Table of Contents
Definition / general | Terminology | ICD coding | Epidemiology | Etiology | Clinical features | Diagnosis | Laboratory | Prognostic factors | Case reports | Treatment | Microscopic (histologic) description | Microscopic (histologic) images | Negative stains | Immunofluorescence description | Immunofluorescence images | Electron microscopy description | Electron microscopy images | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1Cite this page: Ziadie MS. Fibrillary glomerulonephritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneyfibrillarygn.html. Accessed April 24th, 2024.
Definition / general
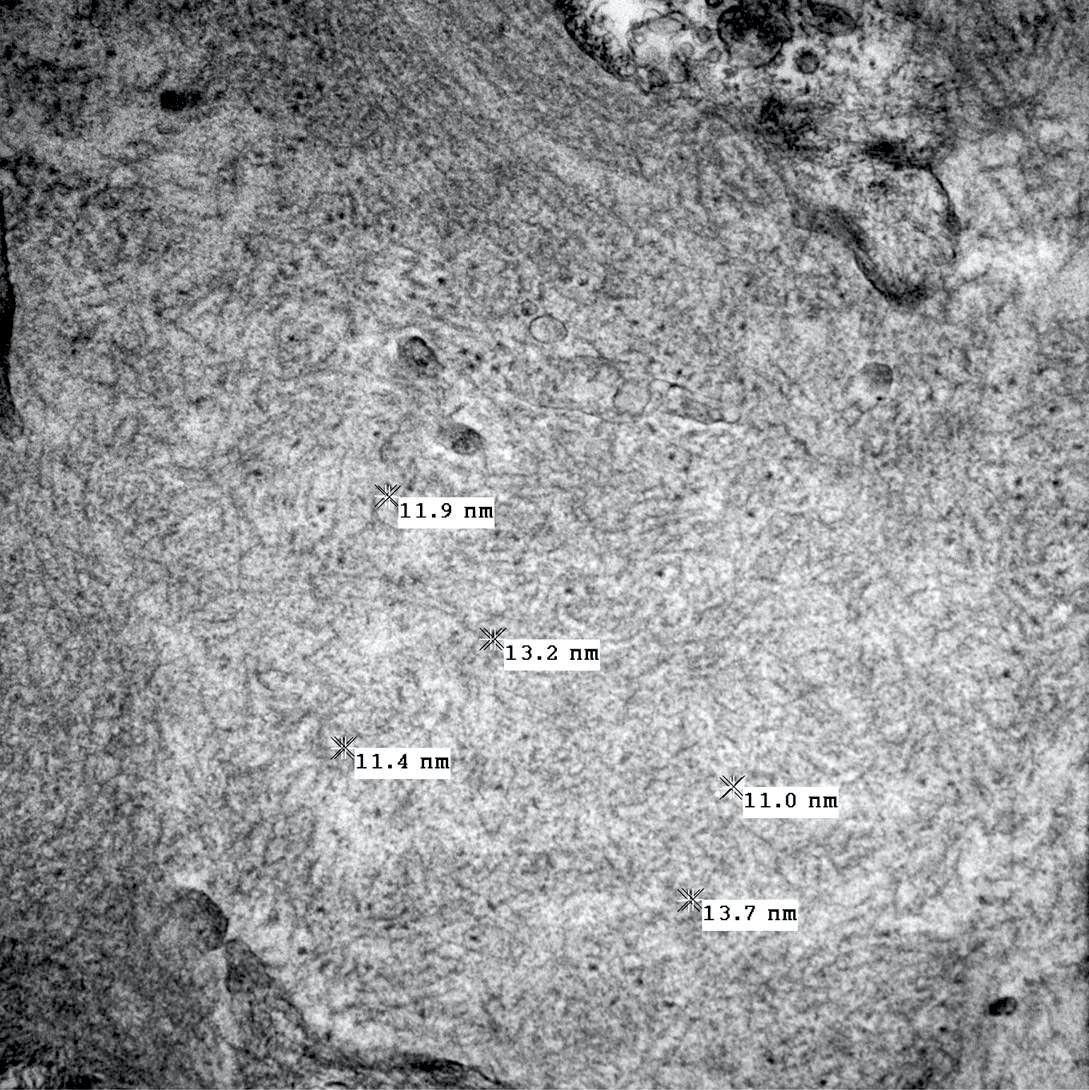
- Glomerular disease characterized by deposition of IgG (usually polytypic) and infiltrative fibrils with a diameter of 12 - 24 nm by electron microscopy
- Most cases (95%) are Congo red negative; rare Congo red positive ones are reported (Am J Kidney Dis 2018;72:325)
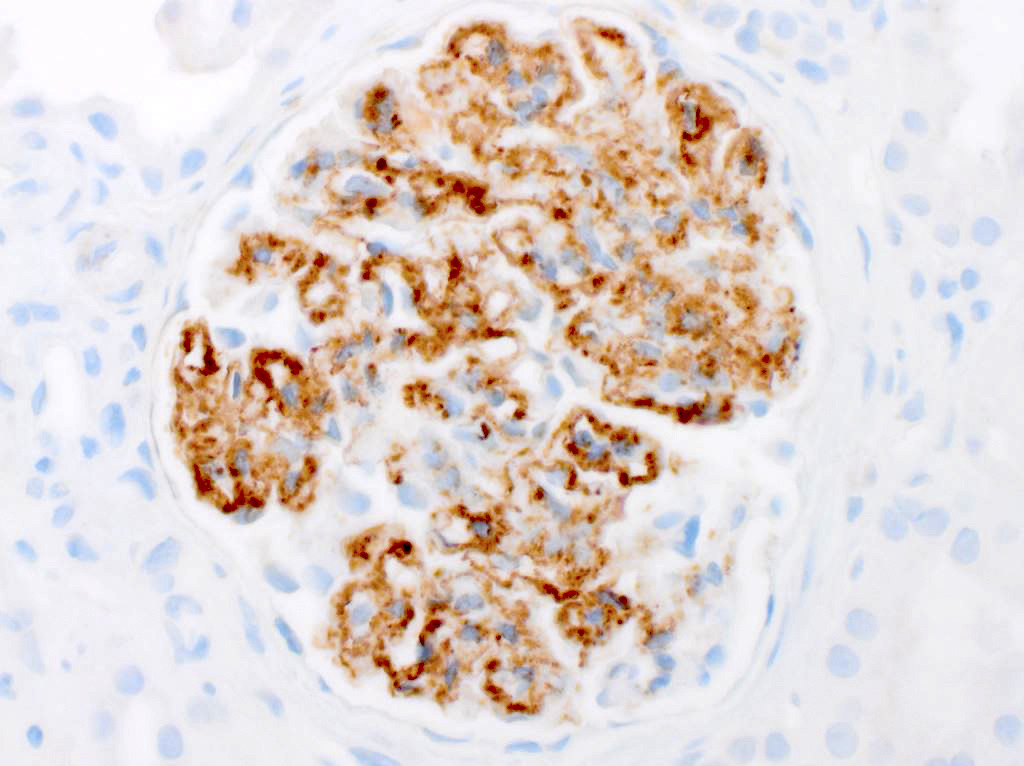
