink bands of collagen (keloidal collagen)
Terminology
- Keloid / keloid scar
- Keloid is Greek for crab claw
- Not to be confused with hypertrophic scar, which is confined to the limits of the injury (Exp Dermatol 2021;30:146)
Epidemiology
- Any age but most are in patients 10 - 30 years old (Front Cell Dev Biol 2020;8:360)
- 15 times more common in Asian, Hispanic and African populations (J Clin Aesthet Dermatol 2021;14:S24)
- Among keloids in the head and neck, 70% occur on the ear / earlobe (Facial Plast Surg Aesthet Med 2021;23:59)
- Common in young African women after ear piercing
- Unique to humans (Adv Wound Care (New Rochelle) 2019;8:77)
- First recorded in the Smith papyrus from Egypt around 1700 B.C. (Exp Dermatol 2021;30:146)
Sites
- Sites of previous surgery, trauma or burns
- Common sites: anterior chest, shoulders, upper back, back of neck, cheeks and earlobes (Clujul Med 2013;86:313)
Pathophysiology
- Exact pathogenesis of keloids and hypertrophic scar formation is unknown
- Keloids and hypertrophic scars are an abnormal response to trauma
- Wounds more likely to undergo keloid formation include wounds healing by secondary intention, wounds with prolonged inflammation (foreign body, infection, burn, earring site) and sites of repeated trauma (Clujul Med 2013;86:313)
- Hypothesized pathogenesis involves excessive and prolonged inflammation leading to dysregulated normal healing with excessive production of collagen, elastin and extracellular matrix (Scars Burn Heal 2021;7:2059513120980320)
