Table of Contents
Definition / general | Essential features | Clinical features | Case reports | Microscopic (histologic) images | Sample pathology report | Differential diagnosis | Type I: classical | Type II: dense deposit | Type III: mixed | Type III: Anders-Strife variant | Type III: Burkholder variant | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Zhang H. MPGN pattern of injury. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneymembranoprolif.html. Accessed April 19th, 2024.
Definition / general
- Also called hypocomplementemic, lobular or mesangiocapillary glomerulonephritis
- Histologic lesion, not a specific disease entity
- MPGN should be diagnosed with specific etiology or underlying cause (such as C3GN, immune complex mediated, monoclonal), not as types I - III (Kidney Int 2012;81:434, N Engl J Med 2012;366:1119)
Essential features
- A morphologic pattern of glomerular injury, characterized by endocapillary and mesangial hypercellularity, mesangial and subendothelial deposits and duplicating of glomerular basement membrane
- Idiopathic membranoproliferative glomerulonephritis (MPGN) thought to be a diagnosis of exclusion
Clinical features
- Either immunoglobulin (polyclonal or monoclonal) mediated or complement mediated
- Immunoglobulin mediated: due to infections, autoimmune diseases, paraproteinemias
- Complement mediated: dysregulation of alternative pathway due to genetic or acquired abnormalities in regulatory factors
- Traditional classification based on electron microscopy findings: MPGN type I (subendothelial and mesangial deposits), MPGN II (intramembranous dense ribbon-like deposits) and MPGN III (subendothelial and subepithelial deposits)
- Newer classification based on immunofluorescence emphasizing pathophysiology: immune complex / monoclonal immunoglobulin mediated MPGN (activation of classic complement pathway) and C3 glomerulopathies (including dense deposit disease, C3 glomerulonephritis and CFHR5 nephropathy, activation of alternate complement pathway)
