Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Immunofluorescence description | Immunofluorescence images | Stains | Electron microscopy description | Electron microscopy images | Videos | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Larqué A. Anti-GBM nephritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyAntiGBMnephritis.html. Accessed April 18th, 2024.
Definition / general
- Immune complex small vessel vasculitis caused by autoantibody to glomerular basement membrane (GBM) collagen, resulting in rapidly progressive glomerulonephritis and sometimes lung hemorrhage (Clin Exp Nephrol 2013;17:603)
Essential features
- Anti-GBM disease
- Rapidly progressive glomerulonephritis
- Crescent formation with segmental fibrinoid necrosis
- Bright linear ribbon-like appearance IgG in GBM
Terminology
- Anti-GBM disease
- Goodpasture syndrome
ICD coding
Epidemiology
- Rare, with an incidence of 0.5 - 1.6 cases per 1 million per year (Clin J Am Soc Nephrol 2017;12:1162, Clin J Am Soc Nephrol 2016;11:1392)
- Bimodal age distribution with peaks in second and sixth decades of life; rare in children < 11 years old
- Male predilection in second decade and female in sixth decade
- More common in Caucasians; rare in African Americans
Sites
- Kidney
- Lung
Pathophysiology
- It is likely that environmental triggers act in genetically susceptible individuals to develop pathogenic autoantibodies against the noncollagenous domain 1 of the a3 chain of type IV collagen (a3(IV)NC1)
- These autoantibodies bind to GBM and activate the classical pathway of the complement system, which starts neutrophil dependent inflammation (Nephrol Dial Transplant 2018;33:196)
