Table of Contents
Definition / general | Essential features | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Case reports | Treatment | Clinical images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2 | Board review style question #3 | Board review style answer #3Cite this page: Aljuboori O, Garcia-Buitrago MT. Lymphocytic esophagitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/esophaguslymphocyticesophagitis.html. Accessed April 18th, 2024.
Definition / general
- Uncommon esophageal histologic pattern of injury related to different etiologies (Am J Surg Pathol 2022;46:e55, Ann N Y Acad Sci 2018;1434:185)
- Controversial diagnosis as a new distinct disease rather than a pattern of injury associated with more prevalent conditions (Am J Surg Pathol 2022;46:e55)
- More common in older women and patients with underlying immunologic abnormalities (Dig Dis Sci 2021;66:3976, Am J Surg Pathol 2022;46:e55)
- Gastroesophageal reflux disease (GERD), Crohn's disease, dysmotility, achalasia and medication induced esophagitis are some of the underlying conditions associated with lymphocytic esophagitis pattern of injury (Am J Surg Pathol 2022;46:e55)
Essential features
- Dysphagia is the most common clinical presentation (Am J Surg Pathol 2020;44:198)
- Histologically characterized by a triad of intraepithelial lymphocytosis, with epithelial damage and no significant granulocytic inflammation
- Unequivocal mucosal lymphocytosis
- Rare to absent granulocytes
- Epithelial damage consists of dyskeratotic keratinocytes (Civatte bodies) and intracellular edema (spongiosis) (Am J Surg Pathol 2022;46:e55)
ICD coding
- ICD-10: K20.90 - esophagitis, unspecified without bleeding
Epidemiology
- Prevalence is estimated to be 0.1% in adult population and 5.7% in pediatric population (Cureus 2022;14:e30300)
- F > M, with median age in the sixth decade (J Clin Gastroenterol 2012;46:828, Gut 2012;61:1108)
- In pediatric population, there is a strong association between lymphocytic esophagitis and Crohn's disease (Inflamm Bowel Dis 2014;20:1324, Inflamm Bowel Dis 2011;17:45)
Sites