- Fibroblasts and mast cells are increased (Scars Burn Heal 2021;7:2059513120980320)
- Growth factors and cytokines such as TGF beta, TNF alpha, interleukins are increased in keloids (Scars Burn Heal 2021;7:2059513120980320)
- Keloids have higher collagenase activity, type III collagen, chondroitin 4 sulphate and glycosaminoglycans than normal scars (Exp Dermatol 2021;30:146)
- Inconsistent genetic associations have been found linked to certain HLA subtypes and blood group A (Téot: Textbook on Scar Management, 1st Edition, 2020)
Etiology
- May develop after minor injuries, trauma, burns, insect bites, surgery, cryotherapy, topical treatments (e.g., imiquimod), acne, infections (e.g., shingles) and immunization (Int J Mol Sci 2017;18:606)
- May arise months or years after injury (Am Fam Physician 2009;80:253)
Clinical features
- Patients usually present with cosmetic concerns but may present with itch or pain (J Clin Aesthet Dermatol 2021;14:S24)
- Red to purple, firm, smooth and raised area with no hair
- Grows slowly, over months to years
- Characteristically grow laterally beyond the border of the original wound (Burns Trauma 2019;7:39)
- Clinical overlap can make distinction from hypertrophic scars and other mimics difficult (Exp Dermatol 2021;30:146)
- Risk factors include
- Age: < 30
- Fitzpatrick skin types 4 - 6 (Cureus 2022;14:e23503)
- Body region (see Sites) (Facial Plast Surg Aesthet Med 2021;23:59)
- Family history
- Previous history or multiple keloids
- History of only minor injury preceding onset of the scar
- Local tension on the skin
- Pregnancy
