Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Case reports | Treatment | Clinical images | Gross description | Microscopic (histologic) description | Microscopic (histologic) images | Videos | Sample pathology report | Differential diagnosis | Additional references | Practice question #1 | Practice answer #1 | Practice question #2 | Practice answer #2Cite this page: Braunberger RC, Hanson JA. Eosinophilic esophagitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophaguseosinophilic.html. Accessed September 14th, 2025.
Definition / general
- Multifactorial, chronic eosinophilic inflammatory condition affecting the esophagus in both adult and pediatric patients that occurs in the absence of identifiable secondary causes (Med Clin North Am 2019;103:29)
- Characterized by a chronic immune reaction to environmental and food allergens leading to a deficient esophageal mucosal barrier (Arch Pediatr 2019;26:182)
Essential features
- Major diagnostic criteria of ≥ 15 eosinophils per high power field (40x magnification) in the proper clinical context (Arch Pediatr 2019;26:182)
Terminology
- Idiopathic or primary eosinophilic esophagitis
- Chronic atopic inflammatory disease of the esophagus
- Allergic or atopic esophagitis
ICD coding
- ICD-10: K20.0 - eosinophilic esophagitis
Epidemiology
- M:F = 3:1 (World J Gastroenterol 2019;25:4598)
- Peak incidence between 30 and 44 years of age (Gastroenterology 2018;154:319)
- Caucasians have threefold increased prevalence compared with other races
- Population based study looking at 7,000 patients diagnosed with eosinophilic esophagitis found 89.3% were Caucasians, 6.1% African American and 5.6% of Asian descent (Gastrointest Endosc Clin N Am 2018;28:27)
- More common in cold and arid climates and rural areas (Med Clin North Am 2019;103:29)
- Incidence:
- Incidence rates vary greatly depending on the geographic location
- Pooled incidence rate of 3.7 cases per 100,000 population per year (95% confidence interval, 1.7 - 6.5) from meta analysis (Gastroenterology 2018;154:319)