- MPGN lesion due to immune complex now referred to simply as MPGN
- Poor prognostic signs including nephrotic syndrome, an elevated serum creatinine and hypertension at presentation, crescents and tubulointerstitial disease on biopsy
Case reports
- 28 year old woman with fever, weight gain of 13 kilograms, lower extremity edema, hepatosplenomegaly and multicentric peripheral lymphadenopathy (Front Immunol 2019;10:1489)
- 46 year old Chinese man presented with bilateral tumor-like nodules (Ren Fail 2019;41:126)
Sample pathology report
- Left kidney, native, needle core biopsy:
- Immune complex mediated membranoproliferative glomerulonephritis (type I) (see comment)
- Cellular / fibrocellular crescent (4/15), fibrous crescents (0/15)
- Global glomerulosclerosis (1/15), segmental glomerulosclerosis (0/15)
- Interstitial fibrosis with tubular atrophy and interstitial fibrosis, mild
- Arteriosclerosis, mild
- Comment: Light microscopy shows glomeruli with diffuse endocapillary hypercellularity and focal cellular crescents. Indirect immunofluorescence studies show diffuse global capillary granular staining of IgG (3+) and C3 (2+) with polyclonal light chain expression and negative staining for IgA, IgM and C1q. Electronic microscopic examination shows subendothelial, mesangial electron dense deposits and mesangial interpositioning. The findings are consistent with type I MPGN. The patient is a young male with no history of infections, autoimmune diseases, paraproteinemias or other known causes of MPGN. An idiopathic MPGN is favored at this point.
Differential diagnosis
- C3 glomerulopathy:
- Abnormal control of complement activation, deposition or degradation and characterized by predominant glomerular C3 fragment deposition (C3c intensity ≥ 2 orders of magnitude more than any other immune reactant) with electron dense deposits on electron microscopy