- Any level within the tubular esophagus can be affected (Am J Surg Pathol 2022;46:e55)
Pathophysiology
- Pathophysiology is currently not well understood
Etiology
- Several conditions and diseases are associated with this pattern of injury, from autoimmune diseases such as Crohn's, rheumatoid arthritis, dysmotility disorder (achalasia) to medication effect (Dig Dis Sci 2021;66:3976)
Clinical features
- Dysphagia is the most common presentation (Dig Dis Sci 2021;66:3976)
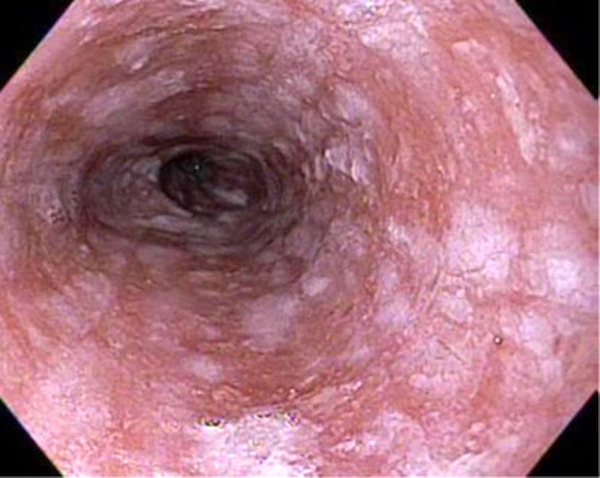
- On endoscopy, features can vary based on the underlying cause from normal appearing esophagus to strictures and edematous esophagus (Am J Surg Pathol 2022;46:e55, Am J Surg Pathol 2015;39:1558, Am J Surg Pathol 2020;44:198)
Diagnosis
- Diagnosis is based on histological findings
Case reports
- 28 year old woman with polyvalent sensitization to food and inhalant allergens presented with intermittent dysphagia (Allergy Asthma Clin Immunol 2021;17:56)
- 66 year old woman complaining of dysphagia for several weeks with the loss of ability to swallow solid foods (Cureus 2022;14:e30300)