Etiology
- The factors that initiate the autoimmune process remain unknown (Clin J Am Soc Nephrol 2017;12:1162)
- Strong HLA gene association, with approximately 80% of patients inheriting an HLA-DR2 haplotype
- Strongly associated with polymorphisms of MHC class II genes, with disease susceptibility correlating with human leucocyte antigen (HLA) DRB1 alleles (Nephrol Dial Transplant 2018;33:196)
- Infectious associations
- Inhalation of hydrocarbons and cigarette smoking (lung hemorrhage)
- Treatment with the anti CD52 mAb, alemtuzumab, a lymphocyte depleting agent that is increasingly used in the treatment of relapsing multiple sclerosis (N Engl J Med 2008;359:768)
Clinical features
- Acute kidney injury (> 90%) with hematuria and proteinuria (rarely in nephrotic range) (J Autoimmun 2014;48-49:108)
- 40 - 60% will have concurrent lung hemorrhage
- Other symptoms are dyspnea, rales, rhonchi, cough, shortness of breath, hemoptysis, chest pain
- A small minority of patients may present with isolated pulmonary disease (5 - 10%)
Diagnosis
- Detection of circulating anti-GBM antibodies in conjunction with rapidly progressive glomerulonephritis or alveolitis
Laboratory
- Detection of circulating anti-GBM antibodies by using Western blot and ELISA (Clin J Am Soc Nephrol 2017;12:1162)
- Titers do not correlate with severity
- The pathogenic antibodies are usually of the IgG class, with IgG1 and IgG3 subclasses predominating
- Approximately 10% of patients do not have identifiable circulating antibodies with conventional assays
- Some female patients have high IgG4 titers associated with pulmonary hemorrhage