- Overlapping with type I and III MPGN (Kidney Int 2013;84:1079)
- Thrombotic microangiopathy (TMA):
- MPGN pattern injury with no immunoglobulins or complements by immunofluorescence or electron microscopy, commonly seen in the chronic phase
Type I: classical
Definition / general
Case reports
Treatment
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Haiyan Zhang, M.D., Ph.D.
Contributed by Nephropath
Immunofluorescence description
Immunofluorescence images
Contributed by Haiyan Zhang, M.D., Ph.D. and Nephropath
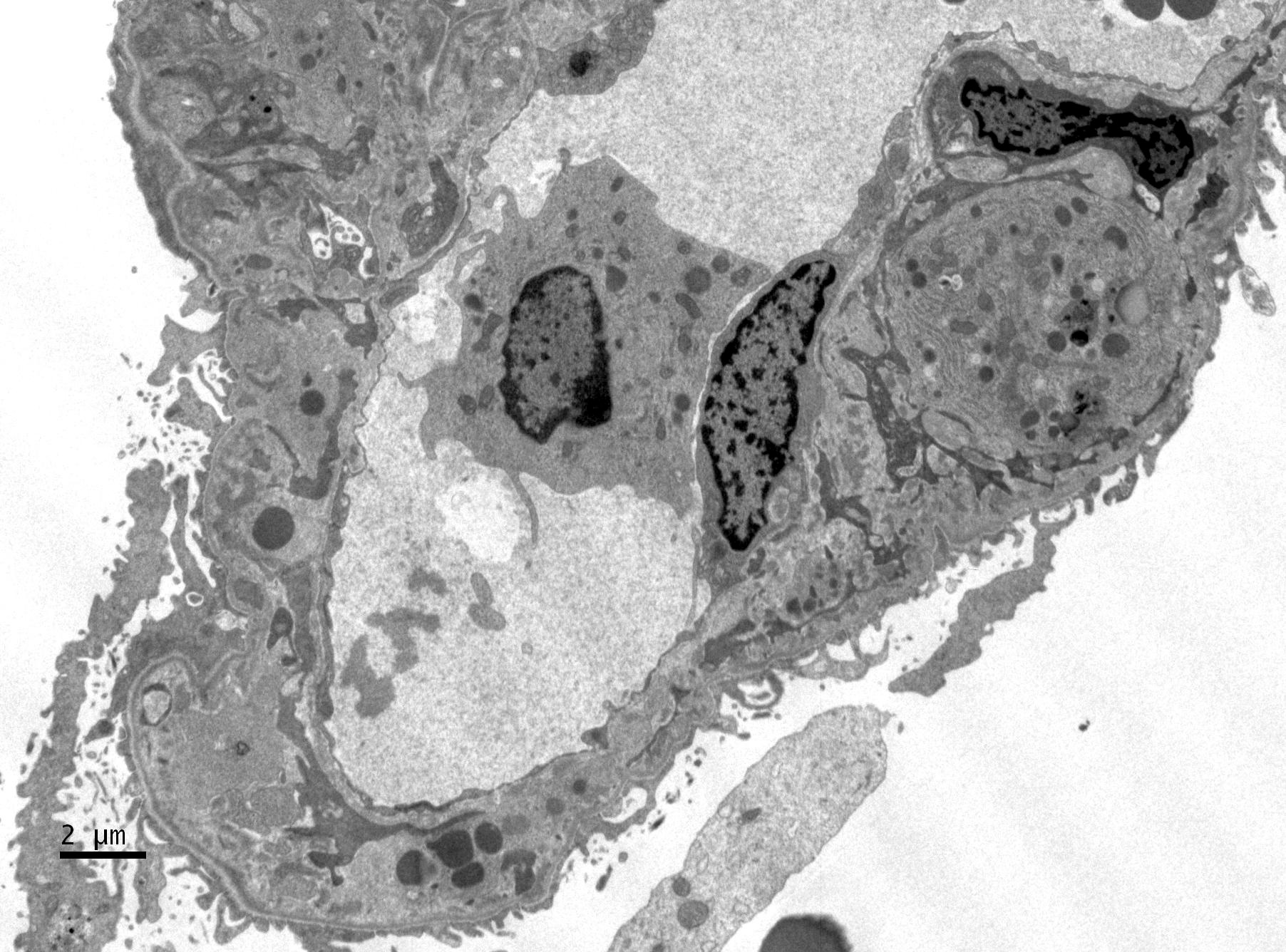
Electron microscopy description
Electron microscopy images
Contributed by Haiyan Zhang, M.D., Ph.D. and Nephropath
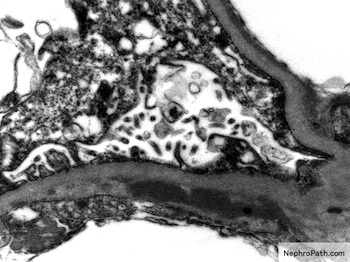
- MPGN pattern of injury with discrete subendothelial and mesangial electron dense deposits
- Mostly immune complex deposition indicating aviation of classic complement pathway and some alternative complement pathway (overlaps with C3 glomerulonephritis)
- Distinguished from new category of C3 glomerulopathies by prominent Ig or C1q
- Primary MPGN mostly affecting adolescents and young adults
- > 50% with nephrotic syndrome
- 10 - 20% with acute nephritis syndrome
- ~50% with low C3
- May be secondary to chronic infections (e.g. hepatitis C), autoimmune diseases (e.g. SLE), paraproteinemias, alpha-1-antitrypsin deficiency and malignancies
- ~50% renal survival at 10 years
- Recurs in ~30% of children 6 - 12 months after transplantation
- MPGN due to a monoclonal gammopathy or complement mediated disease with a higher risk of graft recurrence than immune complex mediated MPGN secondary to infection or autoimmune disease
Case reports
- 5 year old girl with selective IgA deficiency and MPGN (BMC Nephrol 2020;21:68)
- 43 year old woman with recurrent membranoproliferative glomerulonephritis after kidney transplantation due to ventriculoatrial shunt infection (BMC Nephrol 2019;20:296)
Treatment