- 71 year old man with a medical history of squamous cell carcinoma of the tongue treated with external beam radiation 17 years ago presented with dysphagia (Cureus 2018;10:e2153)
Treatment
- No definitive targeted treatment for lymphocytic esophagitis
- Management is pointed towards the underlying condition
- 1 case report listed empiric therapy with oral steroids, proton pump inhibitor and balloon dilation (Cureus 2022;14:e30300)
Microscopic (histologic) description
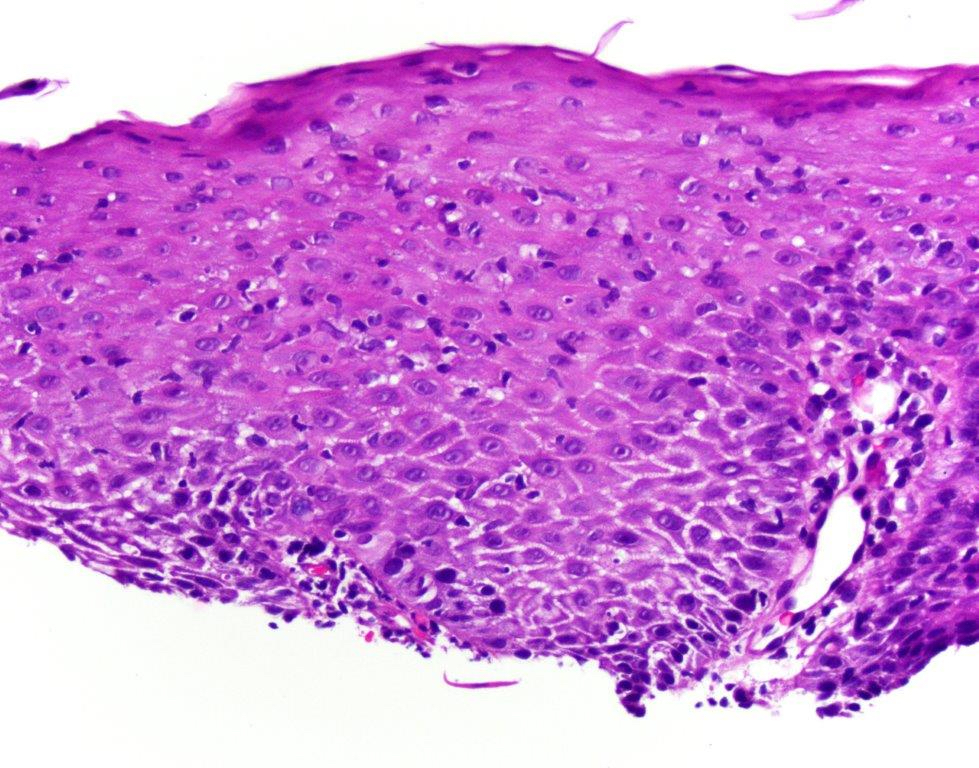
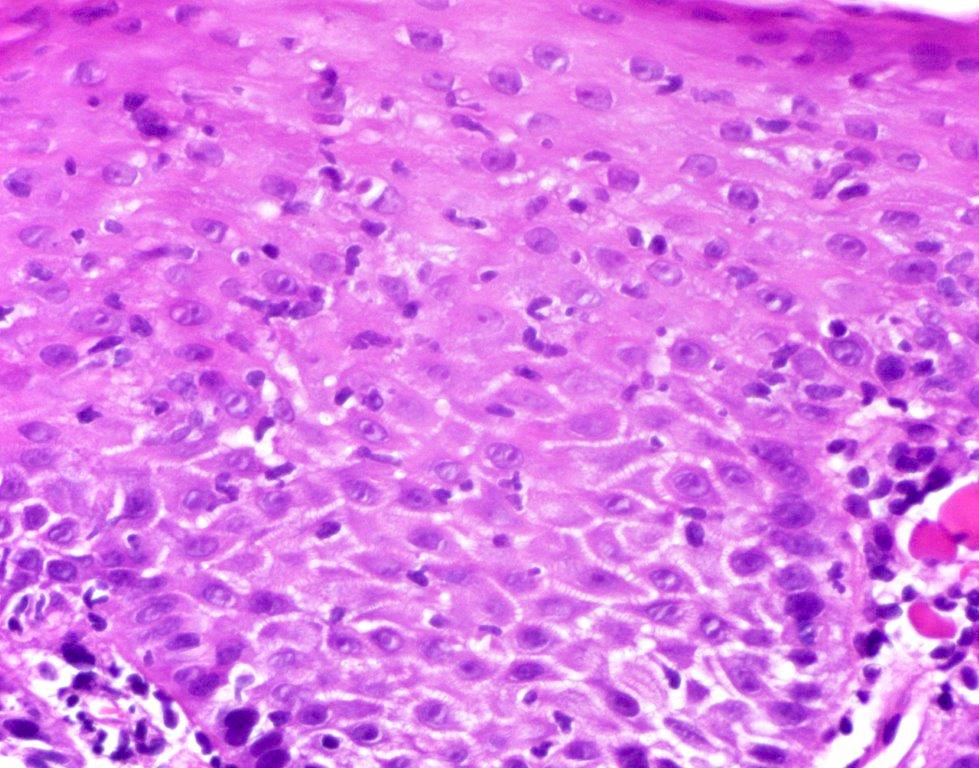
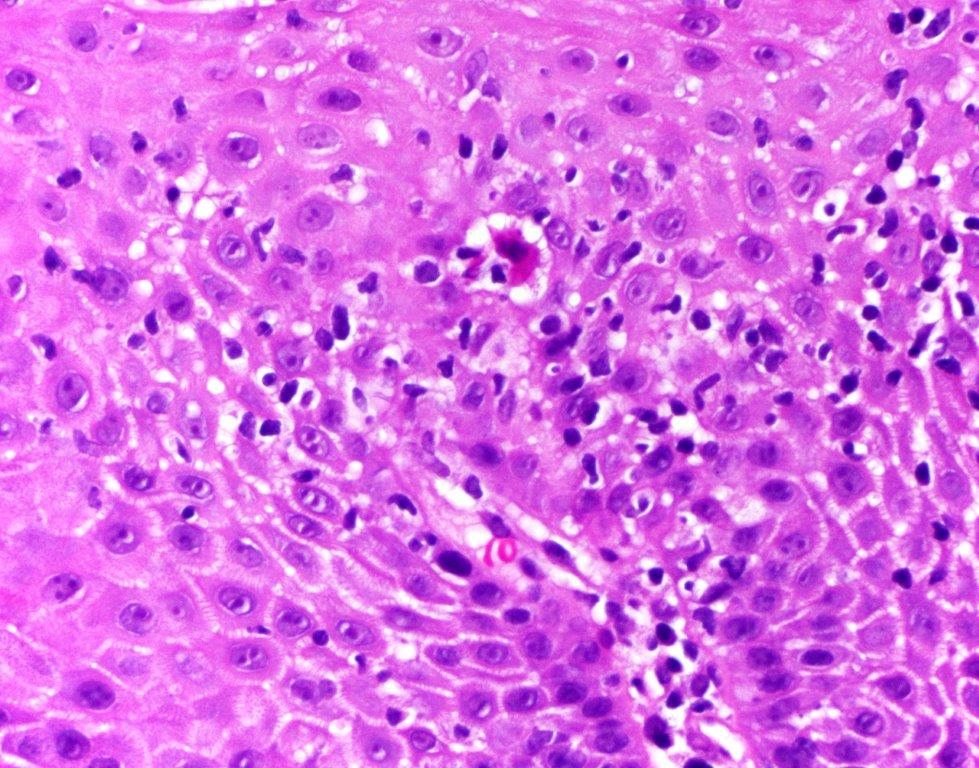
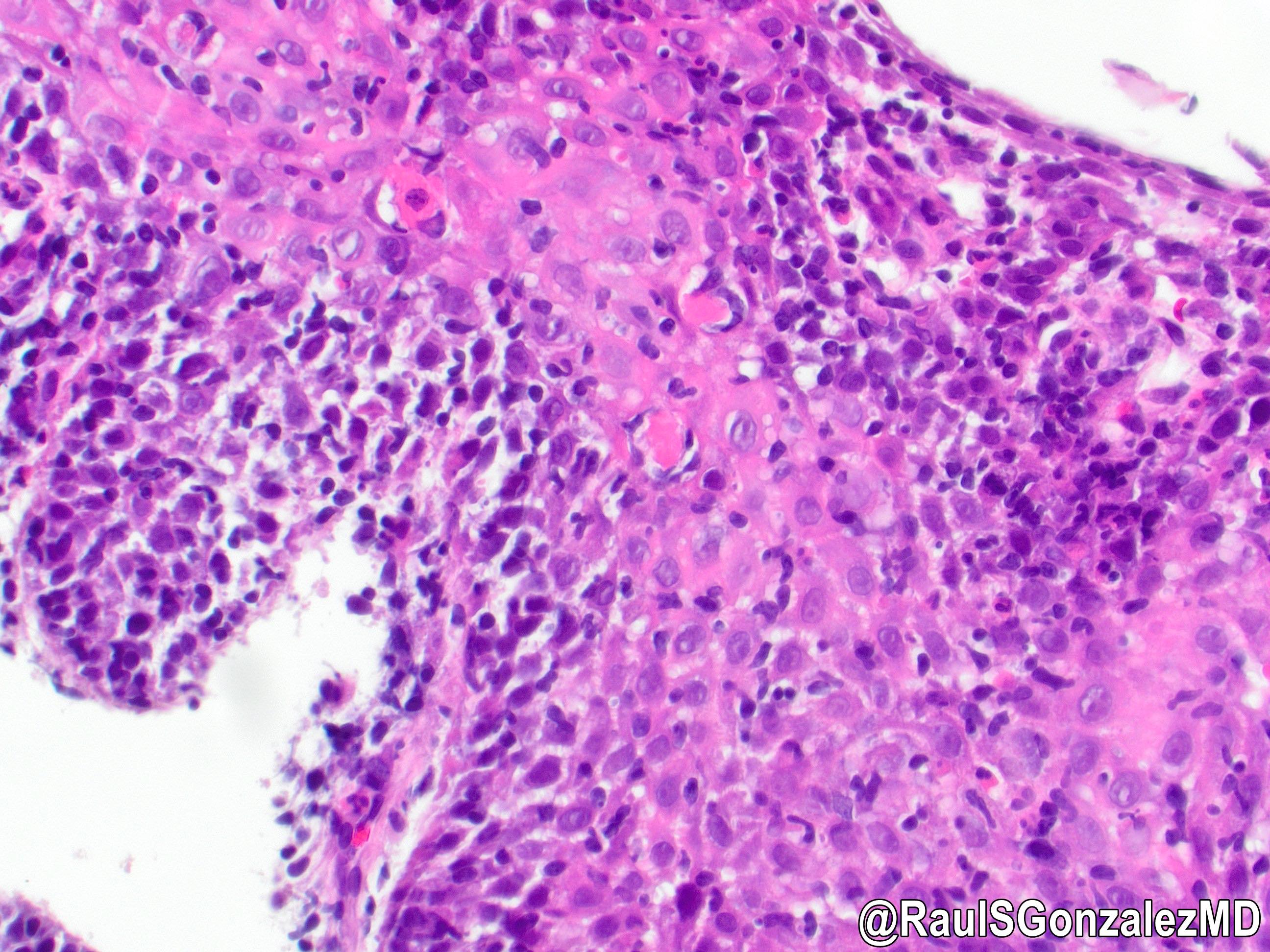
- Characterized by a triad of intraepithelial lymphocytosis, with epithelial damage and no significant granulocytic inflammation
- Unequivocal mucosal lymphocytosis; studies have reported various cutoff values for lymphocytes, ranging from 20 - 50/HPF (Am J Surg Pathol 2022;46:e55)
- Rare to absent granulocytes (if present abundantly it argues against the diagnosis of lymphocytic esophagitis) (Am J Surg Pathol 2022;46:e55)