- Included population based studies in North America, Europe and Australia
- Pooled incidence rate for adults is 7.0 cases per 100,000 population per year (95% confidence interval, 1 - 18.3) (Aliment Pharmacol Ther 2016;43:3)
- Pooled incidence rate for children is 5.1 cases per 100,000 population per year (95% confidence interval, 1.5 - 10.9) (Aliment Pharmacol Ther 2016;43:3)
- Prevalence:
- Pooled prevalence of 22.7 per 100,000 population (95% confidence interval, 12.4 - 36.0) (Gastroenterology 2018;154:319)
Sites
- Can diffusely affect the entire length of the esophagus
Pathophysiology
- Intraepithelial eosinophils recruited via chemotaxis act as antigen presenting cells (APCs) recruiting T cells, activating mast cells and activating basophils (Arch Pediatr 2019;26:182)
- Eosinophils secrete a cationic protein eosinophilic peroxidase (EPO) and major binding protein (MBP) causing cell damage leading to the symptom of esophageal dysmotility (Arch Pediatr 2019;26:182)
- Concentration of eosinophilic peroxidase (EPO) correlates to increased symptomology, not the number of intraepithelial eosinophils (Arch Pediatr 2019;26:182)
- Recruited T cells differentiate into Th2 T cells and secrete IL4, IL5 and IL13 (Arch Pediatr 2019;26:182)
- IL4 promotes the differentiation of naïve T cells into Th2 T cells (Arch Pediatr 2019;26:182)
- IL5 promotes eosinophil survival (Arch Pediatr 2019;26:182)
- IL13 leads to expression of eotaxin3, which is a chemokine that induces eosinophilic activation and infiltration (Med Clin North Am 2019;103:29)
- Activated eosinophils produce TGF beta that promotes tissue remodeling and leads to fibrosis (Med Clin North Am 2019;103:29)
Etiology
- Environmental
- Food allergens
- Most common include milk, wheat, soy, eggs, peanuts / nuts, fish and shellfish (World J Gastroenterol 2019;25:4598)
- Hygiene and bacterial dysbiosis hypothesis
- Improved hygiene conditions lead to reduced bacterial exposures and alterations in the microbiota, which may alter mucosal permeability (World J Gastroenterol 2019;25:4598)