- Most patients with immune complex mediated MPGN have an identifiable underlying cause, such as a chronic infection, autoimmune disease or monoclonal gammopathy
- Such patients should receive therapy directed against the underlying cause of the MPGN, since resolution of the MPGN usually occurs after successful treatment of the primary disease
- For idiopathic MPGN, patients with mild disease may need only conservative therapy with antihypertensive or antiproteinuric regimens
- Patients with heavy proteinuria (> 3 grams/day) or nephrotic syndrome, immunosuppressive therapy in addition to conservative therapy is suggested, such as glucocorticoids and calcineurin inhibitors
- Patients presenting with a rapidly progressive crescentic MPGN should receive immunosuppressive therapy without delay, since they are at high risk for progression to end stage kidney disease if untreated
- We treat such patients with pulse IV methylprednisolone followed by daily oral prednisone and cyclophosphamide (Kidney Int 2020;98:1135)
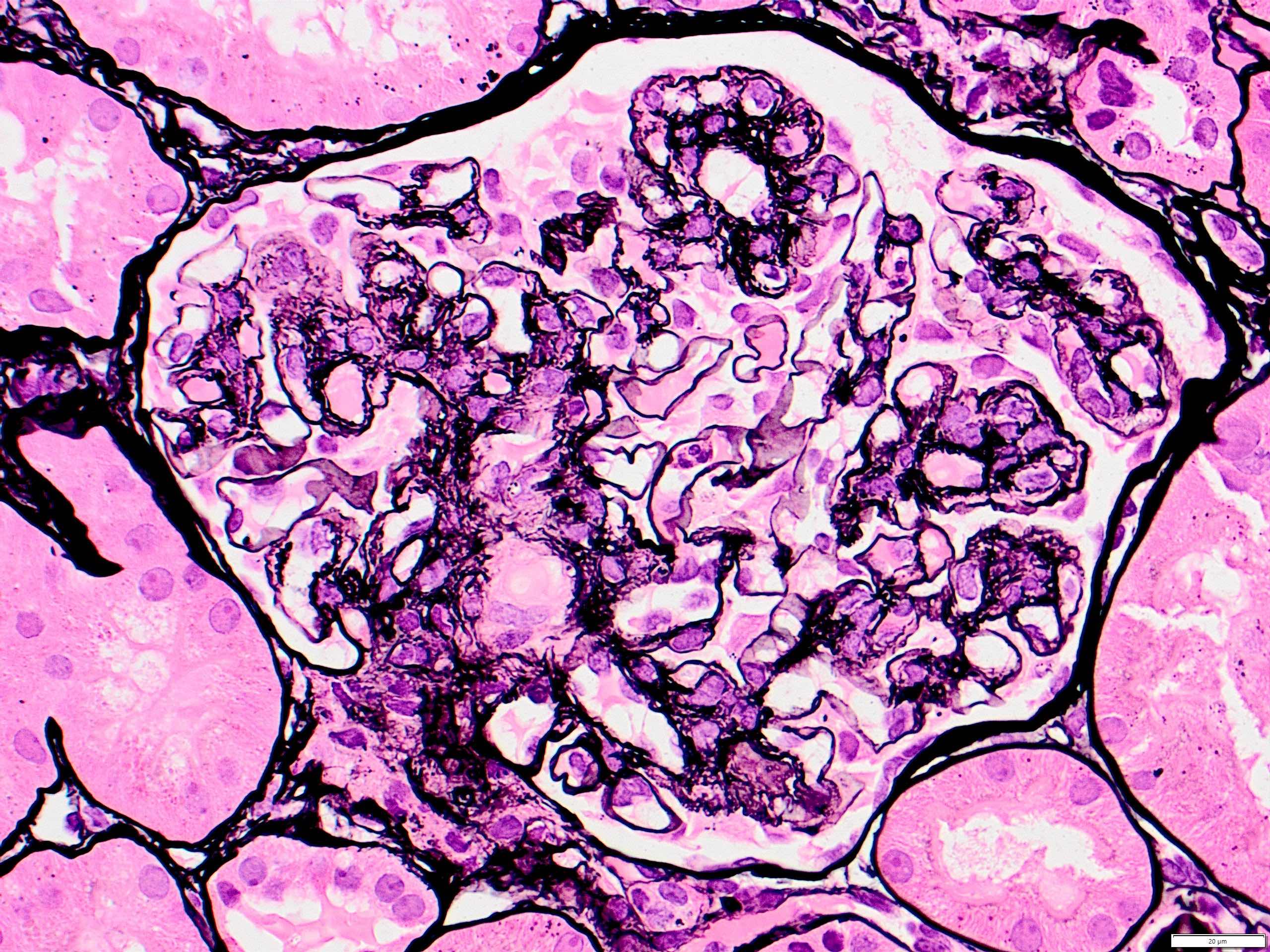
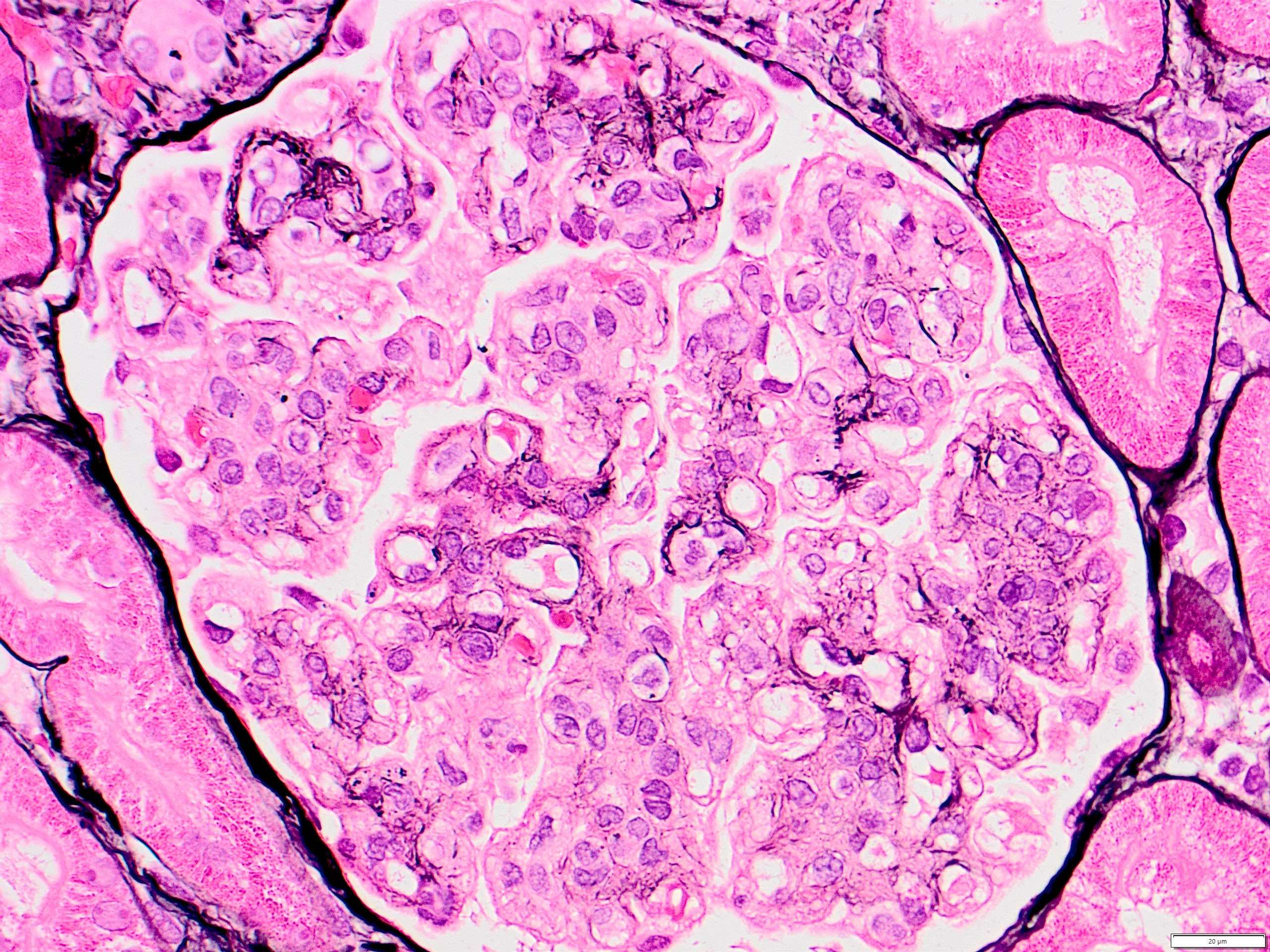
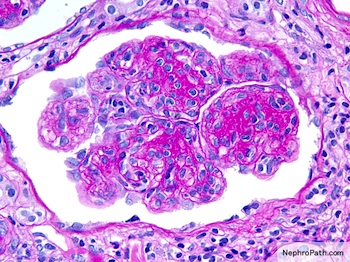
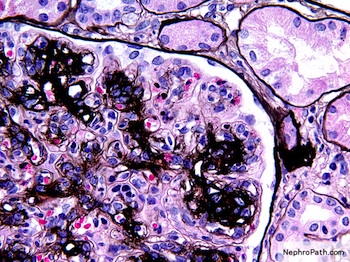
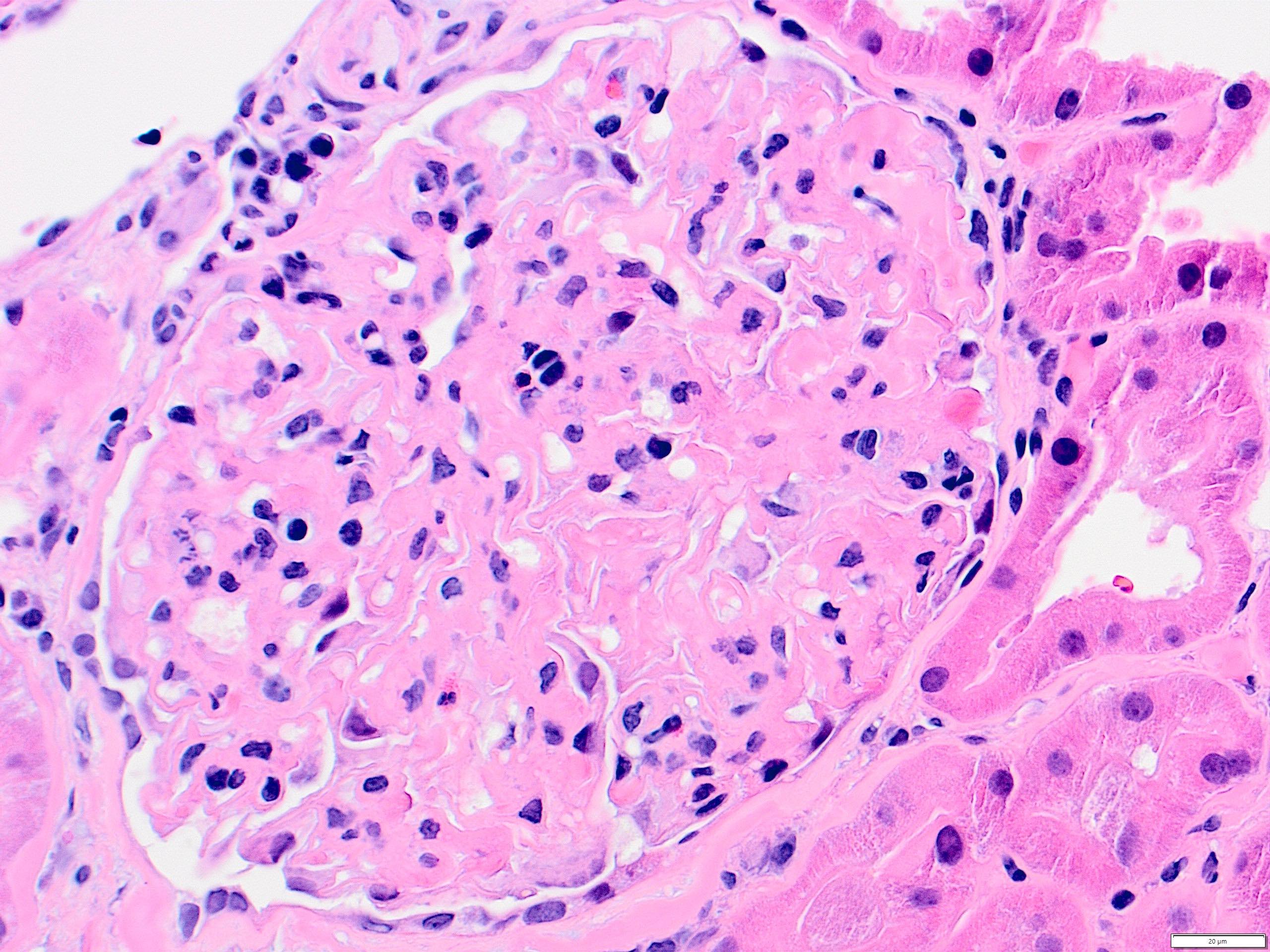
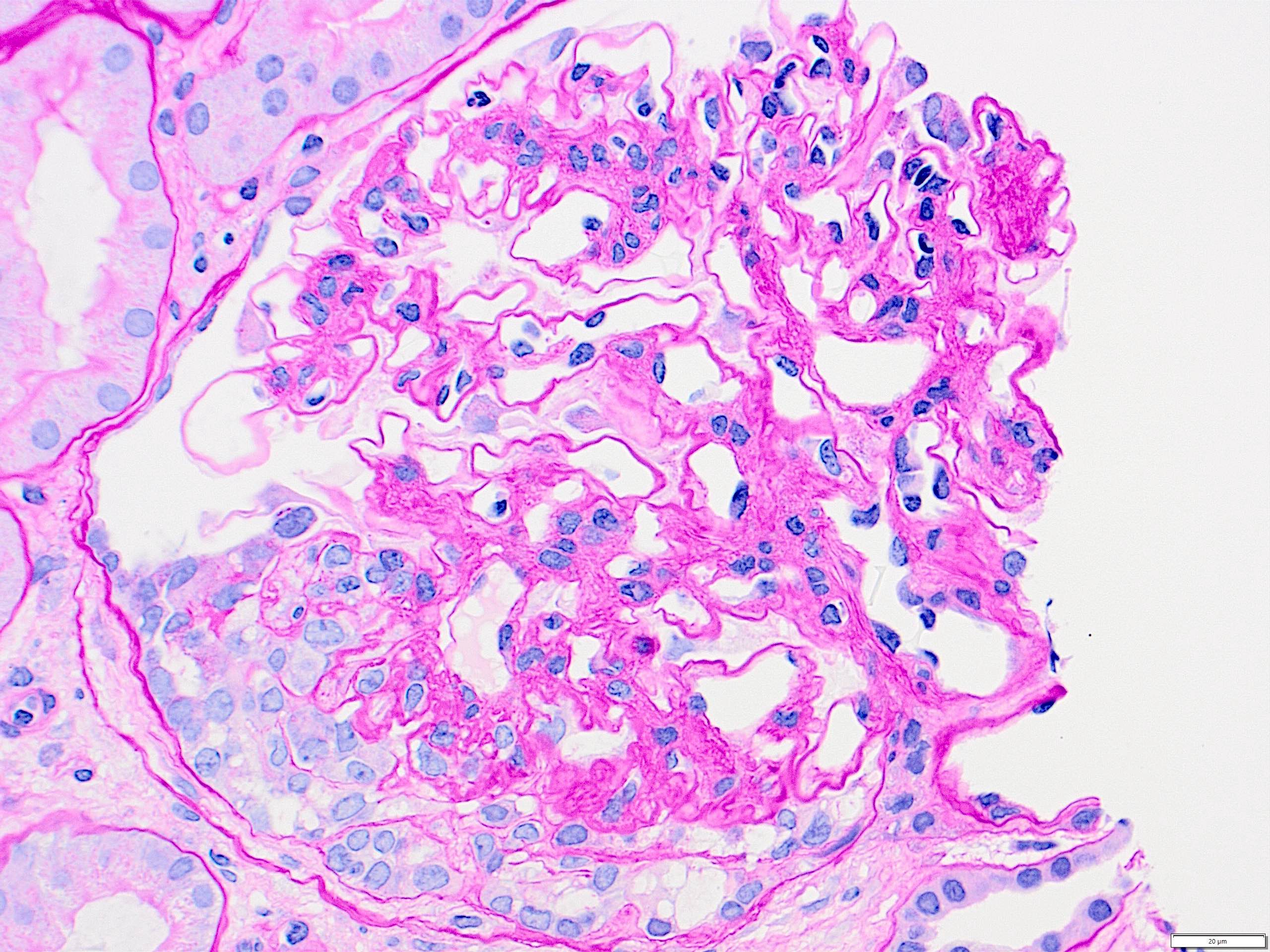
Microscopic (histologic) description
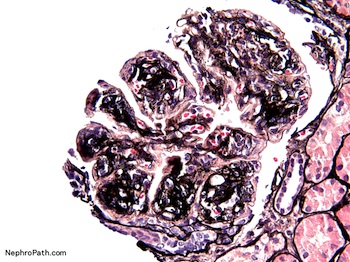
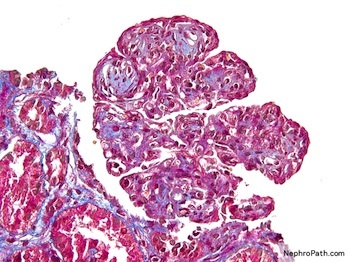
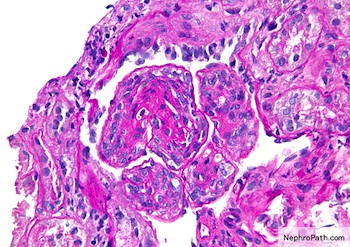
- Mesangial and endocapillary hypercellularity with lobular accentuation
- Irregular thickening of glomerular basement membrane by interposition of mesangial cells between endothelium and basement membrane
- Forming double contour / tram track appearance (PAS or silver stain)
- Crescents in ~20% cases
- Neutrophils (exudate) may present
- May have immune complex aggregates forming hyaline thrombi in capillary lumina
- Reference: Nat Rev Nephrol 2015;11:14
Microscopic (histologic) images
Contributed by Haiyan Zhang, M.D., Ph.D.