- Hypertension
- Rare syndromes (e.g., Noonan syndrome)
- No useful biomarkers exist to predict risk
Diagnosis
- Can usually be diagnosed by visual inspection, palpation and history (Burns Trauma 2019;7:39)
- May mimic a tumor and therefore imaging (ultrasound, CT or MRI) may help define extent and nature but there are no imaging modalities that can accurately identify keloids (Burns Trauma 2019;7:39)
- Ultrasound elastography may be helpful as keloids and hypertrophic scars are harder than the surrounding tissues
- Ultrasound may also assess effect of treatment
Radiology description
- Ultrasound: hypoechoic dermal based lesion
Prognostic factors
- Keloid is biologically harmless with no risk of malignant transformation (Sci Rep 2021;11:9390)
- Most eventually stop growing and remain stable or even involute slightly (J Plast Reconstr Aesthet Surg 2014;67:87)
- Persistence and recurrence are common (Semin Plast Surg 2021;35:145)
- May lead to aesthetic issues and serious adverse psychosocial outcomes (G Ital Dermatol Venereol 2019;154:148)
- May undergo suppuration, in which cystic cavities in keloids result in acute inflammatory flares and oozing (Int J Dermatol 2021;60:1392)
Case reports
- 10 year old child with meatoplasty keloid (J Laryngol Otol 2006;120:594)
- 30 year old woman with keloids in stretch marks (Clin Case Rep 2022;10:e6723)
- 32 year old man developed keloids following cupping therapy (Plast Reconstr Surg Glob Open 2022;10:e4669)
- 47 year old woman with extensive keloid scarring from pemphigus vulgaris (Clin Case Rep 2022;10:e6424)