- Gastroesophageal reflux disease (GERD) leads to increased mucosa permeability to food allergens
- Proton pump inhibitor (PPI) usage
- Reduced acid secretion downregulates digestive enzyme activation
- Food antigens are not degraded, increasing the immune response to these large proteins (World J Gastroenterol 2019;25:4598)
- Food allergens
- Genetic / familial
- Genetic variants at multiple loci have been shown to increase the risk of development of atopic diseases, including eosinophilic esophagitis and asthma
- Genes found with alterations in patients with eosinophilic esophagitis:
- CCL26 - encodes eotaxin3
- Thymic stromal lymphopoietin (TSLP)
- Filaggrin (FLG)
- Desmoglein1 (DSG1)
- STAT6
- Calpain 14 (CAPN14)
- CRLF2
- Genes found with alterations in patients with eosinophilic esophagitis:
- Genetic variants at multiple loci have been shown to increase the risk of development of atopic diseases, including eosinophilic esophagitis and asthma
Clinical features
- Symptoms vary widely based on the age group:
- Pediatrics
- Infants and small children: emesis, food rejection, regurgitation, irritability, dysphagia and rarely growth retardation (World J Gastroenterol 2019;25:4598, Arch Pediatr 2019;26:182)
- School aged children and adolescents: nausea, emesis, regurgitation, chest and abdominal pain, dysphagia and food impaction (World J Gastroenterol 2019;25:4598, Arch Pediatr 2019;26:182)
- Adults
- Dysphagia, chest and abdominal pain and untreatable heartburn (World J Gastroenterol 2019;25:4598, Arch Pediatr 2019;26:182)
- Pediatrics
Diagnosis
- Eosinophilic esophagitis is a clinicopathologic diagnosis and findings should be considered in combination and not independent of each other
- Current diagnostic modalities
- Esophagogastroduodenoscopy (endoscopy)
- Endoscopy may show many characteristic but not pathognomonic changes
- Major criteria: mucosa edema, white exudate, longitudinal furrows, circular esophageal rings (also called pseudotrachea), esophageal stenosis (Gut 2013;62:489)