- Antineutrophil cytoplasmic antibodies (ANCA) present in 1/3 of anti-GBM disease patients
Prognostic factors
- The proportion of crescents observed in the biopsy sample correlates strongly with the degree of renal impairment at presentation (Nephrol Dial Transplant 2015;30:814, Clin J Am Soc Nephrol 2018;13:63)
- Poor prognostic factors
- Dialysis requirement at presentation or Cr > 5 mg/dL
- Oligoanuria
- Low percentage of normal glomeruli and large extent of interstitial infiltrate on biopsy
- Rarely recurs if anti-GBM alone (no ANCA)
- Poor prognostic factors
Case reports
- 33 year old man with bizarre posttransplant anti-GBM disease (Cent Eur J Immunol 2019;44:210)
- 37 year old man with recurrent anti-GBM disease and T cell large granular lymphocytic leukemia (Medicine (Baltimore) 2019;98:e16649)
- 53 year old woman with anti-GBM disease treated with rituximab (Medicine (Baltimore) 2019;98:e17801)
- 61 year old woman with double negative anti-GBM disease (Oxf Med Case Reports 2019;2019:omy124)
- 79 year old woman with ANCA associated vasculitis and anti-GBM antibodies (CEN Case Rep 2020;9:42)
Treatment
- Plasmapheresis along with cyclophosphamide and corticosteroids (Clin J Am Soc Nephrol 2017;12:1162)
Microscopic (histologic) description
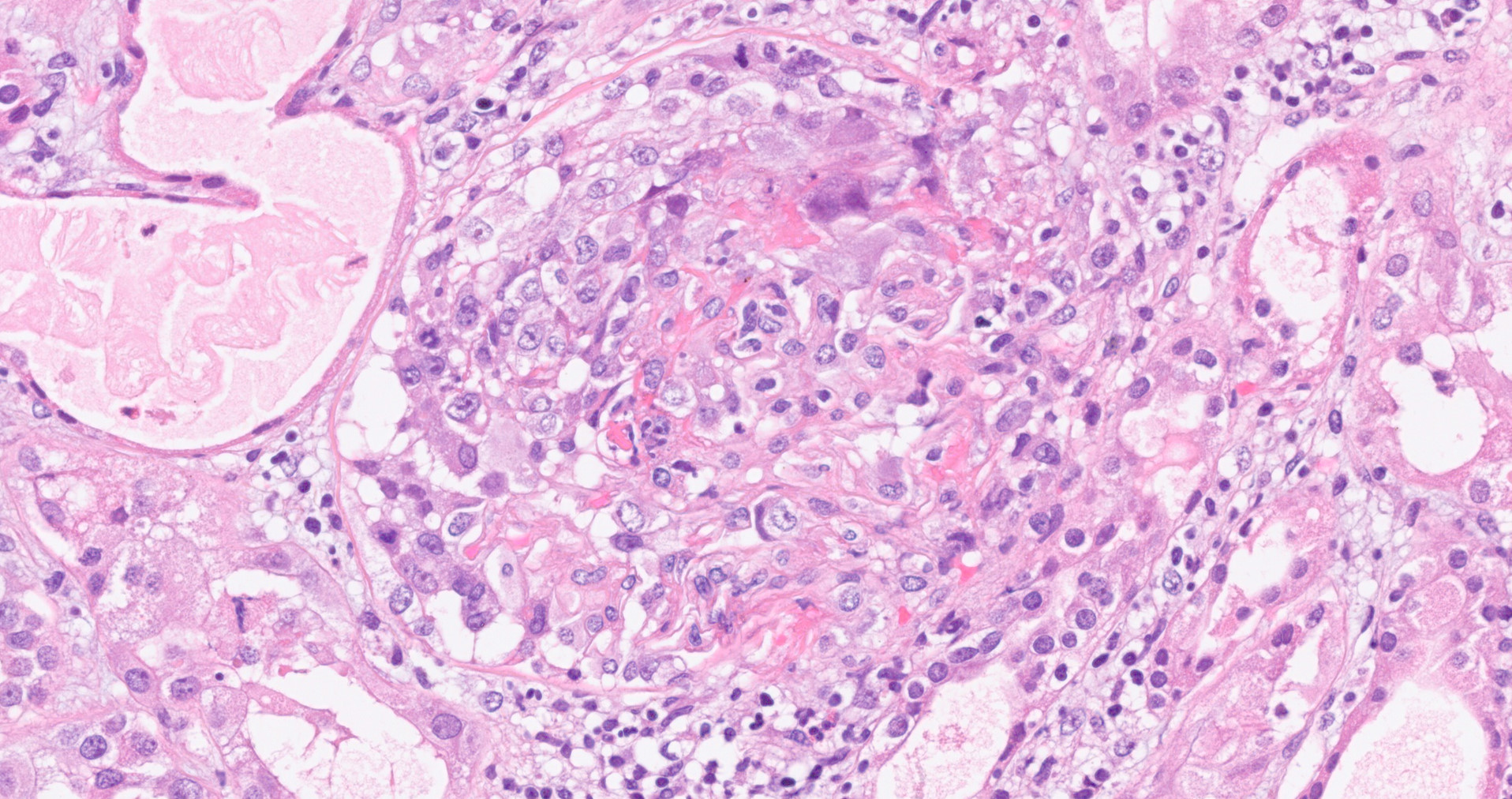
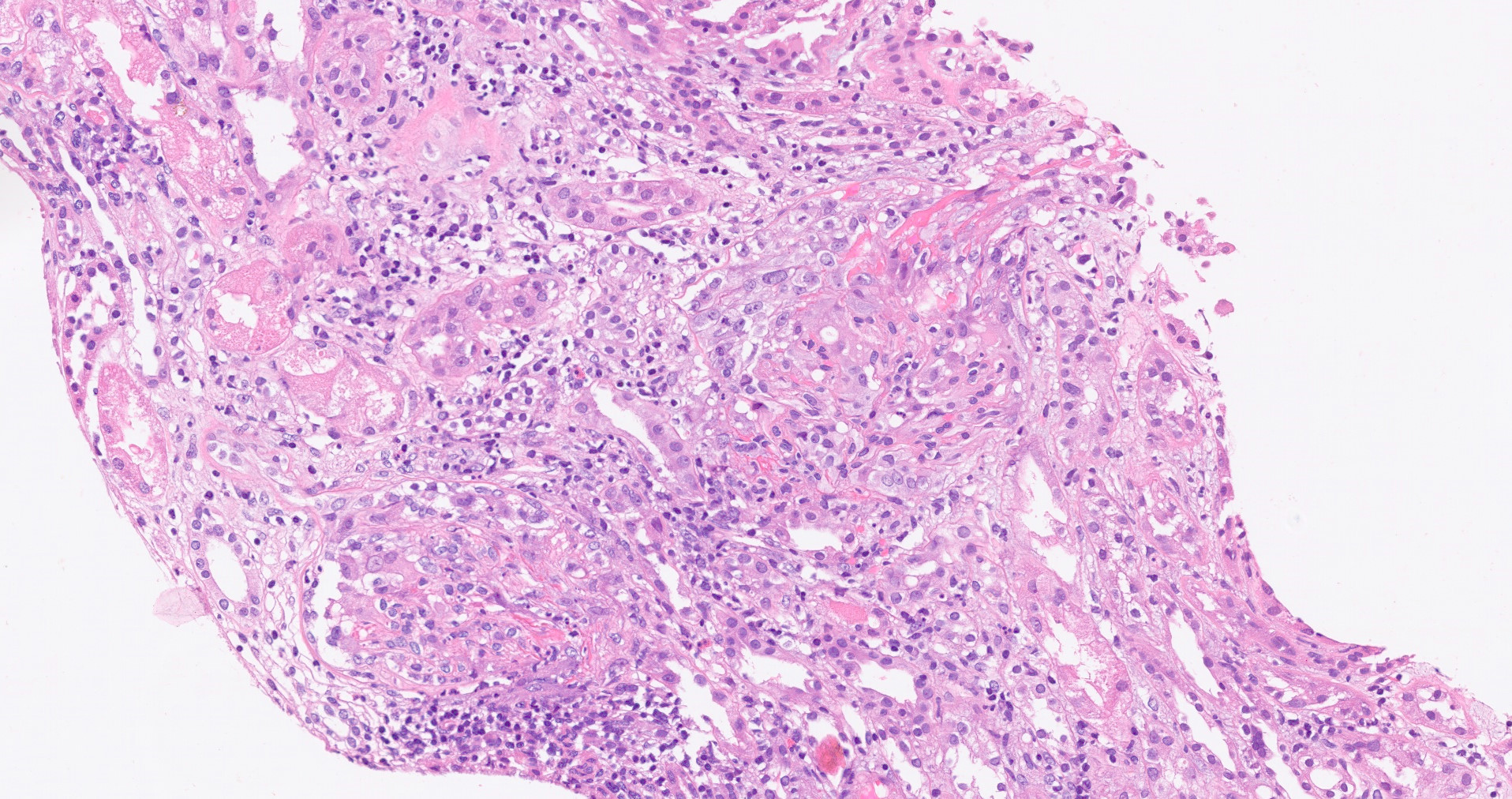
- Glomeruli:
- Cellular crescents ± segmental fibrinoid necrosis (hallmark)
- Often involves > 75% of glomeruli
- These crescents will typically be of uniform age, in contrast to other causes of rapidly progressive glomerulonephritis where a mixture of cellular, fibrocellular and fibrous crescents may be seen