- Epithelial damage consists of dyskeratotic keratinocytes (Civatte bodies) and nonspecific changes such as intracellular edema (spongiosis) (Am J Surg Pathol 2022;46:e55, Am J Surg Pathol 2020;44:198)
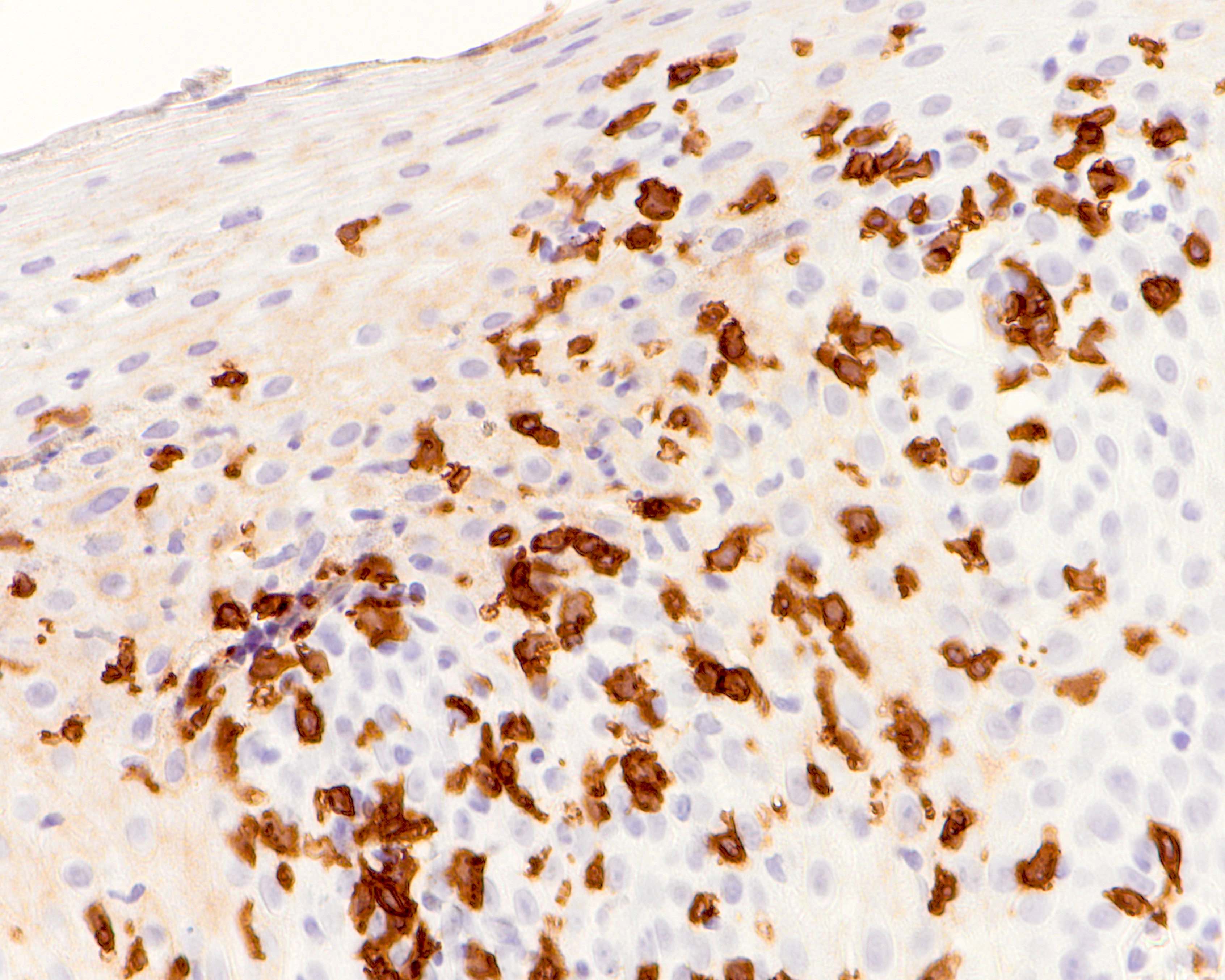
- Depending on the underlying disease, the T cell population may differ
- Crohn's and most GERD patients can have a high CD8:CD4 ratio while dysmotility patients tend to show predominance of CD4 helper T cells with a CD4:CD8 ratio > 1 (neither sensitive nor specific) (Arch Pathol Lab Med 2021;145:1138, Am J Surg Pathol 2015;39:1558)
Microscopic (histologic) images
Contributed by Monica T. Garcia-Buitrago, M.D., Omar Aljuboori, M.B.B.S. and @RaulSGonzalezMD on Twitter
Negative stains
Sample pathology report
- Esophagus, biopsy:
- Esophageal squamous mucosa with lymphocytic esophagitis (see comment)
- Comment: Lymphocytic esophagitis pattern of injury is associated with rheumatological diseases, Crohn's disease, hypothyroidism, immune mediated conditions, medications (i.e., checkpoint inhibitors) and dysmotility disorders.