- Minor criteria: feline esophagus (concentric mucosal rings observed with some types of motility that disappear with air insufflation), narrow caliber esophagus, crêpe paper esophagus, mucosal laceration or fragility with passage of instruments before dilation (Gut 2013;62:489)
- Up to 25% of patients have normal endoscopic findings (World J Gastroenterol 2019;25:4598)
- Endoscopy may show many characteristic but not pathognomonic changes
- Esophageal biopsies are required for diagnosis
- Biopsies need to be taken from the proximal, mid and distal esophagus with a minimum of 2 biopsies per site
- 6 - 9 mucosal biopsies yield a near 100% diagnostic sensitivity (World J Gastroenterol 2019;25:4598)
- Single biopsy yields a sensitivity of 55% (Arch Pediatr 2019;26:182)
- Histology
- Major criteria: ≥ 15 eosinophils per high power field (40x magnification) (Arch Pediatr 2019;26:182)
- Minor criteria: extreme basal zone hyperplasia with papillary hyperplasia, eosinophils concentrated in the surface epithelium as opposed to the base, eosinophilic microabscesses, eosinophil degranulation, surface desquamation, lamina propria fibrosis (Arch Pediatr 2019;26:182)
- Esophagogastroduodenoscopy (endoscopy)
- Noninvasive diagnostic procedures being tested
- Esophageal string test (EST) (Am J Gastroenterol 2019;114:1614)
- Currently in clinical trials
- 1 hour test that can distinguish active from inactive disease in both children and adults
- Minimally invasive way to monitor disease
- Cytosponge (Curr Treat Options Gastroenterol 2019;17:48)
- Mesh sponge tethered by a string that is compressed in a dissolvable capsule
- Capsule is swallowed and then withdrawn through the mouth
- Sensitivity of 75% and specificity of 86%
- MicroRNA expression (Curr Treat Options Gastroenterol 2019;17:48)
- Esophageal brushings obtained via endoscopy or via nasogastric tube are analyzed for the presence and quantity of eosinophil derived neurotoxin, which is overexpressed in eosinophilic esophagitis
- Esophageal string test (EST) (Am J Gastroenterol 2019;114:1614)
Radiology description