Contributed by Nephropath
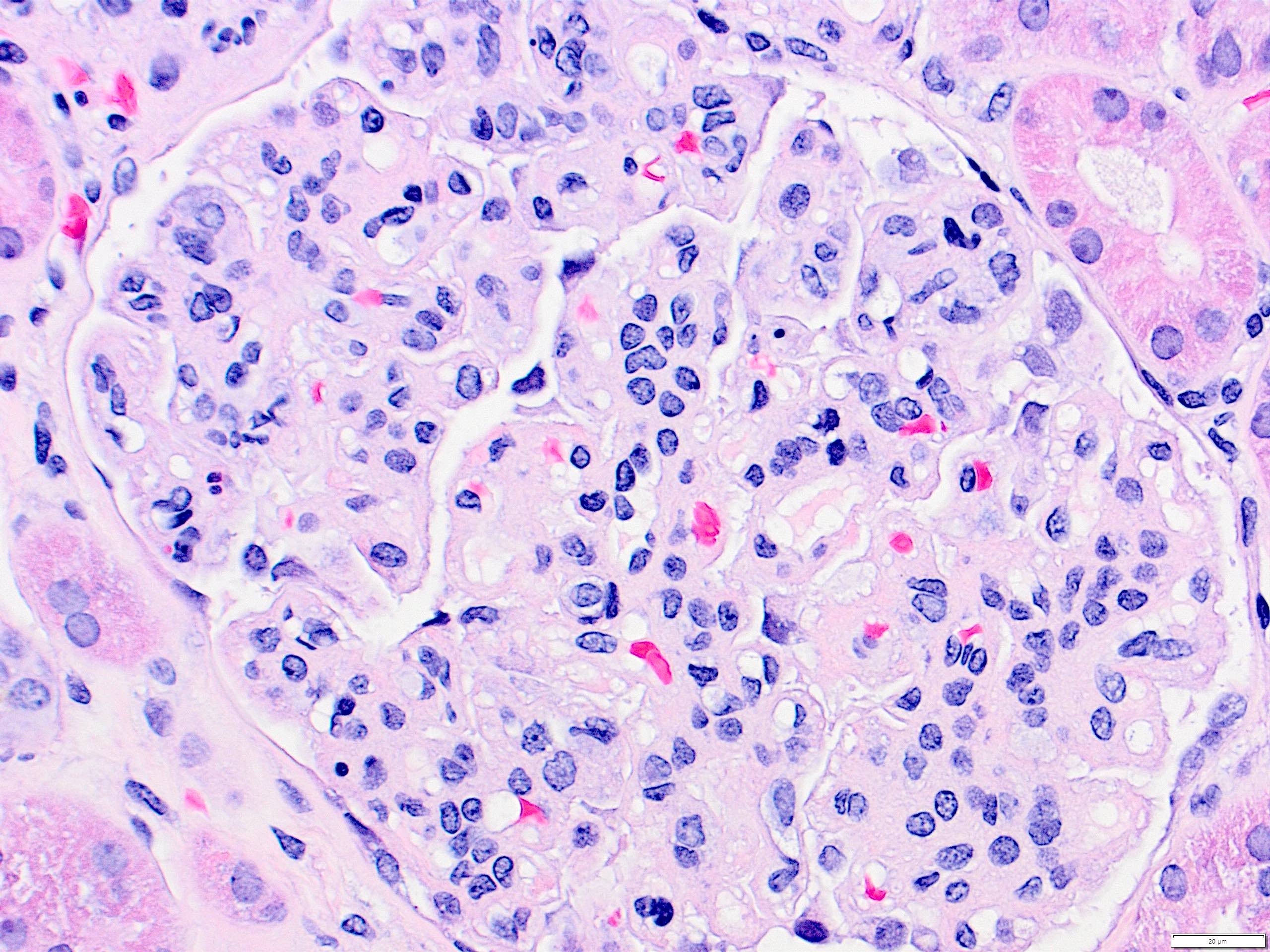
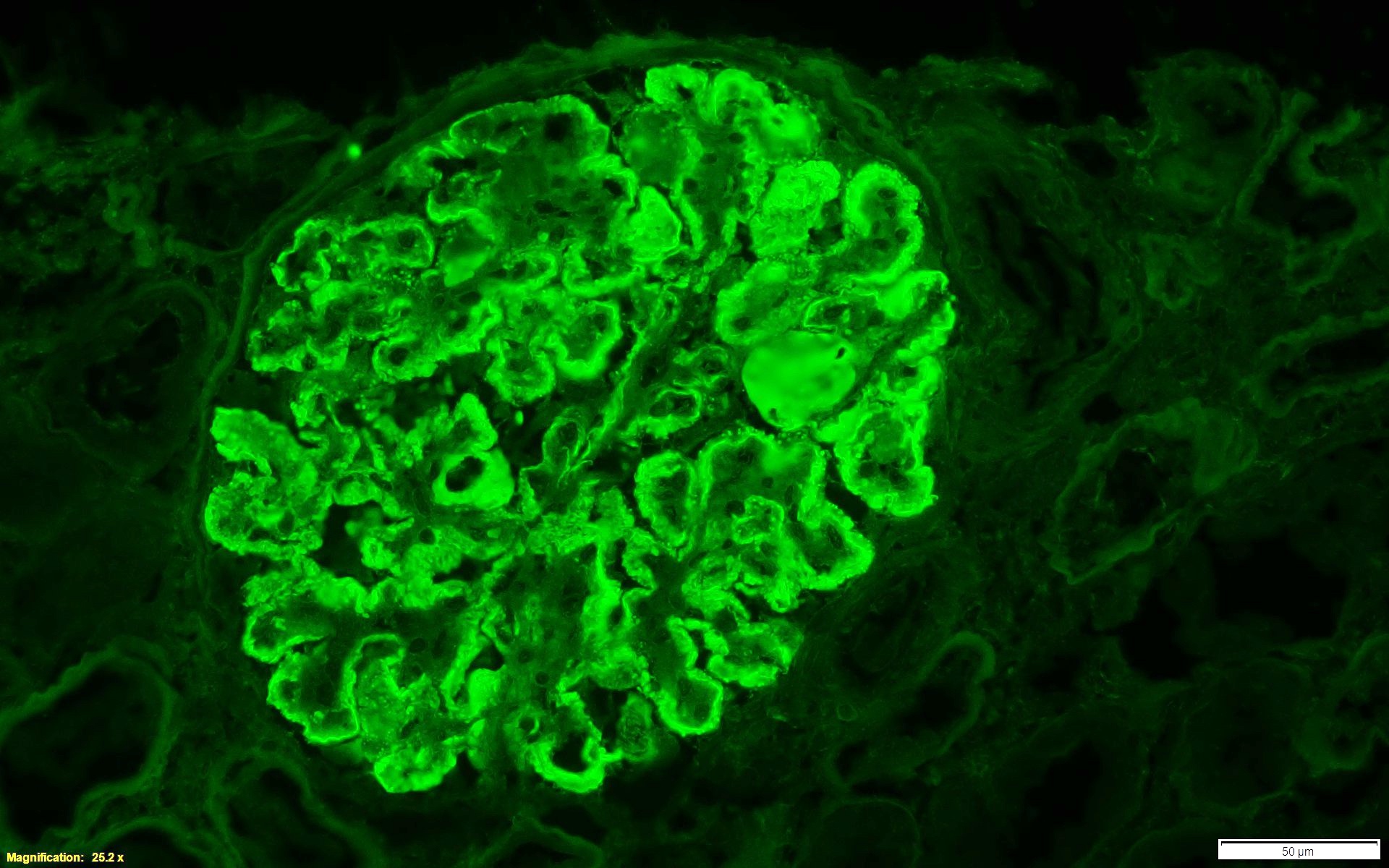
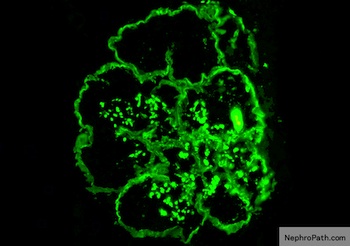
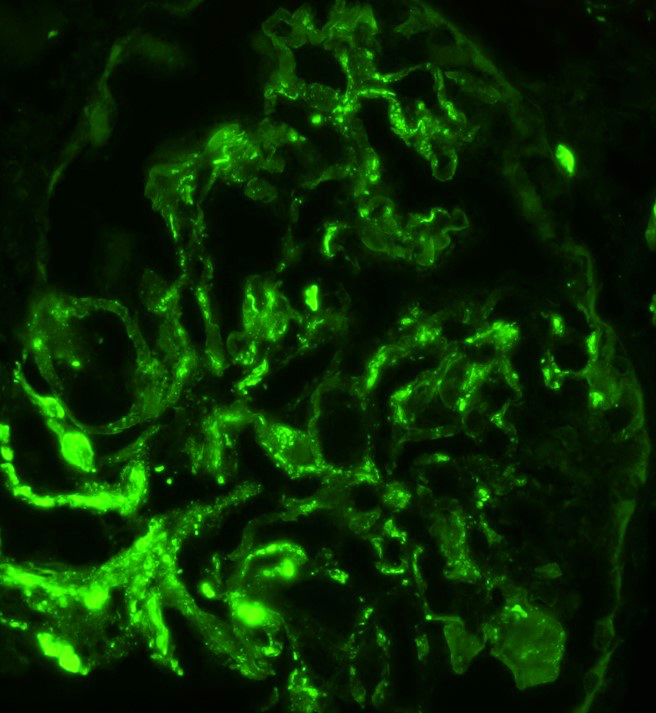
Immunofluorescence description
- Lumpy bumpy (granular) for C3, IgG, early complement (C1q, C4) at subendothelial and mesangial areas
Immunofluorescence images
Contributed by Haiyan Zhang, M.D., Ph.D. and Nephropath
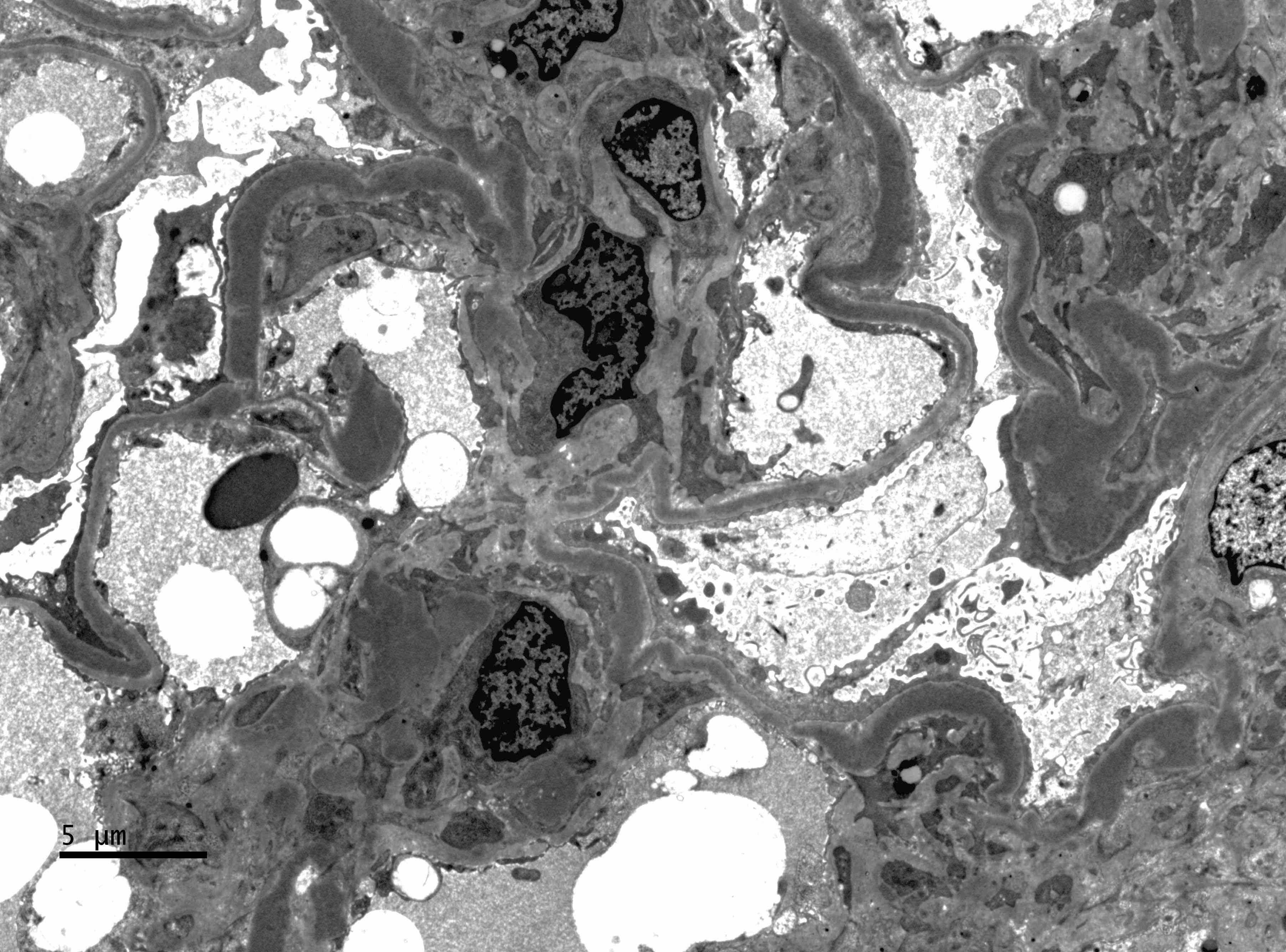
Electron microscopy description
- Subendothelial and mesangial electron dense deposits, mesangial interpositioning with splitting and duplication of basement membrane, possible increased mesangial matrix, variable degree of foot process effacement
Electron microscopy images
Contributed by Haiyan Zhang, M.D., Ph.D. and Nephropath
Type II: dense deposit
Definition / general
Case reports
Treatment
Microscopic (histologic) description
Microscopic (histologic) images
Contributed by Haiyan Zhang, M.D., Ph.D.
Contributed by Nephropath
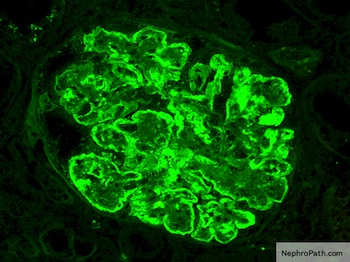
Immunofluorescence description
Immunofluorescence images
Contributed by Haiyan Zhang, M.D., Ph.D.
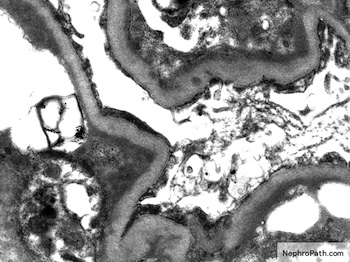
Electron microscopy description
Electron microscopy images
Contributed by Haiyan Zhang, M.D., Ph.D.
Images hosted on other servers:
- Essential diagnostic feature based on the presence of highly electron dense ribbon-like deposits of the glomerular basement membrane
- Now categorized under C3 glomerulopathies
- Could be familial or associated with partial lipodystrophy (~5%)
- Due to uncontrolled activation of alternative complement pathway: autoantibodies, e.g. C3 nephritic factor detected in 80 - 85% cases (stabilizes C3 convertase; promotes C3 degradation); gene mutation complement component, e.g. factor H