- 70 year old woman with spontaneous keloids (Cureus 2022;14:e23227)
Treatment
- Multiple treatment options exist and there is considerable variability in practice
- Optimal treatment will vary depending on the age of the patient (pediatric versus adult) and body site
- An escalating treatment algorithm may be followed (Burns Trauma 2019;7:39)
- Treatment options include
- Emollients and regular massage
- Occlusive dressing
- Compression
- Fixation for lesions on a joint
- Local corticosteroid
- Steroid tape / plaster
- Steroid injections: intralesional steroids (e.g., triamcinolone acetonide)
- Surgical excision
- Recurrence following excision alone 45 - 100%; the new keloid may be larger than the original (Burns Trauma 2020;8:tkaa031)
- Excision may be combined with other modalities including steroids, imiquimod, bleomycin, cryotherapy or radiotherapy and recurrence rates are lower (Dermatol Ther 2022;35:e15425)
- Radiotherapy (Front Med (Lausanne) 2022;9:1043840)
- Laser therapy is not effective as recurrence rates are very high
- Other injectables: 5FU, interferon
- Oral medicines if large or multiple keloids
Gross description
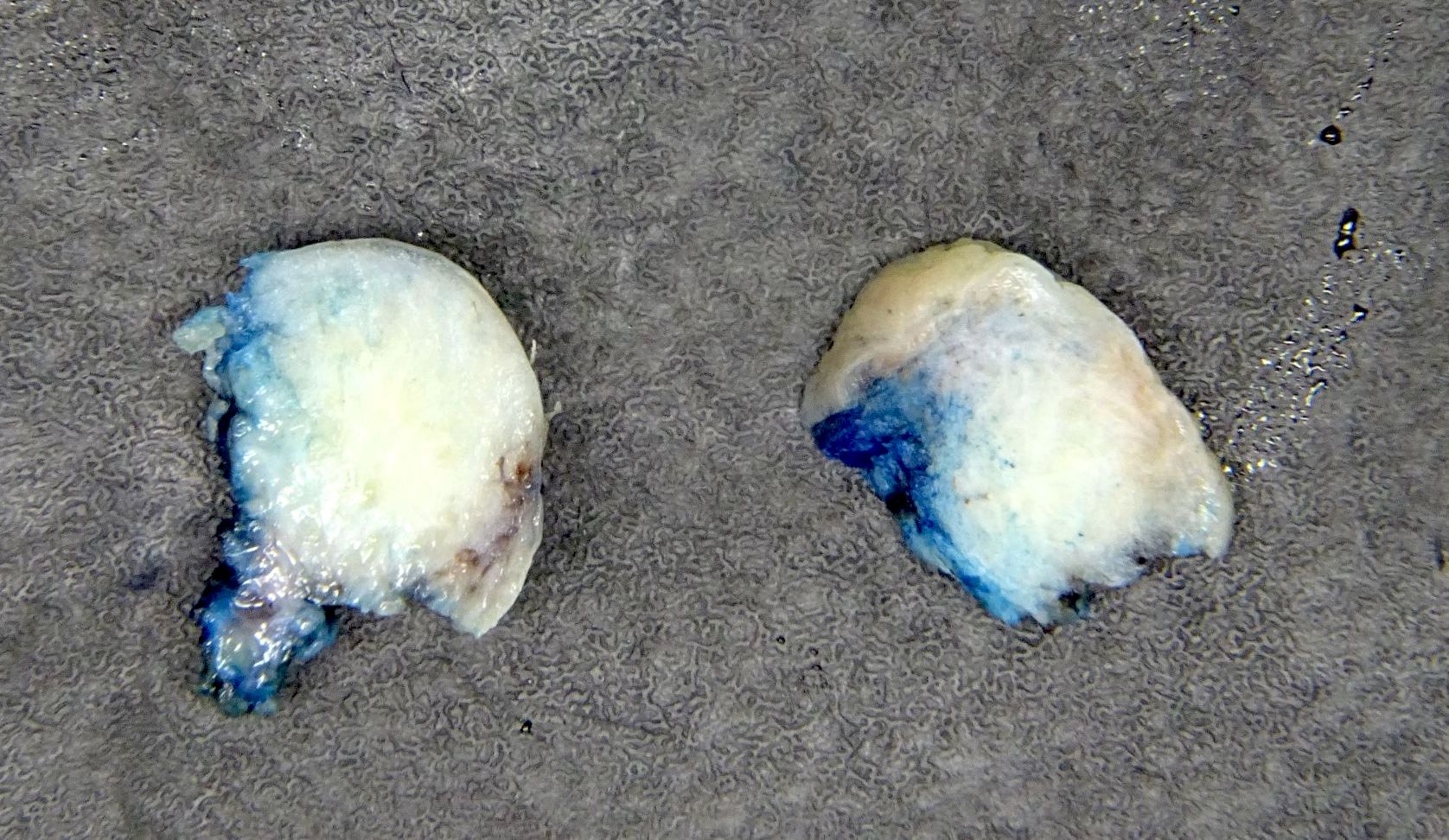
- Polypoid, covered by thin, hairless skin
- Can be small (< 2 cm) up to very large
Gross images
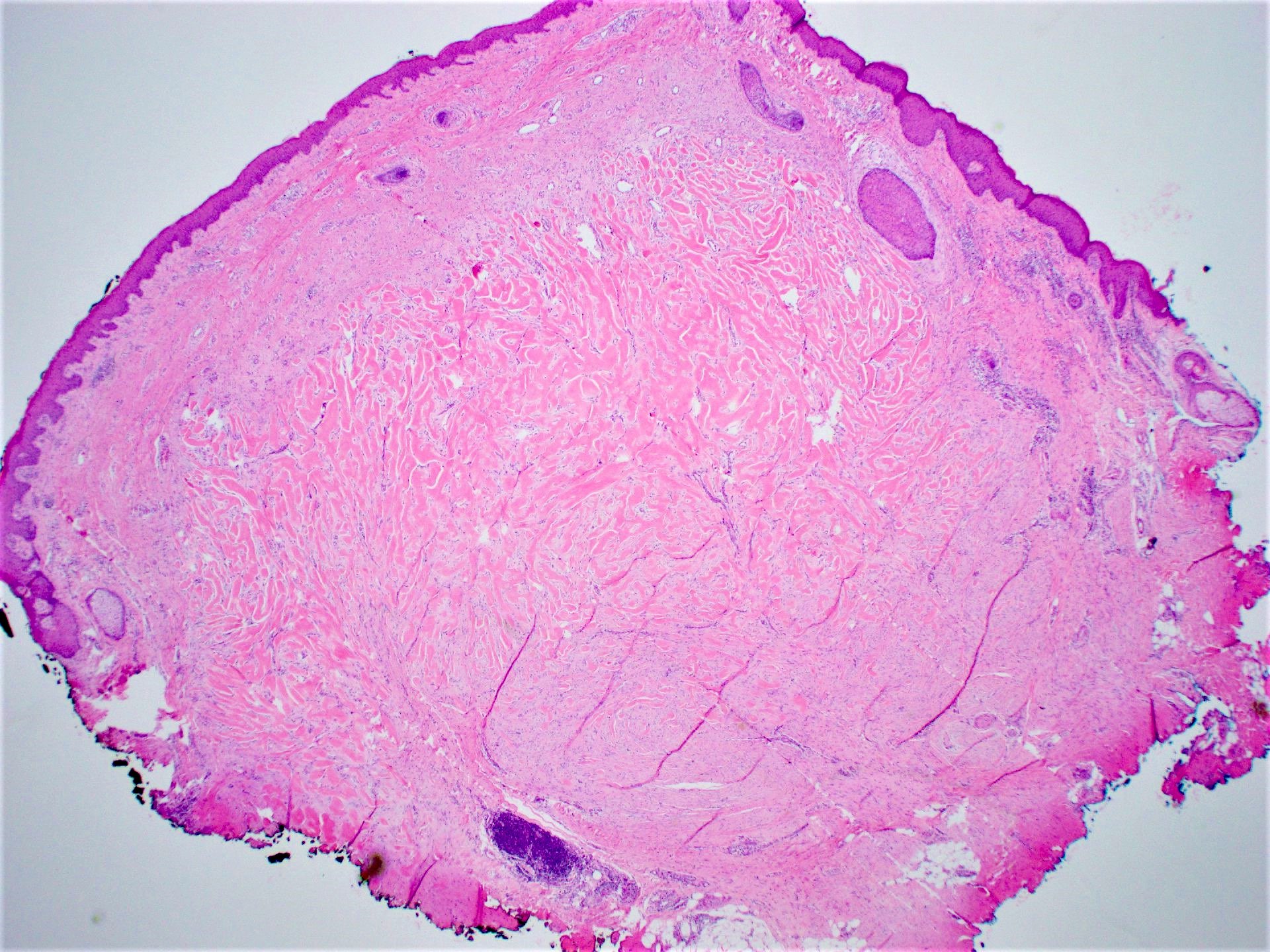
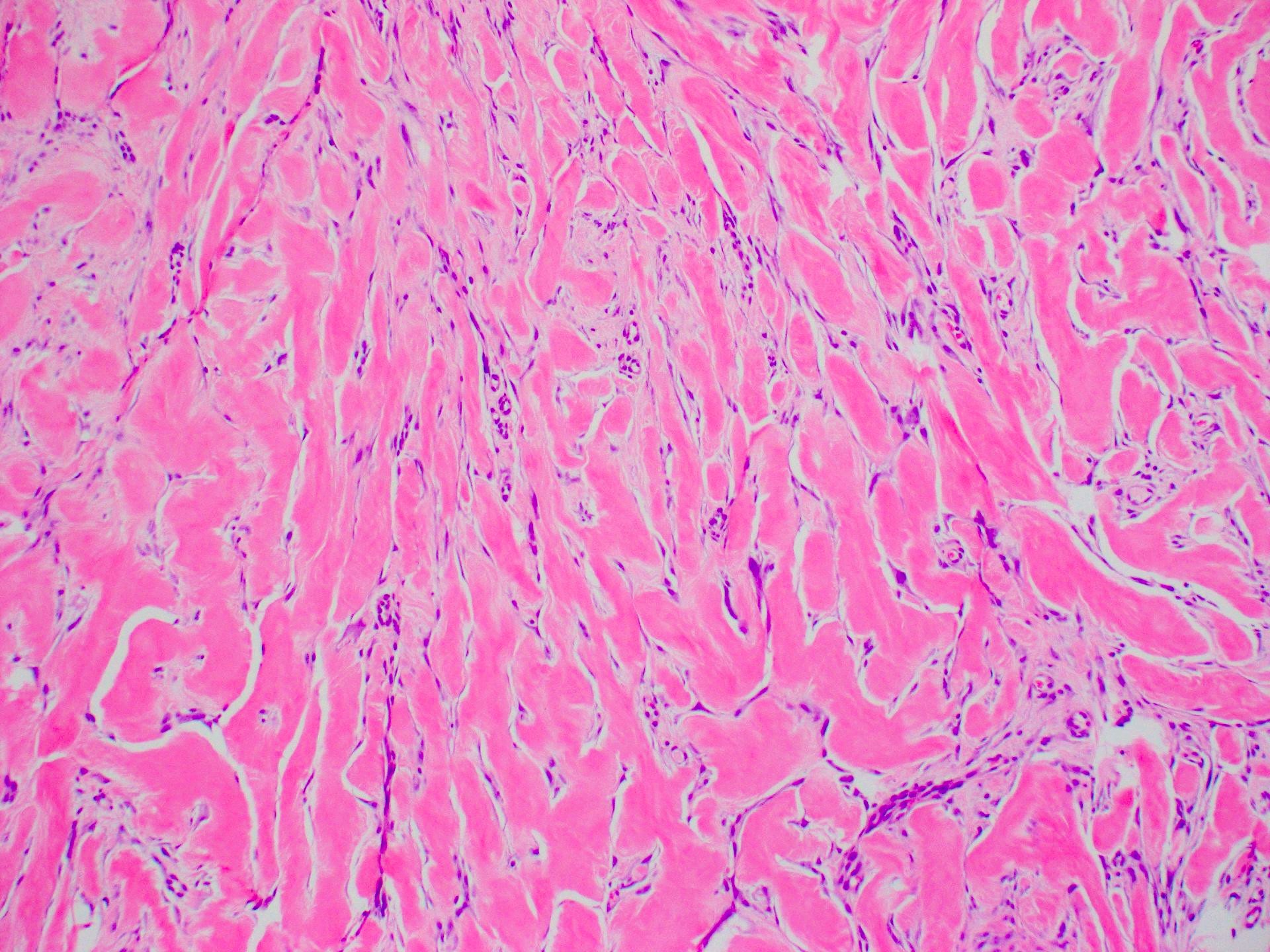
Microscopic (histologic) description
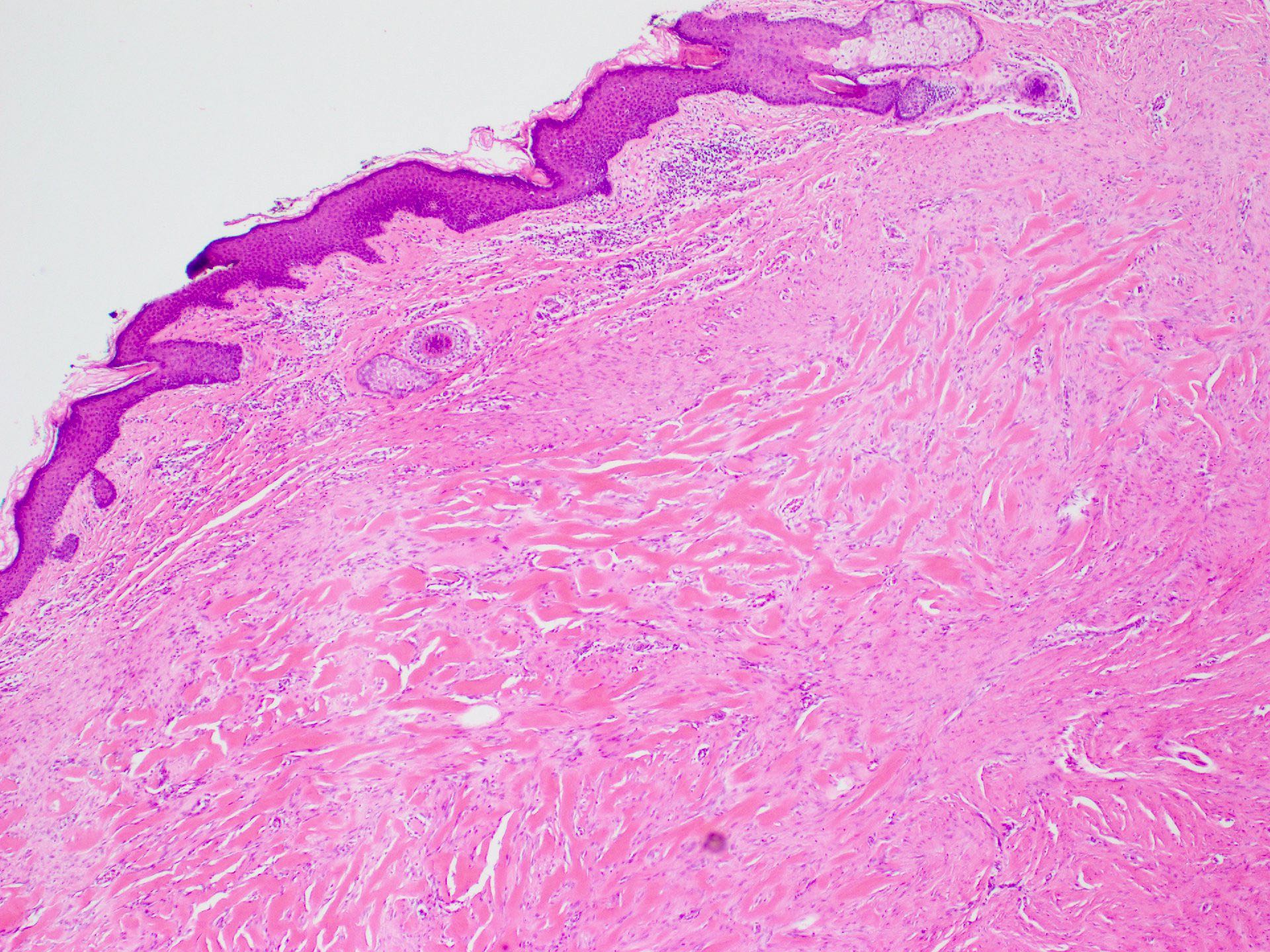
- Lesion of the deep dermis; sparing of papillary dermis (Am J Dermatopathol 2004;26:379)