- DNAJB9 has high sensitivity and specificity for fibrillary GN (J Am Soc Nephrol 2018;29:231, J Am Soc Nephrol 2018;29:51, Kidney Int Rep 2017;3:56)
- Extraglomerular immune deposits may be present
Terminology
- Synonym: fibrillary glomerulopathy
- Unacceptable / unfavored terminology: nonamyloid fibrillary glomerulonephritis, Congo red negative amyloidosis-like glomerulopathy
ICD coding
- ICD-10: N05.8 - unspecified nephritic syndrome with other morphologic changes
Epidemiology
- Rare (~1% of native kidney biopsies)
- Affects Caucasians more often than other races with a very slight female predominance
- Presents in mid to late adulthood (mean, fifth decade) (Clin J Am Soc Nephrol 2011;6:775)
Etiology
- Unknown; some authors postulate that the disease is a result of immune complexes that become polymerized into fibrils (J Am Soc Nephrol 2008;19:34)
- Some associations with malignancy (often carcinoma), autoimmune disease, dysproteinemia and infection (including hepatitis C virus) but many cases have no identified underlying disease (Clin J Am Soc Nephrol 2011;6:775)
- Utilizing laser microdissection assisted liquid chromatography – tandem mass spectrometry, investigators at the Mayo Clinic and the University of Washington independently discovered DNAJ homolog subfamily B member 9 (DNAJB9), a proteomic biomarker for fibrillary glomerulonephritis that has been shown to be quite specific for fibrillary glomerulonephritis; the study authors postulate that the DNAJ proteins act as chaperones to heat shock protein 70s, play a role in protein folding or degradation and may be the precursor fibril protein that is misfolded and trapped in the glomeruli (Kidney Int Rep 2017;3:56, J Am Soc Nephrol 2018;29:51, Kidney Int Rep 2017;3:56)
Clinical features
- Virtually all patients present with proteinuria (often in the nephrotic range) and most have evidence of renal insufficiency; more than half have hematuria or hypertension
