Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Diagrams / tables | Clinical features | Diagnosis | Laboratory | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Gross images | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Davis D, Andeen NK. Takayasu arteritis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/kidneynontumortakayasuarteritis.html. Accessed April 25th, 2024.
Definition / general
- Rare large vessel vasculitis
- Usually occurs in patients younger than 50 years old
- May present with renovascular hypertension, anecdotal association with wide range of renal glomerulopathies
Essential features
- Takayasu arteritis usually involves aorta and its major branches
- Inflammation is granulomatous with lymphoplasmacytic infiltrate and varying numbers of giant cells
- Renal disease is present in most cases, usually as nonspecific changes due to chronic hypertension and renal artery stenosis and other vascular changes (Clin Exp Rheumatol 2007;25:S10)
Terminology
- Pulseless disease
ICD coding
- ICD-10: M31.4 - aortic arch syndrome [Takayasu]
Epidemiology
- Incidence varies: 0.9/million (U.S.); 4.7 - 33/million (Europe); 40/million (Japan) (Int J Nephrol Renovasc Dis 2018;11:225)
- F:M also varies; overall is 8.2 - 9.7:1 but is 1.6 - 2:1 in Middle East and India (J Autoimmun 2014;48:79)
- Women frequently have involvement of the thoracic aorta and its branches
- Men are more likely to have involvement of abdominal aorta and its branches
- Patients commonly 20 - 40 years old (Best Pract Res Clin Rheumatol 2010;24:871)
- Renal artery involvement in Takayasu arteritis is higher in Asian populations and overall ranges from 11.5% to 62%
Sites
- Aorta and its major branches
- Kidney
Pathophysiology
- Genetic predisposition plus environmental factors
- Virus or bacteria via molecular mimicry mechanism leads to autoimmune response (Pathogens 2018;7:E73)
- Inflammatory cells implicated include gamma delta, CD4 and CD8 T cells, natural killer cells, macrophages, dendritic cells and B cells (Am J Med Sci 2013;346:314)
- Autoantibodies include antiaortic, antiendothelial and circulating immune complexes (Autoimmun Rev 2017;16:146)
- Associated with HLA-B genes, especially HLA-B*52 and HLA-B*67 in certain populations and TNFα genes (Int J Nephrol Renovasc Dis 2018;11:225)
- 2 stages of disease:
- Early inflammatory stage with nonspecific symptoms and transmural inflammation
- Later pulseless phase with hypertension, ischemia and occlusive changes including intimal fibrosis
Etiology
- Precise etiology unknown; likely multifactorial with genetic component and potentially viral or bacterial instigator (Pathogens 2018;7:E73)
Clinical features
- Usually subclinical or nonspecific symptoms at disease onset
- Constitutional symptoms (night sweats, weight loss, fever)
- Limb fatigue and pain, different or absent pulses in extremities, blood pressure difference or unobtainable blood pressure (J Autoimmun 2014;48:79)
Diagnosis
- Chapel Hill Consensus Conference 2012: large vessel vasculitis of patients < 50 years old
- 1990 American College of Rheumatology Classification Criteria for Takayasu arteritis: 3 or more of the following criteria yields a sensitivity of 90.5% and a specificity of 97.8% (Arthritis Rheum 1990;33:1129):
- Age at disease onset < 40 years
- Claudication of extremities
- Decreased brachial artery pulse
- Blood pressure difference > 10 mm Hg
- Bruit over subclavian arteries or aorta
- Arteriogram abnormality
Laboratory
- Nonspecific
- Elevated acute phase reactants seen, including erythrocyte sedimentation rate, C reactive protein and IL6
- IL6 best correlates with degree of disease (Am J Med Sci 2013;346:314, Int J Nephrol Renovasc Dis 2018;11:225)
Radiology description
- Early: arterial wall thickening and enhancement
- Late: arterial stenosis, occlusions, aneurysms (AJR Am J Roentgenol 2005;184:1427)
Radiology images
Prognostic factors
- Advances in imaging leading to early detection has improved outcomes (Int J Cardiol 2013;168:3)
- Disease course generally indolent with 10 year survival ranging from 67.4% to 100%, depending on patient ethnicity (Int J Nephrol Renovasc Dis 2018;11:225)
Case reports
- 3 toddlers with constitutional symptoms and malignant hypertension (Pediatr Nephrol 2009;24:1227)
- 15 year old girl with oliguria and acute kidney injury (J Bras Nefrol 2019;41:564)
- 31 year old woman with proteinuria (Clin Res Cardiol 2020;109:1438)
- 54 year old man with progressive edema and nephrotic proteinuria (Case Rep Nephrol Urol 2014;4:60)
- 6 patients with glomerulopathy (Chin Med Sci J 2009;24:69)
Treatment