- Can be acquired by infections or monoclonal paraprotein
- Average age at diagnosis: 14 years
- Typically present with renal insufficiency, nearly all with hematuria and 33% with nephrotic syndrome
- Also deposits in basement membranes of spleen, choroid and Bruch membrane of retina
- Poorer prognosis than type I; 50% have renal failure in 10 years; 80 - 100% recur after renal transplant
Case reports
- 9 year old girl presented with macrohematuria and persistent proteinuria (Clin Nephrol Case Stud 2020;8:96)
- 35 year old man with partial lipoatrophy presented with leg edema and oliguria (Kidney Int 2020;98:1355)
Treatment
- Currently, no targeted therapies are available in clinical settings for the treatment of C3 glomerulopathy, although several new molecules are under investigation
- Treatment with corticosteroids plus mycophenolate mofetil has been shown to be associated with improved renal outcomes, as compared with other immunosuppressive regimens
- Yet, the main determinants of treatment response with this regimen and the influence of the underlying pathogenic drivers have not been extensively studied
- Therapeutic response to eculizumab, an anti-C5 monoclonal antibody, has been shown to be highly heterogeneous (Nephron 2020;144:272)
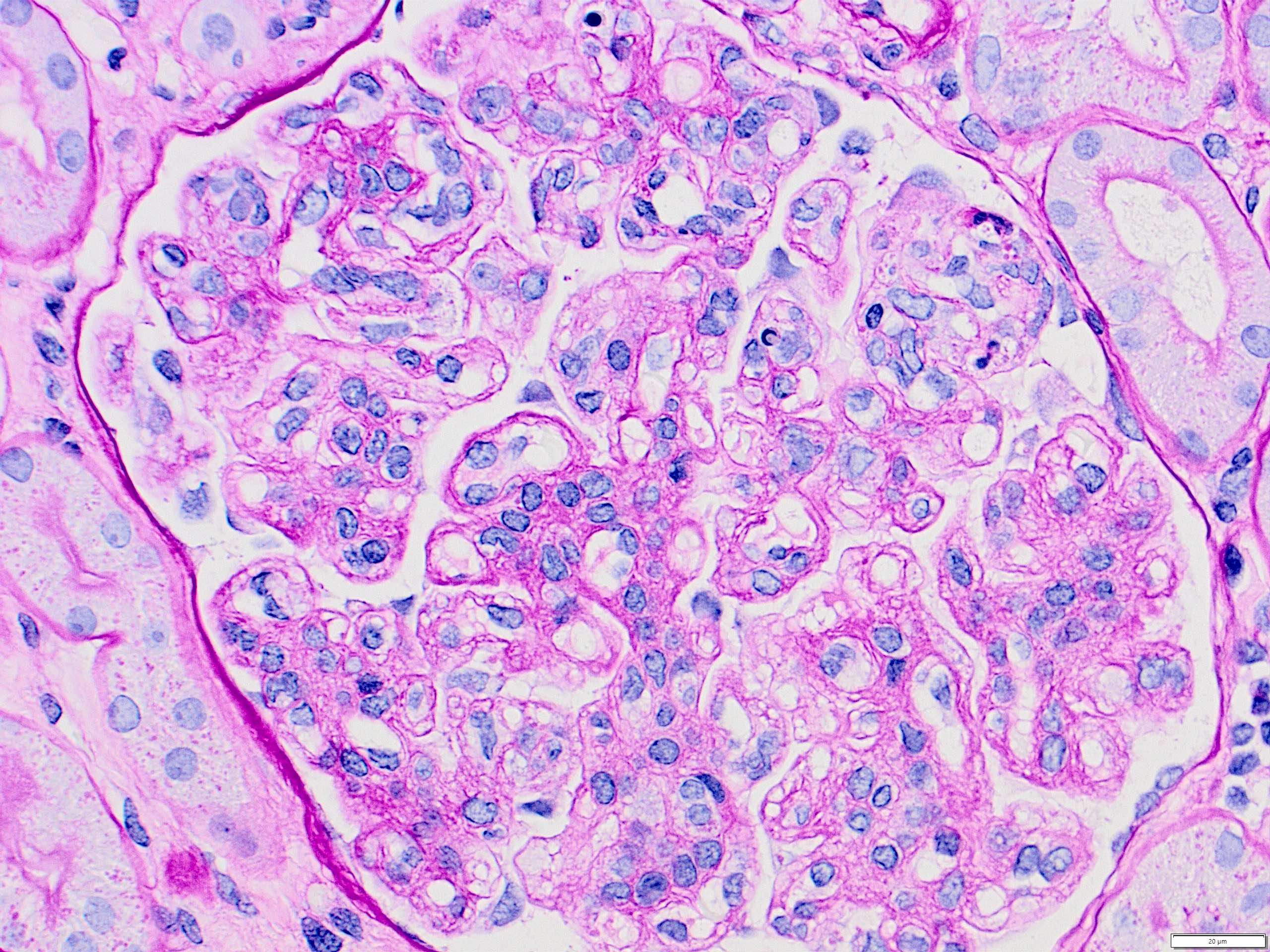
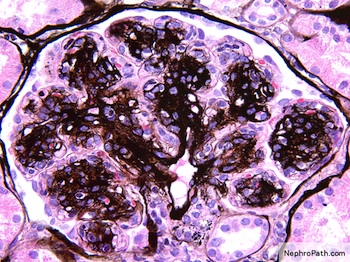
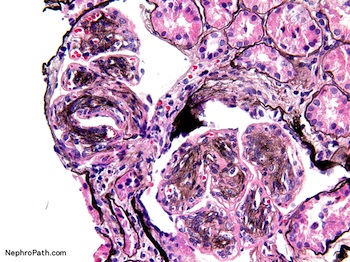
Microscopic (histologic) description
- Similar to type I but less prominent cellular proliferation
- Eosinophilic, refractile and ribbon-like thickening of glomerular basement membrane and basement membrane of Bowman capsule and tubules