Diagnosis
- Deposition of IgG (usually polytypic) and infiltrative fibrils with a diameter of 12 - 24 nm by electron microscopy
- Most cases (95%) are Congo red negative; rare Congo red positive ones are reported (Am J Kidney Dis 2018;72:325)
Laboratory
- Laboratory studies show renal insufficiency and normal complement levels
- Serology is usually negative
Prognostic factors
- Poor prognosis; nearly half of patients progress to ESRD within a few years of diagnosis
- Older age, worse renal function at diagnosis and more severe glomerular sclerosis may be predictors of progression to end stage renal disease (Clin J Am Soc Nephrol 2011;6:775)
Case reports
- 46 year old Indian man with HIV (Indian J Pathol Microbiol 2018;61:610)
- 55 year old woman successfully treated by rituximab (J Clin Med 2018;7: E430)
- 66 year old African American man treated with repository corticotrophin injections (Clin Kidney J 2018;11:788)
- 75 year old woman with Sjögren syndrome (Cureus 2018;10:e2483)
- 77 year old Caucasian woman with concurrent thrombotic microangiopathy (Case Rep Nephrol Dial 2018;8:182)
Treatment
- Poor response to therapy including immunosuppression (steroids, cyclophosphamide, cyclosporine) (Clin J Am Soc Nephrol 2011;6:775)
- Use of rituximab shows some promise (Am J Kidney Dis 2008;52:1158, J Clin Med 2018;7:E430)
- Possible use of repository corticotrophin injections (Clin Kidney J 2018;11:788)
- After transplantation, recurrence risk in patients without monoclonal deposits appears low; in addition, recurrence does not appear to always lead to graft loss
Microscopic (histologic) description
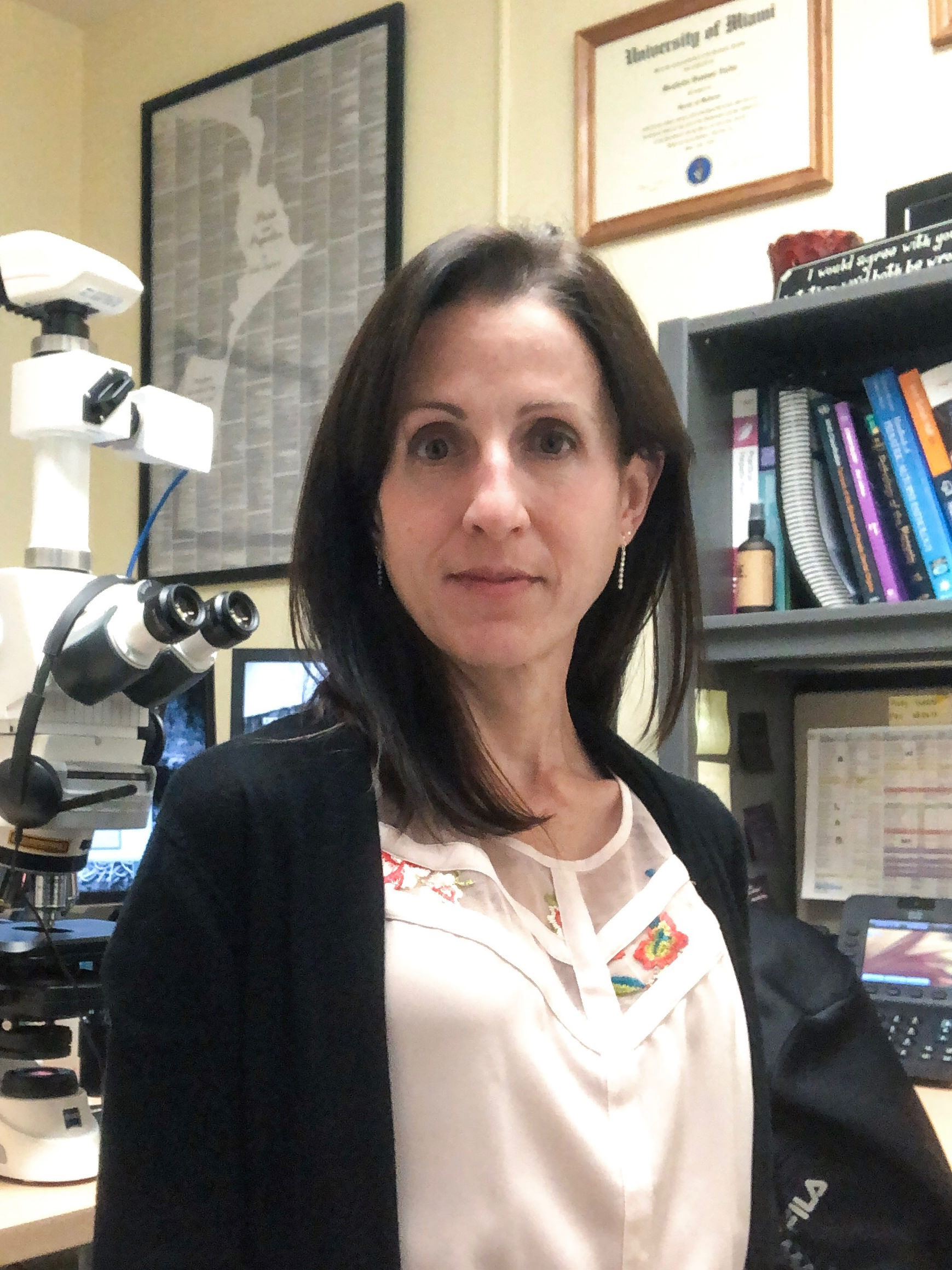
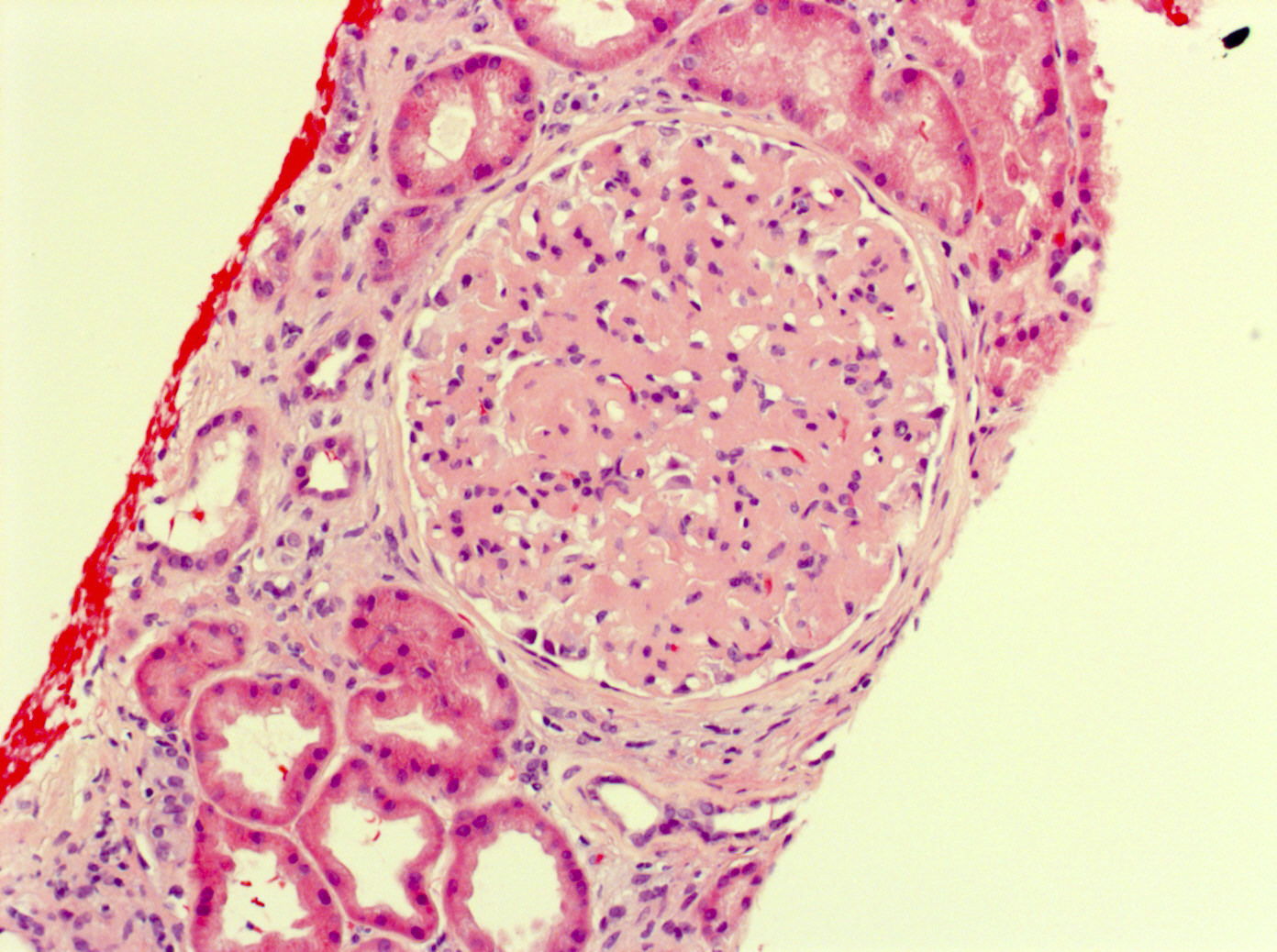
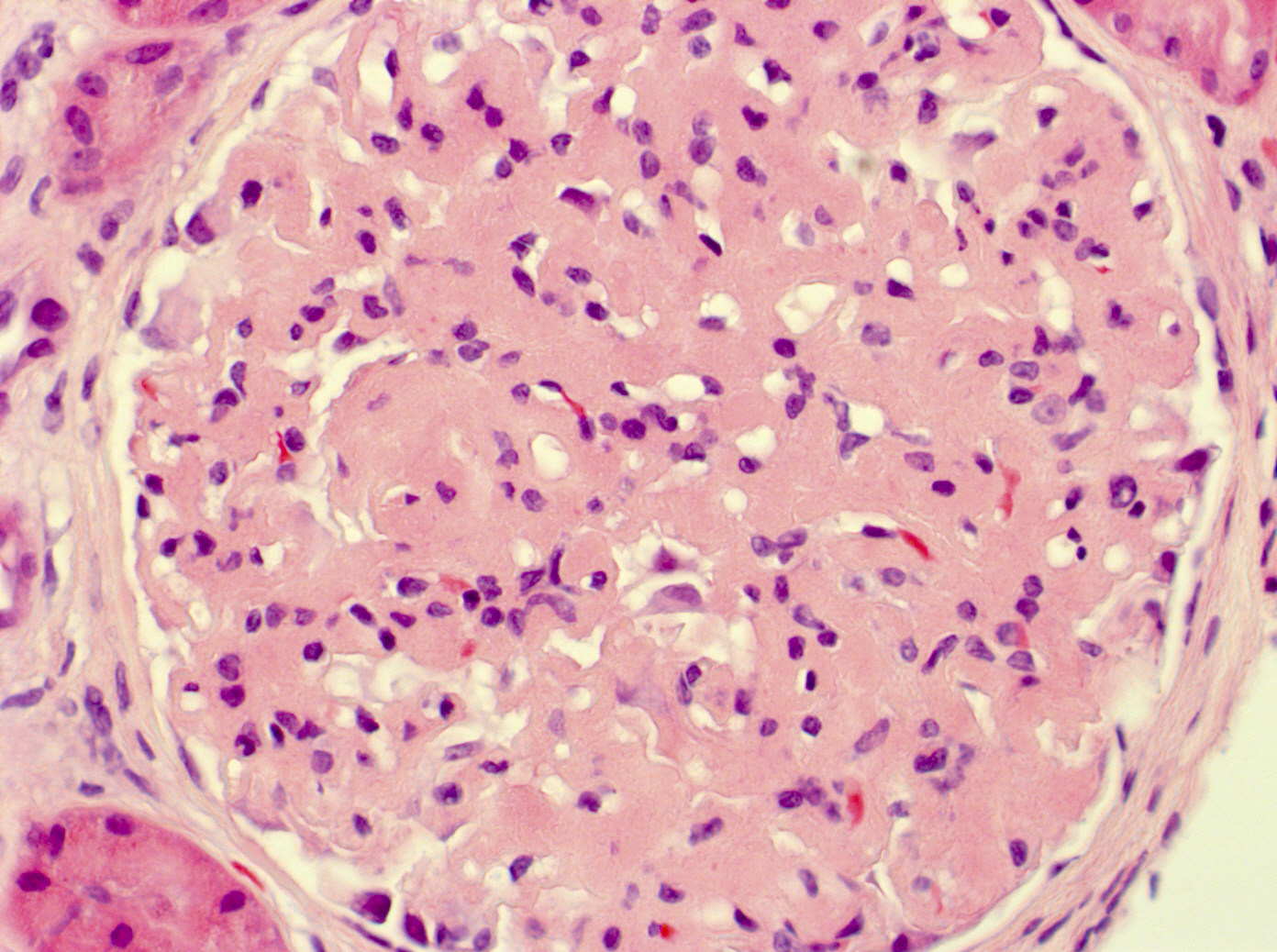
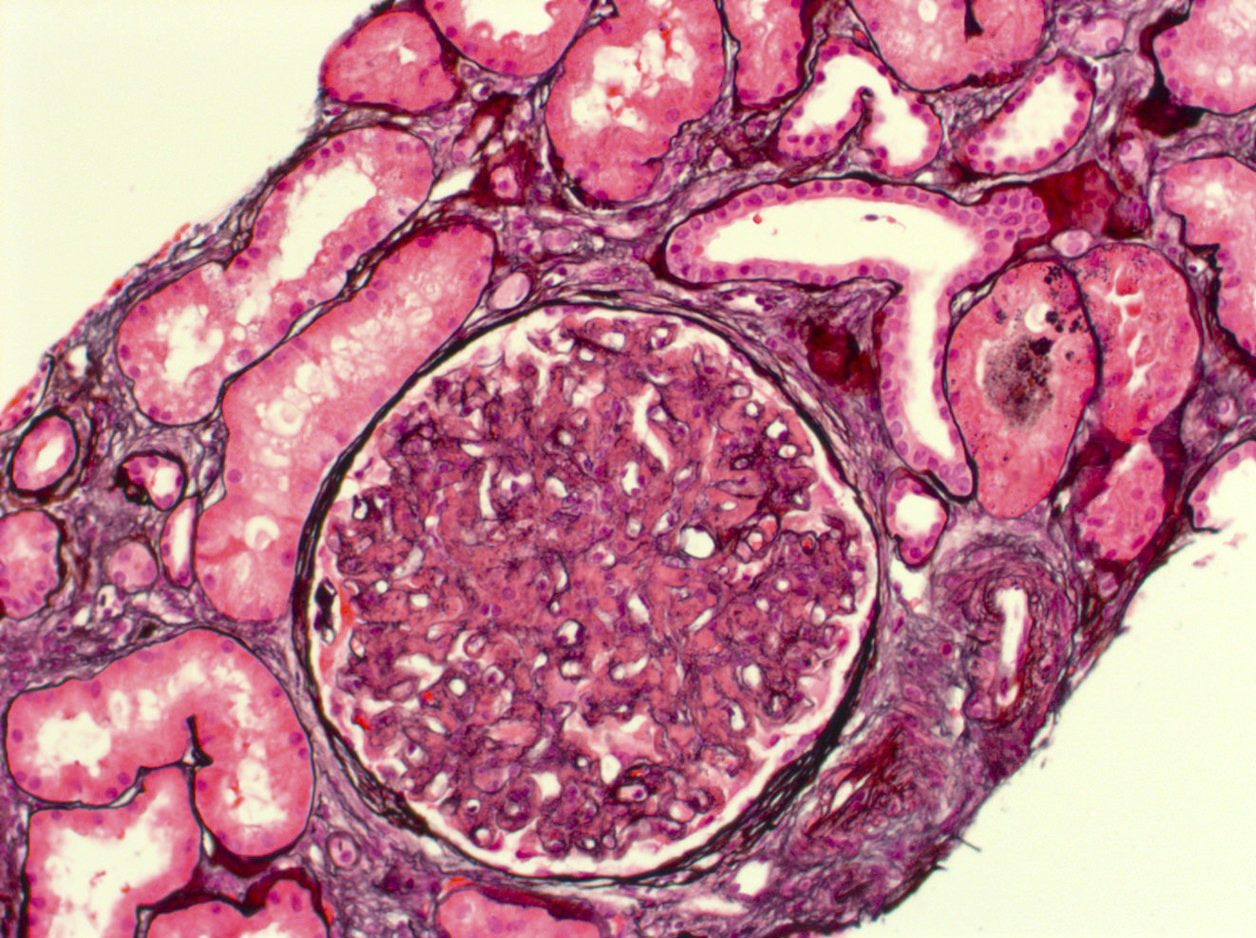
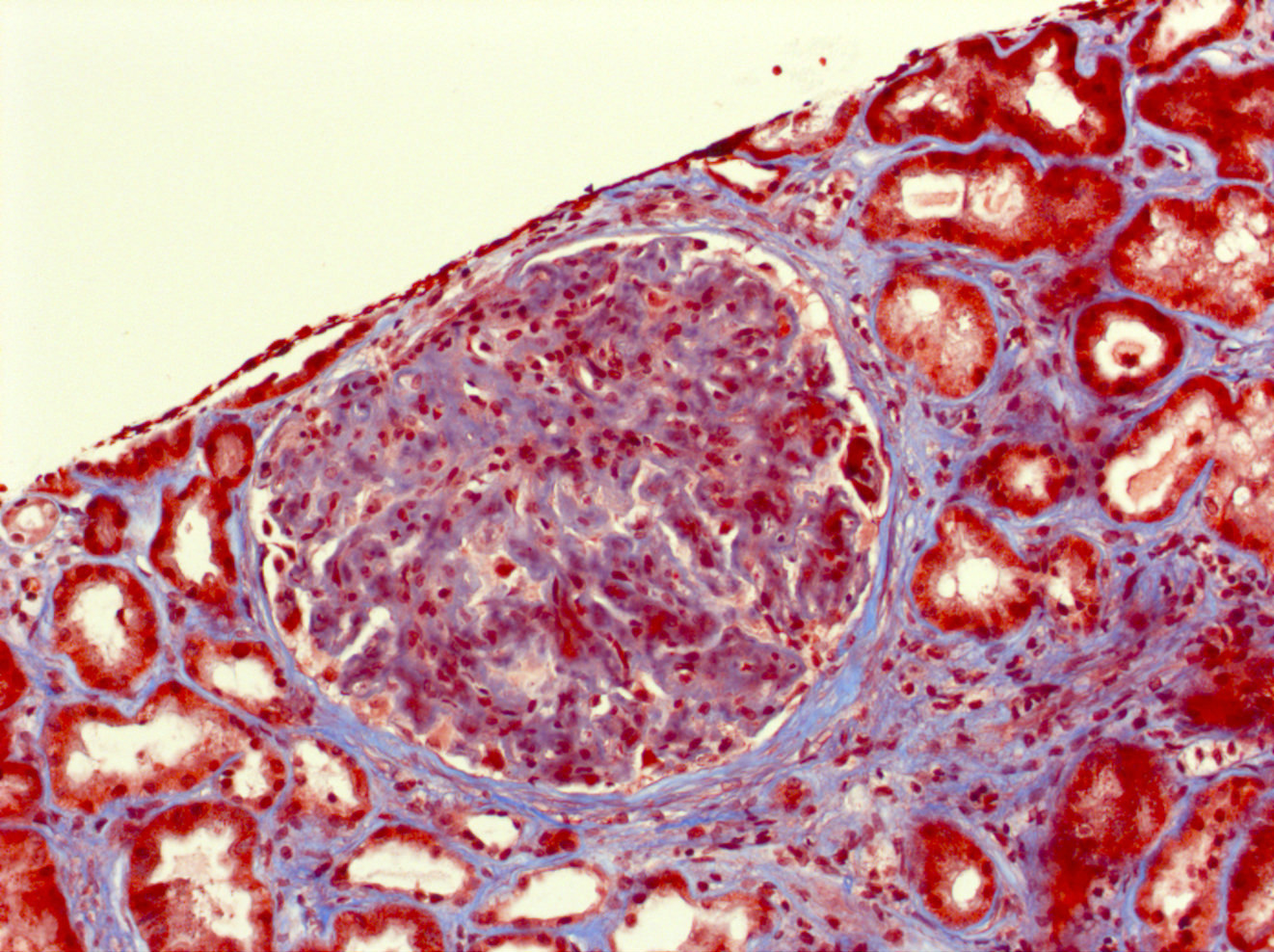