- In early or mild disease, segmental proliferative change may be seen, with infiltrating neutrophils or mononuclear lymphocytes
- In severe disease, rupture of Bowman capsule, periglomerular inflammation progressing to granuloma formation with multinucleate giant cells may be observed in a proportion of cases
- Thrombotic microangiopathy involving glomerular capillaries present in subset of anti-GBM glomerulonephritis
- Noncrescentic glomeruli may have segmental fibrinoid change, although often they may appear completely normal
- Atypical, mild forms with lobular mesangial expansion or minimal glomerular lesions and few crescents
- Cellular crescents ± segmental fibrinoid necrosis (hallmark)
- Interstitium:
- Interstitial inflammation consists of lymphocytes, plasma cells, neutrophils and macrophages
- Necrotizing vasculitis rare, may be due to presence of ANCA
Microscopic (histologic) images
Immunofluorescence description
- Direct immunofluorescence on frozen kidney tissue
- Bright linear ribbon-like appearance IgG in GBM (99%) (hallmark)
- An important caveat is that fluorescence may be negative or unclear in cases with severe glomerular inflammation, in which the underlying architecture is so disrupted that the linear pattern may not be recognized
- Linear tubular basement membrane IgG staining in 10 - 67%
Immunofluorescence images
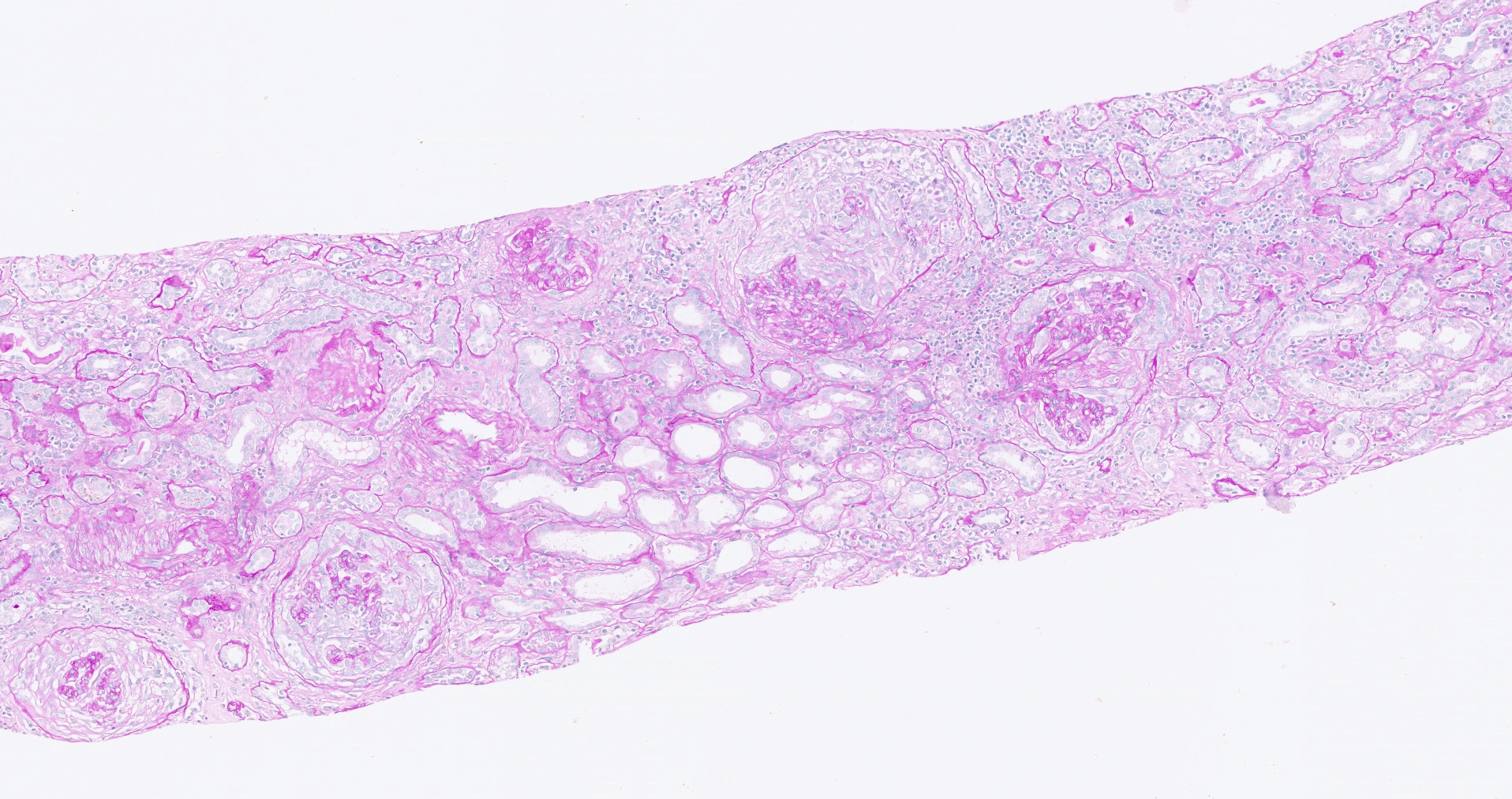
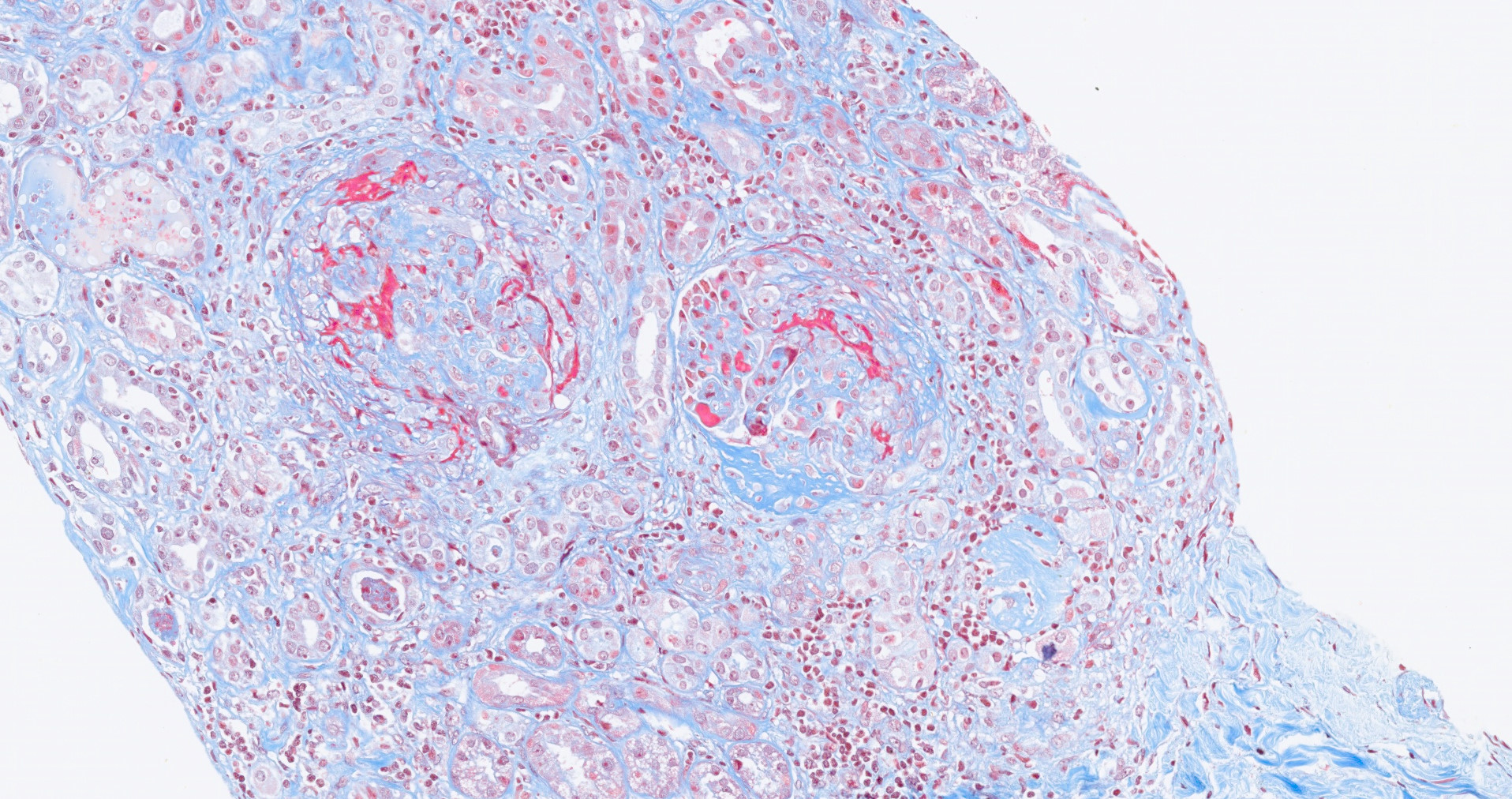
Stains
- Immunohistochemistry not used for diagnosis
- PAS, Jones methenamine silver and trichrome are used to evaluate morphology but are not specific for the type of glomerular disease
Electron microscopy description