- Glucocorticoids and other immunosuppressive therapy including methotrexate, azathioprine and cyclophosphamide
- New studies show success with biologic therapy: anti-TNFα, anti-IL6R and monoclonal antibodies (Curr Opin Rheumatol 2014;26:7)
- Surgical repair: stent or bypass, depending on length of segment (Circulation 2012;125:813, Rheumatology (Oxford) 2006;45:600)
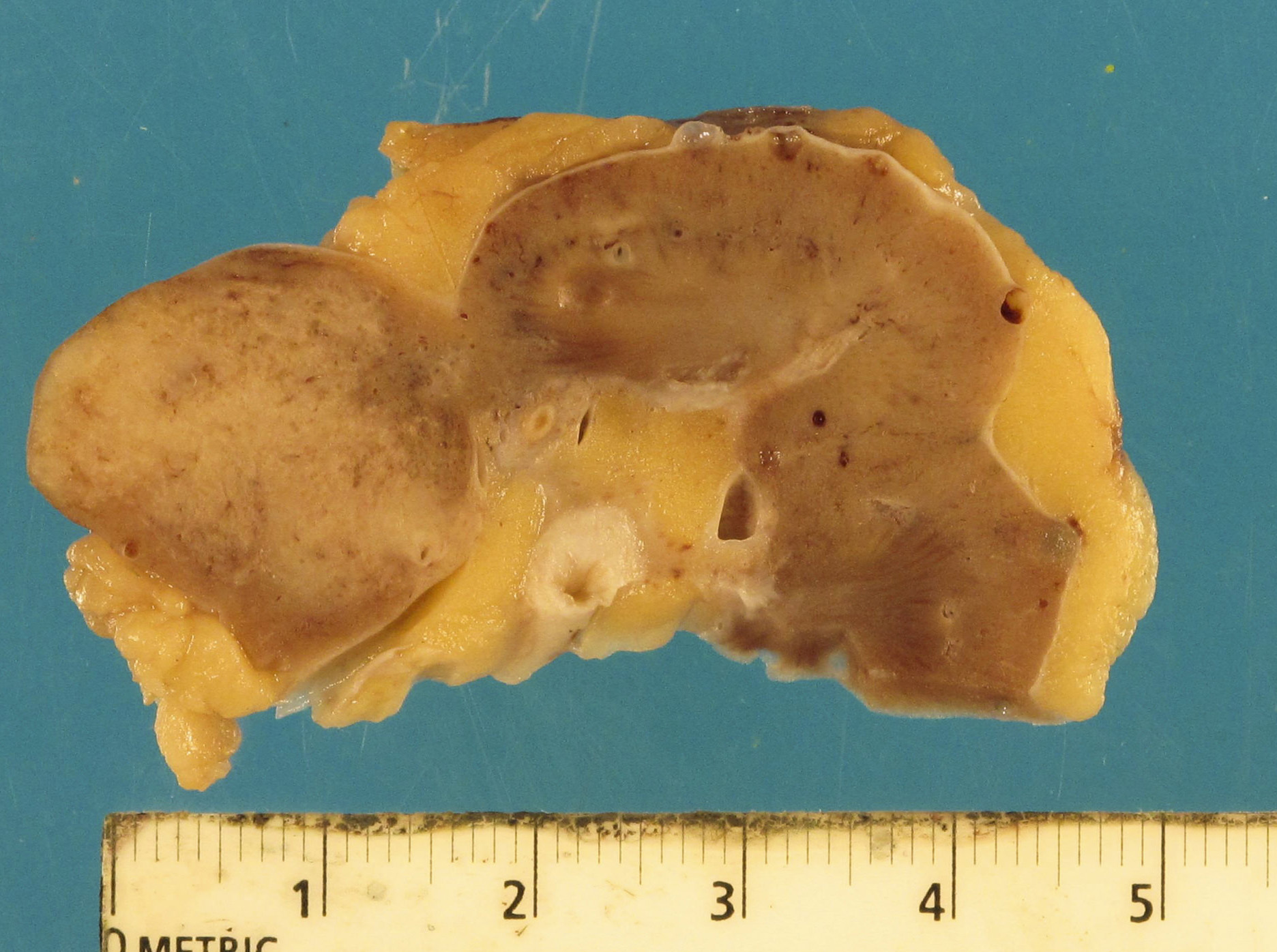
Gross description
- Vascular sclerosis, nonspecific scarring, ill defined white mass-like lesions
Microscopic (histologic) description
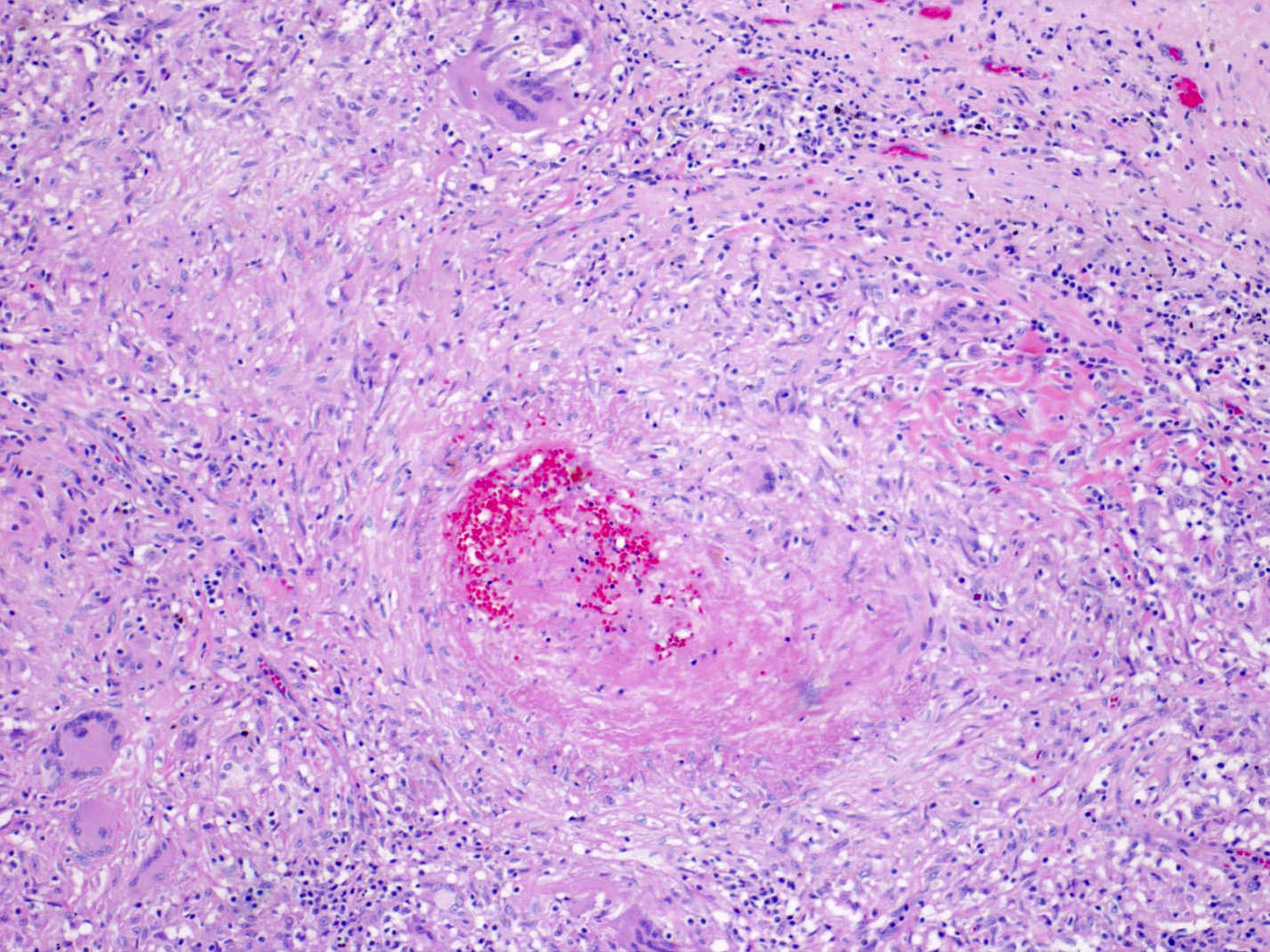
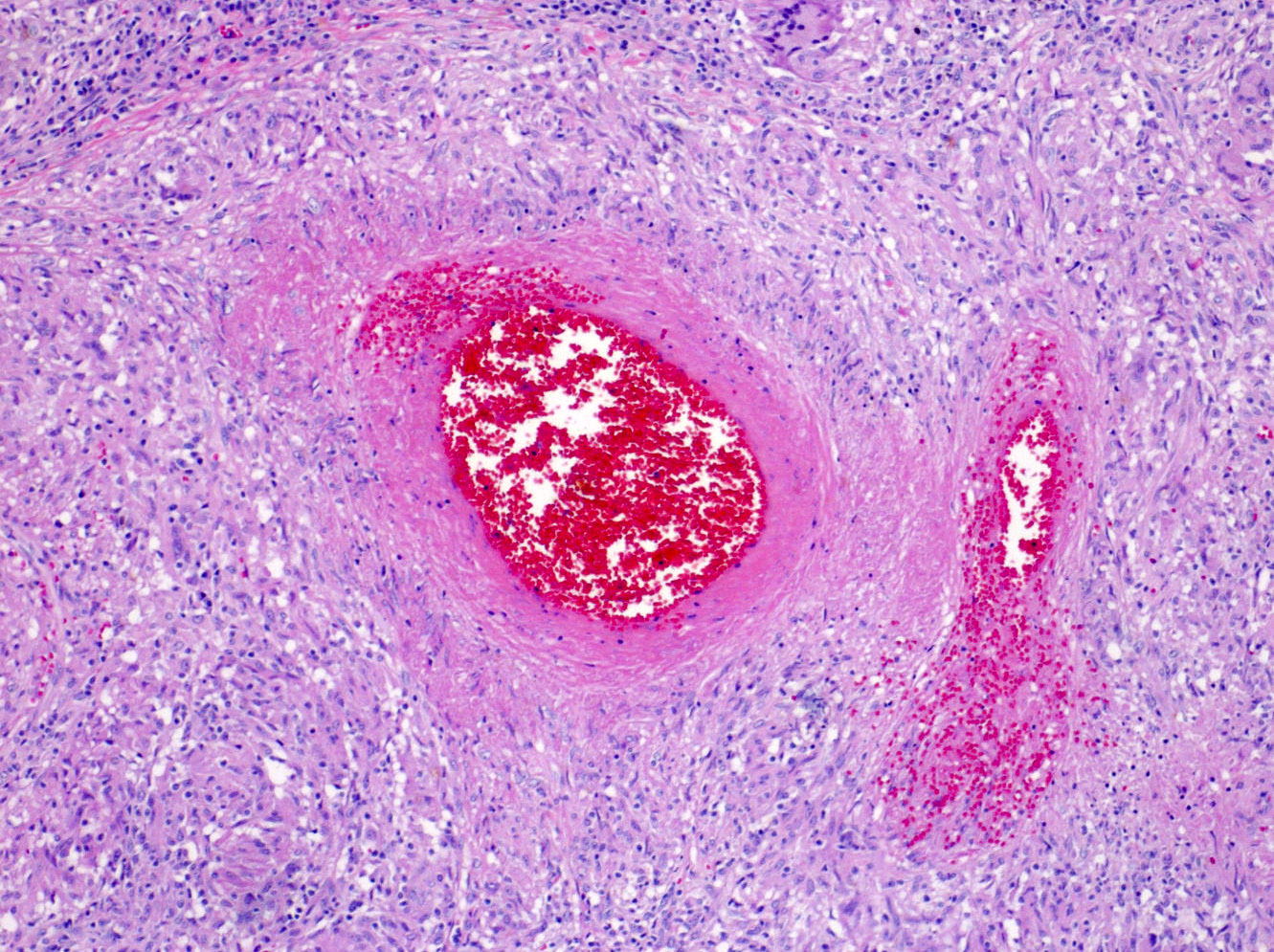
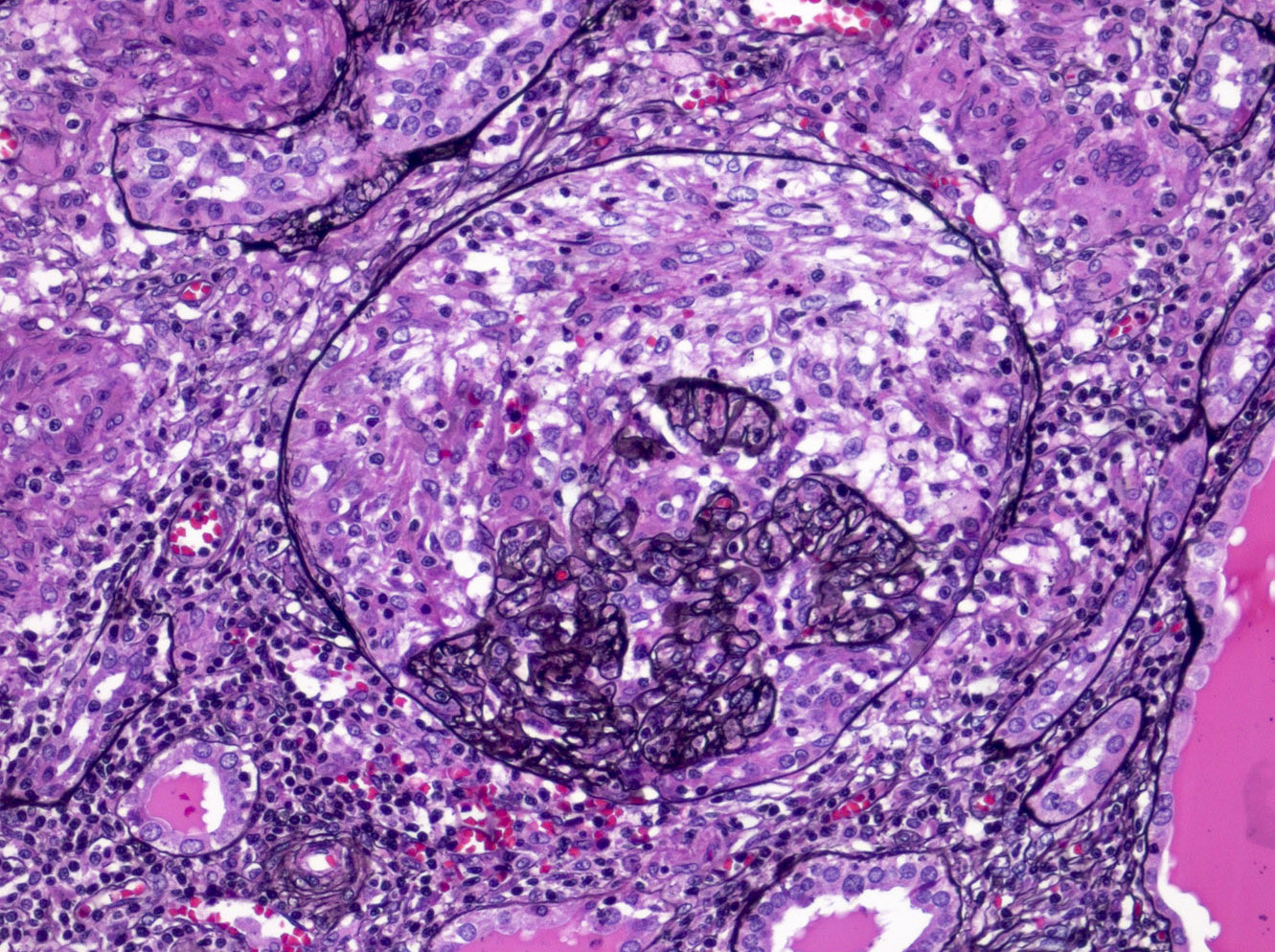
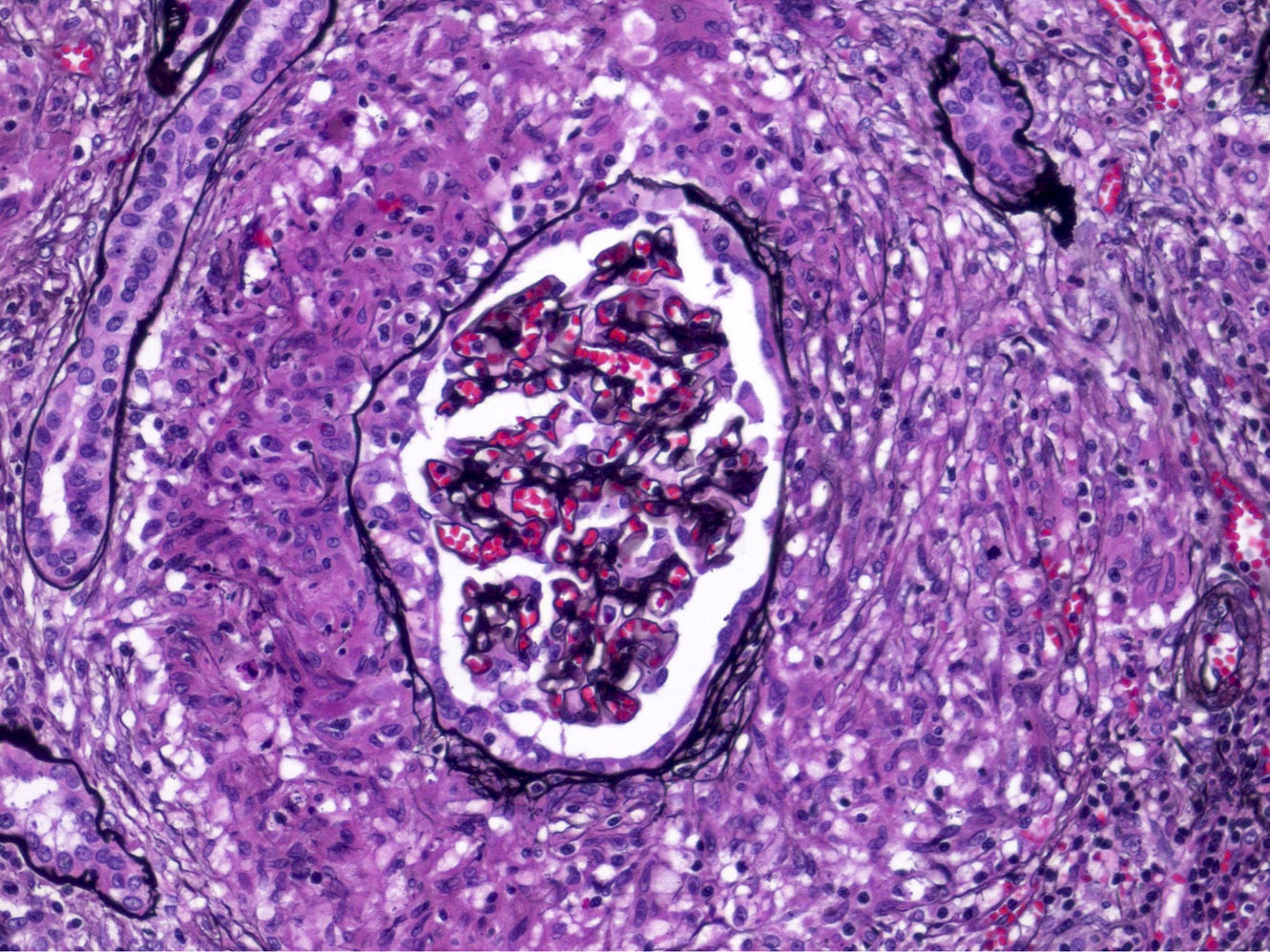
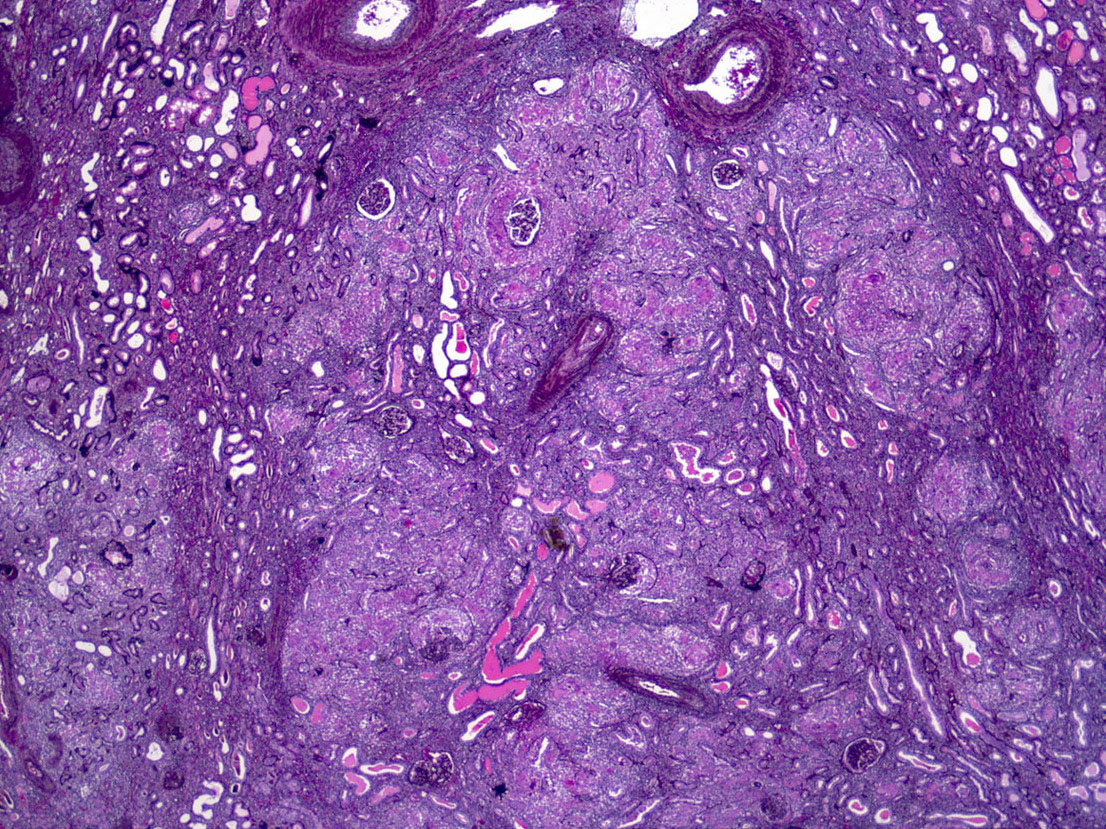
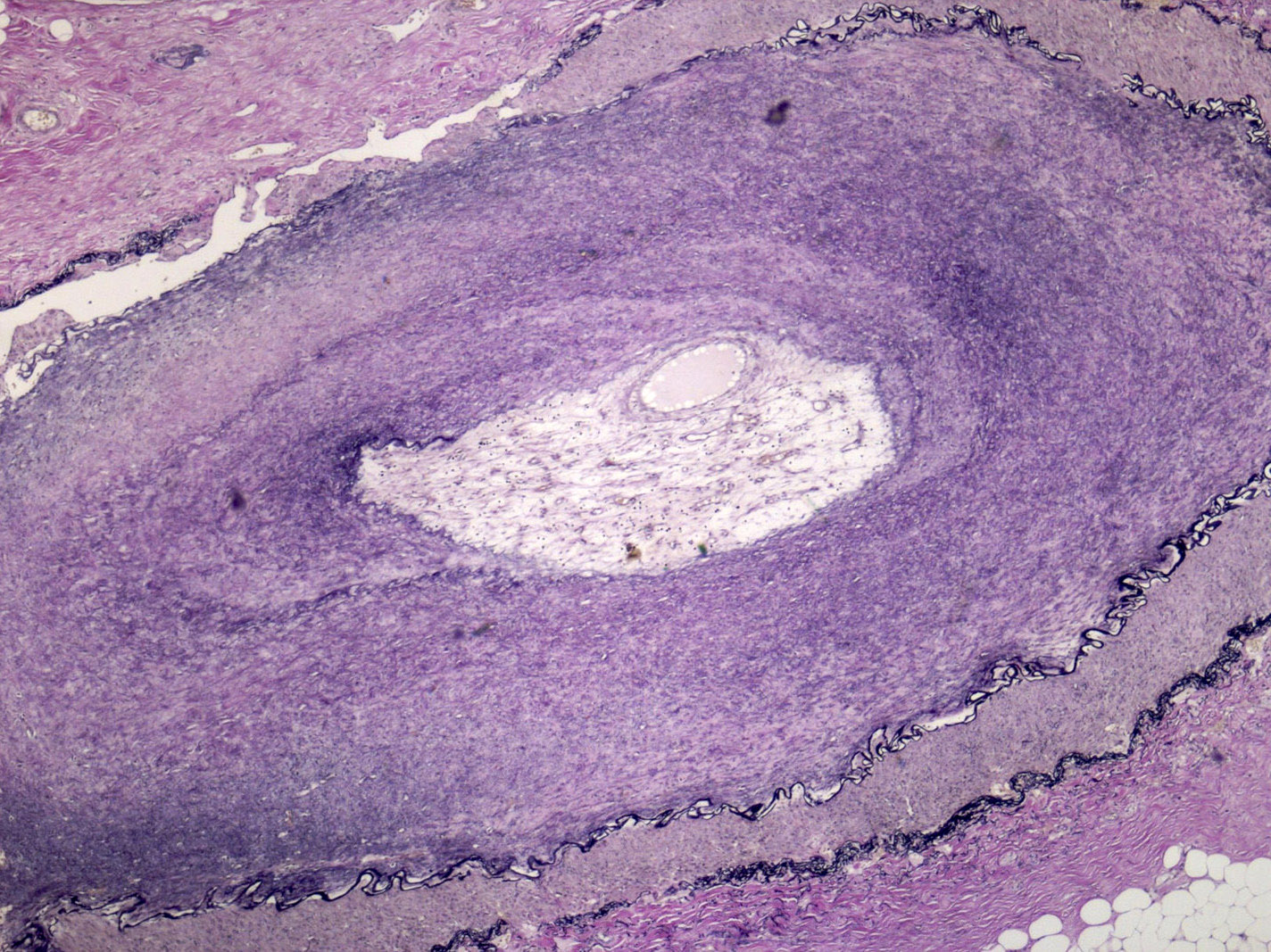
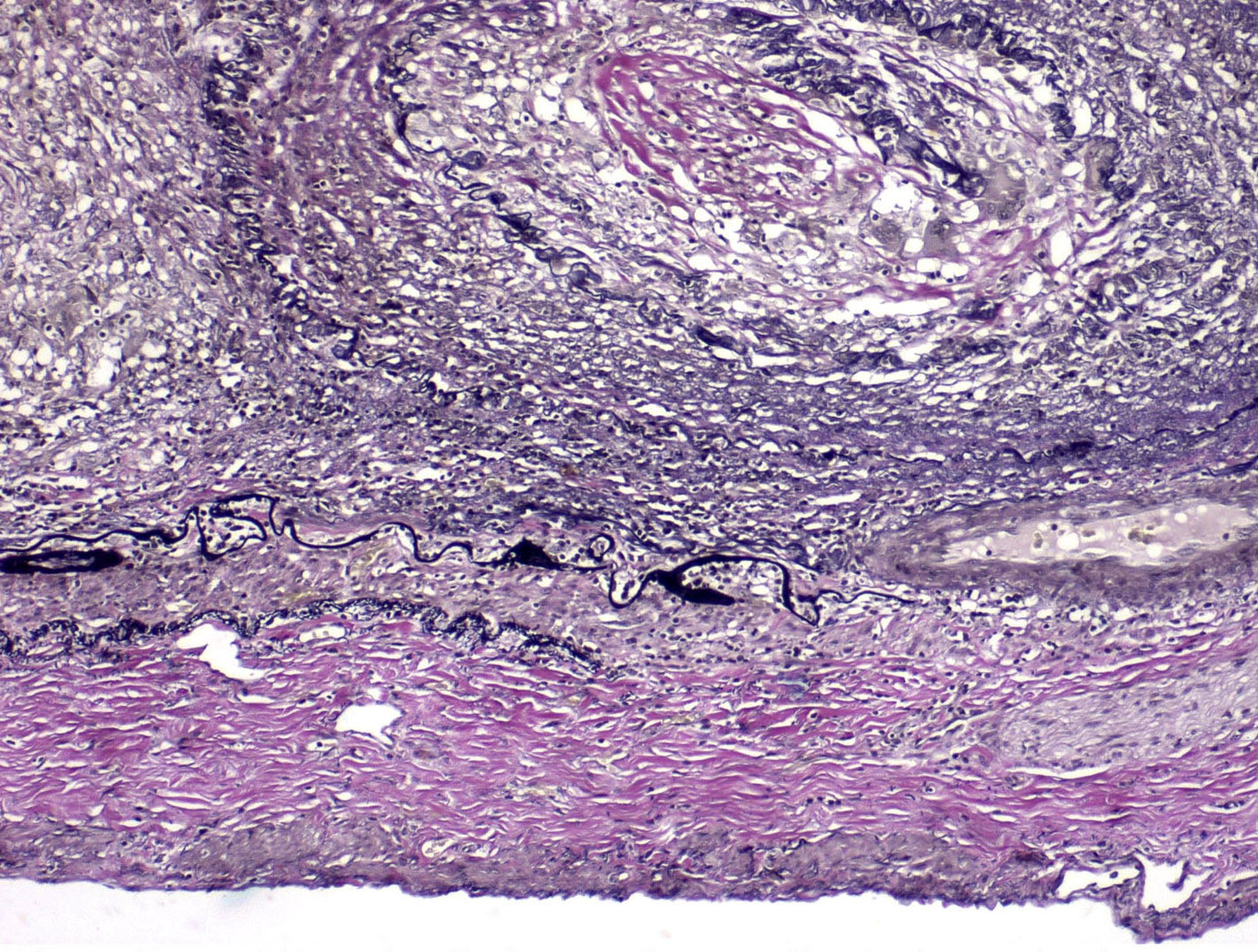
- Granulomatous vasculitis with mixed inflammatory infiltrate, including giant cells, with necrosis, disruption of the elastic lamina and features of recanalization (Int J Nephrol Renovasc Dis 2018;11:225)
- Varying renal vascular and parenchymal changes associated with the degree of chronic hypertension and renal ischemia: atherosclerosis, ischemic change, atrophy, infiltrating lymphocytes, tubular dilation and narrowing and glomerulosclerosis