- Radiology is useful for the evaluation of fibrostenotic disease (Gastrointest Endosc Clin N Am 2018;28:47)
- Barium esophagram is more sensitive than endoscopy for identification of strictures and diffuse small caliber esophagus (Gastrointest Endosc Clin N Am 2018;28:47)
- Strictures are classified by the length of fixed narrowing
- Rings are ≤ 1 cm (Gastrointest Endosc Clin N Am 2018;28:47)
- Strictures ≤ 8 cm (Gastrointest Endosc Clin N Am 2018;28:47)
- Small caliber esophagus > 8 cm (Gastrointest Endosc Clin N Am 2018;28:47)
- Strictures are classified by the length of fixed narrowing
Case reports
- 11 year old boy with allergic rhinitis and chest pain (Clin Endosc 2019;52:606)
- 34 year old man with refractory heartburn following 2 month trial of proton pump inhibitor and intermittent dysphagia (CMAJ 2016;188:893)
- 40 year old Caucasian woman with eosinophilic esophagitis and spontaneous transmural esophageal perforation (J Med Case Rep 2019;13:275)
Treatment
- Treatment revolves around the 3 Ds: drugs, diet and dilation
- Drugs
- Proton pump inhibitors:
- First line therapy
- Generally used in combination with dietary modifications as there is a high association with food allergens
- Corticosteroids:
- Second line therapy
- Topical or systemic (systemic reserved for patients with severe symptoms)
- Proton pump inhibitors:
- Diet
- Dietary modification due to the role that food allergens play in the pathogenesis of the disease
- Elemental diet
- Elimination diets
- Guided by allergy testing
- Empiric elimination diets
- Dietary modification due to the role that food allergens play in the pathogenesis of the disease
- Dilation
- Treatment for esophageal strictures and narrowing
- Improves symptoms of dysphagia only
- A meta analysis showed the risk of perforation from dilation procedures in eosinophilic esophagitis was 0.3% (Med Clin North Am 2019;103:29)
- Treatment for esophageal strictures and narrowing
Gross description
- Major criteria (Gut 2013;62:489)
- Mucosa edema
- Exudate or white plaques
- Longitudinal furrows