- Ultrastructural findings are not specific for anti-GBM disease, showing features of crescentic glomerulonephritis including rupture of the GBM and extracapillary localization of fibrin and proliferating cells
- Electron dense deposits are not seen in isolated anti-GBM disease
Videos
GBM, Alport and anti-GBM
Sample pathology report
- Right kidney, biopsy:
- Anti-glomerular basement membrane glomerulonephritis
- Morphologic pattern:
- Necrotizing and crescentic glomerulonephritis with 85% crescents
- Adequacy:
- Adequate (cortex 80%, medulla 20%)
- Microscopic description:
- 27 glomeruli, 23 of these exhibited cellular crescents, most of them associated with segmental fibrinoid necrosis and/or neutrophilic infiltrate with karyorrhexis. Fibrosis occupies 10% of the interstitium with moderate lymphoplasmacytic infiltrate. Small arteries and arterioles show minimal interstitial fibrosis. There is no vasculitis.
- Immunofluorescence microscopy:
- Number of glomeruli: 3. All glomeruli showed linear IgG staining along the GBM. One glomerulus showed fibrinogen staining.
- Electron microscopy:
- Glomerular capillaries showed neutrophils. Fibrin deposition is present in Bowman space. The glomerular basement membrane showed focal rupture. No electron dense deposits were noted on the glomerular capillary basement membranes or mesangial areas.
Differential diagnosis
- Pauci-immune crescentic glomerulonephritis:
- Lacks strong linear immunoglobulin deposition in GBM
- Presence of fibrocellular to fibrous crescents favors pauciimmune glomerulonephritis
- Immune complex-mediated glomerulonephritis:
- Tends to have more endocapillary cellularity and less necrosis
- Immunofluorescence studies distinguish these types of crescentic glomerulonephritides