- Specific glomerular and tubulointerstitial changes are rare and often manifestations of chronic disease (Chin Med Sci J 2009;24:69)
- Reported glomerular disease includes: mesangial proliferative glomerulonephritis, IgA nephropathy, membranous glomerulonephropathy, membranoproliferative glomerulonephropathy, crescentic glomerulonephropathy, renal amyloidosis and focal glomerulosclerosis (Clin Exp Rheumatol 2007;25:S10)
Microscopic (histologic) images
Positive stains
- Elastin will show disruption of the elastic lamina
- Use immune cell markers as needed
Negative stains
- Fungal, viral, spirochete, acid fast stains to rule out infectious etiologies for granulomatous inflammation
Sample pathology report
- Right kidney, nephrectomy:
- Arteritis with granulomatous inflammation and multinucleated giant cells, active and chronic (see comment)
- Comment: Differential diagnosis for the large vessel vasculitis includes Takayasu arteritis and giant cell arteritis. Other etiologies for the vasculitis include antineutrophil cytoplasmic antibody associated vasculitis, necrotizing sarcoid vasculitis, polyarteritis nodosa or possibly infection. No acid fast or fungal organisms are identified on special stains. Takayasu arteritis usually affects the aorta and its major branches and is more common in women under the age of 50.
Differential diagnosis
- Giant cell arteritis:
- Patient population usually > 50 years, M:F = 1:2
- More common in Caucasian populations
- Temporal artery most frequently involved
- Usually presents with polymyalgia rheumatica and localized headache
- Giant cell arteritis seen in medial layer rather than transmural (Ann Rheum Dis 2012;71:1329, Medicine (Baltimore) 2009;88:221, Int J Rheum Dis 2019;22:41)
- Fibromuscular dysplasia:
- Younger female patients
- Multiple arteries are involved including renal and carotid
- Fibromuscular thickening of media with irregular thinning and loss of internal elastic lamina
- Not a large vessel vasculitis
- Aorta is usually not involved (J Am Soc Hypertens 2018;12:506)
- Atherosclerosis:
- Usually older patients
- Primarily intimal sclerosis, eccentric (Int J Cardiol 2013;168:3)
- Not a large vessel vasculitis
- Infectious vasculitis:
- Rickettsial, bacterial, fungal, viral organisms
- Not typically a large vessel vasculitis
- Granulomatous vasculitis due to sarcoidosis:
- Sarcoid may cause a large vessel vasculitis mimicking Takayasu arteritis
- Distinguish clinically (Clin Exp Rheumatol 2000;18:401)
- Isolated granulomatous arteritis:
- Associated with Marfan syndrome (J Clin Pathol 2012;65:362)
- Medial and cystic necrosis that is not usually transmural
Additional references
Board review style question #1
Which feature associated with Takayasu arteritis helps to distinguish it from other vascular injury processes?
- Granulomatous transmural vascular inflammation with giant cells
- Granulomatous vascular inflammation with giant cells of arterial media
- Positive for antineutrophilic cytoplasmic antibody
- Vascular changes limited to arterial intima
Board review style answer #1
A. Granulomatous transmural vascular inflammation with giant cells
Comment here
Reference: Takayasu arteritis
Comment here
Reference: Takayasu arteritis
Board review style question #2
Board review style answer #2
D. Vasculitis with giant cells, consider Takayasu arteritis
Comment here
Reference: Takayasu arteritis
Comment here
Reference: Takayasu arteritis