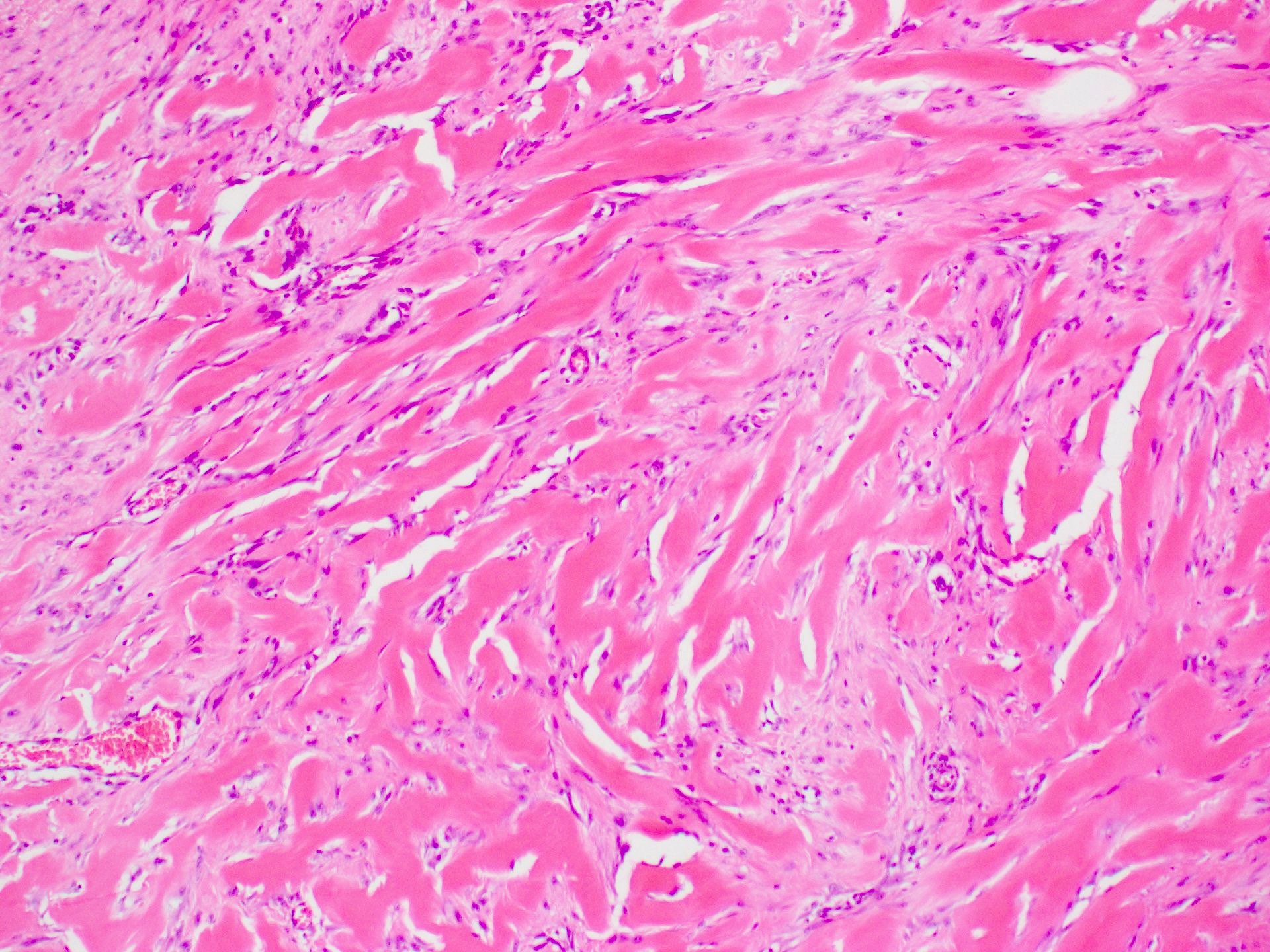
- Characteristic long, broad, closely packed collagen bundles that stain uniformly eosinophilic (keloidal collagen) arranged in haphazard fascicles (Scars Burn Heal 2021;7:2059513120980320)
- Fibroblasts are increased compared to normal skin (Front Cell Dev Biol 2020;8:360)
- May appear edematous due to increased dermal mucosubstances (J Zhejiang Univ Sci B 2022;23:699)
- Tongue-like advancing edge (Front Cell Dev Biol 2020;8:360)
- Epidermis may be normal, thin or thick (most) and may be affected by secondary changes (such as hypertrophy and inflammation due to irritation / scratching) (Front Cell Dev Biol 2020;8:360)
- Lesion replaces adnexal structures (i.e., hair follicles and sweat glands) (Histol Histopathol 2015;30:1033)
- Fewer capillaries and blood vessels than surrounding skin (J Plast Surg Hand Surg 2010;44:272)
- Tend to have marked inflammation in the dermis at the leading edge of growing keloids (Scars Burn Heal 2021;7:2059513120980320)
- Overlap with hypertrophic scar and therefore correlation with the clinical features is recommended
Microscopic (histologic) images
Virtual slides
Videos
Keloid scar:
5 minute pathology pearls
by Dr. Jerad Gardner
Sample pathology report
- Skin sternum, excision:
- Dermal scar with keloidal type collagen (see comment)
- Comment: The histological features are consistent with keloid or hypertrophic scar; correlation with the clinical features is recommended.
Differential diagnosis
- Hypertrophic scar:
- Confined to the area of injury without lateral extension