- Strongly PAS+, stains red with trichrome but dense deposits are pale with silver stain
- Reference: Am J Kidney Dis 2015;66:e21
Microscopic (histologic) images
Contributed by Haiyan Zhang, M.D., Ph.D.
Contributed by Nephropath
Immunofluorescence description
- C3 only or C3 dominant
- C3 irregularly along capillary wall in ribbon-like, granular or discontinuous pattern
- C3 in mesangium with characteristic globular pattern
- Broad linear deposits of TBM (~60%) or Bowman capsule (~30%)
- Reference: Am J Kidney Dis 2015;66:e21
Immunofluorescence images
Contributed by Haiyan Zhang, M.D., Ph.D.
Electron microscopy description
- Highly dense deposits in lamina densa of glomerular basement membrane with ribbon / sausage string appearance
- Nodular deposits of similar material in mesangium
- Similar deposits in TBM (~50%) or Bowman capsule (~45%)
- Reference: Am J Kidney Dis 2015;66:e21
Electron microscopy images
Contributed by Haiyan Zhang, M.D., Ph.D.
Images hosted on other servers:
Type III: mixed
Definition / general
- MPGN pattern with subendothelial and subepithelial deposits
- Some overlapping with new category of C3 glomerulopathies
- 2 rare morphologic subtypes (Anders and Burkholder variants) that are clinically similar to each other and to type I membranous glomerulonephritis
- Reference: Case Rep Nephrol Dial 2019;9:15
Type III: Anders-Strife variant
Definition / general
Electron microscopy description
Electron microscopy images
Images hosted on other servers:
- Hybrid of type I and II MPGN
Electron microscopy description
- Intramembranous deposits in addition to subendothelial and mesangial deposits
- Deposits extending from subendothelial to subepithelial, GBM lamina densa disruption with laminated / woven appearance