Differential diagnosis
- Gastroesophageal reflux disease (GERD):
- Histologic features that are associated with GERD include inflammatory cell infiltrates and classically eosinophils
- Basal cell hyperplasia with elongated vascular papillae and esophageal spongiosis
- Candida esophagitis:
- These patients are usually immunocompromised
- On endoscopy, there are visible white plaques that can be scraped off easily from the underlying mucosa
- Neutrophilic infiltration is seen in biopsy along with fungal pseudohyphae in sloughed epithelial debris or invading intact squamous epithelium perpendicularly
- Radiation esophagitis:
- Acute postradiation esophagitis usually shows mucosal necrosis and neutrophilic infiltration
- In chronic esophagitis, there is submucosal fibrosis, capillary telangiectasia and vascular hyalinization
- Esophageal lichen planus:
- On endoscopy, mucosal denudation, trachealization and hyperkeratosis are seen; esophageal stenosis may occur
- Prominent band-like lymphocytic infiltrate involving the interface of lamina propria and epithelium, intraepithelial lymphocytes and dyskeratotic keratinocytes (Am J Surg Pathol 2013;37:1889)
- Direct immunofluorescence shows diagnostic globular IgM deposits and fibrinogen deposits along the basement membrane zone
- Esophageal graft versus host disease (GVHD):
- History of hematopoietic stem cell or lymphocyte rich transplant
- On endoscopy: esophageal webs or strictures in upper or mid third of the esophagus in chronic GVHD
- Intraepithelial lymphocytosis, basilar vacuolization, epithelial apoptosis and necrosis in severe disease (Best Pract Res Clin Haematol 2008;21:251)
Board review style question #1
A 60 year old woman underwent an upper endoscopy for dysphagia. Endoscopy revealed stricture in the mid esophagus. In addition to the findings pictured, no neutrophilic / eosinophilic infiltrate was present. What is the most probable diagnosis?
- Candida esophagitis
- Gastroesophageal reflux disease (GERD)
- Lymphocytic esophagitis
- Radiation esophagitis
Board review style answer #1
C. Lymphocytic esophagitis. The presence of increased lymphocytic infiltrates, esophageal swelling and absence of neutrophilic and eosinophilic infiltrate point towards the diagnosis of lymphocytic esophagitis. Answer B is incorrect because eosinophilic and neutrophilic infiltrates associated with basal epithelial changes are characteristic of gastroesophageal reflux disease (GERD). Answer A is incorrect because neutrophilic infiltration along with fungal pseudohyphae in sloughed epithelial debris is a hallmark of Candida esophagitis. Answer D is incorrect because radiation esophagitis is usually associated with mucosal necrosis and marked neutrophilic infiltration.
Comment Here
Reference: Lymphocytic esophagitis
Comment Here
Reference: Lymphocytic esophagitis
Board review style question #2
A 71 year old man with a known history of squamous cell carcinoma of the tongue treated with external beam radiation 17 years prior, presented to the clinic for esophagogastroduodenoscopy (EGD) with dilation for esophageal strictures. His only complaint at this time was dysphagia. A biopsy was taken and showed the findings above. Which of the following are characteristic features of lymphocytic esophagitis?
- Basal cell hyperplasia, spongiosis and elongated papillae with intraepithelial lymphocytes can be seen but are accompanied by eosinophils and rare neutrophils
- Intraepithelial lymphocytosis, basilar vacuolization, epithelial apoptosis and necrosis with a history of hematopoietic stem cell transplant
- Intraepithelial lymphocytosis, epithelial damage and paucity of granulocytes
- Prominent band-like lymphocytic infiltrate involving the interface of lamina propria and epithelium, intraepithelial lymphocytes and dyskeratotic keratinocytes
Board review style answer #2
C. Intraepithelial lymphocytosis, epithelial damage and paucity of granulocytes. The presence of lymphocytic infiltrate, esophageal swelling and absence of neutrophilic and eosinophilic infiltrate are the clinical features of lymphocytic esophagitis. Answer D is incorrect because these are the features of esophageal lichenoid planus. Answer B is incorrect because these are the features of graft versus host disease (GVHD). Answer A is incorrect because these are the features of gastroesophageal reflux disease (GERD).