- Histological overlap: tends to have more delicate fibrillar collagen and no abundant mucosubstances
- Does not recur; clinical correlation may be required to help distinction from keloid
- Dermatofibroma, particularly keloidal dermatofibroma:
- More cellular; typically lacks keloidal collagen
- No history of preceding trauma
- Dermatofibrosarcoma protuberans:
- No history of preceding incisions / surgery at the site
- Pseudoepitheliomatous hyperplasia of the overlying epidermis
- Storiform pattern
- More cellular
- Cytological atypia present but may be subtle
- Lacks keloidal collagen
- Infiltrative edges
- Extension into subcutaneous tissue
- Morphea / scleroderma:
- Involves full thickness of dermis
- Architecture of dermis largely intact
- Collagen is thickened and hypereosinophilic but does not form intersecting bands
- Perivascular inflammatory infiltrate of lymphocytes, plasma cells and macrophages in early lesions
- Does not have increased ground substance
- Desmoplastic melanoma:
- Poorly circumscribed with deep infiltration
- Elongated spindle cells surrounded by collagen bundles; also scattered hyperchromatic or multinucleated cells with bizarre nuclei
- May have small foci of lymphoid aggregates
- May be pure or combined with classic melanoma
Additional references
Board review style question #1
Which of the following is true of keloid?
- Hypertrophic scar is synonymous with keloid scar
- Keloids are more common in Asian and African populations
- Recurrence after surgical excision is uncommon
- Thick collagen bundles are unique to keloid