Electron microscopy images
Images hosted on other servers:
Type III: Burkholder variant
Definition / general
Electron microscopy description
Electron microscopy images
Images hosted on other servers:
- Combined features of type I MPGN and membranous glomerulonephritis
- Associated with hepatitis C and HIV coinfection
Electron microscopy description
- Subepithelial deposits similar to membranous glomerulonephritis in addition to subendothelial and mesangial deposits
Electron microscopy images
Images hosted on other servers:
Board review style question #1
A 15 year old boy presents with nephritis syndrome with rising creatine. Urine protein 3 g/24 h, urine red blood cells 5 - 10/high power field, hepatitis B and C negative, C3 decreased, normal C4, ANCA negative, anti-GBM negative, no M spike by serum protein electrophoresis or urine protein electrophoresis. Renal biopsy is performed. Light microscopy shows diffuse global endocapillary hypercellularity with rare cellular crescent. Immunofluorescence studies show IgG weak-1+, IgM weak, IgA negative, C3+ (granular, capillary and mesangial), C1q negative, kappa weak and lambda weak. Electron microscopy shows intramembranous and mesangial deposits as in the picture. What is the most acute diagnosis?
- C3 glomerulonephritis
- Dense deposit disease
- Immune complex mediated membranoproliferative glomerulonephritis
- Thrombotic microangiopathy
Board review style answer #1
Board review style question #2
What type of cell injury is the initial trigger for MPGN type glomerulonephritis?
- Endothelial cell
- Mesangial cell
- Parietal epithelial cell
- Podocyte / visceral epithelial cell
Board review style answer #2