- Circular esophageal rings (pseudotrachea)
- Esophageal stenosis
- Minor criteria (Gut 2013;62:489)
- Feline esophagus
- Concentric mucosal rings observed with some types of motility that disappear with air insufflation
- Narrow caliber esophagus
- Crêpe paper esophagus
- Mucosal laceration or fragility with passage of instruments before dilation
- Feline esophagus
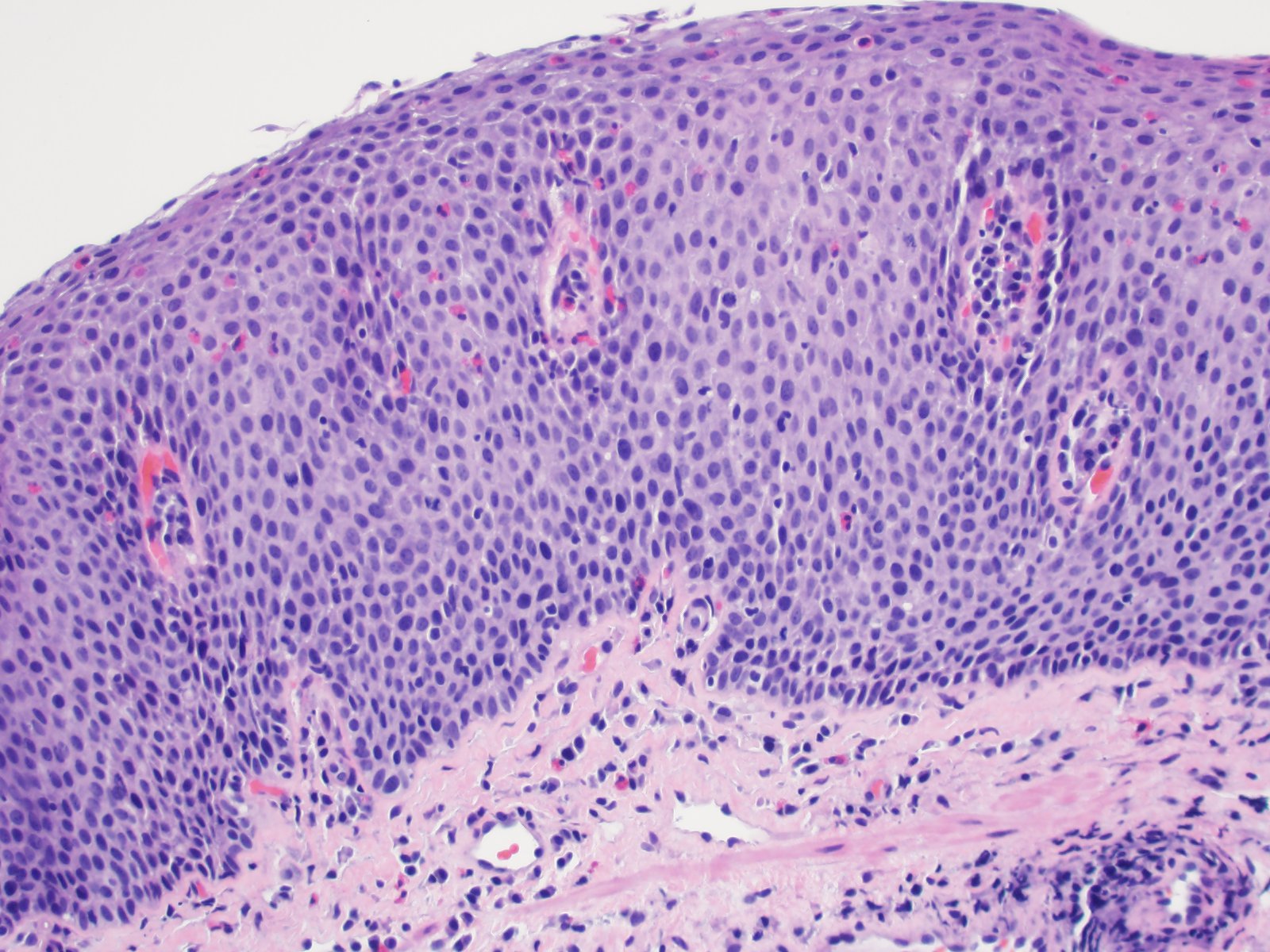
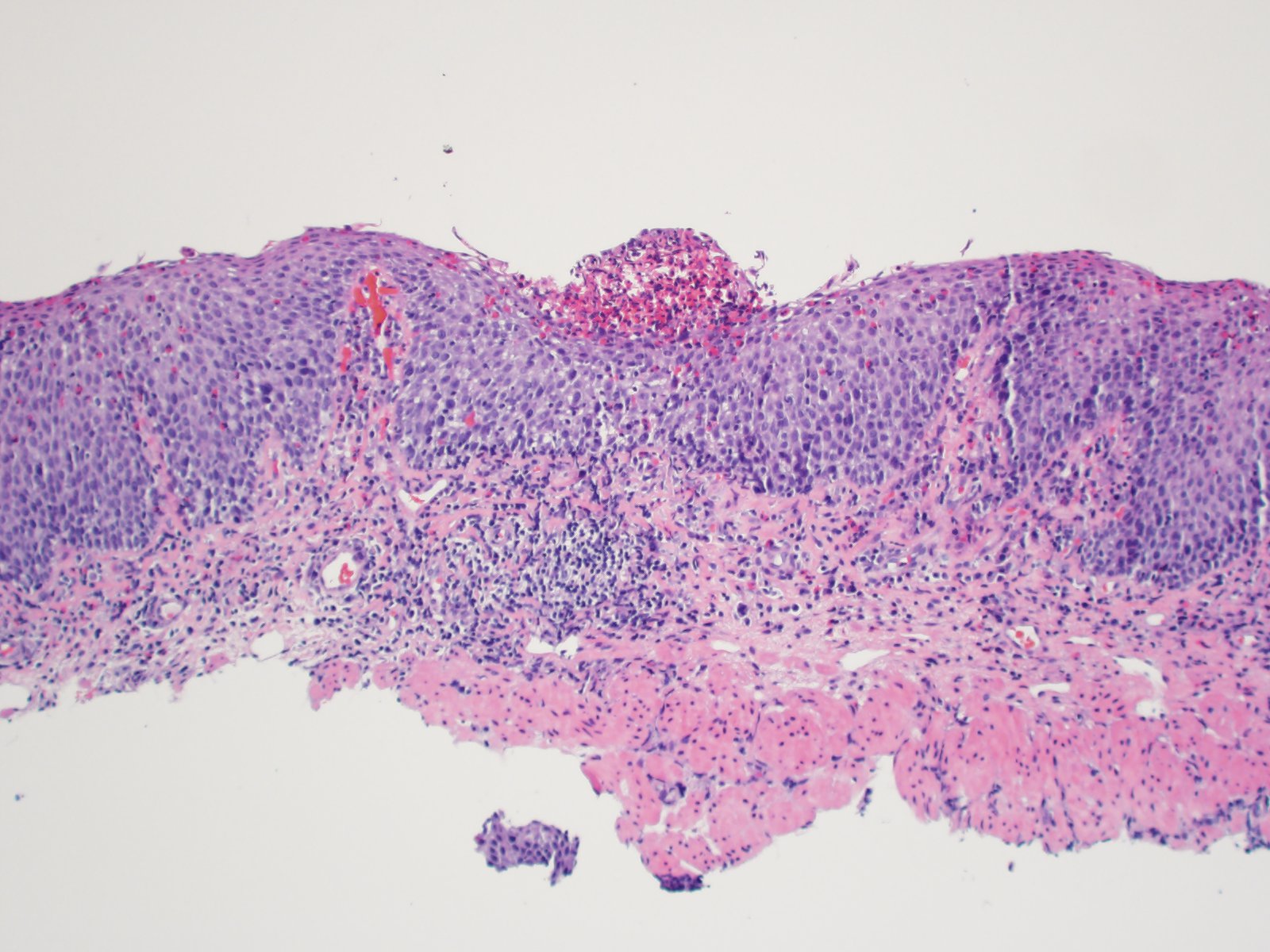
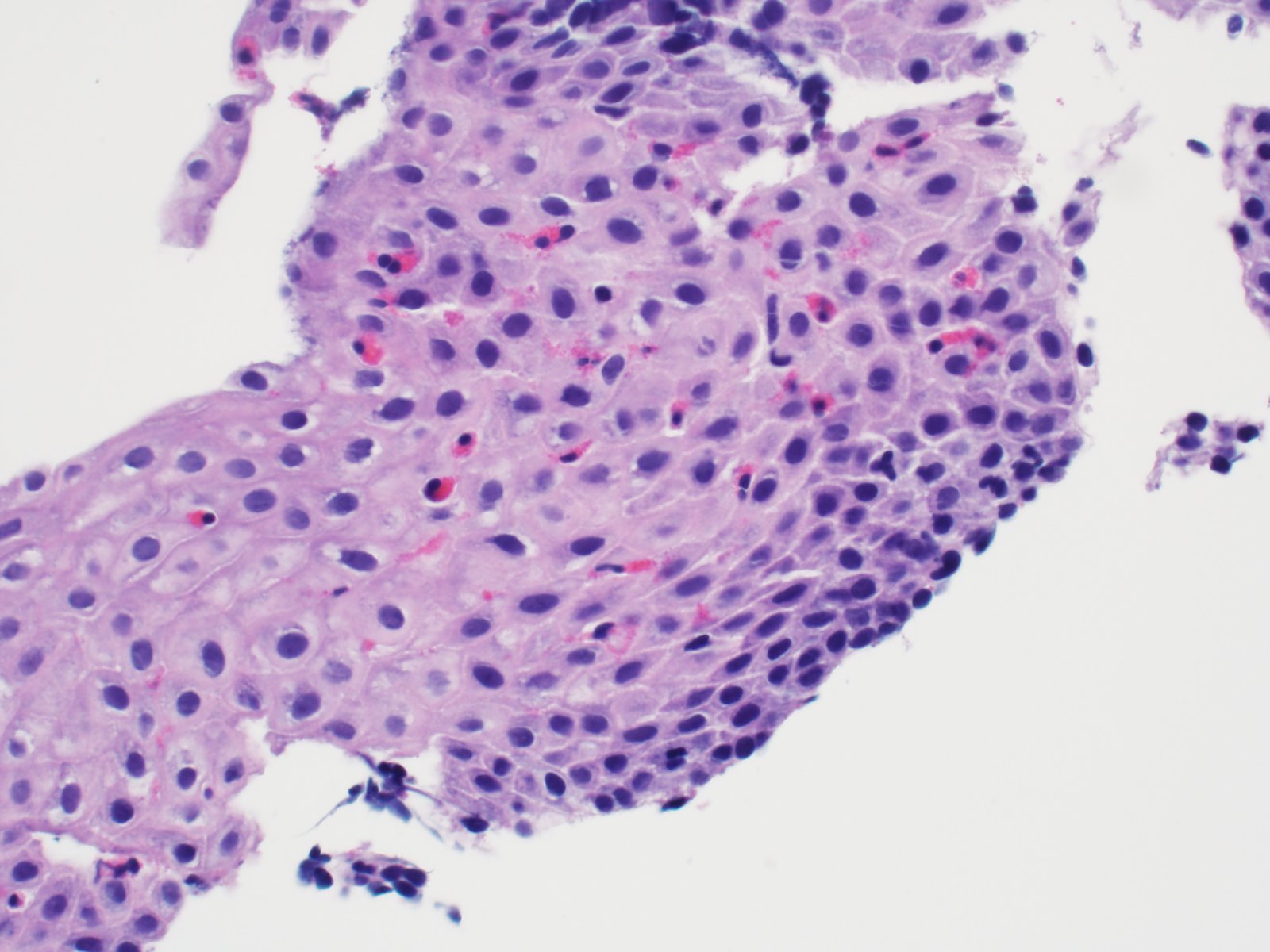
Microscopic (histologic) description
- Major criterion: ≥ 15 eosinophils per high power field (40x magnification) present in the squamous mucosa (Arch Pediatr 2019;26:182)
- Minor criteria: eosinophils concentrated in the surface epithelium as opposed to the base, extreme basal zone hyperplasia, eosinophilic microabscesses, eosinophil degranulation, surface desquamation, lamina propria fibrosis (Arch Pediatr 2019;26:182)
Microscopic (histologic) images
Videos
Endoscopic features of eosinophilic esophagitis
Sample pathology report
- Esophagus, mid, biopsy:
- Eosinophil rich esophagitis (> 50 eosinophils per single high power field, maximum count) (see comment)
- Comment: The biopsy demonstrates marked reactive basal zone hyperplasia with increased eosinophils. The eosinophils have a top heavy distribution and few eosinophilic microabscesses are identified. These features are consistent with eosinophilic esophagitis in the proper clinical context.
Differential diagnosis
- Gastroesophageal reflux disease (GERD):
- Triad of findings includes:
- Hyperplasia of lamina propria papillae (greater than two - thirds of the epithelial thickness)
- Mild basal zone hyperplasia (approximately 15 - 25% of the epithelial thickness)
- Mildly increased intraepithelial eosinophils concentrated at the base of the mucosa as opposed to the surface (usually < 10 per high power field though counts are not pathognomonic for either condition) (Arch Pediatr 2019;26:182)
- Eosinophil counts in GERD are generally higher in distal esophageal biopsies compared with more proximal biopsies (this is reversed in eosinophilic esophagitis but is not pathognomonic)