Board review style answer #1
B. Keloids are more common in Asian and African populations. Keloids are up to 15 times more common in Asians, Hispanics and Africans. Answer A is incorrect because hypertrophic scars overlap histologically with keloid but are a separate clinical entity; clinical correlation may be required to separate them. Answer C is incorrect because recurrence occurs in up to half following simple excision. Answer D is incorrect because keloidal collagen is characteristic of keloid but can be seen to a lesser extent in hypertrophic scars.
Comment Here
Reference: Keloid
Comment Here
Reference: Keloid
Board review style question #2
Board review style answer #2
C. Keloid. The image shows the classic and characteristic appearance of keloidal collagen. Answer A is incorrect because while dermatofibroma can be similar in appearance, it is typically more cellular and is most common on the legs. Answer B is incorrect because while hypertrophic scars can overlap in histological appearance with keloid, they are generally more cellular and have less keloidal collagen. Clinical history helps to make the diagnosis as Asian individuals have a much higher risk, keloids are most common in young people (10 - 30 years old) and the earlobe is a typical site. Answer D is incorrect because while scleroderma / morphea can mimic keloid on a small biopsy, the collagen pattern is different (being more ordered and almost acellular) and the clinical history is not suggestive.
Comment Here
Reference: Keloid
Comment Here
Reference: Keloid