Comment Here
Reference: Lymphocytic esophagitis
Comment Here
Reference: Lymphocytic esophagitis
Board review style question #3
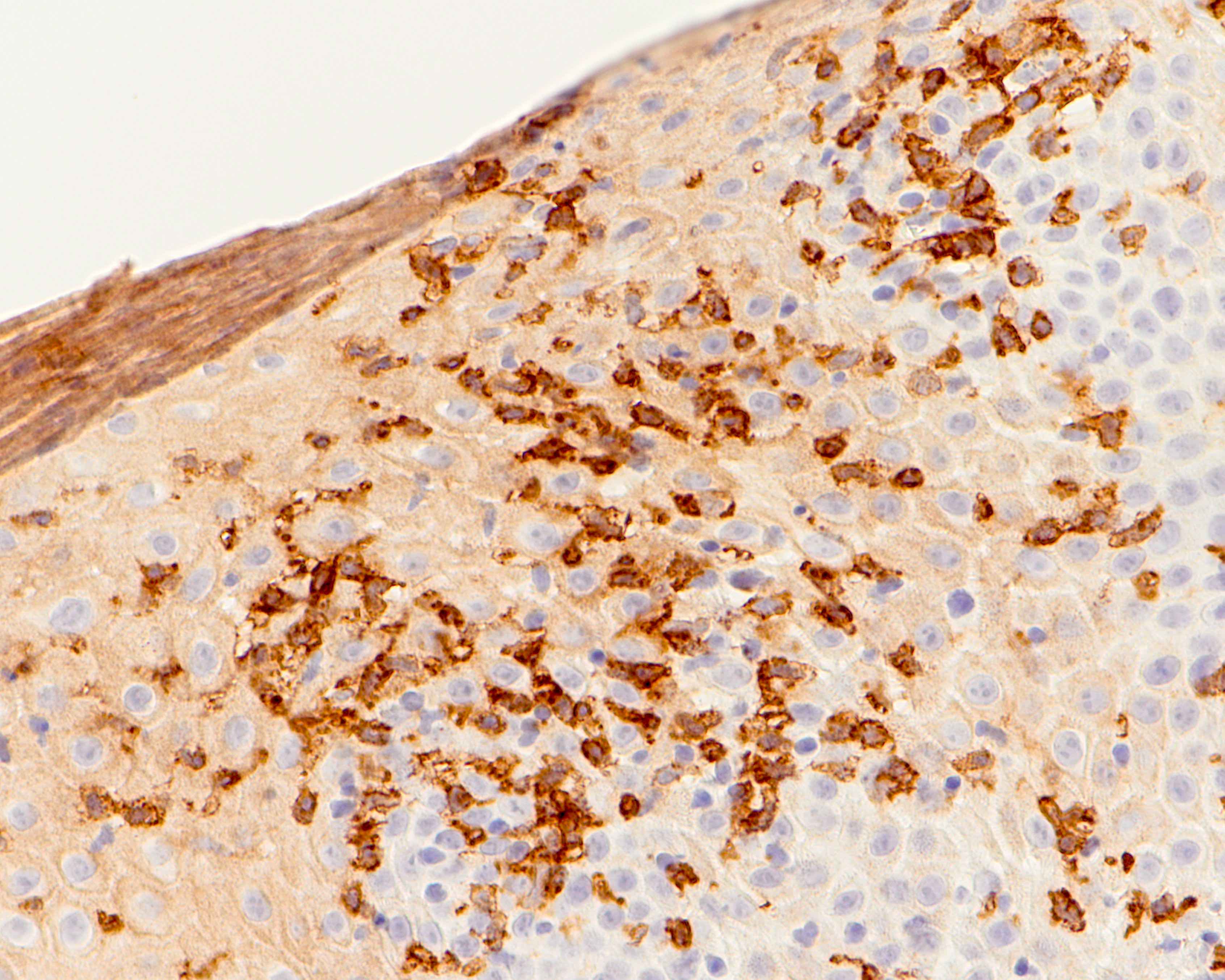
Which of the following stains highlights most of the cells in lymphocytic esophagitis?
- CD3
- CD20
- CD68
- CD138
Board review style answer #3
A. CD3. CD3 stain identifies T cells, increased in lymphocytic esophagitis cases. Answer B is incorrect because CD20 stain shows rare B cells in lymphocytic esophagitis. Answer C is incorrect because CD68 stain is expressed in histiocytic and monocytic cells. Answer D is incorrect because CD138 stain is expressed in plasma cells.
Comment Here
Reference: Lymphocytic esophagitis
Comment Here
Reference: Lymphocytic esophagitis