- Most cases exhibit mesangial expansion with variable hypercellularity or sclerosis; there is variability in the degree of glomerular basement membrane duplication (membranoproliferative pattern)
- Smaller subset may demonstrate endocapillary proliferation, crescentic glomerulonephritis or necrosis (Clin J Am Soc Nephrol 2011;6:775)
Microscopic (histologic) images
Contributed by Mandolin S. Ziadie, M.D. and Nicole K. Andeen, M.D.
Images hosted on other servers:
Negative stains
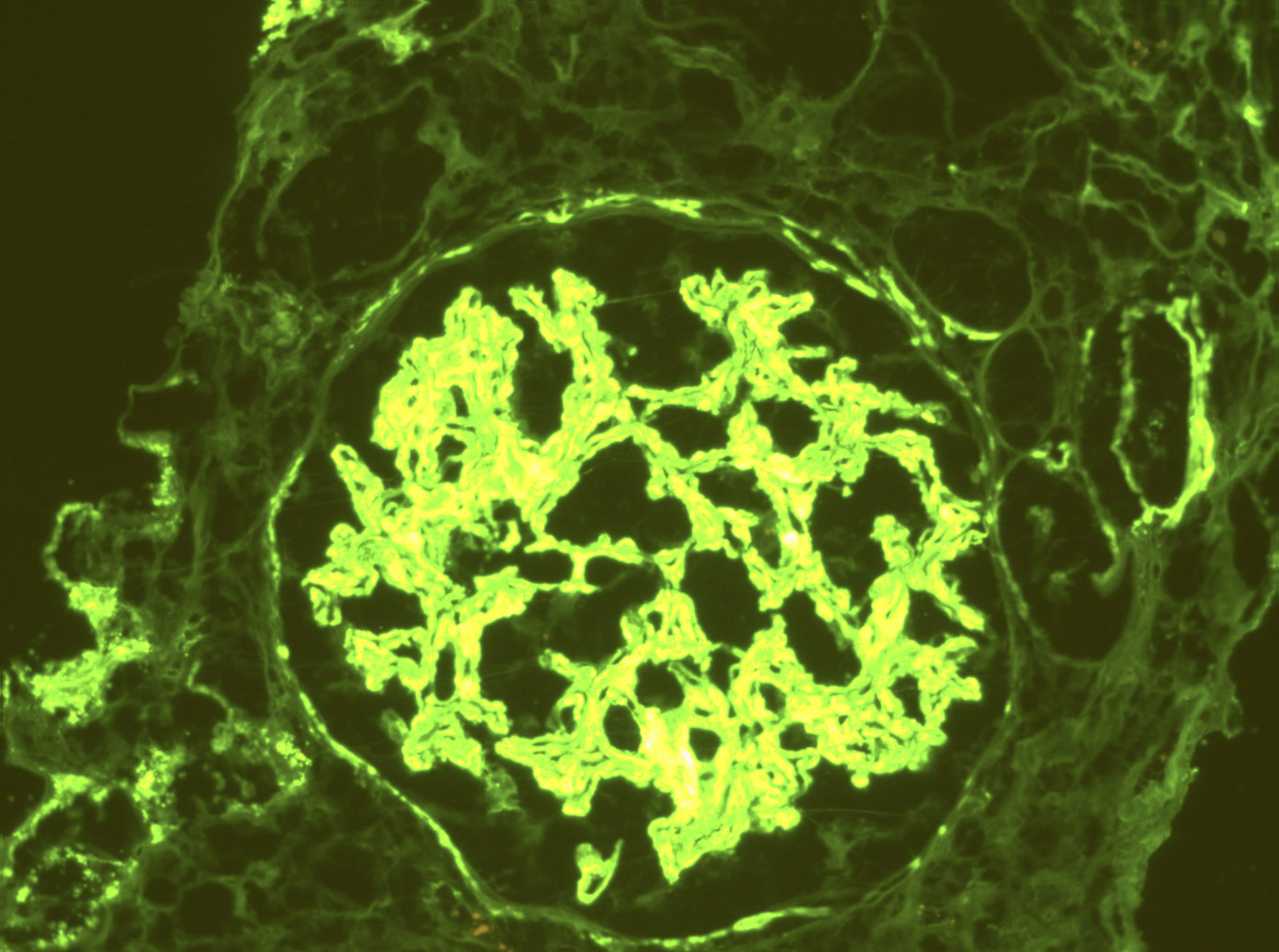
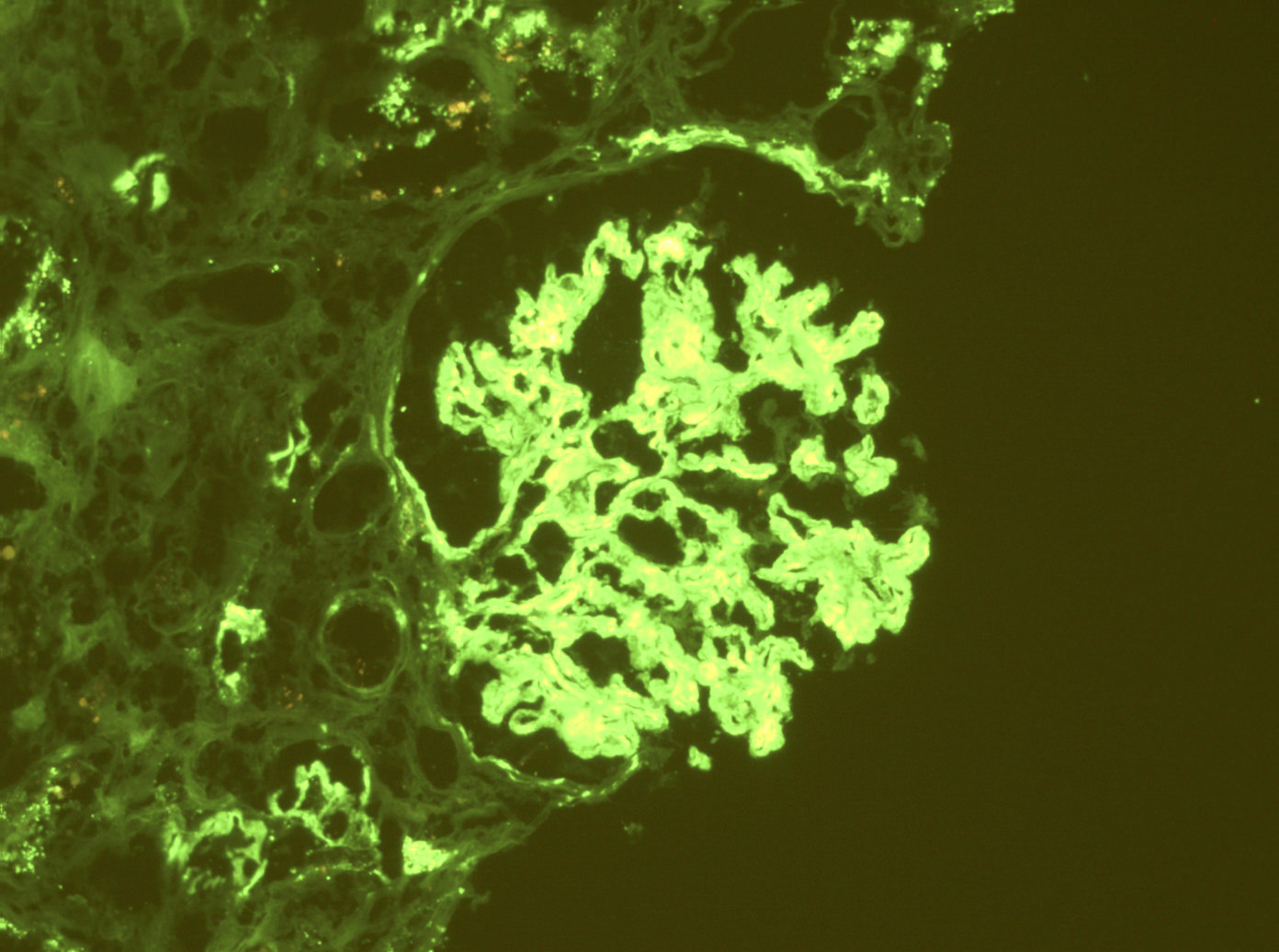
Immunofluorescence description
- Mesangial and variable capillary wall staining for polyclonal IgG and C3 is most common; in a small number of patients, light chain restriction (usually kappa) is seen (J Am Soc Nephrol 2008;19:34)
Immunofluorescence images
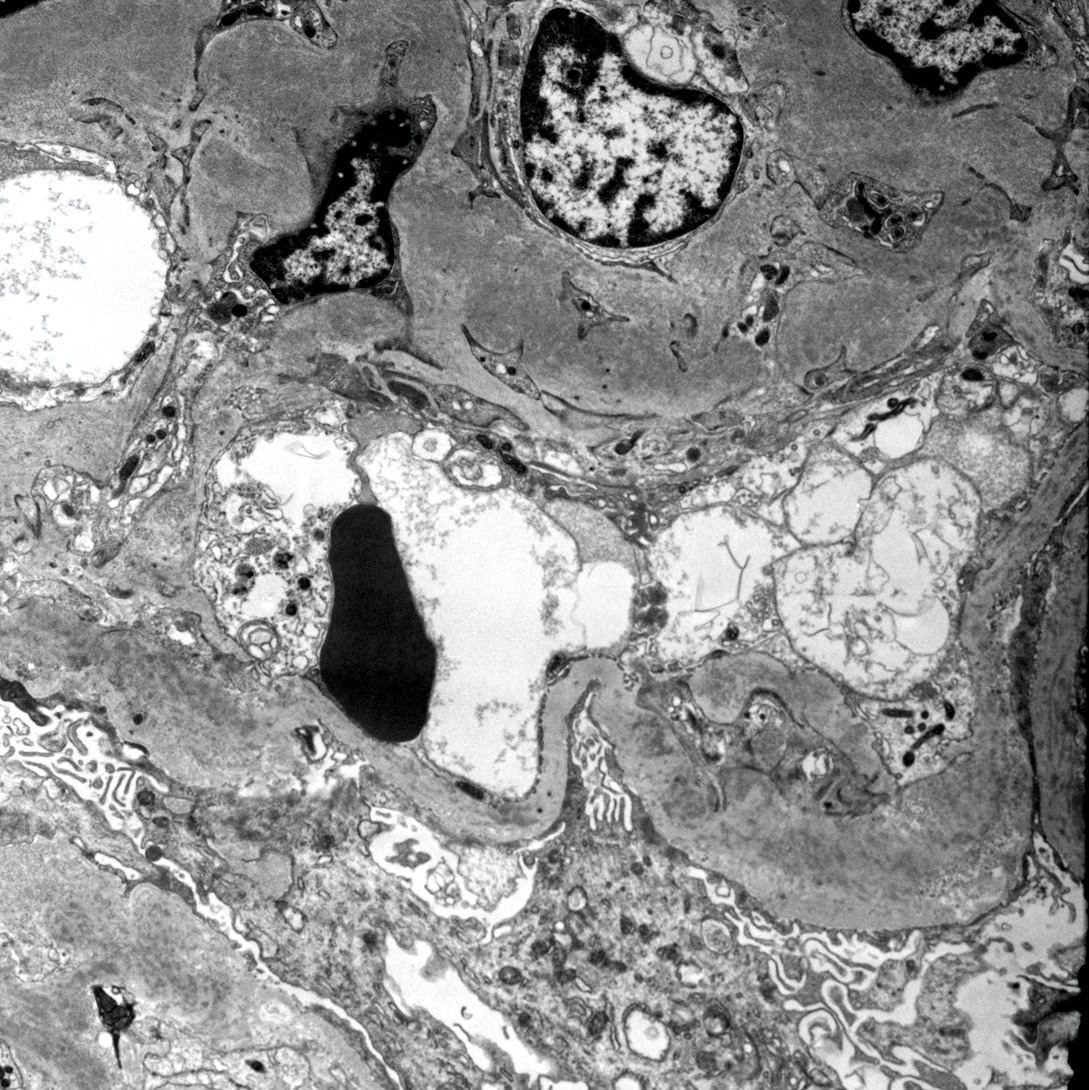
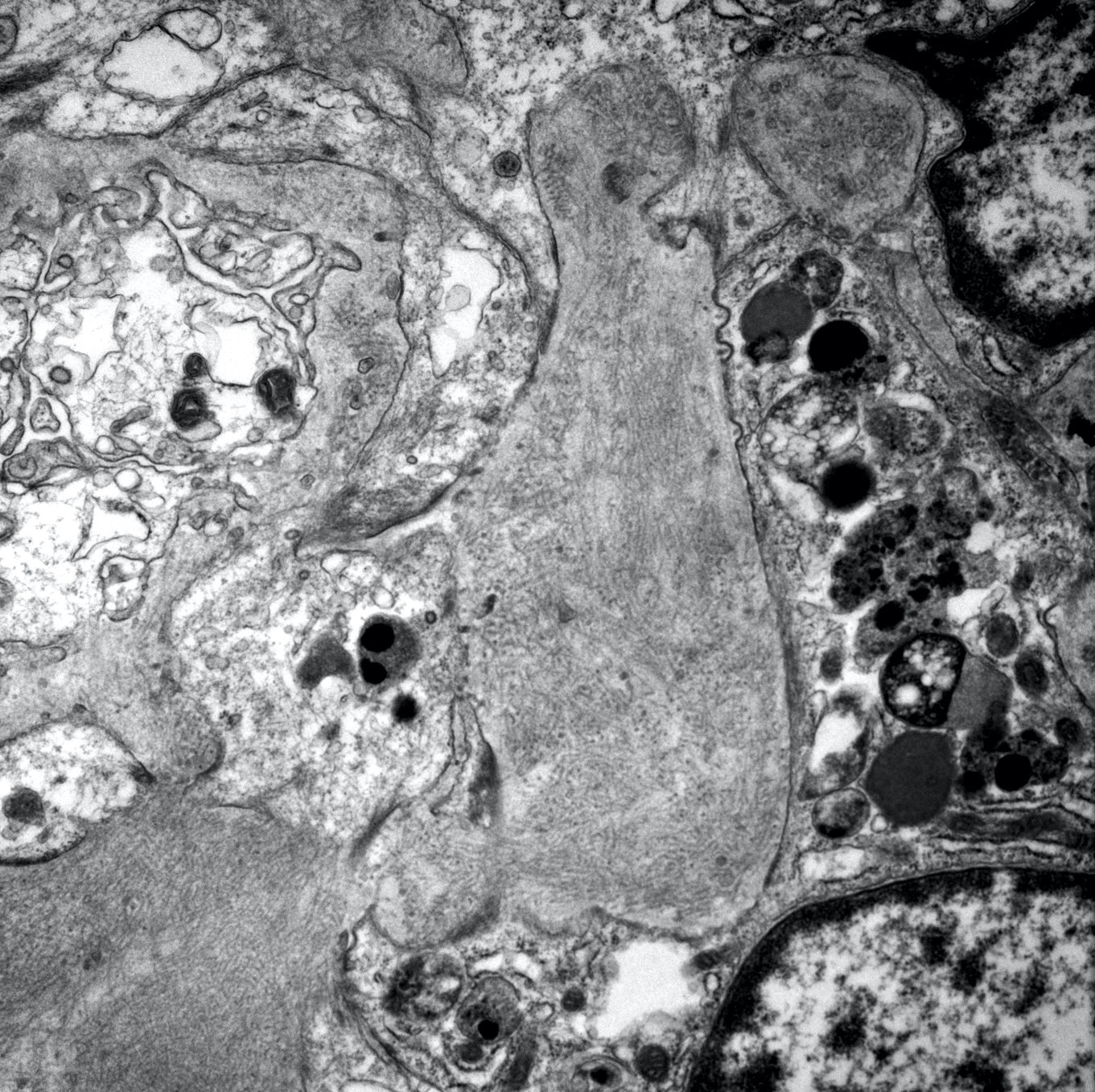
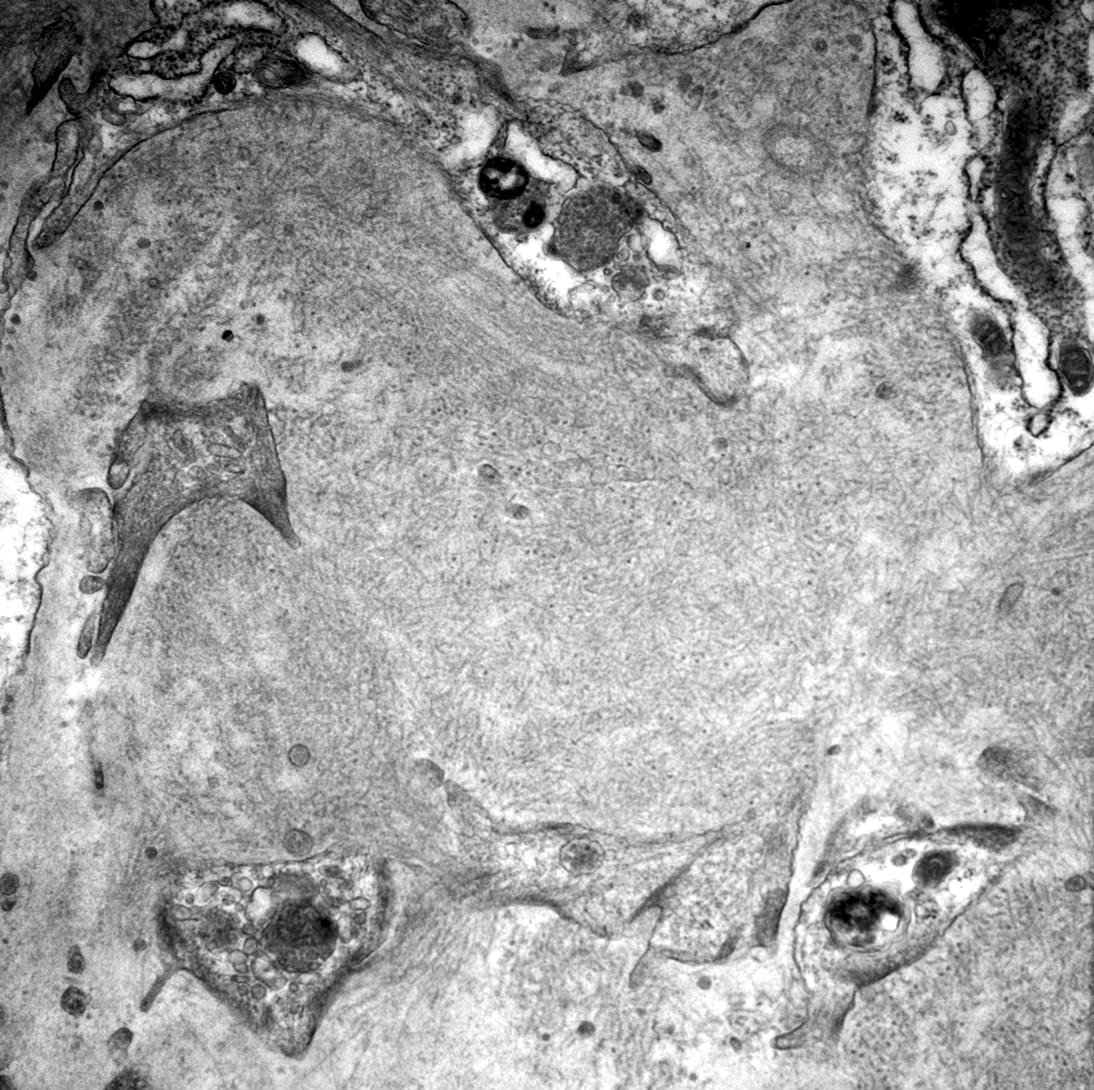
Electron microscopy description