- No surface eosinophilic microabscesses
- No lamina propria fibrosis
- Other intraepithelial inflammatory cells seen in some but not all cases include lymphocytes and neutrophils
- Triad of findings includes:
- Eosinophilic gastroenteritis:
- Affects any portion of the gastrointestinal tract with the stomach and small bowel being the most common locations (Lancet Gastroenterol Hepatol 2018;3:271)
- Symptoms such as diarrhea, intestinal obstruction and ascites are not common in eosinophilic esophagitis
- When seen in the esophagus, can be an exact histologic mimic of eosinophilic esophagitis so clinical presentation and correlation with other mucosal biopsies is essential
- PPI responsive esophageal eosinophilia:
- Same symptomatology and histologic findings as eosinophilic esophagitis but has complete remission with PPI therapy
- May actually be the same disease as eosinophilic esophagitis
Additional references
Practice question #1
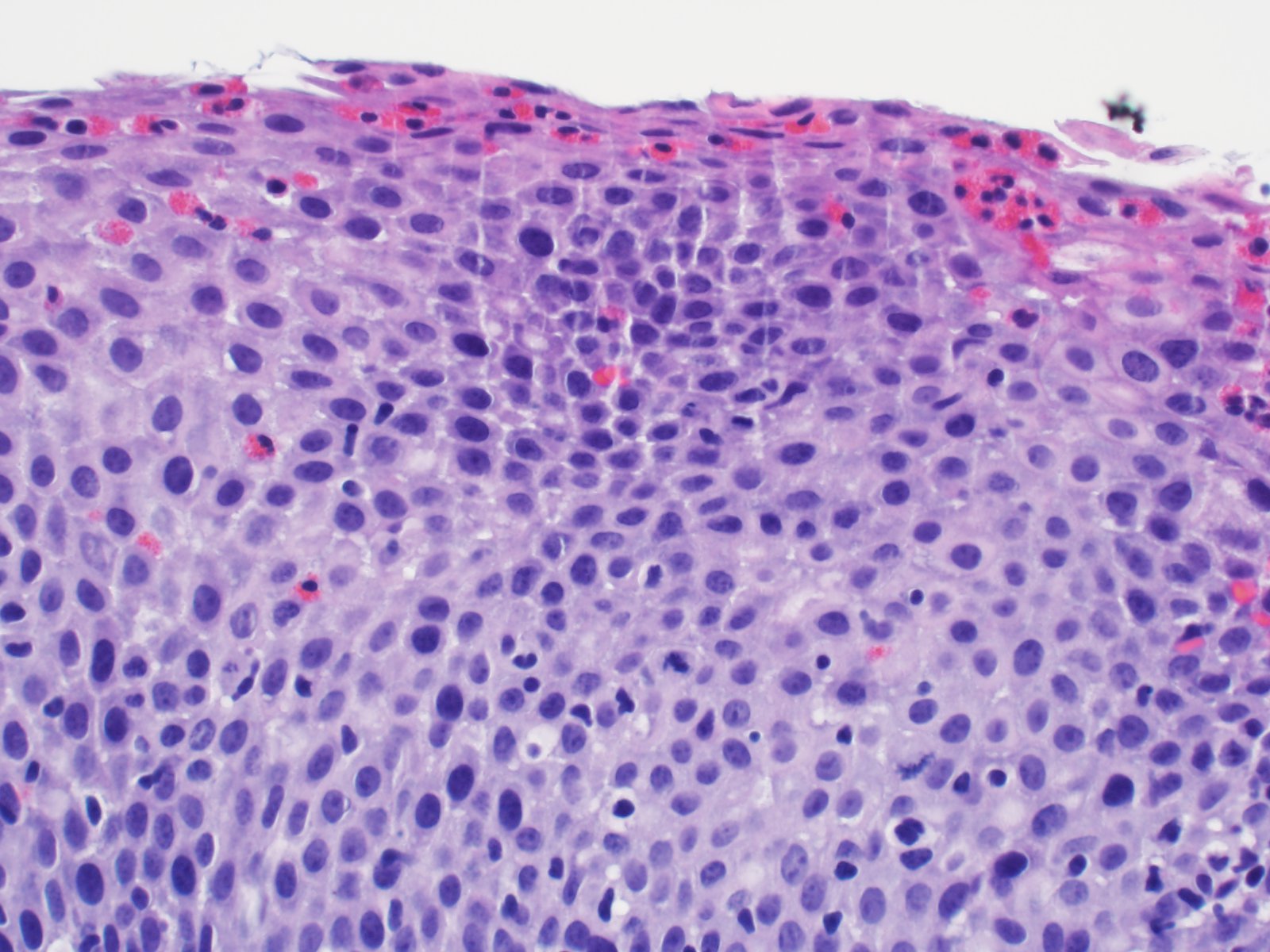
A 12 year old boy with a history of seasonal allergies and asthma complains of dysphagia and abdominal pain. Endoscopic biopsies reveal increased eosinophils in the esophageal squamous mucosa. What feature shown in the image favors eosinophilic esophagitis over GERD as the most likely diagnosis?
- Increased mitotic activity
- Intercellular edema
- Scattered intraepithelial lymphocytes
- Superficial concentration of eosinophils
Practice answer #1
Practice question #2
A 36 year old man presents to clinic with the chief complaint of intermittent dysphagia and heartburn that has not responded to over the counter medications. Endoscopy was notable for white plaques in the esophagus, longitudinal furrows and pseudotrachea. Biopsies taken during endoscopy show increased eosinophils in the distal and proximal specimens. Which chemokine producing immune cell plays an essential role in eosinophil infiltration and activation?
- B cells
- Eosinophils
- Mast cell
- Th2 T cells
Practice answer #2