- Crescentic glomerulonephritis and anti-GBM glomerulonephritis (concurrent):
- Careful evaluation of immunofluorescence and serologic test for anti-GBM necessary to establish diagnosis
- Diabetic nephropathy:
- Linear immunofluorescence of GBM for albumin and IgG may be noted
- Light microscopy appearances distinguish these types of diseases
- Monoclonal immunoglobulin deposition disease:
- Light chain restricted linear deposits along GBM and tubular basement membrane may be noted
- Cellular crescents rare
Additional references
Board review style question #1
- A 28 year old man has had a decreased urine output over the past 6 days. Urinalysis shows 1+ proteinuria, 4+ hematuria and no glucose or ketones. A renal biopsy is done and the immunofluorescence staining with IgG is shown in the image. Which of the following underlying morphological characteristic is most likely to be present on the renal biopsy?
- Cellular crescents
- Hyaline deposits
- Mesangial hypercellularity and nodules
- Spikes in GBM
- Thrombi in glomerulus
Board review style answer #1
A. Cellular crescents. This is anti-glomerular basement membrane nephritis.
Comment Here
Reference: Anti-GBM nephritis
Comment Here
Reference: Anti-GBM nephritis
Board review style question #2
- Which of the following is true about anti-glomerular basement membrane (GBM) nephritis?
- 90% of patients will have concurrent lung hemorrhage
- It is most common in African Americans
- Necrotizing vasculitis is a frequent finding
- The crescents will typically be of uniform age
- Titers of circulating anti-GBM antibodies correlate with severity
Board review style answer #2