- Mesangial and variable capillary wall deposits of randomly organized fibrils that range from 10 - 30 nm in diameter (J Am Soc Nephrol 2008;19:34)
Electron microscopy images
Differential diagnosis
- Amyloidosis: Congo red positivity in deposits with smaller (8 - 12 nm) fibrils on electron microscopy, light chain (kappa or lambda) restriction (AL amyloidosis) or immunoglobulin (IgG, IgA or IgM) restriction (AH amyloidosis) on immunofluorescence, negative DNAJB9 immunohistochemistry, positive Amyloid A protein on immunohistochemistry (AA amyloidosis)
- Immunotactoid glomerulopathy: microtubular substructure of deposits that are larger (30 - 50 nm), IgG1 predominance on immunofluorescence with light chain restriction and C3 staining, negative for DNAJB9 on immunohistochemistry
- Cryoglobulinemic glomerulonephritis: serum cryoglobulin tests positive, "pseudothrombi" in glomerular capillaries, granular subendothelial / mesangial deposits and thrombi positive for IgM, IgG and C3 with equivalent light chains (Type II) or with light and heavy chain restriction, usually IgG and kappa (Type I), negative DNAJB9 staining
- Fibronectin glomerulopathy: deposits are strongly PAS+ with negative standard immunofluorescent studies in most cases, strong positivity for fibronectin, negative DNAJB9 staining, positive family history
Additional references
Board review style question #1
A patient presents with nephrotic range proteinuria with normal serology. Assays for cryoglobulin are negative. A kidney biopsy is performed, showing mesangial expansion by Congo red negative material that is brightly positive for IgG (polyclonal) and c3. Electron microscopy reveals randomly arranged fibrils within the glomerular mesangium and focally within the basement membrane. The fibrils measure 13 - 16 nm in diameter. What is the best diagnosis?
- Amyloidosis
- Fibrillary glomerulonephritis
- Fibronectin glomerulopathy
- Immunotactoid glomerulopathy
Board review style answer #1